Difficult Respiratory Weaning after Cardiac Surgery: A Narrative Review
Abstract
:1. Incidence, Definition, and Risk Factors
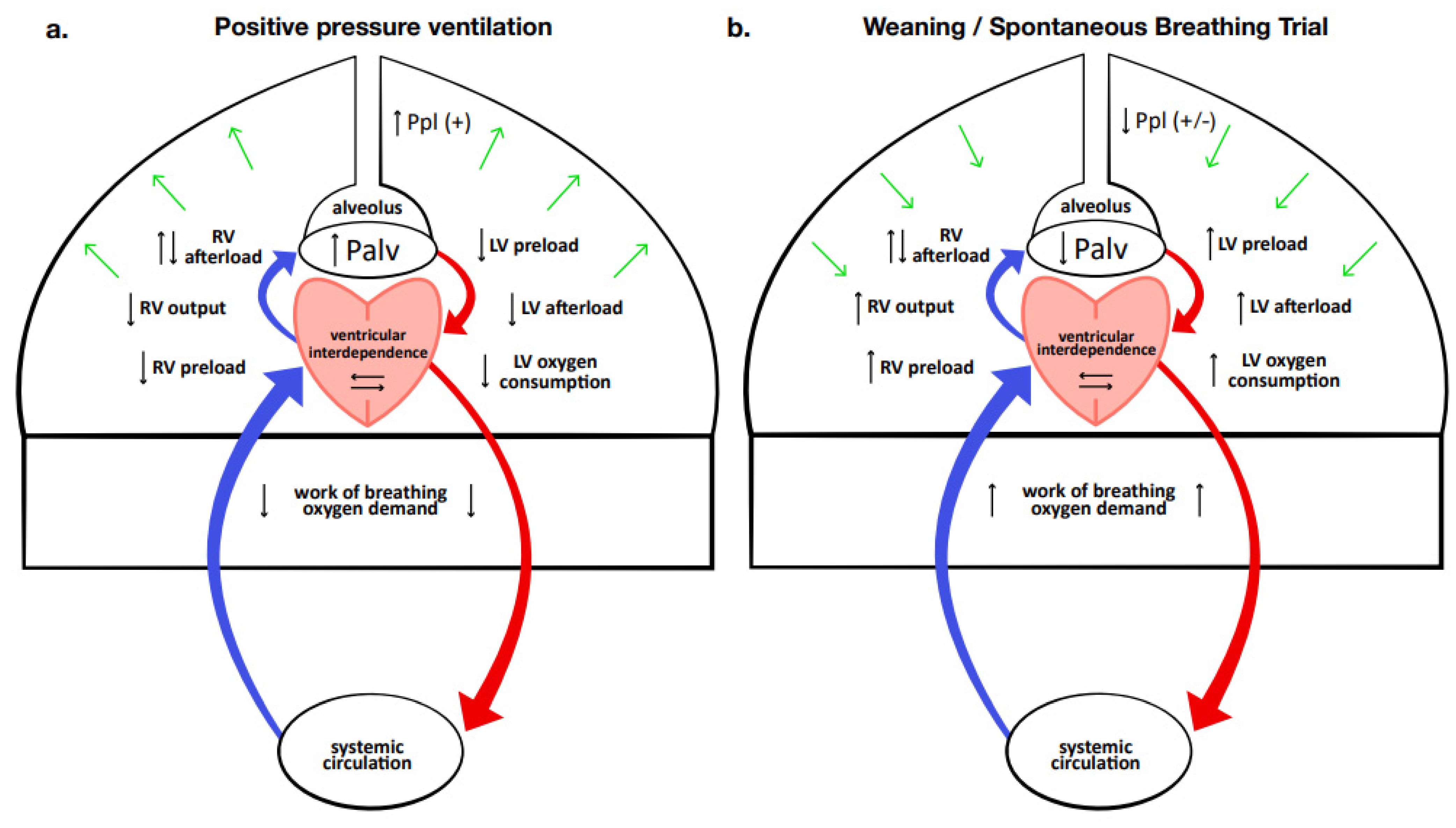
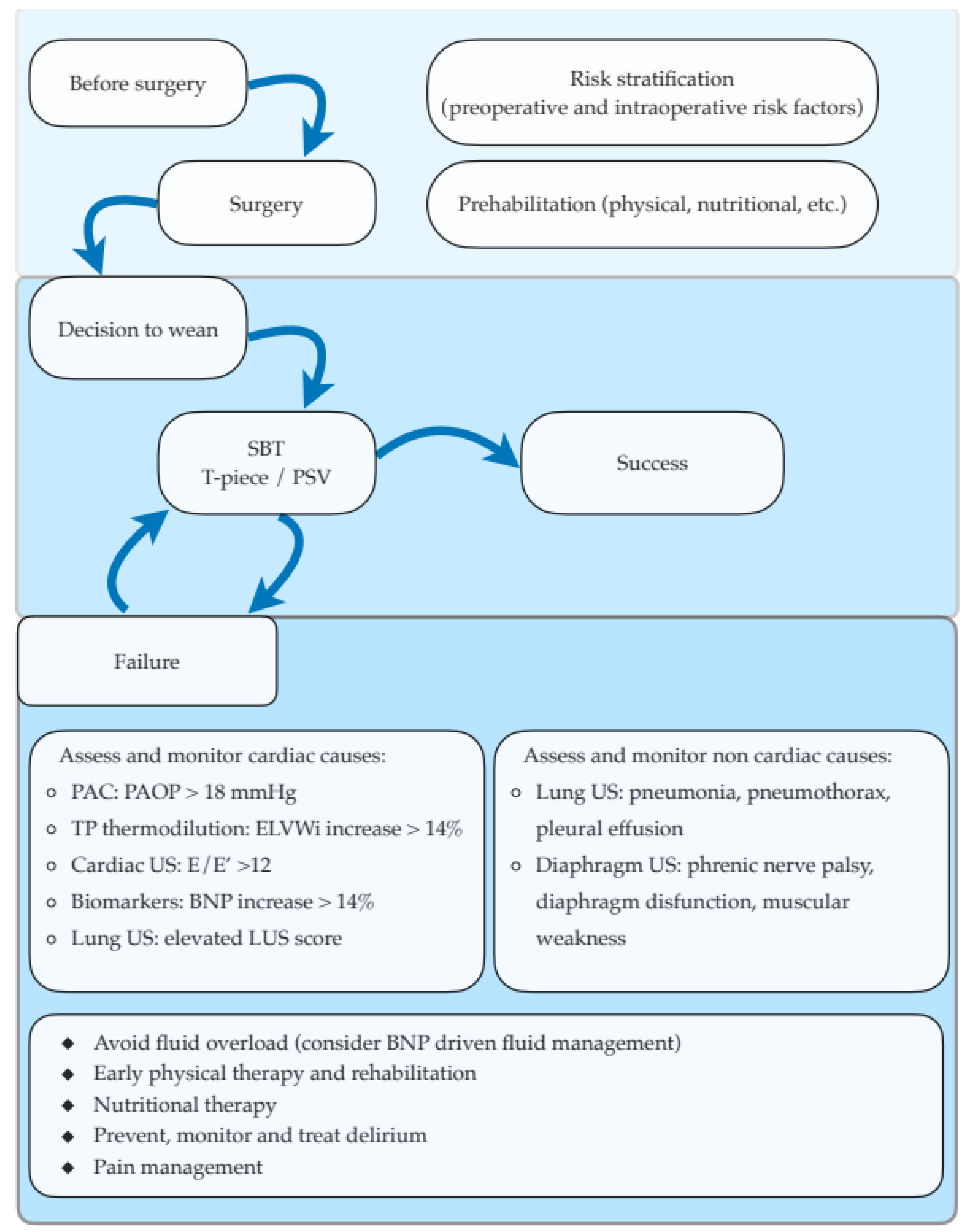
2. Hemodynamic Effects of Weaning
3. Monitoring the Weaning and Assessing Causes of SBT Failure
3.1. Pulmonary Artery Occlusion Pressure
3.2. Ultrasonography
3.2.1. Cardiac Ultrasonography
3.2.2. Lung and Diaphragm Ultrasound
3.3. Cardiac Biomarkers
3.4. Transpulmonary thermodilution and Extravascular Lung Water
4. Ventilatory Strategy
5. Nutrition
6. Prolonged Ventilation and Tracheostomy
6.1. Selection of Patients and Timing of Tracheostomy
6.2. Tracheostomy Technique
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Trouillet, J.-L.; Combes, A.; Vaissier, E.; Luyt, C.-E.; Ouattara, A.; Pavie, A.; Chastre, J. Prolonged Mechanical Ventilation after Cardiac Surgery: Outcome and Predictors. J. Thorac. Cardiovasc. Surg. 2009, 138, 948–953. [Google Scholar] [CrossRef] [Green Version]
- Vagheggini, G.; Vlad, E.P.; Mazzoleni, S.; Bortolotti, U.; Guarracino, F.; Ambrosino, N. Outcomes for Difficult-to-Wean Subjects After Cardiac Surgery. Respir. Care 2015, 60, 56–62. [Google Scholar] [CrossRef] [Green Version]
- Thille, A.W.; Cortés-Puch, I.; Esteban, A. Weaning from the Ventilator and Extubation in ICU. Curr. Opin. Crit. Care 2013, 19, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Saleh, H.Z.; Shaw, M.; Al-Rawi, O.; Yates, J.; Pullan, D.M.; Chalmers, J.A.C.; Fabri, B.M. Outcomes and Predictors of Prolonged Ventilation in Patients Undergoing Elective Coronary Surgery. Interact. Cardiovasc. Thorac. Surg. 2012, 15, 51–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pappalardo, F.; Franco, A.; Landoni, G.; Cardano, P.; Zangrillo, A.; Alfieri, O. Long-Term Outcome and Quality of Life of Patients Requiring Prolonged Mechanical Ventilation after Cardiac Surgery. Eur. J. Cardiothorac. Surg. 2004, 25, 548–552. [Google Scholar] [CrossRef]
- Rajakaruna, C.; Rogers, C.A.; Angelini, G.D.; Ascione, R. Risk Factors for and Economic Implications of Prolonged Ventilation after Cardiac Surgery. J. Thorac. Cardiovasc. Surg. 2005, 130, 1270–1277. [Google Scholar] [CrossRef] [Green Version]
- Boles, J.-M.; Bion, J.; Connors, A.; Herridge, M.; Marsh, B.; Melot, C.; Pearl, R.; Silverman, H.; Stanchina, M.; Vieillard-Baron, A.; et al. Weaning from Mechanical Ventilation. Eur. Respir. J. 2007, 29, 1033–1056. [Google Scholar] [CrossRef] [Green Version]
- Thille, A.W.; Gacouin, A.; Coudroy, R.; Ehrmann, S.; Quenot, J.-P.; Nay, M.-A.; Guitton, C.; Contou, D.; Labro, G.; Reignier, J.; et al. Spontaneous-Breathing Trials with Pressure-Support Ventilation or a T-Piece. N. Engl. J. Med. 2022, 387, 1843–1854. [Google Scholar] [CrossRef]
- Vignon, P. Cardiovascular Failure and Weaning. Ann. Transl. Med. 2018, 6, 354. [Google Scholar] [CrossRef] [PubMed]
- Dres, M.; Teboul, J.-L.; Monnet, X. Weaning the Cardiac Patient from Mechanical Ventilation. Curr. Opin. Crit. Care 2014, 20, 493–498. [Google Scholar] [CrossRef]
- Routsi, C.; Stanopoulos, I.; Kokkoris, S.; Sideris, A.; Zakynthinos, S. Weaning Failure of Cardiovascular Origin: How to Suspect, Detect and Treat—A Review of the Literature. Ann. Intensive Care 2019, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Totonchi, Z.; Baazm, F.; Chitsazan, M.; Seifi, S.; Chitsazan, M. Predictors of Prolonged Mechanical Ventilation after Open Heart Surgery. J. Cardiovasc. Thorac. Res. 2014, 6, 211–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murthy, S.C.; Arroliga, A.C.; Walts, P.A.; Feng, J.; Yared, J.-P.; Lytle, B.W.; Blackstone, E.H. Ventilatory Dependency after Cardiovascular Surgery. J. Thorac. Cardiovasc. Surg. 2007, 134, 484–490.e6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nozawa, E.; Azeka, E.; Feltrim, Z.; Auler Júnior, J.O.C. Factors Associated With Failure of Weaning From Long-Term Mechanical Ventilation After Cardiac Surgery. Int. Heart. J. 2005, 46, 819–831. [Google Scholar] [CrossRef] [Green Version]
- Cislaghi, F.; Condemi, A.M.; Corona, A. Predictors of Prolonged Mechanical Ventilation in a Cohort of 3,269 CABG Patients. Minerva Anestesiol. 2007, 73, 615–621. [Google Scholar] [PubMed]
- Reddy, S.L.C.; Grayson, A.D.; Griffiths, E.M.; Pullan, D.M.; Rashid, A. Logistic Risk Model for Prolonged Ventilation After Adult Cardiac Surgery. Ann. Thorac. Surg. 2007, 84, 528–536. [Google Scholar] [CrossRef]
- Haaksma, M.E.; Tuinman, P.R.; Heunks, L. Weaning the Patient: Between Protocols and Physiology. Curr. Opin. Crit. Care 2021, 27, 29–36. [Google Scholar] [CrossRef]
- Sanfilippo, F.; Di Falco, D.; Noto, A.; Santonocito, C.; Morelli, A.; Bignami, E.; Scolletta, S.; Vieillard-Baron, A.; Astuto, M. Association of Weaning Failure from Mechanical Ventilation with Transthoracic Echocardiography Parameters: A Systematic Review and Meta-Analysis. Br. J. Anaesth. 2021, 126, 319–330. [Google Scholar] [CrossRef]
- Wang, D.; Wang, S.; Song, Y.; Wang, H.; Zhang, A.; Wu, L.; Huang, X.; Ye, P.; Du, X. Predictors and Outcomes of Postoperative Tracheostomy in Patients Undergoing Acute Type A Aortic Dissection Surgery. BMC Cardiovasc. Disord. 2022, 22, 94. [Google Scholar] [CrossRef]
- Frazier, S.K. Cardiovascular Effects of Mechanical Ventilation and Weaning. Nurs. Clin. N. Am. 2008, 43, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Gerbaud, E.; Erickson, M.; Grenouillet-Delacre, M.; Beauvieux, M.-C.; Coste, P.; Durrieu-Jaïs, C.; Hilbert, G.; Castaing, Y.; Vargas, F. Echocardiographic Evaluation and N-Terminal pro-Brain Natriuretic Peptide Measurement of Patients Hospitalized for Heart Failure during Weaning from Mechanical Ventilation. Minerva Anestesiol. 2012, 78, 415–425. [Google Scholar] [PubMed]
- Liu, J.; Shen, F.; Teboul, J.-L.; Anguel, N.; Beurton, A.; Bezaz, N.; Richard, C.; Monnet, X. Cardiac Dysfunction Induced by Weaning from Mechanical Ventilation: Incidence, Risk Factors, and Effects of Fluid Removal. Crit. Care 2016, 20, 369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moschietto, S.; Doyen, D.; Grech, L.; Dellamonica, J.; Hyvernat, H.; Bernardin, G. Transthoracic Echocardiography with Doppler Tissue Imaging Predicts Weaning Failure from Mechanical Ventilation: Evolution of the Left Ventricle Relaxation Rate during a Spontaneous Breathing Trial Is the Key Factor in Weaning Outcome. Crit. Care 2012, 16, R81. [Google Scholar] [CrossRef] [Green Version]
- Dessap, A.M.; Roche-Campo, F.; Kouatchet, A.; Tomicic, V.; Beduneau, G.; Sonneville, R.; Cabello, B.; Jaber, S.; Azoulay, E.; Castanares-Zapatero, D.; et al. Natriuretic Peptide–Driven Fluid Management during Ventilator Weaning: A Randomized Controlled Trial. Am. J. Respir. Crit. Care Med. 2012, 186, 1256–1263. [Google Scholar] [CrossRef] [Green Version]
- Dres, M.; Teboul, J.-L.; Anguel, N.; Guerin, L.; Richard, C.; Monnet, X. Extravascular Lung Water, B-Type Natriuretic Peptide, and Blood Volume Contraction Enable Diagnosis of Weaning-Induced Pulmonary Edema. Crit. Care Med. 2014, 42, 1882–1889. [Google Scholar] [CrossRef] [PubMed]
- Cabello, B.; Thille, A.W.; Roche-Campo, F.; Brochard, L.; Gómez, F.J.; Mancebo, J. Physiological Comparison of Three Spontaneous Breathing Trials in Difficult-to-Wean Patients. Intensive Care Med. 2010, 36, 1171–1179. [Google Scholar] [CrossRef] [PubMed]
- Lamia, B.; Maizel, J.; Ochagavia, A.; Chemla, D.; Osman, D.; Richard, C.; Teboul, J.-L. Echocardiographic Diagnosis of Pulmonary Artery Occlusion Pressure Elevation during Weaning from Mechanical Ventilation. Crit. Care Med. 2009, 37, 1696–1701. [Google Scholar] [CrossRef]
- Nassar, Y.; Abdelbary, A. Risk of Weaning Failure with PAOP ≥15 versus PAOP ≥18. Crit. Care 2013, 17, P148, cc12086. [Google Scholar] [CrossRef] [Green Version]
- Mauri, T.; Yoshida, T.; Bellani, G.; Goligher, E.C.; Carteaux, G.; Rittayamai, N.; Mojoli, F.; Chiumello, D.; Piquilloud, L.; Grasso, S.; et al. Esophageal and Transpulmonary Pressure in the Clinical Setting: Meaning, Usefulness and Perspectives. Intensive Care Med. 2016, 42, 1360–1373. [Google Scholar] [CrossRef]
- Matsushita, K.; Minamishima, T.; Goda, A.; Ishiguro, H.; Kosho, H.; Sakata, K.; Satoh, T.; Yoshino, H. Comparison of the Reliability of E/E′ to Estimate Pulmonary Capillary Wedge Pressure in Heart Failure Patients with Preserved Ejection Fraction versus Those with Reduced Ejection Fraction. Int. J. Cardiovasc. Imaging 2015, 31, 1497–1502. [Google Scholar] [CrossRef] [PubMed]
- Vignon, P.; AitHssain, A.; François, B.; Preux, P.-M.; Pichon, N.; Clavel, M.; Frat, J.-P.; Gastinne, H. Echocardiographic Assessment of Pulmonary Artery Occlusion Pressure in Ventilated Patients: A Transoesophageal Study. Crit. Care 2008, 12, R18. [Google Scholar] [CrossRef] [Green Version]
- Mayo, P.; Volpicelli, G.; Lerolle, N.; Schreiber, A.; Doelken, P.; Vieillard-Baron, A. Ultrasonography Evaluation during the Weaning Process: The Heart, the Diaphragm, the Pleura and the Lung. Intensive Care Med. 2016, 42, 1107–1117. [Google Scholar] [CrossRef]
- Fayssoil, A.; Mansencal, N.; Nguyen, L.S.; Orlikowski, D.; Prigent, H.; Bergounioux, J.; Annane, D.; Lofaso, F. Diaphragm Ultrasound in Cardiac Surgery: State of the Art. Medicines 2022, 9, 5. [Google Scholar] [CrossRef]
- Ji, L.; Cao, C.; Gao, Y.; Zhang, W.; Xie, Y.; Duan, Y.; Kong, S.; You, M.; Ma, R.; Jiang, L.; et al. Prognostic Value of Bedside Lung Ultrasound Score in Patients with COVID-19. Crit. Care 2020, 24, 700. [Google Scholar] [CrossRef] [PubMed]
- Ferré, A.; Guillot, M.; Lichtenstein, D.; Mezière, G.; Richard, C.; Teboul, J.-L.; Monnet, X. Lung Ultrasound Allows the Diagnosis of Weaning-Induced Pulmonary Oedema. Intensive Care Med. 2019, 45, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Haaksma, M.E.; Smit, J.M.; Heldeweg, M.L.A.; Nooitgedacht, J.S.; de Grooth, H.J.; Jonkman, A.H.; Girbes, A.R.J.; Heunks, L.; Tuinman, P.R. Extended Lung Ultrasound to Differentiate Between Pneumonia and Atelectasis in Critically Ill Patients: A Diagnostic Accuracy Study. Crit. Care Med. 2022, 50, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Zambon, M.; Greco, M.; Bocchino, S.; Cabrini, L.; Beccaria, P.F.; Zangrillo, A. Assessment of Diaphragmatic Dysfunction in the Critically Ill Patient with Ultrasound: A Systematic Review. Intensive Care Med. 2017, 43, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Vivier, E.; Mekontso Dessap, A. Bedside Ultrasound for Weaning from Mechanical Ventilation. Anesthesiology 2020, 132, 947–948. [Google Scholar] [CrossRef] [PubMed]
- Llamas-Álvarez, A.M.; Tenza-Lozano, E.M.; Latour-Pérez, J. Diaphragm and Lung Ultrasound to Predict Weaning Outcome. Chest 2017, 152, 1140–1150. [Google Scholar] [CrossRef] [PubMed]
- Santangelo, E.; Mongodi, S.; Bouhemad, B.; Mojoli, F. The Weaning from Mechanical Ventilation: A Comprehensive Ultrasound Approach. Curr. Opin. Crit. Care 2022, 28, 322–330. [Google Scholar] [CrossRef]
- Cao, J.; Wang, B.; Zhu, L.; Song, L. Pooled Analysis of Central Venous Pressure and Brain Natriuretic Peptide Levels in Patients With Extubation Failure. Front. Physiol. 2022, 13, 858046. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Tang, Y.; Zhao, M.; Yu, H.; Li, H. Association between Elevated Brain Natriuretic Peptide Levels and Weaning Failure: A Systematic Review and Meta-analysis. Int. J. Clin. Pract. 2021, 75. [Google Scholar] [CrossRef]
- Farghaly, S.; Galal, M.; Hasan, A.A.; Nafady, A. Brain Natriuretic Peptide as a Predictor of Weaning from Mechanical Ventilation in Patients with Respiratory Illness. Aust. Crit. Care 2015, 28, 116–121. [Google Scholar] [CrossRef]
- Kor, D.J.; Warner, D.O.; Carter, R.E.; Meade, L.A.; Wilson, G.A.; Li, M.; Hamersma, M.J.; Hubmayr, R.D.; Mauermann, W.J.; Gajic, O. Extravascular Lung Water and Pulmonary Vascular Permeability Index as Markers Predictive of Postoperative Acute Respiratory Distress Syndrome: A Prospective Cohort Investigation. Crit. Care Med. 2015, 43, 665–673. [Google Scholar] [CrossRef] [Green Version]
- Emperador, F.; Bennett, S.R.; Gonzalez, J.; Saati, A.; Alsaywid, B.S.; Fernandez, J.A. Extravascular Lung Water and Effect on Oxygenation Assessed by Lung Ultrasound in Adult Cardiac Surgery. Cureus 2020. [CrossRef]
- Monnet, X.; Teboul, J.-L. Transpulmonary Thermodilution: Advantages and Limits. Crit. Care 2017, 21, 147. [Google Scholar] [CrossRef] [PubMed]
- Subirà, C.; Hernández, G.; Vázquez, A.; Rodríguez-García, R.; González-Castro, A.; García, C.; Rubio, O.; Ventura, L.; López, A.; de la Torre, M.-C.; et al. Effect of Pressure Support vs T-Piece Ventilation Strategies During Spontaneous Breathing Trials on Successful Extubation Among Patients Receiving Mechanical Ventilation: A Randomized Clinical Trial. JAMA 2019, 321, 2175–2182. [Google Scholar] [CrossRef]
- Girard, T.D.; Alhazzani, W.; Kress, J.P.; Ouellette, D.R.; Schmidt, G.A.; Truwit, J.D.; Burns, S.M.; Epstein, S.K.; Esteban, A.; Fan, E.; et al. An Official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from Mechanical Ventilation in Critically Ill Adults. Rehabilitation Protocols, Ventilator Liberation Protocols, and Cuff Leak Tests. Am. J. Respir. Crit. Care Med. 2017, 195, 120–133. [Google Scholar] [CrossRef]
- Schreiber, A.F.; Ceriana, P.; Ambrosino, N.; Malovini, A.; Nava, S. Physiotherapy and Weaning From Prolonged Mechanical Ventilation. Respir. Care 2019, 64, 17–25. [Google Scholar] [CrossRef]
- Perkins, G.D.; Mistry, D.; Gates, S.; Gao, F.; Snelson, C.; Hart, N.; Camporota, L.; Varley, J.; Carle, C.; Paramasivam, E.; et al. Effect of Protocolized Weaning With Early Extubation to Noninvasive Ventilation vs Invasive Weaning on Time to Liberation From Mechanical Ventilation Among Patients With Respiratory Failure: The Breathe Randomized Clinical Trial. JAMA 2018, 320, 1881. [Google Scholar] [CrossRef] [PubMed]
- Arnal, J.-M.; Katayama, S.; Howard, C. Closed-Loop Ventilation. Curr. Opin. Crit. Care, 2022; Publish Ahead of Print. [Google Scholar] [CrossRef]
- Rose, L.; Schultz, M.J.; Cardwell, C.R.; Jouvet, P.; McAuley, D.F.; Blackwood, B. Automated versus Non-Automated Weaning for Reducing the Duration of Mechanical Ventilation for Critically Ill Adults and Children: A Cochrane Systematic Review and Meta-Analysis. Crit. Care 2015, 19, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chermesh, I.; Hajos, J.; Mashiach, T.; Bozhko, M.; Shani, L.; Nir, R.-R.; Bolotin, G. Malnutrition in Cardiac Surgery: Food for Thought. Eur. J. Prev. Cardiol. 2014, 21, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.-J.; Cassiere, H.A.; Dellis, S.L.; Manetta, F.; Kohn, N.; Hartman, A.R. Impact of Preoperative Prealbumin on Outcomes After Cardiac Surgery. J. Parenter. Enter. Nutr. 2015, 39, 870–874. [Google Scholar] [CrossRef] [PubMed]
- Reeves, B.C.; Ascione, R.; Chamberlain, M.H.; Angelini, G.D. Effect of Body Mass Index on Early Outcomes in Patients Undergoing Coronary Artery Bypass Surgery. J. Am. Coll. Cardiol. 2003, 42, 668–676. [Google Scholar] [CrossRef] [Green Version]
- Lopez-Delgado, J.C.; Muñoz-del Rio, G.; Flordelís-Lasierra, J.L.; Putzu, A. Nutrition in Adult Cardiac Surgery: Preoperative Evaluation, Management in the Postoperative Period, and Clinical Implications for Outcomes. J. Cardiothorac. Vasc. Anesth. 2019, 33, 3143–3162. [Google Scholar] [CrossRef]
- Bassili, H.R.; Deitel, M. Effect of Nutritional Support on Weaning Patients Off Mechanical Ventilators. J. Parenter. Enter. Nutr. 1981, 5, 161–163. [Google Scholar] [CrossRef]
- Huang, S.-W.; Lin, H.-C.; Chou, Y.-F.; Lin, T.-Y.; Lo, C.-Y.; Huang, H.-Y.; Fang, Y.-F.; Hsieh, M.-H.; Lin, S.-M.; Lo, Y.-L.; et al. The Impact of Higher Protein Intake in Patients with Prolonged Mechanical Ventilation. Nutrients 2022, 14, 4395. [Google Scholar] [CrossRef]
- Lo, S.-C.; Ma, K.S.-K.; Li, Y.-R.; Li, Z.-Y.; Lin, C.-H.; Lin, H.-C.; Yang, S.-F. Nutritional Support for Successful Weaning in Patients Undergoing Prolonged Mechanical Ventilation. Sci. Rep. 2022, 12, 12044. [Google Scholar] [CrossRef]
- Abd El Sabour Faramawy, M.; Abd Allah, A.; El Batrawy, S.; Amer, H. Impact of High Fat Low Carbohydrate Enteral Feeding on Weaning from Mechanical Ventilation. Egypt. J. Chest Dis. Tuberc. 2014, 63, 931–938. [Google Scholar] [CrossRef]
- Doig, G.S.; Simpson, F.; Sweetman, E.A.; Finfer, S.R.; Cooper, D.J.; Heighes, P.T.; Davies, A.R.; O’Leary, M.; Solano, T.; Peake, S.; et al. Early Parenteral Nutrition in Critically Ill Patients with Short-Term Relative Contraindications to Early Enteral Nutrition: A Randomized Controlled Trial. JAMA 2013, 309, 2130–2138. [Google Scholar] [CrossRef] [Green Version]
- Chen, Q.-H.; Yang, Y.; He, H.-L.; Xie, J.-F.; Cai, S.-X.; Liu, A.-R.; Wang, H.-L.; Qiu, H.-B. The Effect of Glutamine Therapy on Outcomes in Critically Ill Patients: A Meta-Analysis of Randomized Controlled Trials. Crit. Care Lond. Engl. 2014, 18, R8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, A.; Nesterova, E.; Lomivorotov, V.; Efremov, S.; Goetzenich, A.; Benstoem, C.; Zamyatin, M.; Chourdakis, M.; Heyland, D.; Stoppe, C. Current Evidence about Nutrition Support in Cardiac Surgery Patients—What Do We Know? Nutrients 2018, 10, 597. [Google Scholar] [CrossRef] [Green Version]
- Sareh, S.; Toppen, W.; Ugarte, R.; Sanaiha, Y.; Hadaya, J.; Seo, Y.J.; Aguayo, E.; Shemin, R.; Benharash, P. Impact of Early Tracheostomy on Outcomes After Cardiac Surgery: A National Analysis. Ann. Thorac. Surg. 2021, 111, 1537–1544. [Google Scholar] [CrossRef]
- Clec’h, C.; Alberti, C.; Vincent, F.; Garrouste-Orgeas, M.; de Lassence, A.; Toledano, D.; Azoulay, E.; Adrie, C.; Jamali, S.; Zaccaria, I.; et al. Tracheostomy Does Not Improve the Outcome of Patients Requiring Prolonged Mechanical Ventilation: A Propensity Analysis. Crit. Care Med. 2007, 35, 132–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toeg, H.; French, D.; Gilbert, S.; Rubens, F. Incidence of Sternal Wound Infection after Tracheostomy in Patients Undergoing Cardiac Surgery: A Systematic Review and Meta-Analysis. J. Thorac. Cardiovasc. Surg. 2017, 153, 1394–1400.e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litton, E.; Law, T.; Stamp, N. Tracheostomy in Patients Requiring Prolonged Mechanical Ventilation After Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2019, 33, 91–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okada, M.; Watanuki, H.; Masato, T.; Sugiyama, K.; Futamura, Y.; Matsuyama, K. Impact of Tracheostomy Timing on Outcomes After Cardiovascular Surgery. J. Cardiothorac. Vasc. Anesth. 2022, 36, 2335–2338. [Google Scholar] [CrossRef]
- Affronti, A.; Casali, F.; Eusebi, P.; Todisco, C.; Volpi, F.; Beato, V.; Manini, E.V.; Scopetani, G.; Ragni, T. Early Versus Late Tracheostomy in Cardiac Surgical Patients: A 12-Year Single Center Experience. J. Cardiothorac. Vasc. Anesth. 2019, 33, 82–90. [Google Scholar] [CrossRef]
- Krebs, E.D.; Chancellor, W.Z.; Beller, J.P.; Mehaffey, J.H.; Hawkins, R.B.; Sawyer, R.G.; Yarboro, L.T.; Ailawadi, G.; Teman, N.R. Long-Term Implications of Tracheostomy in Cardiac Surgery Patients: Decannulation and Mortality. Ann. Thorac. Surg. 2021, 111, 594–599. [Google Scholar] [CrossRef]
- Ballotta, A.; Kandil, H.; Generali, T.; Menicanti, L.; Pelissero, G.; Ranucci, M. Tracheostomy After Cardiac Operations: In-Hospital and Long-Term Survival. Ann. Thorac. Surg. 2011, 92, 528–533. [Google Scholar] [CrossRef]
- Ben-Avi, R.; Ben-Nun, A.; Levin, S.; Simansky, D.; Zeitlin, N.; Sternik, L.; Raanani, E.; Kogan, A. Tracheostomy After Cardiac Surgery: Timing of Tracheostomy as a Risk Factor for Mortality. J. Cardiothorac. Vasc. Anesth. 2014, 28, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Chorath, K.; Hoang, A.; Rajasekaran, K.; Moreira, A. Association of Early vs Late Tracheostomy Placement With Pneumonia and Ventilator Days in Critically Ill Patients: A Meta-Analysis. JAMA Otolaryngol. Neck Surg. 2021, 147, 450. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Jeong, I.B.; Kwon, S.J.; Son, J.W.; Ku, G.W. Safety and Feasibility of Hybrid Tracheostomy. Acute Crit. Care 2021, 36, 369–373. [Google Scholar] [CrossRef]
- Molardi, A.; Benassi, F.; Manca, T.; Ramelli, A.; Vezzani, A.; Nicolini, F.; Romano, G.; Ricci, M.; Carino, D.; Di Chicco, M.V.; et al. Parma Tracheostomy Technique: A Hybrid Approach to Tracheostomy between Classical Surgical and Percutaneous Tracheostomies. J. Thorac. Dis. 2016, 8, 3633–3638. [Google Scholar] [CrossRef] [Green Version]
- Di Lella, F.; Picetti, E.; Ciavarro, G.; Pepe, G.; Malchiodi, L.; D’Angelo, G.; Grossi, S.; Rossi, S.; Falcioni, M. Bedside Surgical Tracheostomy in the Intensive Care Unit during Covid-19 Pandemic. Ann. Otol. Rhinol. Laryngol. 2021, 130, 304–306. [Google Scholar] [CrossRef] [PubMed]
- Bermede, O.; Cahit Sarıcaoğlu, M.; Baytaş, V.; İhsan Hasde, A.; Bahadır İnan, M.; Rüçhan Akar, A. Percutaneous Ultrasound-Guided versus Bronchoscopy-Guided Dilatational Tracheostomy after Median Sternotomy: A Case-Control Study. Turk. J. Thorac. Cardiovasc. Surg. 2021, 29, 457–464. [Google Scholar] [CrossRef]
- Brass, P.; Hellmich, M.; Ladra, A.; Ladra, J.; Wrzosek, A. Percutaneous Techniques versus Surgical Techniques for Tracheostomy. Cochrane Database Syst. Rev. 2016, 7. [Google Scholar] [CrossRef] [PubMed]
| Author, Year, Reference | Patients | Preoperative Risk Factors | Intra/Postoperative Risk Factors | Protective Factors |
|---|---|---|---|---|
| Totonchi et al., 2014 [12] | 743 consecutive CPB patients | female sex, hypertension, COPD, CKD | endocarditis surgery, bleeding, inotrope dependency | isolated CABG, duration of surgery <4 h, CPB < 60 min |
| Murthy et al., 2007 [13] | 12,777 consecutive cardiovascular patients (excluding HTX and VAD) | BMI, NYHA class, COPD | aortic surgery, CPB time, bleeding, inotrope dependency, low cardiac index, early postoperative complications * | |
| Nozawa et al., 2005, [14] | 52 patients on prolonged ventilation (mean 10 days) after CPB surgery. † | cardiac complications ‡, RRT, inotrope dependency | ||
| Cislaghi et al., 2007, [15] | 3269 on-pump CABG patients | LVEF < 30% | re-do surgery, CPB > 90 min, PRBC transfusion, FFP transfusion | |
| Reddy et al., 2007, [16] | 12,662 consecutive cardiac surgery patients (both on- and off-pump) | age, FEV1 < 70%, current smoker, serum creatinine, peripheral vascular disease, LVEF < 30%, recent MI, preoperative ventilation | re-do surgery, urgent-emergent surgery, mitral valve surgery, aortic surgery, use of CPB | |
| Wang et al., 2022, [19] | 5323 CPB patients | age, renal failure, DM, COPD, preoperative pulmonary oedema | combined CABG + valvular surgery, aortic surgery, emergent surgery |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicolotti, D.; Grossi, S.; Nicolini, F.; Gallingani, A.; Rossi, S. Difficult Respiratory Weaning after Cardiac Surgery: A Narrative Review. J. Clin. Med. 2023, 12, 497. https://doi.org/10.3390/jcm12020497
Nicolotti D, Grossi S, Nicolini F, Gallingani A, Rossi S. Difficult Respiratory Weaning after Cardiac Surgery: A Narrative Review. Journal of Clinical Medicine. 2023; 12(2):497. https://doi.org/10.3390/jcm12020497
Chicago/Turabian StyleNicolotti, Davide, Silvia Grossi, Francesco Nicolini, Alan Gallingani, and Sandra Rossi. 2023. "Difficult Respiratory Weaning after Cardiac Surgery: A Narrative Review" Journal of Clinical Medicine 12, no. 2: 497. https://doi.org/10.3390/jcm12020497






