The ongoing improvement of imaging and diagnostic techniques have resulted in an increase in the preoperative diagnosis of body-tail pancreatic cancer involving adjacent or distant organs [
16,
17]. In our experience of 101 distal pancreatectomy for adenocarcinoma of the pancreas, 36% of the patients had an associated resection of other structures involved by cancer. Our result is in alignment with the 25–78% range reported by other series [
5,
18,
19], confirming the high tendency to perform more extended and eventually more challenging surgical procedures to achieve R0 resection for cancer located in the distal pancreas [
20]. When performing more extended operation for this well-known aggressive cancer, some questions may arise: (1) does the associated resection of other organs or structures increase the risk of operation in terms of mortality and morbidity? (2) Does extended resection modify the rate and type of recurrence when compared to the standard distal pancreatectomy with splenectomy? (3) Is the overall survival impacted by the removal of other organs or vascular structures? The rate of complications (35%) and pancreatic fistula (12%), in our experience, were in line with those previously reported in the literature, and did not show a significant difference in the extended and standard resection groups; two patients died in the postoperative period with a mortality rate of 2.1%. Although the mortality rate after pancreatic resection has decreased considerably in high-volume centers [
1], morbidity remains high, as well as after distal pancreatectomy [
2,
10,
11]. The analysis of the literature shows contrasting results. While several single-institution studies showed no increase in mortality with extended resection [
19,
21,
22,
23], a recent study reported higher 60-day mortality for patients undergoing extended DP compared to those undergoing a standard DP (4.8% vs. 0.8%), [
24]. A study by Siripong et al. [
25] looking at morbidity in standard DP versus extended DP reported that the rates of surgical complications were almost 20% greater in extended than standard DP alone. Another study by Burdelski et al. [
23] reports a 32% increase in the rate of major complications in extended pancreatectomies versus standard resections. In terms of relative risk, the above-mentioned authors [
23] report an almost 6-fold increase in the risk of complications with concurrent colectomy in their univariate analysis, but not in their multivariable analysis. Beetz et al. [
26] showed that clinically-relevant pancreatic fistula was more frequent after extended distal pancreatectomy, but without statistical significance. Hartwig et al. [
8] found that extended DP was associated with a significant increase in overall and surgical morbidity but not mortality. In a recent report by Tangtawee et al. [
27], univariate and multivariate analysis showed that extended resection was not a risk factor for pancreatic fistula or major complications. Thus, it is obvious that morbidity after extended DP may be increased by specific complications related to organ resection, but there are many reports confirming no increase in mortality. Morbidity may potentially affect patients’ survival because patients with major post-operative complications do not receive the recommended adjuvant cancer treatment [
28]. Recurrence after curative distal pancreatectomy for pancreatic cancer has rarely been reported separately [
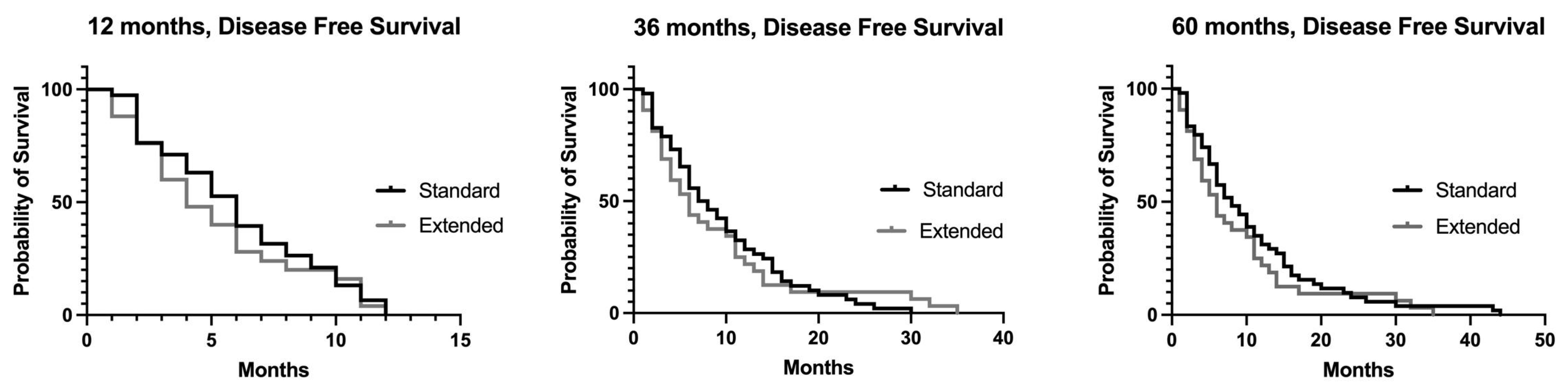
29,
30]. In our experience, 95% of the patients who underwent resection for distal pancreatic adenocarcinoma presented tumor recurrence, with a median disease-free survival of 8 months. The tumor stage and margin of resection were independent predictors of disease-free survival. In alignment with other reports, our study did not show any significant difference in the recurrence rates between the extended and standard resection groups. Roch et al. reported a 17.4% rate for local recurrence after extended DP versus 11.4% after standard DP (
p = 0.48); splenic vein thrombosis and invasion were not significantly associated with higher rates of recurrence as local or distant metastases [
31].
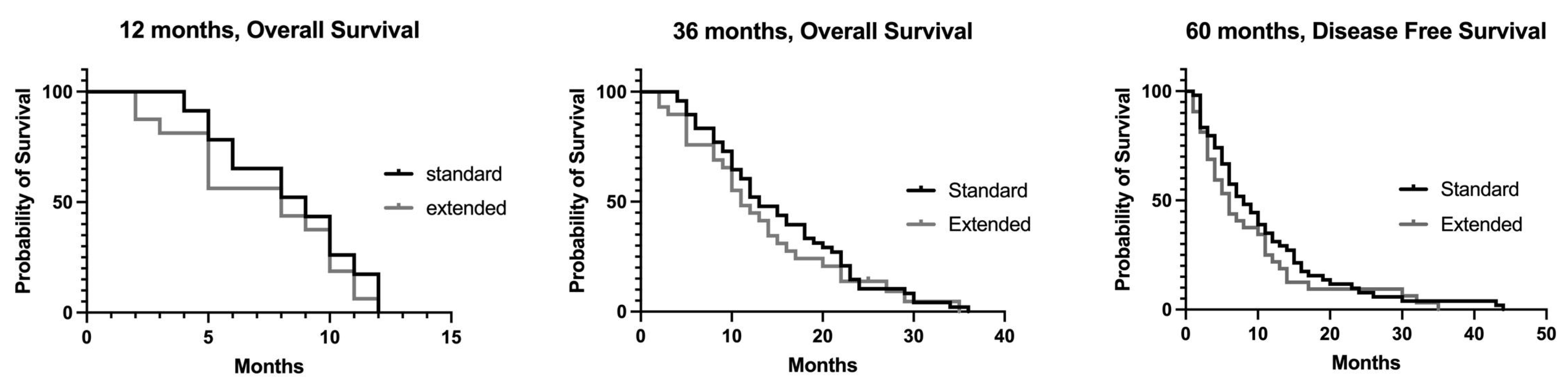
During the follow-up period, we re-operated on nine patients for recurrent pancreatic cancer, and radical resection was performed on five patients: the median survival after re-operation was 18 months (range: 5–156 months); one patient is still alive 54 months after re-resection. Although the number of patients is low, this result emphasizes the need for the accurate and long-term follow-up of patients who undergo resection for pancreatic cancer and the possible role of surgery in the multimodality management of patients with recurrent cancer. In terms of survival, our study showed that the median survival in patients with extended resection was comparable to the survival after standard resection. However, regarding patients who underwent vascular resection, the overall survival rate was lower. These data are similar to those reported by Beetz et al. [
26], who reported lower survival in patients treated with associate vascular resection. Malinka et al. observed a median survival of 29 months in patients with adenocarcinoma who underwent extended DP, which was similar to the survival after standard DP (34 months) [
21]. In the work by Hartwig et al., the median survival of 19.8 months after extended DP was comparable to the survival after standard resection [
32]. Further support of our results comes from the work of Burdelski et al., which reported a significant survival benefit with extended DP in comparison to palliative surgery (16 vs. 6 months;
p < 0.005) [
23]. In a recent systematic review of the literature, Chandrashekhar et al. [
33] analyzed 15 studies focused on extended distal pancreatectomy for pancreatic adenocarcinoma; all but one were retrospective studies. Extended DP was associated with major complications, re-operations and mortality. However, 3- and 5-year survival after extended DP was similar to standard DP. Two recently published articles focused on arterial resection (celiac axis) combined with distal pancreatectomy (DP-CAR). Loos et al. [
34] study, from a specialized high-volume German center, focused on 71 consecutive patients, 61% of which received neoadjuvant chemotherapy prior to surgery and 31 patients underwent concomitant venous resection. In total, 32% of the patients developed major complications and 30% of the patients required re-operation, with 30- and 90-day mortalities of 3% and 8%, respectively. The median survival was 28 months, with an encouraging 5-year survival rate of 19.4%. Yoon et al. [
35] reported a Korean multicenter study of 75 patients treated with DP-CAR: 56% of the patients underwent neoadjuvant therapy. Twenty (26.7%) patients experienced major complications, with a 4% 90-day mortality. The median disease-free survival was 7 months and the median overall survival was 19 months with a 5-year actuarial OS rate of 24.4% (7 patients surviving at 5-year with an actual survival of 9.3%). The extent of lymphadenectomy during distal pancreatectomy for left-sided pancreatic cancer has been evaluated by Sakamoto et al. [
36] in a propensity-score matched multicenter study in Japan. Among 145 patients, 55 patients underwent D1 DP (dissection of 10, 11 and 18 node stations) and 90 underwent D2 DP (dissection of 7, 8, 9, 10, 11, 14 and 18 stations). The long-term survival and the recurrence rate were not significantly different between the two groups, confirming that extended lymphadenectomy does not improve the outcome of patients with left-sided pancreatic cancer.
The main limitations of our study are the retrospective nature of the study and the relatively small sample of patients included. Moreover, the study covers a long period of time, during which adjuvant therapy has been inevitably changed, with new drug combination. A further limitation is the low number of patients who underwent neoadjuvant therapy: therefore, it is reasonable to investigate the role of preoperative therapy in a prospective setting.