Effectiveness and Consequences of Direct Access in Physiotherapy: A Systematic Review
Abstract
:1. Introduction
2. Material and Methods
- Protocol and Registration
- Eligibility criteria
2.1. Literature Search
- Study selection and data collection process
- Data synthesis
2.2. Risk of Bias Assessment
3. Results
3.1. Population
3.2. DAPT Management Accuracy
3.3. Cost-Effectiveness
3.4. Work Related Outcomes
- -
- -
- -
- -
- Labor participation measured on a 3-point scale (1 = did not return to work; 2 = returned to work with adaptations; or 3 = returned to work without adaptations) [39];
- -
3.5. Patient Satisfaction
- -
- -
- -
- Qualitative surveys [34].
- -
- A questionnaire related to the satisfaction in care received [47];
- -
- A modified and adapted questionnaire for assessing the quality of direct remote-access care (telephone) [36];
- -
- The Quality from the Patient’s Perspective Questionnaire (QPP) [33];
- -
- A patient satisfaction questionnaire and a physician satisfaction questionnaire related to how the physiotherapist performed the triage [18];
- -
- -
- A questionnaire on patients’ experience of care [31];
- -
- A questionnaire on patient satisfaction/dissatisfaction with being referred to another professional or additional diagnostic investigations (e.g., X-ray) [27].
- -
- patient dissatisfaction with staff communication;
- -
- patient dissatisfaction with the quality of treatment received;
- -
- patient dissatisfaction with the facilities.
3.6. DAPT Safety
3.7. Health Outcomes
- -
- -
- -
- -
- Perception of disability was evaluated in four studies through the Pain Disability Index (PDI) [17], the Disease Repercussions Profile [42], or the Measure Yourself Medical Outcomes Profile and global improvement [34]. Koojiman et al. [35] analyzed and compared the percentage of patients who achieved the expected outcomes between patients who underwent DAPT and those who went to the physiotherapist following medical referral;
- -
- One study [38] assessed functional disability in ADLs with the Disability Rating Index (DRI) and the patient’s attitudes towards their musculoskeletal disorder through the Attitude Responsibility for Musculoskeletal disorders scale (ARM);
- -
- Oostendorp et al. [39] evaluated the patient’s coping through the Pain Coping Inventory (PCI) and general health with the Global Perceived Effect (GPE);
- -
- -
- -
- -
- -
- -
- -
- One study [46] used the Patient-Specific Functional-Scale (PSFS) for physical function and the Patient Acceptability Symptom State (PASS) to measure acceptability of symptoms.
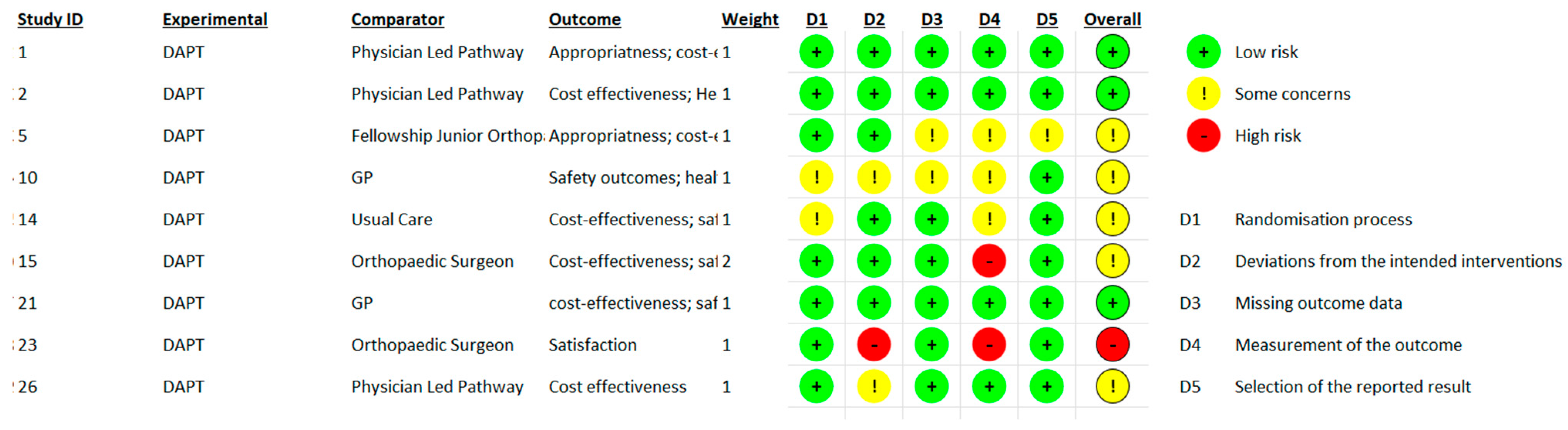
3.8. Risk of Bias Assessment
4. Discussion
5. Limitations
Implications for Practice
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Academies of Sciences, Engineering, and Medicine. Musculoskeletal Disorders. In Selected Health Conditions and Likelihood of Improvement with Treatment; The National Academic Press: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Briggs, A.M.; Woolf, A.D.; Dreinhöfer, K.; Homb, N.; Hoy, D.G.; Kopansky-Giles, D.; Åkesson, K.; March, L. Reducing the Global Burden of Musculoskeletal Conditions. Bull. World Health Organ. 2018, 96, 366–368. [Google Scholar] [CrossRef]
- The Burden of Musculoskeletal Diseases in the United States|Prevalence, Societal and Economic Cost. Available online: https://www.boneandjointburden.org/ (accessed on 12 December 2022).
- APTA APTA Direct Access Advocacy. Available online: https://www.apta.org/advocacy/issues/direct-access-advocacy (accessed on 19 March 2022).
- Hon, S.; Ritter, R.; Allen, D.D. Cost-Effectiveness and Outcomes of Direct Access to Physical Therapy for Musculoskeletal Disorders Compared to Physician-First Access in the United States: Systematic Review and Meta-Analysis. Phys. Ther. 2021, 101, pzaa201. [Google Scholar] [CrossRef] [PubMed]
- Demont, A.; Bourmaud, A.; Kechichian, A.; Desmeules, F. The impact of direct access physiotherapy compared to primary care physician led usual care for patients with musculoskeletal disorders: A systematic review of the literature. Disabil. Rehabil. 2021, 43, 1637–1648. [Google Scholar] [CrossRef] [PubMed]
- Ojha, H.A.; Snyder, R.S.; Davenport, T.E. Direct access compared with referred physical therapy episodes of care: A systematic review. Phys. Ther. 2014, 94, 14–30. [Google Scholar] [CrossRef] [PubMed]
- Samsson, K.S.; Grimmer, K.; Larsson, M.E.H.; Morris, J.; Bernhardsson, S. Effects on health and process outcomes of physiotherapist-led orthopaedic triage for patients with musculoskeletal disorders: A systematic review of comparative studies. BMC Musculoskelet. Disord. 2020, 21, 673. [Google Scholar] [CrossRef]
- Bornhöft, L.; Thorn, J.; Svensson, M.; Nordeman, L.; Eggertsen, R.; Larsson, M.E.H. More cost-effective management of patients with musculoskeletal disorders in primary care after direct triaging to physiotherapists for initial assessment compared to initial general practitioner assessment. BMC Musculoskelet. Disord. 2019, 20, 186. [Google Scholar] [CrossRef]
- Gazzetta Ufficiale Law n 25/2018. Available online: https://www.gazzettaufficiale.it/eli/id/2018/1/31/18G00019/sg (accessed on 26 September 2022).
- Gazzetta Ufficiale Law n 64/2017. Available online: https://www.gazzettaufficiale.it/eli/id/2017/03/17/17G00041/sg (accessed on 18 September 2022).
- Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; Abegaz, K.H.; Abolhassani, H.; Aboyans, V.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Advocacy|World Physiotherapy. Available online: https://world.physio/what-we-do/advocacy (accessed on 18 September 2022).
- Maselli, F.; Piano, L.; Cecchetto, S.; Storari, L.; Rossettini, G.; Mourad, F. Direct Access to Physical Therapy: Should Italy Move Forward? Int. J. Environ. Res. Public Health 2022, 19, 555. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef]
- Sephton, R.; Hough, E.; Roberts, S.A.; Oldham, J. Evaluation of a primary care musculoskeletal clinical assessment service: A preliminary study. Physiotherapy 2010, 96, 296–302. [Google Scholar] [CrossRef]
- Samsson, K.S.; Larsson, M.E. Physiotherapy triage assessment of patients referred for orthopaedic consultation—Long-term follow-up of health-related quality of life, pain-related disability and sick leave. Man. Ther. 2015, 20, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Oldmeadow, L.B.; Bedi, H.S.; Burch, H.T.; Smith, J.S.; Leahy, E.S.; Goldwasser, M. Experienced physiotherapists as gatekeepers to hospital orthopaedic outpatient care. Med. J. Aust. 2007, 186, 625–628. [Google Scholar] [CrossRef] [PubMed]
- Lyons, R.F.; Cassells, M.; Hynes, D.; Mullett, H.; Groarke, P.J. A physiotherapy triage service for orthopaedic upper limb service: An effective way to reduce clinic visits and identify patients for operative intervention. Ir. J. Med. Sci. 2022, 191, 771–775. [Google Scholar] [CrossRef]
- McGowan, J.; Sampson, M.; Salzwedel, D.M.; Cogo, E.; Foerster, V.; Lefebvre, C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J. Clin. Epidemiol. 2016, 75, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.D.; Quatman, C.E.; Manring, M.M.; Siston, R.A.; Flanigan, D.C. How to Write a Systematic Review. Am. J. Sports Med. 2014, 42, 2761–2768. [Google Scholar] [CrossRef]
- Harris, J.D.; Brophy, R.H.; Siston, R.A.; Flanigan, D.C. Treatment of Chondral Defects in the Athlete’s Knee. Arthrosc. J. Arthrosc. Relat. Surg. 2010, 26, 841–852. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: https://pdfs.semanticscholar.org/5b63/3ae0fca9ba9ddb97b4c35b8c3b264fd5104a.pdf (accessed on 1 August 2022).
- Piscitelli, D.; Furmanek, M.; Meroni, R.; De Caro, W.; Pellicciari, L. Direct access in physical therapy: A systematic review. La Clin. Ter. 2018, 169, e249–e260. [Google Scholar] [PubMed]
- Caffrey, A.; Smart, K.M.; FitzGerald, O. Physiotherapist-Led Triage at a Rheumatology-Based Musculoskeletal Assessment Clinic: An 18-Month Service Evaluation of Activity and Outcomes. ACR Open Rheumatol. 2019, 1, 213–218. [Google Scholar] [CrossRef]
- Peterson, G.; Portström, M.; Frick, J. Extended roles in primary care when physiotherapist-initiated referral to X-ray can save time and reduce costs. Int. J. Qual. Heal. Care 2021, 33, mzab122. [Google Scholar] [CrossRef]
- Bird, S.; Thompson, C.; Williams, K.E. Primary contact physiotherapy services reduce waiting and treatment times for patients presenting with musculoskeletal conditions in Australian emergency departments: An observational study. J. Physiother. 2016, 62, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.T.; Gavaghan, B.; O’Leary, S.; McBride, L.-J.; Raymer, M. Do patients discharged from advanced practice physiotherapy-led clinics re-present to specialist medical services? Aust. Health Rev. 2018, 42, 334–339. [Google Scholar] [CrossRef] [PubMed]
- Samsson, K.S.; Bernhardsson, S.; Larsson, M.E.H. Perceived quality of physiotherapist-led orthopaedic triage compared with standard practice in primary care: A randomised controlled trial. BMC Musculoskelet. Disord. 2016, 17, 257. [Google Scholar] [CrossRef]
- Downie, F.; McRitchie, C.; Monteith, W.; Turner, H. Physiotherapist as an Alternative to a GP for Musculoskeletal Conditions. Br. J. Gen. Pract. 2019, 69, e314–e320. [Google Scholar] [CrossRef] [PubMed]
- Bishop, A.; Ogollah, R.O.; Jowett, S.; Kigozi, J.; Tooth, S.; Protheroe, J.; Hay, E.M.; Salisbury, C.; Foster, N.E. STEMS pilot trial: A pilot cluster randomised controlled trial to investigate the addition of patient direct access to physiotherapy to usual GP-led primary care for adults with musculoskeletal pain. BMJ Open 2017, 7, e012987. [Google Scholar] [CrossRef]
- Samsson, K.; Larsson, M.E. Physiotherapy screening of patients referred for orthopaedic consultation in primary healthcare—A randomised controlled trial. Man. Ther. 2014, 19, 386–391. [Google Scholar] [CrossRef]
- Salisbury, C.; Foster, N.; Hopper, C.; Bishop, A.; Hollinghurst, S.; Coast, J.; Kaur, S.; Pearson, J.; Franchini, A.; Hall, J.; et al. A pragmatic randomised controlled trial of the effectiveness and cost-effectiveness of ‘PhysioDirect’ telephone assessment and advice services for physiotherapy. Health Technol. Assess. 2013, 17, 1–157. [Google Scholar] [CrossRef]
- Kooijman, M.; Swinkels, I.; van Dijk, C.; de Bakker, D.; Veenhof, C. Patients with shoulder syndromes in general and physiotherapy practice: An observational study. BMC Musculoskelet. Disord. 2013, 14, 128. [Google Scholar] [CrossRef]
- Mallett, R.; Bakker, E.; Burton, M. Is Physiotherapy Self-Referral with Telephone Triage Viable, Cost-effective and Beneficial to Musculoskeletal Outpatients in a Primary Care Setting? Musculoskelet. Care 2014, 12, 251–260. [Google Scholar] [CrossRef]
- Bornhöft, L.; Larsson, M.E.H.; Thorn, J. Physiotherapy in Primary Care Triage—The effects on utilization of medical services at primary health care clinics by patients and sub-groups of patients with musculoskeletal disorders: A case-control study. Physiother. Theory Pract. 2015, 31, 45–52. [Google Scholar] [CrossRef]
- Bornhöft, L.; Larsson, M.E.; Nordeman, L.; Eggertsen, R.; Thorn, J. Health effects of direct triaging to physiotherapists in primary care for patients with musculoskeletal disorders: A pragmatic randomized controlled trial. Ther. Adv. Musculoskelet. Dis. 2019, 11, 1759720X19827504. [Google Scholar] [CrossRef] [PubMed]
- AB Oostendorp, R.; Elvers, J.H.; van Trijffel, E.; Rutten, G.M.; Scholten-Peeters, G.G.; Heijmans, M.; Hendriks, E.; Mikolajewska, E.; De Kooning, M.; Laekeman, M.; et al. Clinical Characteristics and Patient-Reported Outcomes of Primary Care Physiotherapy in Patients with Whiplash-Associated Disorders: A Longitudinal Observational Study. Patient Prefer. Adherence 2020, 14, 1733–1750. [Google Scholar] [CrossRef] [PubMed]
- O’farrell, S.; Smart, K.M.; Caffrey, A.; Daly, O.; Doody, C. Orthopaedic triage at a physiotherapist-led ‘Musculoskeletal Assessment Clinic’: A seven-month service evaluation of outcomes. Ir. J. Med Sci. 2014, 183, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Kerridge-Weeks, M.; Langridge, N.J. Orthopaedic Spinal Triage: An Evaluation of Decision Making and Outcome in a Physiotherapy Led Service. Int. J. Health Gov. 2016, 21, 5–17. [Google Scholar] [CrossRef]
- Daker-White, G.; Carr, A.J.; Harvey, I.; Woolhead, G.; Bannister, G.; Nelson, I.; Kammerling, M. A randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. J. Epidemiol. Community Health 1999, 53, 643–650. [Google Scholar] [CrossRef]
- Phillips, C.J.; Phillips, R.; Main, C.J.; Watson, P.J.; Davies, S.; Farr, A.; Harper, C.; Noble, G.; Aylward, M.; Packman, J.; et al. The cost effectiveness of NHS physiotherapy support for occupational health (OH) services. BMC Musculoskelet. Disord. 2012, 13, 29. [Google Scholar] [CrossRef]
- Lankhorst, N.; Barten, J.; Meerhof, R.; Bierma-Zeinstra, S.; van Middelkoop, M. Characteristics of patients with knee and ankle symptoms accessing physiotherapy: Self-referral vs general practitioner’s referral. Physiotherapy 2020, 108, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Ho-Henriksson, C.-M.; Svensson, M.; Thorstensson, C.A.; Nordeman, L. Physiotherapist or physician as primary assessor for patients with suspected knee osteoarthritis in primary care—A cost-effectiveness analysis of a pragmatic trial. BMC Musculoskelet. Disord. 2022, 23, 260. [Google Scholar] [CrossRef]
- Ojha, H.A.; Fritz, J.M.; Malitsky, A.L.; Wu, J.; Weiner, M.G.; Brandi, J.A.; Rhon, D.I.; Mobo, B.H.P.; Fleming, K.M.; Beidleman, R.R.; et al. Comparison of Physical Therapy and Physician Pathways for Employees with Recent Onset Musculoskeletal Pain: A Randomized Controlled Trial. PM&R 2020, 12, 1071–1080. [Google Scholar] [CrossRef]
- Ludvigsson, M.L.; Enthoven, P. Evaluation of physiotherapists as primary assessors of patients with musculoskeletal disorders seeking primary health care. Physiotherapy 2012, 98, 131–137. [Google Scholar] [CrossRef]
- Szymanek, E.; Jones, M.; Shutt-Hoblet, C.; Halle, R. Implementation of Direct Access Physical Therapy Within the Military Medical System. Mil. Med. 2022, 187, e649–e654. [Google Scholar] [CrossRef] [PubMed]
- Peterson, S. Telerehabilitation booster sessions and remote patient monitoring in the management of chronic low back pain: A case series. Physiother. Theory Pract. 2018, 34, 393–402. [Google Scholar] [CrossRef]
- Kremer, E.; Atkinson, H.J.; Ignelzi, R.J. Measurement of pain: Patient preference does not confound pain measurement. Pain 1981, 10, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Diehl, A.K. Patient Satisfaction with Medical Care for Low-Back Pain. Spine 1986, 11, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Finucane, L.M.; Downie, A.; Mercer, C.; Greenhalgh, S.M.; Boissonnault, W.G.; Pool-Goudzwaard, A.L.; Beneciuk, J.M.; Leech, R.L.; Selfe, J. International Framework for Red Flags for Potential Serious Spinal Pathologies. J. Orthop. Sports Phys. Ther. 2020, 50, 350–372. [Google Scholar] [CrossRef]
- Storari, L.; Signorini, M.; Barbari, V.; Mourad, F.; Bisconti, M.; Salomon, M.; Rossettini, G.; Maselli, F. A Thoracic Outlet Syndrome That Concealed a Glioblastoma. Findings from a Case Report. Medicina 2021, 57, 908. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, R.S.; Cheruvu, M.S.; Ansari, H.; van Liefland, M. Cauda equina compression in metastatic prostate cancer. BMJ Case Rep. 2020, 13, e237779. [Google Scholar] [CrossRef]
- Desmeules, F.; Roy, J.-S.; MacDermid, J.C.; Champagne, F.; Hinse, O.; Woodhouse, L.J. Advanced practice physiotherapy in patients with musculoskeletal disorders: A systematic review. BMC Musculoskelet. Disord. 2012, 13, 107. [Google Scholar] [CrossRef]
- Bech, M. The economics of non-attendance and the expected effect of charging a fine on non-attendees. Health Policy 2005, 74, 181–191. [Google Scholar] [CrossRef]
- Duijn, E.A.H.D.; Roy van, S.; Karel, Y.H.J.M.; Provyn, S.; Pouliart, N. An Interexaminer Agreement and Reliability Study on Cadavers with Musculoskeletal Ultrasound of the Shoulder Performed by Physiotherapists and Radiologists Compared with Dissection. Musculoskelet. Sci. Pract. 2022, 60, 102569. [Google Scholar] [CrossRef]
- Glogovac, G.; Kennedy, M.E.; Weisgerber, M.R.; Kakazu, R.; Grawe, B.M. Wait Times in Musculoskeletal Patients: What Contributes to Patient Satisfaction. J. Patient Exp. 2020, 7, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Grimmer-Somers, K.; Milanese, S.; Kumar, S.; Morris, J. Extended scope physiotherapy roles for orthopedic outpatients: An update systematic review of the literature. J. Multidiscip. Health 2012, 5, 37–45. [Google Scholar] [CrossRef]
- Cook, C.E.; Denninger, T.; Lewis, J.; Diener, I.; Thigpen, C. Providing value-based care as a physiotherapist. Arch. Physiother. 2021, 11, 12. [Google Scholar] [CrossRef] [PubMed]
- Blæhr, E.E.; Væggemose, U.; Søgaard, R. Effectiveness and cost-effectiveness of fining non-attendance at public hospitals: A randomised controlled trial from Danish outpatient clinics. BMJ Open 2018, 8, e019969. [Google Scholar] [CrossRef] [PubMed]
- Triemstra, J.D.; Lowery, L. Prevalence, Predictors, and the Financial Impact of Missed Appointments in an Academic Adolescent Clinic. Cureus 2018, 10, e3613. [Google Scholar] [CrossRef] [PubMed]
- George, A.; Rubin, G. Non-attendance in general practice: A systematic review and its implications for access to primary health care. Fam. Pract. 2003, 20, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Denninger, T.R.; Cook, C.E.; Chapman, C.G.; McHenry, T.; Thigpen, C.A. The Influence of Patient Choice of First Provider on Costs and Outcomes: Analysis from a Physical Therapy Patient Registry. J. Orthop. Sports Phys. Ther. 2018, 48, 63–71. [Google Scholar] [CrossRef]
- Mitchell, J.M.; de Lissovoy, G. A Comparison of Resource Use and Cost in Direct Access Versus Physician Referral Episodes of Physical Therapy. Phys. Ther. 1997, 77, 10–18. [Google Scholar] [CrossRef]
- Ansell, D.; Crispo, J.A.G.; Simard, B.; Bjerre, L.M. Interventions to reduce wait times for primary care appointments: A systematic review. BMC Health Serv. Res. 2017, 17, 295. [Google Scholar] [CrossRef]
- Robinson, J.; Porter, M.; Montalvo, Y.; Peden, C.J. Losing the wait: Improving patient cycle time in primary care. BMJ Open Qual. 2020, 9, e000910. [Google Scholar] [CrossRef]
- Babatunde, O.O.; Bishop, A.; Cottrell, E.; Jordan, J.L.; Corp, N.; Humphries, K.; Hadley-Barrows, T.; Huntley, A.L.; van der Windt, D.A. A systematic review and evidence synthesis of non-medical triage, self-referral and direct access services for patients with musculoskeletal pain. PLoS ONE 2020, 15, e0235364. [Google Scholar] [CrossRef] [PubMed]
- Goff, A.J.; Silva, D.D.O.; Merolli, M.; Bell, E.C.; Crossley, K.M.; Barton, C.J. Patient education improves pain and function in people with knee osteoarthritis with better effects when combined with exercise therapy: A systematic review. J. Physiother. 2021, 67, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Gardner, T.; Refshauge, K.; McAuley, J.; Hübscher, M.; Goodall, S.; Smith, L. Combined education and patient-led goal setting intervention reduced chronic low back pain disability and intensity at 12 months: A randomised controlled trial. Br. J. Sports Med. 2019, 53, 1424–1431. [Google Scholar] [CrossRef]
- Davis, K.; Schoenbaum, S.C.; Audet, A.-M. A 2020 vision of patient-centered primary care. J. Gen. Intern. Med. 2005, 20, 953–957. [Google Scholar] [CrossRef]
- Deslauriers, S.; Déry, J.; Proulx, K.; Laliberté, M.; Desmeules, F.; Feldman, D.E.; Perreault, K. Effects of waiting for outpatient physiotherapy services in persons with musculoskeletal disorders: A systematic review. Disabil. Rehabil. 2021, 43, 611–620. [Google Scholar] [CrossRef]
- Lewis, A.K.; Harding, K.E.; Snowdon, D.A.; Taylor, N.F. Reducing wait time from referral to first visit for community outpatient services may contribute to better health outcomes: A systematic review. BMC Health Serv. Res. 2018, 18, 869. [Google Scholar] [CrossRef] [PubMed]
- Maselli, F.; Piano, L.; Cecchetto, S.; Storari, L.; Rossettini, G.; Mourad, F. Reply to Moretti et al. Would Moving Forward Mean Going Back? Comment on “Maselli et al. Direct Access to Physical Therapy: Should Italy Move Forward? Int. J. Environ. Res. Public Health 2022, 19, 555”. Int. J. Environ. Res. Public Health 2022, 19, 4620. [Google Scholar]


| Inclusion Criteria: | Exclusion Criteria: |
|---|---|
|
|
| No | Searches | Results |
|---|---|---|
| 1 | (“Physical therapy” [All Fields] OR “physiotherapy” [All Fields]) | 144,912 |
| 2 | (“Ambulatory Care” [All Fields] OR “Primary Health Care” [All Fields] OR “outpatient*” [All Fields] OR “primary care” [All Fields] OR “ambulator*” [All Fields] OR “delivery of health care” [All Fields]) | 713,311 |
| 3 | (“Referral and Consultation” [All Fields] OR (“Referral and Consultation” [MeSH Terms] OR (“referral” [All Fields] AND “consultation” [All Fields]) OR “Referral and Consultation” [All Fields] OR “referral” [All Fields] OR “referrals” [All Fields] OR “referrer” [All Fields] OR “referrers” [All Fields]) OR “direct access” [All Fields] OR “dapt” [All Fields]) OR (“triage” [MeSH Terms] OR “triage” [All Fields] OR “triages” [All Fields] OR “triaged” [All Fields] OR “triaging” [All Fields]) OR “direct access physical therapy” [All Fields] OR “self-referral” [All Fields] OR “physical therapy direct access” [All Fields]) | 234,596 |
| 4 | (“musculoskeletal disease*” [All Fields] OR “musculoskeletal disease” [All Fields] OR “musculoskeletal disorder*” [All Fields] OR “orthopedic disorder*” [All Fields]) | 25,095 |
| 5 | (“cost-effectiveness” [All Fields] OR “effectiveness” [All Fields] OR “cost savings” [All Fields] OR (“economics” [MeSH Subheading] OR “economics” [All Fields] OR “cost” [All Fields] OR “costs and cost analysis” [MeSH Terms] OR (“costs” [All Fields] AND “cost” [All Fields] AND “analysis” [All Fields]) OR “costs and cost analysis” [All Fields]) OR “outcome*” [All Fields] OR (“prognosis” [MeSH Terms] OR “prognosis” [All Fields] OR “prognoses” [All Fields])) | 4,901,682 |
| 6 | 1 AND 2 AND 3 AND 4 AND 5 | 70 |
| Age (mean) | 49 Years |
| Sex (%) | 57% F–43% M |
| Type of MSDs (%) | Upper Limb 15% Spine 50% Lower Limb 25% Widespread/Mixed Pain 7% Rheumatological Disease 3% |
| Onset (%) | Acute (<6 weeks) 40% Sub-acute (6 weeks to 3 months) 25% Chronic (>3 months) 35% |
| Type of Specialization | Nr. of Studies |
|---|---|
| Post-graduate specialization/ doctorate or musculoskeletal certification | 2 studies |
| 1 day out for training; direct access to primary care and mentoring | 1 study |
| From 6 to 28 years of experience | 5 studies |
| At least 3 years of experience in primary care + at least 1 orthopedic manipulative physiotherapist specialization | 4 studies |
| Extended or advanced scope practitioner | 11 studies |
| Degree of physiotherapy | 2 studies |
| Specialization not specified | 3 studies |
| Parameter | Range | Mean |
|---|---|---|
| Patients independently screened by physiotherapist | 69–97 | 80.6% |
| Surgical conversion rate | 40–89.3% | 67.4% |
| DAPT Mean (Min–Max) | Medical Model Mean (Min–Max) | Mean Difference | |
|---|---|---|---|
| Imaging | 21% (0–63%) | 49% (27–86%) | 28% |
| Medication | 22.3% (8–50%) | 63.5% (60–73.1%) | 41.2% |
| Referral | 9.3% (2.9–19.3%) | 30% (14–40%) | 20.7% |
| DAPT Mean (Min–Max) | Medical Model Mean (Min–Max) | Mean Difference | |
|---|---|---|---|
| Cost for episode of care | EUR 301.5 (255.55–628.24) | EUR 743.44 (498.38–988.51) | EUR 441.9 |
| DAPT Mean (Min–Max) | Medical Model Mean (Min–Max) | Mean Difference | |
|---|---|---|---|
| Presence to visit | 93.5% (90–97.1%) | 87.5% (86–89%) | 6% |
| DAPT Mean | Medical Model Mean | Mean Difference | |
|---|---|---|---|
| Time to triage in minutes | 108 min | 148 min | 40 min |
| Percentage of patients discharged within 4 h in primary care | 93% | 75% | 18% |
| Number of sessions/days to discharge (Ankle MSDs) | 5.6 sessions/ no difference | 6.7 sessions/ no difference | 1.1 sessions |
| Number of sessions/days to discharge (Knee MSDs) | 6.3 sessions/ 49.7 days | 9.1 sessions/ 60.2 days | 2.8 sessions/ 10.5 days |
| DAPT Mean (Min–Max) | Medical Model Mean (Min–Max) | Mean Difference | |
|---|---|---|---|
| Percentage of sick leave prescriptions | 9% (3–15.1%) | 12.16% (7.3–23.5%) | 5% |
| Number of sick leave days prescribed | 13.5 days (0–27 days) | 50.5 days (26–75 days) | 37 days |
| Authors | Evaluation of DAPT Safety | Results |
|---|---|---|
| Peterson et al., 2021 [27] | Number of adverse events | none |
| Bishop et al., 2017 [32] | Number of adverse events | none |
| Salisbury et al., 2013 [34] | Number of adverse events | none |
| Bornhöft et al., 2019 [38] | Number of adverse events | none |
| Ojha et al., 2020 [46] | Number and type of adverse events | 4 mild adverse events: 2/77 DAPT group 2/73 medical group Two patients in the medical group had an accidental fall at home, and unclear diagnosis of ankle pain at one-year and two patients in the DAPT group had side effects from an emergency room medication, and unclear diagnosis of low back pain. |
| DAPT Mean (Min–Max) | Physician-Led Care Model Mean (Min–Max) | Mean Difference | |
|---|---|---|---|
| Waiting times in days | 12.31 (3.55–26 days) | 35.59 (28–57 days) | 23.28 days |
| Primary care waiting time (min) | n.a. | n.a. | 31 min |
| Reference | Selection of Case and Controls | Comparability of Cases and Controls | Exposure | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| ITEM#1 Is the case definition adequate | ITEM#2 Representativeness of the cases | ITEM#3 Selection of Controls | ITEM#4 Definition of Controls Not Present at Start | ITEM#5 Comparability of cases and controls on the basis of the design or analysis | ITEM#6 Ascertainment of exposure | ITEM#7 Same method of ascertainment for cases and controls | ITEM#8 Non-Response Rate | ||
| Bird et al., 2016 [28] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 8/9 | |
| Bornhöft et al., 2015 [37] | ✸ | ✸ | ✸ | ✸ | 5/9 | ||||
| Kooijman et al., 2013 [35] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 6/9 | ||
| Lankhorst et al., 2017 [44] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 7/9 | |
| Ludvigsson et al., 2012 [47] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 7/9 | |
| Mallet et al., 2014 [36] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 7/9 | |
| Oldmeadow et al., 2007 [18] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 7/9 | |
| Phillips et al., 2012 [43] | ✸ | ✸ | ✸ | ✸ | 4/9 | ||||
| Szymanek et al., 2022 [48] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 8/9 |
| Reference | Selection of Cohorts | Comparability of Cohorts | Outcome | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| ITEM#1 Representativeness of the Exposed Cohort | ITEM#2 Selection of the Non-Exposed | ITEM#3 Ascertainment of Exposure | ITEM#4 Demonstration that outcome of interest was not present at start of study | ITEM#5 Comparability of cohorts on the basis of the design or analysis | ITEM#6 Assessment of Outcome | ITEM#7 Was follow up long enough for outcomes to occur | ITEM#8 Adequacy of Follow Up of Cohorts | ||
| Caffrey et al., 2019 [26] | ✸ | ✸ | ✸ | ✸ | ✸ | 5/9 | |||
| Chang et al., 2018 [29] | ✸ | ✸ | ✸ | ✸ | 4/9 | ||||
| Downie et al., 2019 [31] | ✸ | ✸ | ✸ | ✸ | ✸ | 5/9 | |||
| Kerridge-Weeks et al., 2016 [41] | ✸ | ✸ | ✸ | ✸ | ✸ | ✸ | 6/9 | ||
| Lyons et al., 2022 [19] | ✸ | ✸ | ✸ | ✸ | ✸ | 4/9 | |||
| O’Farrell et al., 2014 [40] | ✸ | ✸ | ✸ | ✸ | ✸ | 5/9 | |||
| Peterson et al., 2021 [27] | ✸ | ✸ | ✸ | ✸ | ✸ | 5/9 | |||
| Szymanek et al., 2022 [48] | ✸ | ✸ | ✸ | ✸ | 4/9 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gallotti, M.; Campagnola, B.; Cocchieri, A.; Mourad, F.; Heick, J.D.; Maselli, F. Effectiveness and Consequences of Direct Access in Physiotherapy: A Systematic Review. J. Clin. Med. 2023, 12, 5832. https://doi.org/10.3390/jcm12185832
Gallotti M, Campagnola B, Cocchieri A, Mourad F, Heick JD, Maselli F. Effectiveness and Consequences of Direct Access in Physiotherapy: A Systematic Review. Journal of Clinical Medicine. 2023; 12(18):5832. https://doi.org/10.3390/jcm12185832
Chicago/Turabian StyleGallotti, Marco, Benedetta Campagnola, Antonello Cocchieri, Firas Mourad, John D. Heick, and Filippo Maselli. 2023. "Effectiveness and Consequences of Direct Access in Physiotherapy: A Systematic Review" Journal of Clinical Medicine 12, no. 18: 5832. https://doi.org/10.3390/jcm12185832
APA StyleGallotti, M., Campagnola, B., Cocchieri, A., Mourad, F., Heick, J. D., & Maselli, F. (2023). Effectiveness and Consequences of Direct Access in Physiotherapy: A Systematic Review. Journal of Clinical Medicine, 12(18), 5832. https://doi.org/10.3390/jcm12185832









