Hyperacusis Assessment Questionnaire—A New Tool Assessing Hyperacusis in Subjects with Tinnitus
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
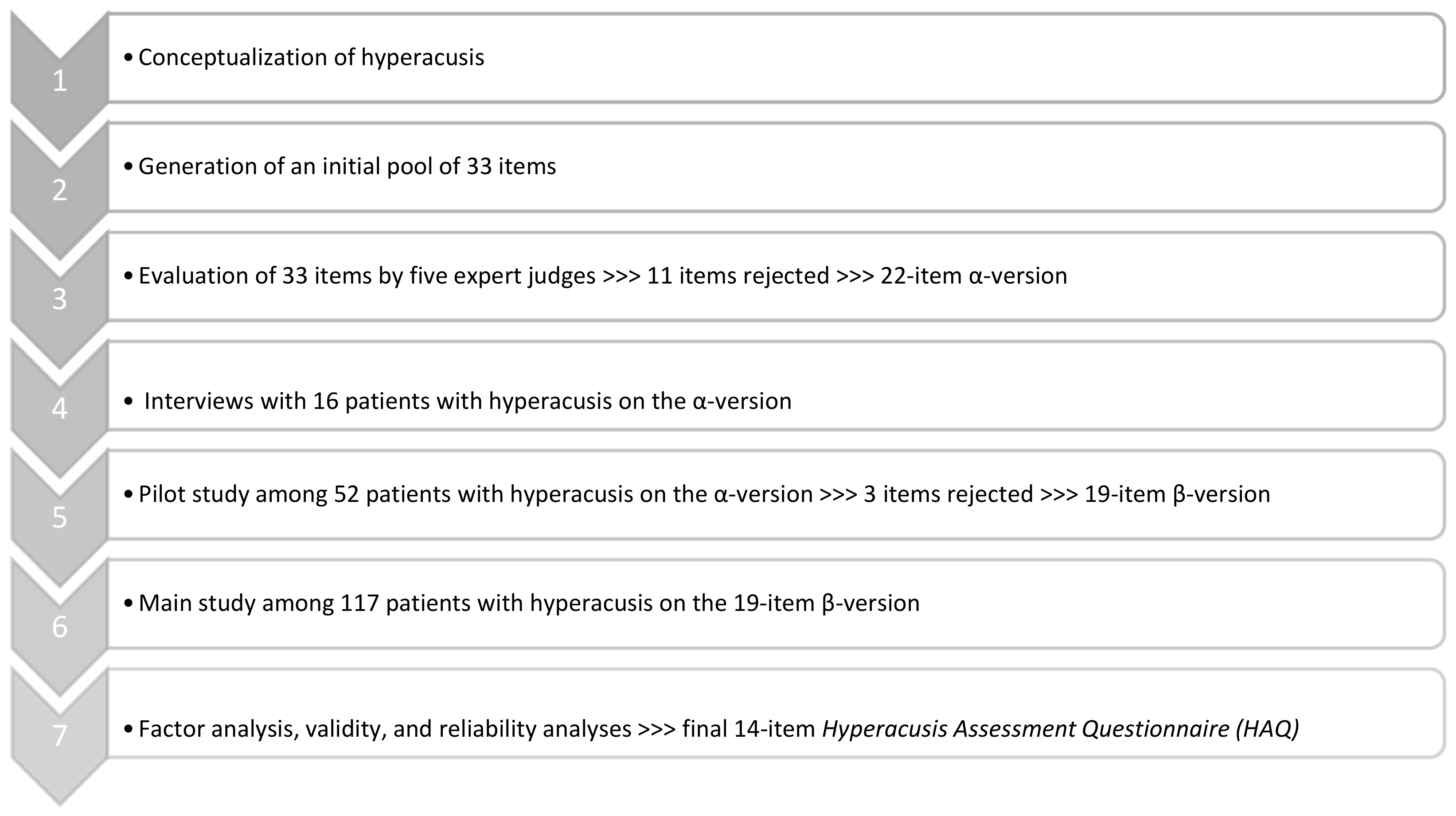
2.2. Hyperacusis Assessment Questionnaire Development
2.3. Measures
2.3.1. Interview
2.3.2. Audiological Examination
2.3.3. Patient-Reported Outcome Measures (PROMs)
2.4. Statistical Analysis
2.5. Participants
3. Results
3.1. Interview Data
3.2. Results of Audiological Evaluation
3.3. Factor Analysis
3.4. Subscales and Global Score of the Hyperacusis Assessment Questionnaire (HAQ)
3.5. Relationships between HAQ Scores and Other Measures
3.6. Internal Consistency and Reproducibility
4. Discussion
4.1. Factor Structure of HAQ
4.2. Correlations with Other Tools Measuring Hyperacusis
4.3. Hyperacusis and Tinnitus Severity
4.4. Hyperacusis and Anxiety
4.5. Hyperacusis, Hearing Thresholds, and Uncomfortable Loudness Level
4.6. Hyperacusis in Relation to Age and Gender
4.7. Limitations of the Study and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tyler, R.S.; Pienkowski, M.; Roncancio, E.R.; Jun, H.J.; Brozoski, T.; Dauman, N.; Dauman, N.; Andersson, G.; Keiner, A.J.; Cacace, A.T.; et al. A Review of Hyperacusis and Future Directions: Part I. Definitions and Manifestations. Am. J. Audiol. 2014, 23, 402–419. [Google Scholar] [CrossRef] [PubMed]
- Jüris, L.; Andersson, G.; Larsen, H.C.; Ekselius, L. Psychiatric Comorbidity and Personality Traits in Patients with Hyperacusis. Int. J. Audiol. 2013, 52, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Fabijańska, A.; Rogowski, M.; Bartnik, G.; Skarzynski, H. Program Badań Epidemiologicznych Nad Występowaniem Szumów i Nadwrażliwości Słuchowej w Polsce. Nowa Audiofonologia 1999, 13, 261–266. [Google Scholar]
- Andersson, G.; Lindvall, N.; Hursti, T.; Carlbring, P. Hypersensitivity to Sound (Hyperacusis): A Prevalence Study Conducted via the Internet and Post. Int. J. Audiol. 2002, 41, 545–554. [Google Scholar] [CrossRef]
- Hannula, S.; Bloigu, R.; Majamaa, K.; Sorri, M.; Mäki-Torkko, E. Self-Reported Hearing Problems among Older Adults: Prevalence and Comparison to Measured Hearing Impairment. J. Am. Acad. Audiol. 2011, 22, 550–559. [Google Scholar] [CrossRef]
- Paulin, J.; Andersson, L.; Nordin, S. Characteristics of Hyperacusis in the General Population. Noise Health 2016, 18, 178–184. [Google Scholar] [CrossRef]
- Hall, D.A.; Haider, H.; Szczepek, A.J.; Lau, P.; Rabau, S.; Jones-Diette, J.; Londero, A.; Edvall, N.K.; Cederroth, C.R.; Mielczarek, M.; et al. Systematic Review of Outcome Domains and Instruments Used in Clinical Trials of Tinnitus Treatments in Adults. Trials 2016, 17, 270. [Google Scholar] [CrossRef]
- Ren, J.; Xu, T.; Xiang, T.; Pu, J.; Liu, L.; Xiao, Y.; Lai, D. Prevalence of Hyperacusis in the General and Special Populations: A Scoping Review. Front. Neurol. 2021, 12, 706555. [Google Scholar] [CrossRef]
- Baguley, D.M.; Hoare, D.J. Hyperacusis: Major Research Questions. HNO 2018, 66, 358–363. [Google Scholar] [CrossRef]
- Adams, B.; Sereda, M.; Casey, A.; Byrom, P.; Stockdale, D.; Hoare, D.J. A Delphi Survey to Determine a Definition and Description of Hyperacusis by Clinician Consensus. Int. J. Audiol. 2021, 60, 607–613. [Google Scholar] [CrossRef]
- Jastreboff, P.; Jastreboff, M. Decreased Sound Tolerance and Tinnitus Retraining Therapy (TRT). Aust. N. Z. J. Audiol. 2002, 24, 74–84. [Google Scholar] [CrossRef]
- Tyler, R.S.; Conrad-Armes, D. The Determination of Tinnitus Loudness Considering the Effects of Recruitment. J. Speech Hear. Res. 1983, 26, 59–72. [Google Scholar] [CrossRef] [PubMed]
- Fackrell, K.; Sereda, M.; Smith, S.; Sheldrake, J.; Hoare, D.J. What Should Be Considered When Assessing Hyperacusis? A Qualitative Analysis of Problems Reported by Hyperacusis Patients. Brain Sci. 2022, 12, 1615. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, B.D.; Rodrigues, P.V.; Salvi, R.J. Central Gain Control in Tinnitus and Hyperacusis. Front. Neurol. 2014, 5, 206. [Google Scholar] [CrossRef] [PubMed]
- Knipper, M.; Van Dijk, P.; Nunes, I.; Rüttiger, L.; Zimmermann, U. Advances in the Neurobiology of Hearing Disorders: Recent Developments Regarding the Basis of Tinnitus and Hyperacusis. Prog. Neurobiol. 2013, 111, 17–33. [Google Scholar] [CrossRef] [PubMed]
- Zeng, F.-G. An Active Loudness Model Suggesting Tinnitus as Increased Central Noise and Hyperacusis as Increased Nonlinear Gain. Hear. Res. 2013, 295, 172–179. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Li, X.; Liu, L.; Wang, J.; Lu, C.-Q.; Yang, M.; Jiao, Y.; Zang, F.-C.; Radziwon, K.; Chen, G.-D.; et al. Tinnitus and Hyperacusis Involve Hyperactivity and Enhanced Connectivity in Auditory-Limbic-Arousal-Cerebellar Network. Elife 2015, 4, e06576. [Google Scholar] [CrossRef]
- Pienkowski, M. Rationale and Efficacy of Sound Therapies for Tinnitus and Hyperacusis. Neuroscience 2019, 407, 120–134. [Google Scholar] [CrossRef]
- Behler, O.; Uppenkamp, S. The Representation of Level and Loudness in the Central Auditory System for Unilateral Stimulation. Neuroimage 2016, 139, 176–188. [Google Scholar] [CrossRef]
- Behler, O.; Uppenkamp, S. Activation in Human Auditory Cortex in Relation to the Loudness and Unpleasantness of Low-Frequency and Infrasound Stimuli. PLoS ONE 2020, 15, e0229088. [Google Scholar] [CrossRef]
- Koops, E.A.; van Dijk, P. Hyperacusis in Tinnitus Patients Relates to Enlarged Subcortical and Cortical Responses to Sound except at the Tinnitus Frequency. Hear. Res. 2021, 401, 108158. [Google Scholar] [CrossRef]
- Vernon, J.A. Pathophysiology of Tinnitus: A Special Case—Hyperacusis and a Proposed Treatment. Otol. Neurotol. 1987, 8, 201–202. [Google Scholar]
- Gabriels, P. Hyperacusis—Can We Help? Aust. J. Audiol. 1993, 15, 1–4. [Google Scholar]
- Noreña, A.J.; Chery-Croze, S. Enriched Acoustic Environment Rescales Auditory Sensitivity. Neuroreport 2007, 18, 1251–1255. [Google Scholar] [CrossRef] [PubMed]
- Formby, C.; Hawley, M.; Sherlock, L.; Gold, S.; Parton, J.; Brooks, R.; Payne, J. Intervention for Restricted Dynamic Range and Reduced Sound Tolerance: Clinical Trial Using a Tinnitus Retraining Therapy Protocol for Hyperacusis. J. Acoust. Soc. Am. 2013, 133, 3382. [Google Scholar] [CrossRef]
- Formby, C.; Hawley, M.L.; Sherlock, L.P.; Gold, S.; Payne, J.; Brooks, R.; Parton, J.M.; Juneau, R.; Desporte, E.J.; Siegle, G.R. A Sound Therapy-Based Intervention to Expand the Auditory Dynamic Range for Loudness among Persons with Sensorineural Hearing Losses: A Randomized Placebo-Controlled Clinical Trial. Semin. Hear. 2015, 36, 77–110. [Google Scholar] [CrossRef]
- Silverstein, H.; Ojo, R.; Daugherty, J.; Nazarian, R.; Wazen, J. Minimally Invasive Surgery for the Treatment of Hyperacusis. Otol. Neurotol. 2016, 37, 1482–1488. [Google Scholar] [CrossRef]
- Silverstein, H.; Kellermeyer, B.; Martinez, U. Minimally Invasive Surgery for the Treatment of Hyperacusis: New Technique and Long Term Results. Am. J. Otolaryngol. 2020, 41, 102319. [Google Scholar] [CrossRef]
- Hoffman, H.; Reed, G. Epidemiology of tinnitus. In Tinnitus: Theory and Management; BC Decker Inc.: Hamilton, ON, Canada, 2004; pp. 16–41. [Google Scholar]
- Jastreboff, P.; Jastreboff, M. Decreased Sound Tolerance: Hyperacusis, Misophonia, Diplacousis, and Polyacousis. Handb. Clin. Neurol. 2015, 129C, 375–387. [Google Scholar] [CrossRef]
- Anari, M.; Axelsson, A.; Eliasson, A.; Magnusson, L. Hypersensitivity to Sound–Questionnaire Data, Audiometry and Classification. Scand. Audiol. 1999, 28, 219–230. [Google Scholar] [CrossRef]
- Schecklmann, M.; Landgrebe, M.; Langguth, B.; TRI Database Study Group. Phenotypic Characteristics of Hyperacusis in Tinnitus. PLoS ONE 2014, 9, e86944. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, T.G.; Moraes, F.; Casseb, J.; Cota, J.; Freire, K.; Roberts, L.E. Tinnitus Is Associated with Reduced Sound Level Tolerance in Adolescents with Normal Audiograms and Otoacoustic Emissions. Sci. Rep. 2016, 6, 27109. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.W.; Jacobson, G.P.; Spitzer, J.B. Development of the Tinnitus Handicap Inventory. Arch. Otolaryngol. Head Neck Surg. 1996, 122, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.W.; Sandridge, S.A.; Jacobson, G.P. Psychometric Adequacy of the Tinnitus Handicap Inventory (THI) for Evaluating Treatment Outcome. J. Am. Acad. Audiol. 1998, 9, 153–160. [Google Scholar] [PubMed]
- Meikle, M.B.; Henry, J.A.; Griest, S.E.; Stewart, B.J.; Abrams, H.B.; McArdle, R.; Myers, P.J.; Newman, C.W.; Sandridge, S.; Turk, D.C.; et al. The Tinnitus Functional Index: Development of a New Clinical Measure for Chronic, Intrusive Tinnitus. Ear Hear. 2012, 33, 153–176. [Google Scholar] [CrossRef] [PubMed]
- Khalfa, S.; Dubal, S.; Veuillet, E.; Perez-Diaz, F.; Jouvent, R.; Collet, L. Psychometric Normalization of a Hyperacusis Questionnaire. ORL J. Otorhinolaryngol. Relat. Spec. 2002, 64, 436–442. [Google Scholar] [CrossRef]
- Fackrell, K.; Fearnley, C.; Hoare, D.J.; Sereda, M. Hyperacusis Questionnaire as a Tool for Measuring Hypersensitivity to Sound in a Tinnitus Research Population. Biomed. Res. Int. 2015, 2015, 290425. [Google Scholar] [CrossRef]
- Dauman, R.; Bouscau-Faure, F. Assessment and Amelioration of Hyperacusis in Tinnitus Patients. Acta Otolaryngol. 2005, 125, 503–509. [Google Scholar] [CrossRef]
- Prabhu, P.; Nagaraj, M.K. Development and Validation of Hyperacusis Handicap Questionnaire in Individuals with Tinnitus Associated with Hyperacusis. J. Otol. 2020, 15, 124–128. [Google Scholar] [CrossRef]
- Greenberg, B.; Carlos, M. Psychometric Properties and Factor Structure of a New Scale to Measure Hyperacusis: Introducing the Inventory of Hyperacusis Symptoms. Ear Hear. 2018, 39, 1025–1034. [Google Scholar] [CrossRef]
- Aazh, H.; Danesh, A.A.; Moore, B.C.J. Internal Consistency and Convergent Validity of the Inventory of Hyperacusis Symptoms. Ear Hear. 2021, 42, 917–926. [Google Scholar] [CrossRef] [PubMed]
- Skarzynski, P.H.; Raj-Koziak, D.; Rajchel, J. Adaptation of the Tinnitus Handicap Inventory into Polish and Its Testing on a Clinical Population of Tinnitus Sufferers. Int. J. Audiol. 2017, 56, 711–715. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.; Gorsuch, R.; Lushene, R.; Vagg, P.; Jacobs, G. Manual for the State-Trait Anxiety Inventory (Form Y1–Y2); Consulting Psychologists Press: Palo Alto, CA, USA, 1983; Volume IV. [Google Scholar]
- Wrześniewski, K.; Sosnowski, T.; Jaworowska, A.; Fecenec, D. Inwentarz Stanu i Cechy Lęku. Polska Adaptacja STAI; Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego: Warszawa, Poland, 2011. [Google Scholar]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory; McGraw-Hill Series in Psychology; 3rd ed. McGraw-Hill: New York, NY, USA, 1994; ISBN 978-0-07-047849-7. [Google Scholar]
- De Vet, H.C.W.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine—A Practical Guide; Cambridge University Press: New York, NY, USA, 2011. [Google Scholar]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 4th ed.; Allyn and Bacon: Boston, MA, USA, 2010. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson New International Edition; Pearson Education Limited: Harlow, UK, 2014; ISBN 978-1-292-02190-4. [Google Scholar]
- Fackrell, K.; Hall, D.A.; Barry, J.; Hoare, D.J. Tools for Tinnitus Measurement: Development and Validity of Questionnaires to Assess Handicap and Treatment Effects. In Tinnitus: Causes, Treatment and Short & Long Term Health Effects; Nova Science Publishers: Hauppauge, NY, USA, 2014; pp. 13–60. ISBN 978-1-63117-556-5. [Google Scholar]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality Criteria Were Proposed for Measurement Properties of Health Status Questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Williams, Z.J.; He, J.L.; Cascio, C.J.; Woynaroski, T.G. A Review of Decreased Sound Tolerance in Autism: Definitions, Phenomenology, and Potential Mechanisms. Neurosci. Biobehav. Rev. 2021, 121, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Swedo, S.; Baguley, D.M.; Denys, D.; Dixon, L.J.; Erfanian, M.; Fioretti, A.; Jastreboff, P.J.; Kumar, S.; Rosenthal, M.Z.; Rouw, R.; et al. A Consensus Definition of Misophonia: Using a Delphi Process to Reach Expert Agreement. medRxiv 2021. [Google Scholar] [CrossRef]
- Jager, I.; de Koning, P.; Bost, T.; Denys, D.; Vulink, N. Misophonia: Phenomenology, Comorbidity and Demographics in a Large Sample. PLoS ONE 2020, 15, e0231390. [Google Scholar] [CrossRef]
- Cederroth, C.R.; Lugo, A.; Edvall, N.K.; Lazar, A.; Lopez-Escamez, J.-A.; Bulla, J.; Uhlen, I.; Hoare, D.J.; Baguley, D.M.; Canlon, B.; et al. Association between Hyperacusis and Tinnitus. J. Clin. Med. 2020, 9, 2412. [Google Scholar] [CrossRef]
- Raj-Koziak, D.; Gos, E.; Kutyba, J.; Skarzynski, H.; Skarzynski, P.H. Decreased Sound Tolerance in Tinnitus Patients. Life 2021, 11, 87. [Google Scholar] [CrossRef]
- Blaesing, L.; Kroener-Herwig, B. Self-Reported and Behavioral Sound Avoidance in Tinnitus and Hyperacusis Subjects, and Association with Anxiety Ratings. Int. J. Audiol. 2012, 51, 611–617. [Google Scholar] [CrossRef]
- Nelting, M.; Rienhoff, N.; Hesse, G.; Lamparter, U. Die Erfassung Des Subjektiven Leidens Uner Hyperakusis Mit Einem Selbstbeurteilungsbogen Zur Geruschόberempfindlichkeit (GÜF). Laryngo-Rhino-Otologie 2002, 81, 327–334. [Google Scholar] [CrossRef]
- Ke, J.; Du, Y.; Tyler, R.S.; Perreau, A.; Mancini, P.C. Complaints of People with Hyperacusis. J. Am. Acad. Audiol. 2020, 31, 553–558. [Google Scholar] [CrossRef] [PubMed]
- Sherlock, L.P.; Formby, C. Estimates of Loudness, Loudness Discomfort, and the Auditory Dynamic Range: Normative Estimates, Comparison of Procedures, and Test-Retest Reliability. J. Am. Acad. Audiol. 2005, 16, 85–100. [Google Scholar] [CrossRef] [PubMed]
- Sheldrake, J.; Diehl, P.U.; Schaette, R. Audiometric Characteristics of Hyperacusis Patients. Front. Neurol. 2015, 6, 105. [Google Scholar] [CrossRef] [PubMed]


| Item Content | Factor I | Factor II | Factor III | Item Mean (SD) | Corrected Item–Total Correlation |
|---|---|---|---|---|---|
| 1. I perceive louder sounds as annoying | 0.782 | 0.077 | 0.037 | 3.49 (0.75) | 0.615 |
| 2. Some sounds, not disturbing to others, are too loud for me | 0.818 | 0.108 | 0.190 | 3.32 (0.71) | 0.511 |
| 3. I often find my surroundings too loud, while others are not bothered | 0.700 | −0.042 | −0.163 | 2.86 (1.09) | 0.668 |
| 4. Some domestic sounds are too loud for me, for example, dishes, cutlery, vacuum cleaner, kitchen mixer, hairdryer | 0.513 | 0.005 | −0.024 | 2.67 (1.26) | 0.413 |
| 5. It is definitely too loud for me at concerts, cinema, or sports events | 0.759 | 0.001 | −0.013 | 3.13 (1.12) | 0.627 |
| 6. I react to loud sounds more strongly than most people | 0.626 | −0.001 | −0.271 | 3.14 (0.99) | 0.699 |
| 7. I avoid situations that could be too loud for me | 0.567 | −0.154 | −0.381 | 2.80 (1.16) | 0.694 |
| 8. I often think there will be situations when it will be too loud for me | 0.241 | −0.053 | −0.772 | 2.09 (1.34) | 0.776 |
| 9. I am afraid of all loud sounds | 0.157 | 0.167 | −0.728 | 2.11 (1.31) | 0.475 |
| 10. I fear that in a while I will hear a loud sound, unpleasant for me | −0.096 | 0.089 | −0.955 | 1.81 (1.35) | 0.507 |
| 11. I am afraid that I will be exposed to loud sounds | −0.028 | 0.066 | −0.943 | 1.92 (1.36) | 0.515 |
| 12. Some sounds cause me ear pain and/or headache | 0.027 | 0.923 | −0.002 | 2.57 (1.35) | 0.822 |
| 13. After spending time in noisy places, I have ear pain and/or headache | 0.060 | 0.861 | −0.025 | 2.60 (1.21) | 0.711 |
| 14. Some sounds are so unpleasant that they are painful | −0.026 | 0.898 | −0.098 | 2.56 (1.33) | 0.743 |
| Min | Max | M | SD | Q1 | Me | Q3 | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|---|---|---|
| HAQ Loudness | 7 | 28 | 21.22 | 5.35 | 19 | 22 | 26 | −0.81 | −0.04 |
| HAQ Fear | 0 | 16 | 7.88 | 4.87 | 4 | 8 | 12 | −0.02 | −1.29 |
| HAQ Pain | 0 | 12 | 7.70 | 3.59 | 4 | 9 | 11 | −0.51 | −0.94 |
| HAQ Global score | 7 | 56 | 36.80 | 11.39 | 29 | 38 | 45 | −0.38 | −0.44 |
| VAS L | VAS F | VAS P | VAS M | KHQ | STAI | THI | ULL RE | ULL LE | AC RE | AC LE | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| M; SD | 67.6; 23.5 | 61.2; 29.4 | 42.6; 32.4 | 36.8; 33.5 | 21.7; 8.7 | 47.5; 9.3 | 56.1; 26.4 | 73.4; 17.8 | 73.5; 18.1 | 16.9; 11.8 | 17.7; 14.1 |
| HAQ-L | 0.62 *** | 0.60 *** | 0.37 *** | 0.16 | 0.69 *** | 0.33 *** | 0.28 ** | 0.05 | 0.03 | 0.08 | 0.11 |
| HAQ-F | 0.50 *** | 0.67 *** | 0.36 *** | 0.18 | 0.56 *** | 0.46 *** | 0.36 *** | 0.19 | 0.10 | 0.03 | 0.04 |
| HAQ-P | 0.26 ** | 0.34 *** | 0.77 *** | 0.05 | 0.40 *** | 0.11 | 0.08 | −0.09 | −0.12 | −0.15 | −0.13 |
| HAQ global score | 0.58 *** | 0.69 *** | 0.57 *** | 0.17 | 0.69 *** | 0.39 *** | 0.31 ** | 0.08 | 0.02 | 0.01 | 0.03 |
| Tinnitus as the Most Troublesome Problem (n = 72) | Hyperacusis as the Most Troublesome Problem (n = 26) | t | p | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| HAQ Loudness | 20.28 | 5.74 | 22.83 | 3.94 | 2.02 | 0.046 |
| HAQ Fear | 7.35 | 4.69 | 8.71 | 5.29 | 1.53 | 0.237 |
| HAQ Pain | 7.28 | 3.68 | 8.54 | 3.45 | 1.48 | 0.143 |
| HAQ global score | 34.90 | 11.70 | 40.08 | 10.41 | 1.19 | 0.057 |
| HQ | 20.88 | 8.67 | 22.88 | 9.81 | 0.95 | 0.346 |
| STAI | 47.65 | 9.17 | 47.38 | 11.11 | 0.12 | 0.903 |
| THI | 58.83 | 23.70 | 53.50 | 33.51 | 0.79 | 0.433 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raj-Koziak, D.; Gos, E.; Kutyba, J.J.; Skarzynski, P.H.; Skarzynski, H. Hyperacusis Assessment Questionnaire—A New Tool Assessing Hyperacusis in Subjects with Tinnitus. J. Clin. Med. 2023, 12, 6622. https://doi.org/10.3390/jcm12206622
Raj-Koziak D, Gos E, Kutyba JJ, Skarzynski PH, Skarzynski H. Hyperacusis Assessment Questionnaire—A New Tool Assessing Hyperacusis in Subjects with Tinnitus. Journal of Clinical Medicine. 2023; 12(20):6622. https://doi.org/10.3390/jcm12206622
Chicago/Turabian StyleRaj-Koziak, Danuta, Elżbieta Gos, Justyna Jolanta Kutyba, Piotr H. Skarzynski, and Henryk Skarzynski. 2023. "Hyperacusis Assessment Questionnaire—A New Tool Assessing Hyperacusis in Subjects with Tinnitus" Journal of Clinical Medicine 12, no. 20: 6622. https://doi.org/10.3390/jcm12206622






