The Feasibility and Early Results of Multivessel Minimally Invasive Coronary Artery Bypass Grafting for All Comers
Abstract
:1. Introduction
2. Methods
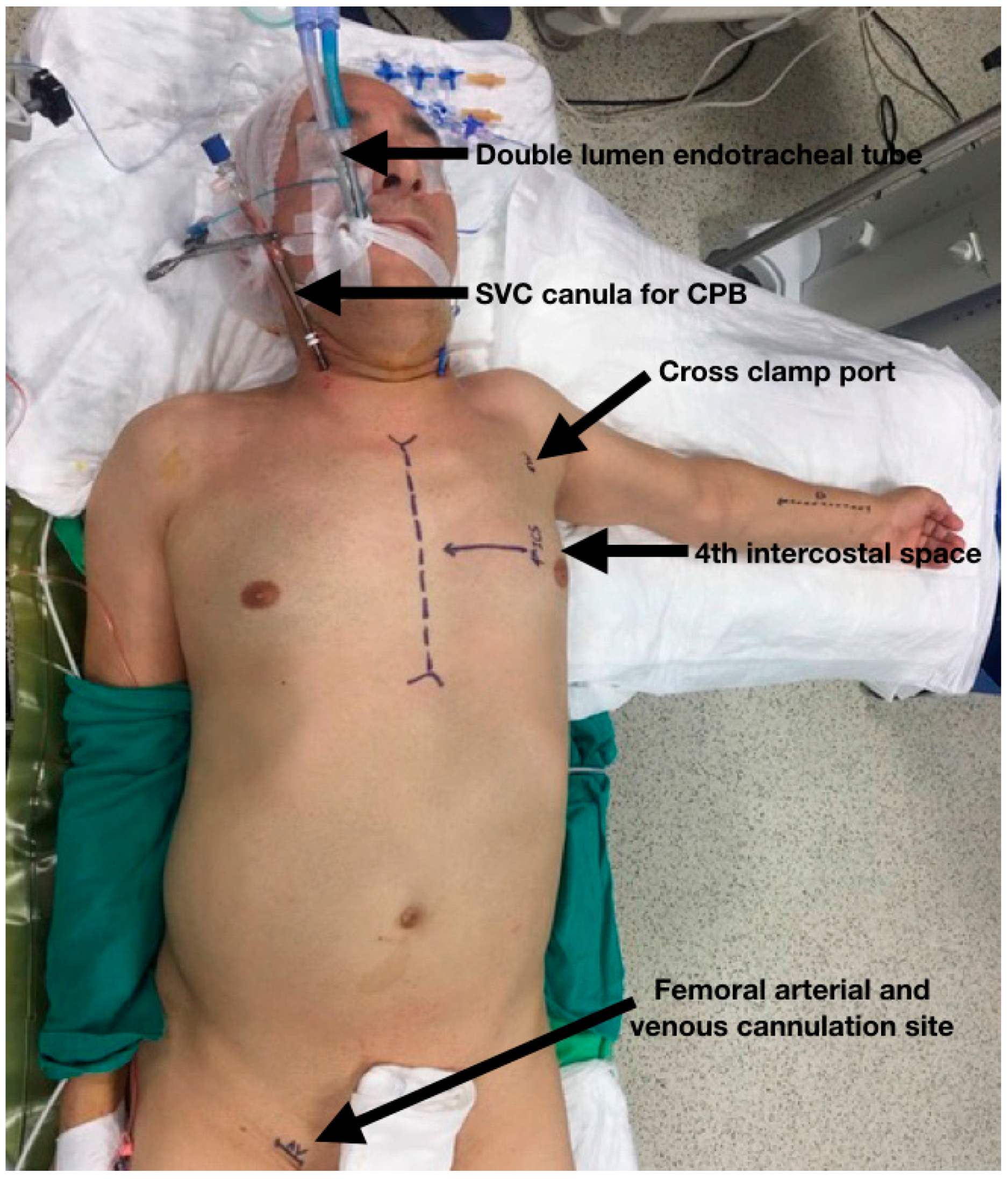
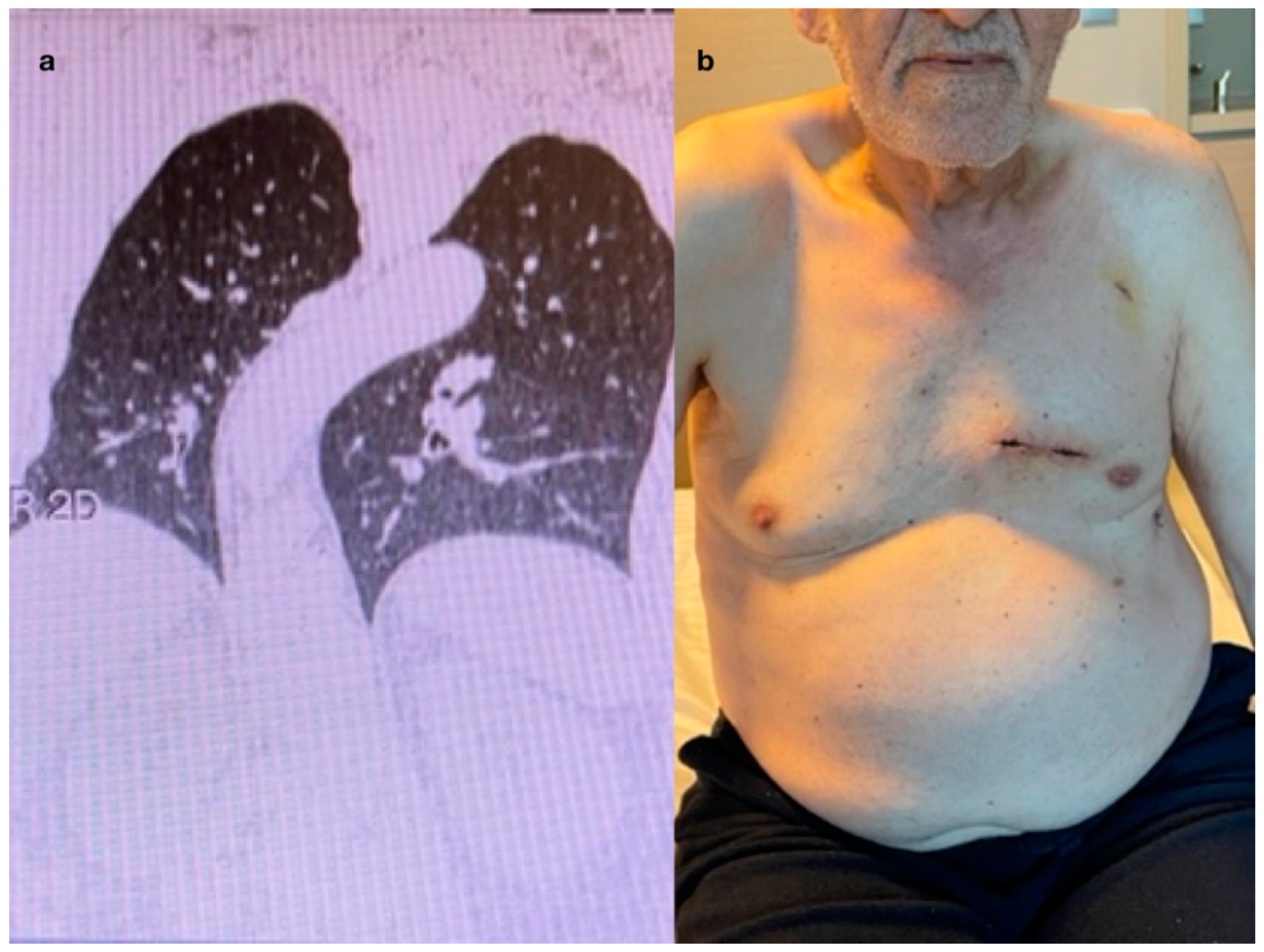
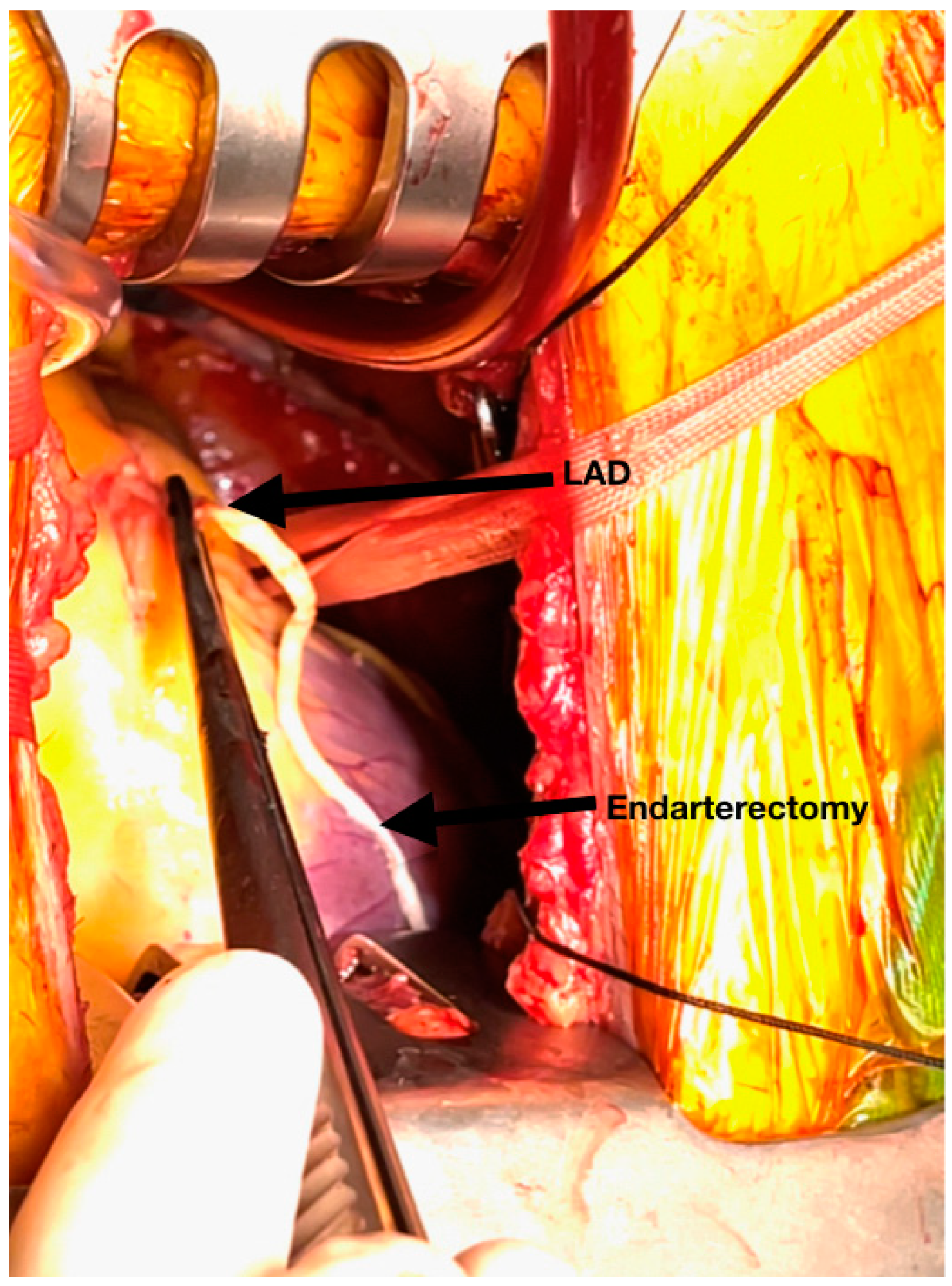
2.1. Preoperative Preparation and Operative Technique
Perioperative Details (Video)
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benedetto, U.; Altman, D.G.; Gerry, S.; Gray, A.; Lees, B.; Pawlaczyk, R.; Flather, M.; Taggart, D.P.; Arterial Revascularization Trial investigators. Pedicled and skeletonized single and bilateral internal thoracic artery grafts and the incidence of sternal wound complications: Insights from the Arterial Revascularization Trial. J. Thorac. Cardiovasc. Surg. 2016, 152, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Abu-Omar, Y.; Kocher, G.J.; Bosco, P.; Barbero, C.; Waller, D.; Gudbjartsson, T.; Sousa-Uva, M.; Licht, P.B.; Dunning, J.; Schmid, R.A.; et al. European Association for Cardio-Thoracic Surgery expert consensus statement on the prevention and management of mediastinitis. Eur. J. Cardiothorac. Surg. 2017, 51, 10–29. [Google Scholar] [CrossRef] [PubMed]
- Kaspersen, A.E.; Nielsen, S.J.; Orrason, A.W.; Petursdottir, A.; Sigurdsson, M.I.; Jeppsson, A.; Gudbjartsson, T. Short- and long-term mortality after deep sternal wound infection following cardiac surgery: Experiences from SWEDEHEART. Eur. J. Cardiothorac. Surg. 2021, 60, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Barnason, S.; Zimmerman, L.; Nieveen, J.; Schulz, P.; Miller, C.; Hertzog, M.; Tu, C. Influence of a symptom management telehealth intervention on older adults’ early recovery outcomes after coronary artery bypass surgery. Heart Lung 2009, 38, 364–376. [Google Scholar] [CrossRef]
- Bonatti, J.; Wallner, S.; Crailsheim, I.; Grabenwöger, M.; Winkler, B. Minimally invasive and robotic coronary artery bypass grafting-a 25-year review. J. Thorac. Dis. 2021, 13, 1922–1944. [Google Scholar] [CrossRef]
- Calafiore, A.M.; Giammarco, G.D.; Teodori, G.; Bosco, G.; D’Annunzio, E.; Barsotti, A.; Maddestra, N.; Paloscia, L.; Vitolla, G.; Sciarra, A.; et al. Left anterior descending coronary artery grafting via left anterior small thoracotomy without cardiopulmonary bypass. Ann. Thorac. Surg. 1996, 61, 1658–1663; discussion 1664–1665. [Google Scholar] [CrossRef]
- McGinn, J.T., Jr.; Usman, S.; Lapierre, H.; Pothula, V.R.; Mesana, T.G.; Ruel, M. Minimally invasive coronary artery bypass grafting: Dual-center experience in 450 consecutive patients. Circulation 2009, 120 (Suppl. 11), S78–S84. [Google Scholar] [CrossRef]
- Andrawes, P.A.; Shariff, M.A.; Nabagiez, J.P.; Steward, R.; Azab, B.; Povar, N.; Sarza, M.; Demissie, S.; Sadel, S.M.; Nichols, M.; et al. Evolution of Minimally Invasive Coronary Artery Bypass Grafting: Learning Curve. Innovations 2018, 13, 81–90. [Google Scholar] [CrossRef]
- Rodriguez, M.L.; Lapierre, H.R.; Sohmer, B.; Glineur, D.; Ruel, M. Mid-Term Follow-up of Minimally Invasive Multivessel Coronary Artery Bypass Grafting: Is the Early Learning Phase Detrimental? Innovations 2017, 12, 116–120. [Google Scholar] [CrossRef]
- Liu, J.J.; Liang, L.; Kong, Q.Y.; Ma, X.L.; Chi, L.Q.; Lai, Y.Q. A study on the perioperative effects of obesity on minimally invasive coronary artery bypass grafting and its surgical techniques. Interdiscip. Cardiovasc. Thorac. Surg. 2023, 36, ivad092. [Google Scholar] [CrossRef]
- Mastroiacovo, G.; Manganiello, S.; Pirola, S.; Tedesco, C.; Cavallotti, L.; Antona, C.; Alamanni, F.; Pompilio, G. Very Long-term Outcome of Minimally Invasive Direct Coronary Artery Bypass. Ann. Thorac. Surg. 2021, 111, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Repossini, A.; Di Bacco, L.; Nicoli, F.; Passaretti, B.; Stara, A.; Jonida, B.; Muneretto, C. Minimally invasive coronary artery bypass: Twenty-year experience. J. Thorac. Cardiovasc. Surg. 2019, 158, 127–138.e1. [Google Scholar] [CrossRef]
- Guo, M.H.; Toubar, O.; Issa, H.; Glineur, D.; Ponnambalam, M.; Vo, T.X.; Rahmouni, K.; Chong, A.Y.; Ruel, M. Long-Term Survival, Cardiovascular, and Functional Outcomes after Minimally Invasive Coronary Artery Bypass Grafting in 566 Patients. J. Thorac. Cardiovasc. Surg. 2023. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mavioglu, I.; Vallely, M.P. Minimally invasive off-pump anaortic coronary artery bypass (MACAB). J. Card. Surg. 2022, 37, 4944–4951. [Google Scholar] [CrossRef] [PubMed]
- Mavioglu, I. Minimally Invasive Off-Pump Anaortic Complete Arterial Coronary Artery Bypass: How to Do It? Innovations 2023. Epub ahead of print. [Google Scholar] [CrossRef]
- Vassiliades, T.A., Jr.; Reddy, V.S.; Puskas, J.D.; Guyton, R.A. Long-term results of the endoscopic atraumatic coronary artery bypass. Ann. Thorac. Surg. 2007, 83, 979–984; discussion 984–985. [Google Scholar] [CrossRef]
- Tomita, S.; Watanabe, G.; Tabata, S.; Nishida, S. Total Endoscopic Beating-Heart Coronary Artery Bypass Grafting Using A New 3D Imaging System. Innovations 2006, 1, 243–246. [Google Scholar] [CrossRef]
- Endo, Y.; Nakamura, Y.; Kuroda, M.; Ito, Y.; Hori, T. The Utility of a 3D Endoscope and Robot-Assisted System for MIDCAB. Ann. Thorac. Cardiovasc. Surg. 2019, 25, 200–204. [Google Scholar] [CrossRef]
- Kieser, T.M.; Rose, M.S.; Aluthman, U.; Narine, K. Quicker yet safe: Skeletonization of 1640 internal mammary arteries with harmonic technology in 965 patients. Eur. J. Cardiothorac. Surg. 2014, 45, e142–e150. [Google Scholar] [CrossRef]
- Mavioglu, I. Internal thoracic artery harvesting with a LigaSure device. Asian Cardiovasc. Thorac. Ann. 2019, 27, 707–709. [Google Scholar] [CrossRef]
- Jacobs, J.P.; Edwards, F.H.; Shahian, D.M.; Prager, R.L.; Wright, C.D.; Puskas, J.D.; Morales, D.L.; Gammie, J.S.; Sanchez, J.A.; Haan, C.K.; et al. Successful linking of the Society of Thoracic Surgeons database to social security data to examine survival after cardiac operations. Ann. Thorac. Surg. 2011, 92, 32–37; discussion 38–39. [Google Scholar] [CrossRef]
- Puskas, J.D.; Martin, J.; Cheng, D.C.; Benussi, S.; Bonatti, J.O.; Diegeler, A.; Ferdinand, F.D.; Kieser, T.M.; Lamy, A.; Mack, M.J.; et al. ISMICS Consensus Conference and Statements of Randomized Controlled Trials of Off-Pump Versus Conventional Coronary Artery Bypass Surgery. Innovations 2015, 10, 219–229. [Google Scholar] [CrossRef]
- Tachibana, K.; Kikuchi, K.; Narayama, K.; Okawa, A.; Iwashiro, Y.; Arihara, A.; Yamauchi, A. Minimally invasive coronary artery bypass grafting with ultrasonically skeletonized internal thoracic artery. JTCVS Tech. 2022, 14, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Oosterlinck, W.; Algoet, M.; Balkhy, H.H. Minimally Invasive Coronary Surgery: How Should It Be Defined? Innovations 2023, 18, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Mavioglu, I. Anaortic With No Touch to the Aorta Is a Central Technique to Decrease Invasiveness of CABG. Innovations 2023, 18, 295. [Google Scholar] [CrossRef] [PubMed]
- Balkhy, H.H.; Nisivaco, S.; Kitahara, H.; Torregrossa, G.; Patel, B.; Grady, K.; Coleman, C. Robotic off-pump totally endoscopic coronary artery bypass in the current era: Report of 544 patients. Eur. J. Cardiothorac. Surg. 2022, 61, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Taggart, D.P.; Thuijs, D.J.; Di Giammarco, G.; Puskas, J.D.; Wendt, D.; Trachiotis, G.D.; Kieser, T.M.; Kappetein, A.P.; Head, S.J. Intraoperative transit-time flow measurement and high-frequency ultrasound assessment in coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 2020, 159, 1283–1292.e2. [Google Scholar] [CrossRef]
- Gaudino, M.; Sandner, S.; Di Giammarco, G.; Di Franco, A.; Arai, H.; Asai, T.; Bakaeen, F.; Doenst, T.; Fremes, S.E.; Glineur, D.; et al. The Use of Intraoperative Transit Time Flow Measurement for Coronary Artery Bypass Surgery: Systematic Review of the Evidence and Expert Opinion Statements. Circulation 2021, 144, 1160–1171. [Google Scholar] [CrossRef]
- Thuijs, D.J.F.M.; Davierwala, P.; Milojevic, M.; Deo, S.V.; Noack, T.; Kappetein, A.P.; Serruys, P.W.; Mohr, F.W.; Morice, M.C.; Mack, M.J.; et al. SYNTAX Extended Survival Investigators. Long-term survival after coronary bypass surgery with multiple versus single arterial grafts. Eur. J. Cardiothorac. Surg. 2022, 61, 925–933. [Google Scholar] [CrossRef]
- Alsaleh, D.; Sun, E.; Alzahrani, A.; Itagaki, S.; Puskas, J.; Chikwe, J.; Egorova, N. Multiple arterial versus single arterial grafting in patients with diabetes undergoing coronary artery bypass surgery. JTCVS Open 2023, 13, 119–135. [Google Scholar] [CrossRef]
- Gillmore, T.; Rocha, R.V.; Fremes, S.E. Evidence-based selection of the second and third arterial conduit. JTCVS Open 2020, 5, 66–69. [Google Scholar] [CrossRef] [PubMed]
- Gaudino, M.; Audisio, K.; Di Franco, A.; Alexander, J.H.; Kurlansky, P.; Boening, A.; Chikwe, J.; Devereaux, P.J.; Diegeler, A.; Dimagli, A.; et al. Radial artery versus saphenous vein versus right internal thoracic artery for coronary artery bypass grafting. Eur. J. Cardiothorac. Surg. 2022, 62, ezac345. [Google Scholar] [CrossRef]
- Hamilton, G.W.; Raman, J.; Moten, S.; Matalanis, G.; Rosalion, A.; Dimagli, A.; Seevanayagam, S.; Gaudino, M.F.; Hare, D.L.; RAPCO Investigators. Radial artery vs. internal thoracic artery or saphenous vein grafts: 15-year results of the RAPCO trials. Eur. Heart J. 2023, 44, 2406–2408. [Google Scholar] [CrossRef] [PubMed]
- Arjomandi Rad, A.; Hajzamani, D.; Sardari Nia, P. Simulation-based training in cardiac surgery: A systematic review. Interdiscip. Cardiovasc. Thorac. Surg. 2023, 37, ivad079. [Google Scholar] [CrossRef] [PubMed]


| n (Percentage %) | |
|---|---|
| Mean age (y) (range) | 60.17 ± 10.3 |
| Female | 24 (10.4%) |
| BMI > 30 | 28.7 ± 4.4 |
| Chronic obstructive lung disease | 136 (59.1%) |
| Smoking | 133 (57.8%) |
| Hyperlipidemia | 136 (59.1%) |
| Hypertension | 147 (63.9%) |
| Diabetes mellitus | 147 (63.9%) |
| Cancer under remission | 9 (3.9%) |
| Patients on hemodialysis | 4 (1.7%) |
| Peripheral vascular disease | 39 (17.0%) |
| Porcelain aorta | 16 (7.0%) |
| Cerebrovascular disease | 10 (4.3%) |
| Previous myocardial infarction | 86 (37.4%) |
| EF (mean ± SD) | 53.4 ± 9.6 |
| Low EF < 30 | 14 (6.1%) |
| EF < 50 | 88 (38.3%) |
| Left main coronary artery disease | 9 (3.9%) |
| n (%) | |
|---|---|
| Bypass number (mean ± SD) | 3.0 ± 0.9 |
| Single bypass | 18 (7.8%) |
| Double bypass | 51 (22.2%) |
| Triple bypass | 90 (39.1%) |
| Quadruple bypass | 65 (28.3%) |
| Quintet bypass | 6 (2.6%) |
| LITA | 225 (97.8%) |
| RA | 88 (38.2%) |
| RITA | 2 (0.9%) |
| RCA bypass | 138 (60.0%) |
| Sequential | 83 (36.1%) |
| Off pump | 47 (20.4%) |
| On pump | 183 (79.6%) |
| CPT (mean ± SD) | 151 ± 45.4 |
| CCT (mean ± SD) | 78 ± 22.4 |
| Total operation time (mean ± SD) | 4.3 ± 1.0 |
| Conversion to sternotomy | 0 (0%) |
| IABP | 2 (0.9%) |
| n (%) | |
|---|---|
| Early mortality (postop < 30 days) | 2 (0.86%) |
| Return to OR due to bleeding | 5 (2.19%) |
| Stroke | 3 (1.32%) |
| New onset hemodialysis | 1 (0.44%) |
| New onset atrial fibrillation | 17 (7.45%) |
| Phrenic nerve palsy | 2 (0.88%) |
| Chylothorax | 1 (0.44%) |
| Thoracic infection | 4 (1.75%) |
| Early graft occlusion | 4 (1.75%) |
| Early reoperation (sternotomy) | 0 |
| Drainage (mL) | 434.5 ± 181.9 |
| LOS (d) (mean ± SD) | 5.5 ± 2.2 |
| ICU stay (h) (mean ± SD) | 1.5 ± 1.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Demirsoy, E.; Mavioglu, I.; Dogan, E.; Gulmez, H.; Dindar, I.; Erol, M.K. The Feasibility and Early Results of Multivessel Minimally Invasive Coronary Artery Bypass Grafting for All Comers. J. Clin. Med. 2023, 12, 5663. https://doi.org/10.3390/jcm12175663
Demirsoy E, Mavioglu I, Dogan E, Gulmez H, Dindar I, Erol MK. The Feasibility and Early Results of Multivessel Minimally Invasive Coronary Artery Bypass Grafting for All Comers. Journal of Clinical Medicine. 2023; 12(17):5663. https://doi.org/10.3390/jcm12175663
Chicago/Turabian StyleDemirsoy, Ergun, Ilhan Mavioglu, Emre Dogan, Harun Gulmez, Ismet Dindar, and Mustafa Kemal Erol. 2023. "The Feasibility and Early Results of Multivessel Minimally Invasive Coronary Artery Bypass Grafting for All Comers" Journal of Clinical Medicine 12, no. 17: 5663. https://doi.org/10.3390/jcm12175663
APA StyleDemirsoy, E., Mavioglu, I., Dogan, E., Gulmez, H., Dindar, I., & Erol, M. K. (2023). The Feasibility and Early Results of Multivessel Minimally Invasive Coronary Artery Bypass Grafting for All Comers. Journal of Clinical Medicine, 12(17), 5663. https://doi.org/10.3390/jcm12175663








