Correlation Analysis of Nasal Septum Deviation and Results of AI-Driven Automated 3D Cephalometric Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
- CT scan covering the region from the chin to the vertex;
- Age 18–30 years, to exclude multiple missing teeth and acquired craniofacial deformations from the measurements conducted;
- Centric occlusion of the patient’s teeth.
- Fractures of the craniofacial bones;
- Severe motion artifacts;
- >4 teeth missing per dental arch;
- Tumors in the craniofacial area;
- Severe metal artifacts.
2.2. Cephalometric Analysis
2.3. NSD Analysis
2.4. Error Study
2.5. Statistical Evaluation
3. Results
3.1. Population
3.2. Automatic Cephalometric Analysis
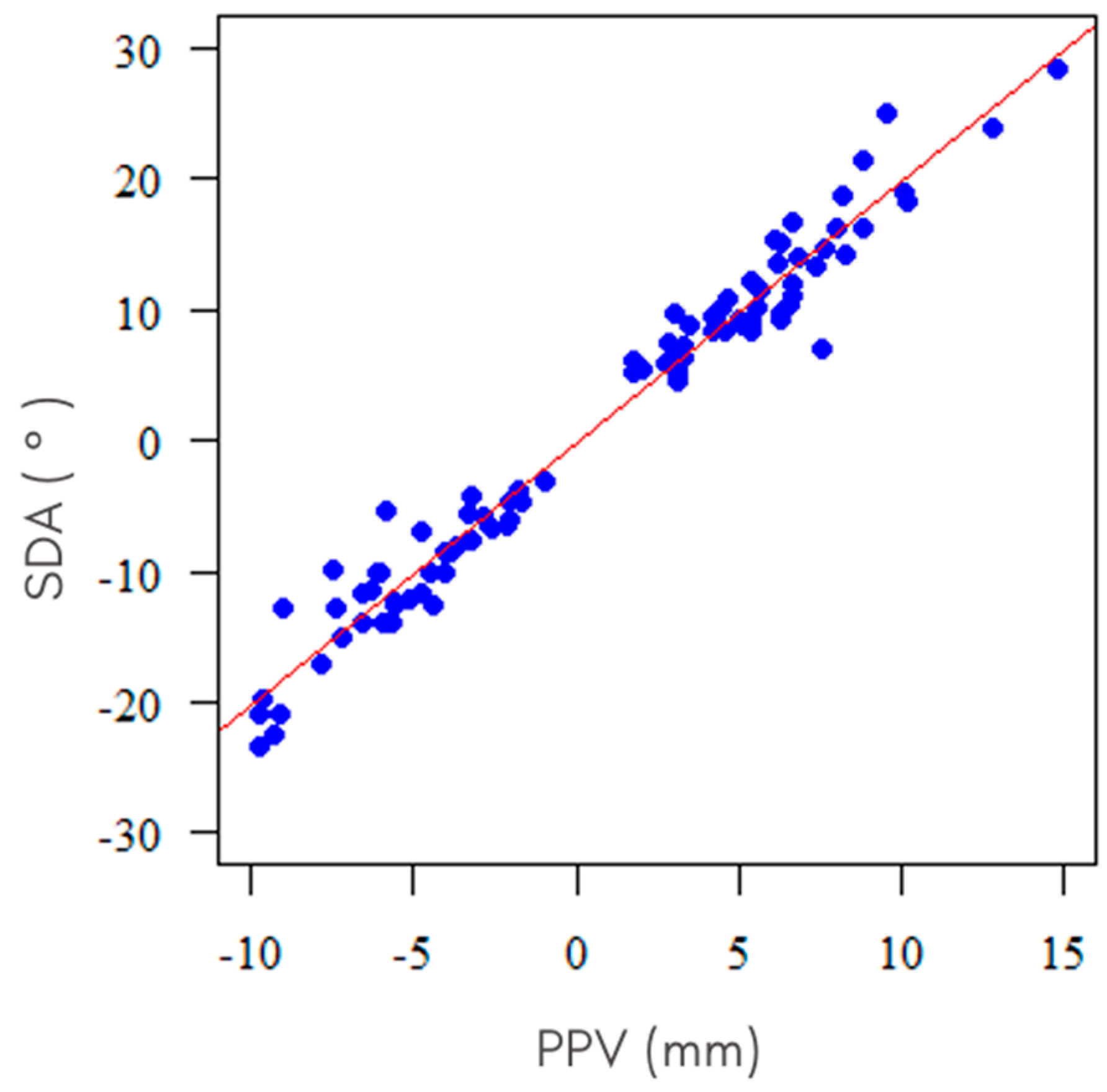
3.3. NSD Analysis
3.4. Error Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Latham, R.A. Maxillary Development and Growth: The Septo-Premaxillary Ligament. J. Anat. 1970, 107, 471–478. [Google Scholar]
- Goergen, M.J.; Holton, N.E.; Grünheid, T. Morphological Interaction between the Nasal Septum and Nasofacial Skeleton during Human Ontogeny. J. Anat. 2017, 230, 689–700. [Google Scholar] [CrossRef]
- Pirsig, W. Growth of the Deviated Septum and Its Influence on Midfacial Development. Facial Plast. Surg. 1992, 8, 224–232. [Google Scholar] [CrossRef]
- Hartman, C.; Holton, N.; Miller, S.; Yokley, T.; Marshall, S.; Srinivasan, S.; Southard, T. Nasal Septal Deviation and Facial Skeletal Asymmetries. Anat. Rec. 2015, 299, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Denour, E.; Roussel, L.O.; Woo, A.S.; Boyajian, M.; Crozier, J. Quantification of Nasal Septal Deviation with Computed Tomography Data. J. Craniofacial Surg. 2020, 31, 1659–1663. [Google Scholar] [CrossRef]
- Rönning, O.; Kantomaa, T. Experimental Nasal Septum Deviation in the Rat. Eur. J. Orthod. 1985, 7, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, D.E.; Hallgrímsson, B.; Liu, W.; Parsons, T.E.; Jamniczky, H.A. Spatial Packing, Cranial Base Angulation, and Craniofacial Shape Variation in the Mammalian Skull: Testing a New Model Using Mice. J. Anat. 2008, 212, 720–735. [Google Scholar] [CrossRef] [PubMed]
- Baddam, P.; Kung, T.; Adesida, A.B.; Graf, D. Histological and Molecular Characterization of the Growing Nasal Septum in Mice. J. Anat. 2020, 238, 751–764. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.E.; Downey, C.M.; Jirik, F.R.; Hallgrimsson, B.; Jamniczky, H.A. Mind the Gap: Genetic Manipulation of Basicranial Growth within Synchondroses Modulates Calvarial and Facial Shape in Mice through Epigenetic Interactions. PLoS ONE 2015, 10, e0118355. [Google Scholar] [CrossRef]
- Babula, W.J.; Smiley, G.R.; Dixon, A.D. The Role of the Cartilaginous Nasal Septum in Midfacial Growth. Am. J. Orthod. 1970, 58, 250–263. [Google Scholar] [CrossRef]
- Hall, B.K.; Precious, D.S. Cleft Lip, Nose, and Palate: The Nasal Septum as the Pacemaker for Midfacial Growth. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Holton, N.E.; Yokley, T.R.; Figueroa, A. Nasal Septal and Craniofacial Form in European- and African-Derived Populations. J. Anat. 2012, 221, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Stallman, J.S.; Lobo, J.N.; Som, P.M. The Incidence of Concha Bullosa and Its Relationship to Nasal Septal Deviation and Paranasal Sinus Disease. Am. J. Neuroradiol. 2004, 25, 1613–1618. [Google Scholar]
- Smith, K.D.; Edwards, P.C.; Saini, T.S.; Norton, N.S. The Prevalence of Concha Bullosa and Nasal Septal Deviation and Their Relationship to Maxillary Sinusitis by Volumetric Tomography. Int. J. Dent. 2010, 2010, 404982. [Google Scholar] [CrossRef]
- Zielnik-Jurkiewicz, B.; Olszewska-Sosińska, O. The Nasal Septum Deformities in Children and Adolescents from Warsaw, Poland. Int. J. Pediatr. Otorhinolaryngol. 2006, 70, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Šubarić, M.; Mladina, R. Nasal Septum Deformities in Children and Adolescents: A Cross Sectional Study of Children from Zagreb, Croatia. Int. J. Pediatr. Otorhinolaryngol. 2002, 63, 41–48. [Google Scholar] [CrossRef]
- Egeli, E.; Demirci, L.; Yazýcý, B.; Harputluoglu, U. Evaluation of the Inferior Turbinate in Patients with Deviated Nasal Septum by Using Computed Tomography. Laryngoscope 2004, 114, 113–117. [Google Scholar] [CrossRef]
- Estomba, C.C.; Schmitz, T.R.; Echeverri, C.C.O.; Reinoso, F.A.B.R.; Velasquez, A.O.; Hidalgo, C.S. Compensatory Hypertrophy of the Contralateral Inferior Turbinate in Patients with Unilateral Nasal Septal Deviation. A Computed Tomography Study. Otolaryngol. Polska 2015, 69, 14–20. [Google Scholar] [CrossRef]
- Orhan, I.; Aydin, S.; Ormeci, T.; Yilmaz, F. A Radiological Analysis of Inferior Turbinate in Patients with Deviated Nasal Septum by Using Computed Tomography. Am. J. Rhinol. Allergy 2014, 28, e68–e72. [Google Scholar] [CrossRef]
- Gray, L.P.; Brogan, W.F. Septal Deformity Malocclusion and Rapid Maxillary Expansion. Orthodontist 1972, 4, 2–14. [Google Scholar]
- Gray, L.P. The Development and Significance of Septal and Dental Deformity from Birth to Eight Years. Int. J. Pediatr. Otorhinolaryngol. 1984, 6, 265–277. [Google Scholar] [CrossRef]
- Kim, Y.M.; Rha, K.S.; Weissman, J.D.; Hwang, P.H.; Most, S.P. Correlation of Asymmetric Facial Growth with Deviated Nasal Septum. Laryngoscope 2011, 121, 1144–1148. [Google Scholar] [CrossRef]
- Gray, L.P.; Dillon, P.I.; Brogan, W.F.; Henry, P.J. The Development of Septal and Dental Deformity from Birth. Angle Orthod. 1982, 52, 265–278. [Google Scholar]
- Vig, K.W. Nasal Obstruction and Facial Growth: The Strength of Evidence for Clinical Assumptions. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 603–611. [Google Scholar] [CrossRef]
- D’Ascanio, L.; Lancione, C.; Pompa, G.; Rebuffini, E.; Mansi, N.; Manzini, M. Craniofacial Growth in Children with Nasal Septum Deviation: A Cephalometric Comparative Study. Int. J. Pediatr. Otorhinolaryngol. 2010, 74, 1180–1183. [Google Scholar] [CrossRef]
- Freng, A.; Kvam, E.; Kramer, J. Facial Skeletal Dimensions in Patients with Nasal Septal Deviation. Scand. J. Plast. Reconstr. Surg. 1988, 22, 77–81. [Google Scholar] [CrossRef]
- Leonardi, R.; Giordano, D.; Maiorana, F.; Spampinato, C. Automatic Cephalometric Analysis: A Systematic Review. Angle Orthod. 2008, 78, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.J.; Chen, S.K.; Yao, J.C.C.; Chang, H.F. The Effects of Differences in Landmark Identification on the Cephalometric Measurements in Traditional versus Digitized Cephalometry. Angle Orthod. 2004, 74, 155–161. [Google Scholar] [PubMed]
- Dias Da Silveira, H.L.; Dias Silveira, H.E. Reproducibility of Cephalometric Measurements Made by Three Radiology Clinics. Angle Orthod. 2006, 76, 394–399. [Google Scholar]
- Hwang, H.-W.; Moon, J.-H.; Kim, M.-G.; Donatelli, R.E.; Lee, S.-J. Evaluation of Automated Cephalometric Analysis Based on the Latest Deep Learning Method. Angle Orthod. 2021, 91, 329–335. [Google Scholar] [CrossRef]
- Hwang, H.W.; Park, J.H.; Moon, J.H.; Yu, Y.; Kim, H.; Her, S.B.; Srinivasan, G.; Aljanabi, M.N.A.; Donatelli, R.E.; Lee, S.J. Automated Identification of Cephalometric Landmarks: Part 2-Might It Be Better than Human? Angle Orthod. 2020, 90, 69–76. [Google Scholar] [CrossRef]
- Nishimoto, S. Locating Cephalometric Landmarks with Multi-Phase Deep Learning. J. Dent. Health Oral Res. 2023, 4, 1–13. [Google Scholar] [CrossRef]
- Kang, S.H.; Jeon, K.; Kang, S.H.; Lee, S.H. 3D Cephalometric Landmark Detection by Multiple Stage Deep Reinforcement Learning. Sci. Rep. 2021, 11, 17509. [Google Scholar] [CrossRef]
- Chung, E.J.; Yang, B.E.; Park, I.Y.; Yi, S.; On, S.W.; Kim, Y.H.; Kang, S.H.; Byun, S.H. Effectiveness of Cone-Beam Computed Tomography-Generated Cephalograms Using Artificial Intelligence Cephalometric Analysis. Sci. Rep. 2022, 12, 20585. [Google Scholar] [CrossRef]
- Meric, P.; Naoumova, J. Web-Based Fully Automated Cephalometric Analysis: Comparisons between App-Aided, Computerized, and Manual Tracings. Turk. J. Orthod. 2020, 33, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, H. Evaluation of an Online Website-Based Platform for Cephalometric Analysis. J. Stomatol. Oral Maxillofac. Surg. 2020, 121, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Bulatova, G.; Kusnoto, B.; Grace, V.; Tsay, T.P.; Avenetti, D.M.; Sanchez, F.J.C. Assessment of Automatic Cephalometric Landmark Identification Using Artificial Intelligence. Orthod. Craniofac. Res. 2021, 24, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Tsolakis, I.A.; Tsolakis, A.I.; Elshebiny, T.; Matthaios, S.; Palomo, J.M. Comparing a Fully Automated Cephalometric Tracing Method to a Manual Tracing Method for Orthodontic Diagnosis. J. Clin. Med. 2022, 11, 6854. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Spampinato, C.; Leonardi, R. Fully Automatic Segmentation of the Mandible Based on Convolutional Neural Networks (CNNs). Orthod. Craniofac. Res. 2021, 24, 100–107. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Gastaldi, G.; Leonardi, R. Assessment of the Accuracy of Imaging Software for 3D Rendering of the Upper Airway, Usable in Orthodontic and Craniofacial Clinical Settings. Prog. Orthod. 2022, 23, 22. [Google Scholar] [CrossRef] [PubMed]
- Mosleh, M.A.A.; Baba, M.S.; Malek, S.; Almaktari, R.A. Ceph-X: Development and Evaluation of 2D Cephalometric System. BMC Bioinform. 2016, 17, 499 . [Google Scholar] [CrossRef]
- Lin, J.K.; Wheatley, F.C.; Handwerker, J.; Harris, N.J.; Wong, B.J.F. Analyzing Nasal Septal Deviations to Develop a New Classification System: A Computed Tomography Study Using MATLAB and OsiriX. JAMA Facial Plast. Surg. 2014, 16, 183–187. [Google Scholar] [CrossRef]
- Dalili, K.Z.; Khademi, J.; Nemati, S.; Niksolat, E. The Effects of Septal Deviation, Concha Bullosa, and Their Combination on the Depth of Posterior Palatal Arch in Cone-Beam Computed Tomography. J. Dent. 2016, 17, 26–31. [Google Scholar]
- Lee, J.H.; Yu, H.J.; Kim, M.J.; Kim, J.W.; Choi, J. Automated Cephalometric Landmark Detection with Confidence Regions Using Bayesian Convolutional Neural Networks. BMC Oral Health 2020, 20, 270. [Google Scholar] [CrossRef]
- Song, Y.; Qiao, X.; Iwamoto, Y.; Chen, Y.W. Automatic Cephalometric Landmark Detection on X-Ray Images Using a Deep-Learning Method. Appl. Sci. 2020, 10, 2547. [Google Scholar] [CrossRef]
- Bao, H.; Zhang, K.; Yu, C.; Li, H.; Cao, D.; Shu, H.; Liu, L.; Yan, B. Evaluating the Accuracy of Automated Cephalometric Analysis Based on Artificial Intelligence. BMC Oral Health 2023, 23, 191. [Google Scholar] [CrossRef] [PubMed]
- Barretto, M.D.A.; Melhem-Elias, F.; Deboni, M.C.Z. Methods of Mandibular Condyle Position and Rotation Center Used for Orthognathic Surgery Planning: A Systematic Review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 345–352. [Google Scholar]
- Ricketts, R.M. Perspectives in the Clinical Application of Cephalometrics. The First Fifty Years. Angle Orthod. 1981, 51, 115–150. [Google Scholar] [PubMed]
- Solow, B.; Tallgren, A. Natural Head Position in Standing Subjects. Acta Odontol. Scand. 1971, 29, 591–607. [Google Scholar] [CrossRef]
- Billiaert, K.; Al-Yassary, M.; Antonarakis, G.S.; Kiliaridis, S. Measuring the Difference in Natural Head Position between the Standing and Sitting Positions Using an Inertial Measurement Unit. J. Oral Rehabil. 2021, 48, 1144–1149. [Google Scholar] [CrossRef] [PubMed]
- Torre, C.; Capasso, R.; Zaghi, S.; Williams, R.; Liu, S.Y.-C. High Incidence of Posterior Nasal Cavity Obstruction in Obstructive Sleep Apnea Patients. Sleep Sci. Pract. 2017, 1, 286. [Google Scholar] [CrossRef][Green Version]
- Wong, E.; Deboever, N.; Sritharan, N.; Singh, N. Laryngopharyngeal Reflux Is Associated with Nasal Septal Deviation. Eur. J. Rhinol. Allergy 2020, 3, 1–3. [Google Scholar] [CrossRef]
- Kwon, S.H.; Lee, E.J.; Yeo, C.D.; Kim, M.G.; Kim, J.S.; Noh, S.J.; Kim, E.J.; Kim, S.G.; Lee, J.-H.; Yoo, J.S.; et al. Is Septal Deviation Associated with Headache? Medicine 2020, 99, e20337. [Google Scholar] [CrossRef]
- Orlandi, R.R. A Systematic Analysis of Septal Deviation Associated with Rhinosinusitis. Laryngoscope 2010, 120, 1687–1695. [Google Scholar] [CrossRef]
- Grymer, L.F.; Bosch, C. The Nasal Septum and the Development of the Midface. A Longitudinal Study of a Pair of Monozygotic Twins. Rhinology 1997, 35, 6–10. [Google Scholar]
- Pirsig, W. Historical Notes and Actual Observations on the Nasal Septal Abscess Especially in Children. Int. J. Pediatr. Otorhinolaryngol. 1984, 8, 43–54. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, S.W.; Kim, S.W.; Cho, J.H.; Park, Y.J. Role of the Sphenoidal Process of the Septal Cartilage in the Development of Septal Deviation. Otolaryngol. Head Neck Surg. 2012, 146, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Mays, S. Nasal Septal Deviation in a Mediaeval Population. Am. J. Phys. Anthropol. 2012, 148, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Peck, H.; Peck, S. A Concept of Facial Esthetics. Angle Orthod. 1970, 40, 284–317. [Google Scholar]
- Masoud, M.I.; Bansal, N.; Castillo, J.C.; Manosudprasit, A.; Allareddy, V.; Haghi, A.; Hawkins, H.C.; Otárola-Castillo, E. 3D Dentofacial Photogrammetry Reference Values: A Novel Approach to Orthodontic Diagnosis. Eur. J. Orthod. 2017, 39, 215–225. [Google Scholar] [CrossRef]
- Tanikawa, C. Facial Morphospace: A Clinical Quantitative Analysis of the Three-Dimensional Face in Patients with Cleft Lip and Palate. Plast. Aesthet. Res. 2020, 7, 48. [Google Scholar] [CrossRef]
- Tanikawa, C.; Akcam, M.O.; Takada, K. Quantifying Faces Three-Dimensionally in Orthodontic Practice. J. Cranio Maxillofac. Surg. 2019, 47, 867–875. [Google Scholar] [CrossRef]
- Tomaka, A.A.; Luchowski, L.; Pojda, D.; Tarnawski, M.; Domino, K. The Dynamics of the Stomatognathic System from 4D Multimodal Data. In Multiscale Locomotion: Its Active-Matter Addressing Physical Principles; Gadomski, A., Ed.; Publishing Department of the UTP University of Science & Technology: Bydgoszcz, Poland, 2019. [Google Scholar]
- Joda, T.; Gallucci, G.O. The Virtual Patient in Dental Medicine. Clin. Oral Implants. Res. 2015, 26, 725–726. [Google Scholar] [CrossRef] [PubMed]
- Tanikawa, C.; Yamashiro, T. Development of Novel Artificial Intelligence Systems to Predict Facial Morphology after Orthognathic Surgery and Orthodontic Treatment in Japanese Patients. Sci. Rep. 2021, 11, 15853. [Google Scholar] [CrossRef] [PubMed]
- Resnick, C.M.; Dang, R.R.; Glick, S.J.; Padwa, B.L. Accuracy of Three-Dimensional Soft Tissue Prediction for Le Fort I Osteotomy Using Dolphin 3D Software: A Pilot Study. Int. J. Oral Maxillofac. Surg. 2017, 46, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Elshebiny, T.; Morcos, S.; Mohammad, A.; Quereshy, F.; Valiathan, M. Accuracy of Three-Dimensional Soft Tissue Prediction in Orthognathic Cases Using Dolphin Three-Dimensional Software. J. Craniofacial Surg. 2019, 30, 525–528. [Google Scholar] [CrossRef]
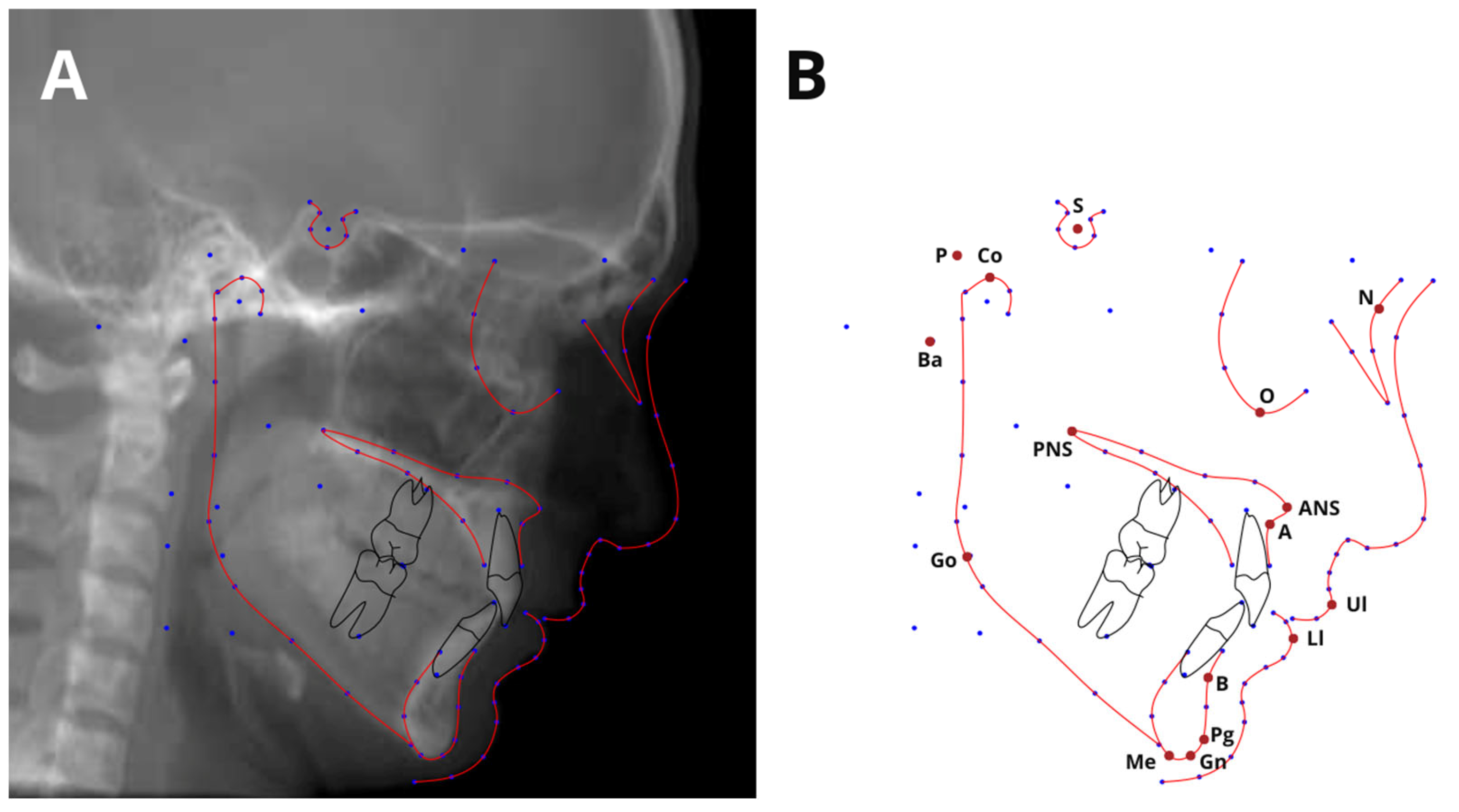


| Landmark | Definition | |
|---|---|---|
| S | Sella | Midpoint of the sella turcica |
| Co | Condylion | The extreme superior point on the condylar head |
| ANS | Anterior Nasal Spine | Tip of the bony anterior nasal spine in the midline |
| N | Nasion | The most anterior point of the frontonasal suture |
| A | Point A | The innermost point on the contour of the maxilla between the anterior nasal spine and the alveolar crest |
| B | Point B | The most posterior point in the concavity along the anterior border of the symphysis |
| Go | Gonion | The most prominent point on the angle of the mandible formed by the junction of the ramus and the body of the mandible |
| Gn | Gnathion | The most inferior bony point of the mandible |
| Ll | Lower Lip | The most anterior point of the lower lip |
| Me | Menton | The most inferior point of the mandibular symphysis in the midline |
| N | Nasion | The most anterior point of the frontonasal suture |
| Or | Orbitale | The lowest point on the inferior margin of the orbit |
| P | Porion | The central point on the upper margin of the external auditory meatus |
| Pr | Prosthion | The point of alveolar contact with the upper central incisor |
| Pg | Pogonion | The most anterior point on the contour of the bony chin |
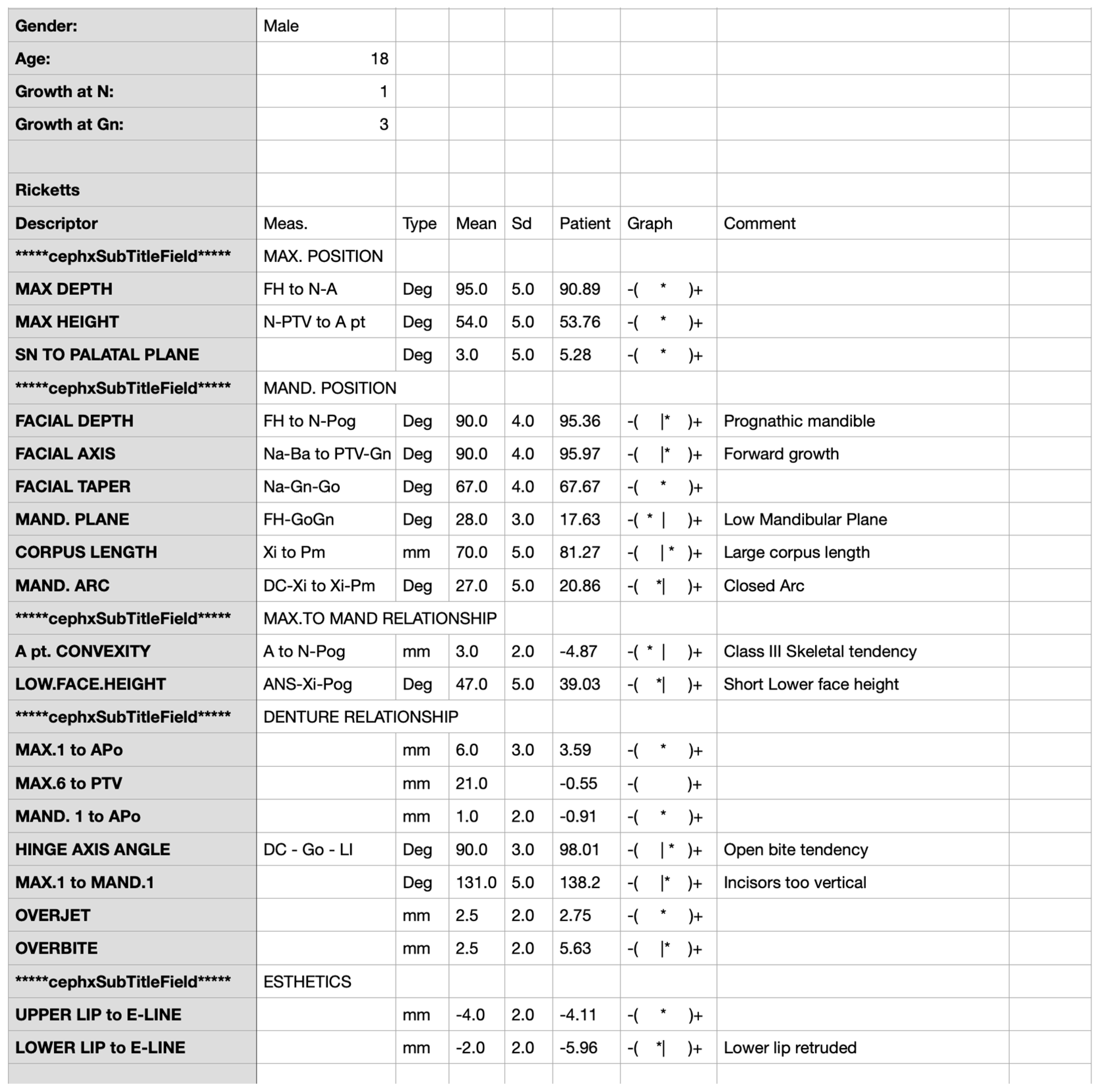
| Parameter | SDA (°) | PPV (mm) |
|---|---|---|
| Spearman’s Rank Correlation Coefficient | Spearman’s Rank Correlation Coefficient | |
| HINGE AXIS ANGLE (°) | r= −0.218, p = 0.039 * | r = −0.186, p = 0.079 |
| Björk–Jarabak cephalometric analysis | ||
| SADDLE ANGLE (°) | r = 0.017, p = 0.875 | r = −0.02, p = 0.853 |
| ARTICULAR ANGLE (°) | r = 0.103, p = 0.335 | r = 0.104, p = 0.329 |
| GONIAL ANGLE (°) | r = −0.154, p = 0.148 | r = −0.129, p = 0.226 |
| SUM OF ANGLES (°) | r = 0.044, p = 0.679 | r = 0.03. p = 0.782 |
| UPPER GONIAL ANGLE (°) | r = −0.175, p = 0,099 | r = −0.183, p = 0.084 |
| LOWER GONIAL ANGLE (°) | r = −0.002, p = 0.984 | r = 0.023, p = 0.826 |
| ANT. CRANIAL BASE (mm) | r = −0.011, p = 0.915 | r = 0.018, p = 0.67 |
| POST. CRANIAL BASE (mm) | r = 0.018, p = 0.866 | r = 0.052, p = 0.626 |
| RAMUS HEIGHT (mm) | r = 0.024, p = 0.825 | r = 0.099, p = 0.353 |
| MANDIBULAR BODY (mm) | r = −0.02, p = 0.851 | r = −0.004, p = 0.972 |
| POST. FACE HEIGHT (mm) | r = 0.031, p = 0.77 | r = 0.096, p = 0.368 |
| ANT. FACE HEIGHT (mm) | r = −0.016, p = 0.879 | r = 0.043, p = 0.69 |
| PFH:AFH (%) | r = 0.023, p = 0.832 | r = 0.053, p = 0.623 |
| ACB:MAND.BODY (%) | r = 0.004, p = 0.97 | r = −0.023, p = 0.832 |
| UI to SN (°) | r = −0.096, p = 0.37 | r = −0.094, p = 0.376 |
| UI to FH (°) | r = −0.073, p = 0.497 | r = −0.074, p = 0.486 |
| UPPER FACE HEIGHT (%) | r = −0.127, p = 0.233 | r = −0.057, p = 0.596 |
| LOWER FACE HEIGHT (%) | r = 0.125, p = 0.24 | r = 0.065, p = 0.544 |
| Parameter | Measurement I (Mean ± SD) | Measurement II (Mean ± SD) | ICC | 95% CI | Agreement (Cicchetti) | Agreement (Koo and Li) | |
|---|---|---|---|---|---|---|---|
| PPV (mm) | 5.19 ± 2.6 | 5.28 ± 2.49 | 0.974 | 0.937 | 0.990 | Excellent | PPV (mm) |
| SDA (°) | 10.78 ± 5.69 | 10.85 ± 5.73 | 0.972 | 0.931 | 0.989 | Excellent | SDA (°) |
| Parameter | Measurement 1 (Mean ± SD) | Measurement 2 (Mean ± SD) | ICC | 95% CI | Agreement (Cicchetti) | Agreement (Koo and Li) | |
|---|---|---|---|---|---|---|---|
| LI-N-B | 21.73 ± 8.41 | 36.67 ± 45.54 | 0.000 | −0.536 | 0.548 | Poor | Poor |
| Pr-N-A | 1.76 ± 0.66 | 1.85 ± 0.54 | 0.302 | −0.287 | 0.730 | Poor | Poor |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kazimierczak, N.; Kazimierczak, W.; Serafin, Z.; Nowicki, P.; Lemanowicz, A.; Nadolska, K.; Janiszewska-Olszowska, J. Correlation Analysis of Nasal Septum Deviation and Results of AI-Driven Automated 3D Cephalometric Analysis. J. Clin. Med. 2023, 12, 6621. https://doi.org/10.3390/jcm12206621
Kazimierczak N, Kazimierczak W, Serafin Z, Nowicki P, Lemanowicz A, Nadolska K, Janiszewska-Olszowska J. Correlation Analysis of Nasal Septum Deviation and Results of AI-Driven Automated 3D Cephalometric Analysis. Journal of Clinical Medicine. 2023; 12(20):6621. https://doi.org/10.3390/jcm12206621
Chicago/Turabian StyleKazimierczak, Natalia, Wojciech Kazimierczak, Zbigniew Serafin, Paweł Nowicki, Adam Lemanowicz, Katarzyna Nadolska, and Joanna Janiszewska-Olszowska. 2023. "Correlation Analysis of Nasal Septum Deviation and Results of AI-Driven Automated 3D Cephalometric Analysis" Journal of Clinical Medicine 12, no. 20: 6621. https://doi.org/10.3390/jcm12206621
APA StyleKazimierczak, N., Kazimierczak, W., Serafin, Z., Nowicki, P., Lemanowicz, A., Nadolska, K., & Janiszewska-Olszowska, J. (2023). Correlation Analysis of Nasal Septum Deviation and Results of AI-Driven Automated 3D Cephalometric Analysis. Journal of Clinical Medicine, 12(20), 6621. https://doi.org/10.3390/jcm12206621








