Nighttime versus Fulltime Brace Treatment for Adolescent Idiopathic Scoliosis: Which Brace to Choose? A Retrospective Study on 358 Patients
Abstract
:1. Introduction
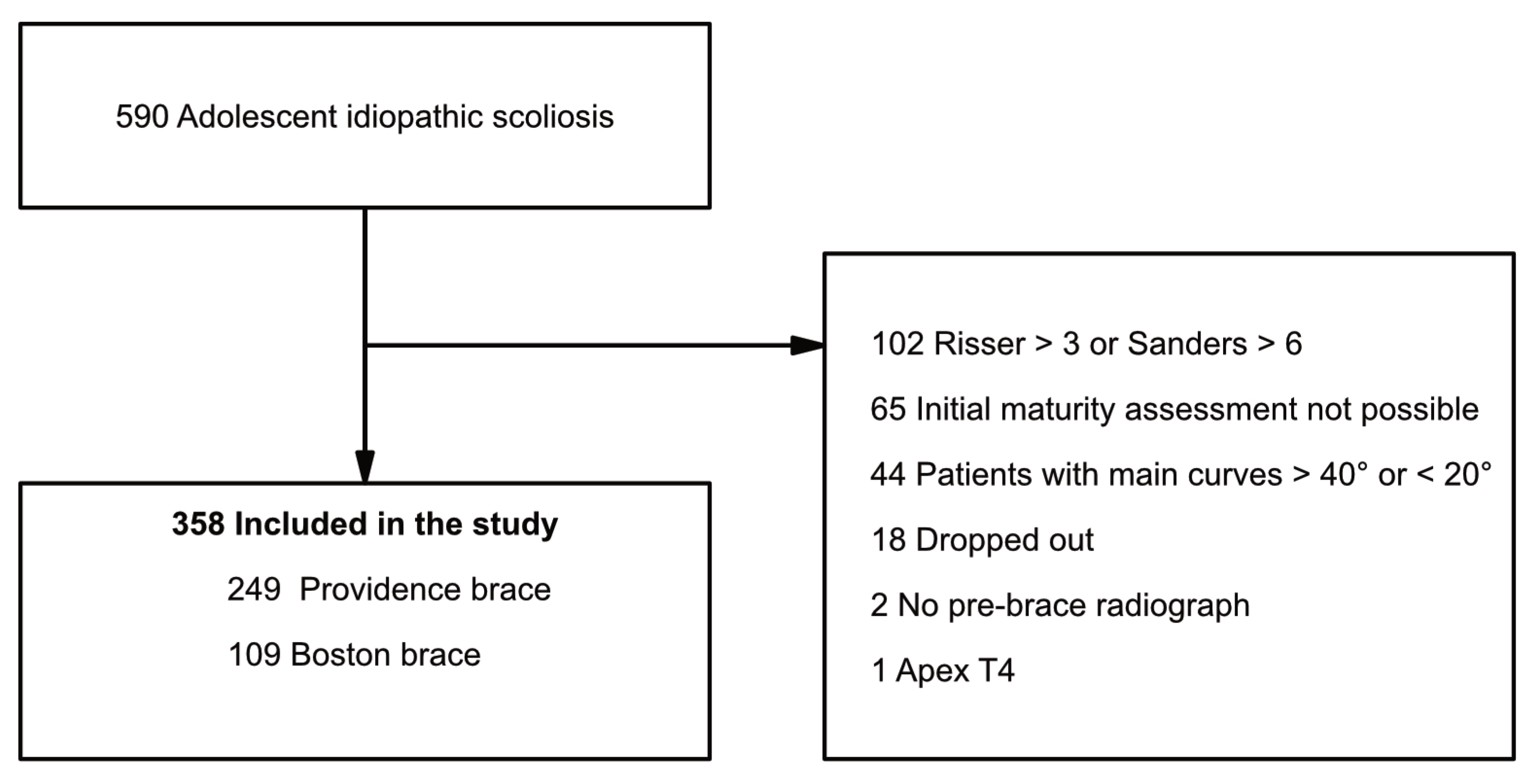
2. Materials and Methods
2.1. Study Design
2.2. Treatment Procedure
2.3. Outcome Measures and Variables
2.4. Compliance
2.5. Statistical Analyses
3. Results
3.1. Study Population
3.2. Main Outcome
3.3. Per Protocol Analysis
3.4. Secondary Outcomes
4. Discussion
4.1. Main Results
4.2. Secondary Outcomes
4.3. Limitations
4.4. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Angevine, P.D.; Deutsch, H. Idiopathic scoliosis. Neurosurgery 2008, 63, 86–93. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.A.; Wright, J.G.; Dobbs, M.B. Effects of bracing in adolescents with idiopathic scoliosis. N. Engl. J. Med. 2013, 369, 1512–1521. [Google Scholar] [CrossRef]
- Nachemson, A.L.; Peterson, L.E. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J. Bone Joint Surg. Am. 1995, 77, 815–822. [Google Scholar] [CrossRef]
- Katz, D.E.; Durrani, A.A. Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine 2001, 26, 2354–2361. [Google Scholar] [CrossRef] [PubMed]
- Antoine, L.; Nathan, D.; Laure, M.; Briac, C.; Jean-Francois, M.; Corinne, B. Compliance with night-time overcorrection bracing in adolescent idiopathic scoliosis: Result from a cohort follow-up. Med. Eng. Phys. 2020, 77, 137–141. [Google Scholar] [CrossRef]
- MacLean, W.E., Jr.; Green, N.E.; Pierre, C.B.; Ray, D.C. Stress and coping with scoliosis: Psychological effects on adolescents and their families. J. Pediatr. Orthop. 1989, 9, 257–261. [Google Scholar] [CrossRef]
- D’Amato, C.R.; Griggs, S.; McCoy, B. Nighttime bracing with the Providence brace in adolescent girls with idiopathic scoliosis. Spine 2001, 26, 2006–2012. [Google Scholar] [CrossRef]
- Price, C.T.; Scott, D.S.; Reed, F.R., Jr.; Sproul, J.T.; Riddick, M.F. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston Bending Brace: Long-term follow-up. J. Pediatr. Orthop. 1997, 17, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Bohl, D.D.; Telles, C.J.; Golinvaux, N.S.; Basques, B.A.; DeLuca, P.A.; Grauer, J.N. Effectiveness of Providence nighttime bracing in patients with adolescent idiopathic scoliosis. Orthopedics 2014, 37, e1085–e1090. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.; Murphy, J.S.; Shaw, K.A.; Cash, K.; Devito, D.P.; Schmitz, M.L. Nighttime bracing with the Providence thoracolumbosacral orthosis for treatment of adolescent idiopathic scoliosis: A retrospective consecutive clinical series. Prosthet. Orthot. Int. 2019, 43, 158–162. [Google Scholar] [CrossRef]
- Gepstein, R.; Leitner, Y.; Zohar, E.; Angel, I.; Shabat, S.; Pekarsky, I.; Friesem, T.; Folman, Y.; Katz, A.; Fredman, B. Effectiveness of the Charleston bending brace in the treatment of single-curve idiopathic scoliosis. J. Pediatr. Orthop. 2002, 22, 84–87. [Google Scholar] [CrossRef]
- Howard, A.; Wright, J.G.; Hedden, D. A comparative study of TLSO, Charleston, and Milwaukee braces for idiopathic scoliosis. Spine 1998, 23, 2404–2411. [Google Scholar] [CrossRef] [PubMed]
- Janicki, J.A.; Poe-Kochert, C.; Armstrong, D.G.; Thompson, G.H. A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: Results using the new SRS inclusion and assessment criteria for bracing studies. J. Pediatr. Orthop. 2007, 27, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.S.; Hwang, C.J.; Kim, D.J.; Kim, J.H.; Kim, Y.T.; Lee, M.Y.; Yoon, S.J.; Lee, D.H. Effectiveness of the Charleston night-time bending brace in the treatment of adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2012, 32, 368–372. [Google Scholar] [CrossRef]
- Ohrt-Nissen, S.; Lastikka, M.; Andersen, T.B.; Helenius, I.; Gehrchen, M. Conservative treatment of main thoracic adolescent idiopathic scoliosis: Full-time or nighttime bracing? J. Orthop. Surg. 2019, 27, 2309499019860017. [Google Scholar] [CrossRef]
- Simony, A.; Beuschau, I.; Quisth, L.; Jespersen, S.M.; Carreon, L.Y.; Andersen, M.O. Providence nighttime bracing is effective in treatment for adolescent idiopathic scoliosis even in curves larger than 35 degrees. Eur. Spine J. 2019, 28, 2020–2024. [Google Scholar] [CrossRef] [PubMed]
- Wiemann, J.M.; Shah, S.A.; Price, C.T. Nighttime bracing versus observation for early adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2014, 34, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Richards, B.S.; Bernstein, R.M.; D’Amato, C.R.; Thompson, G.H. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine 2005, 30, 2068–2075; discussion 2067–2076. [Google Scholar] [CrossRef]
- Emans, J.B.; Kaelin, A.; Bancel, P.; Hall, J.E.; Miller, M.E. The Boston bracing system for idiopathic scoliosis. Follow-up results in 295 patients. Spine 1986, 11, 792–801. [Google Scholar] [CrossRef]
- Sanders, J.O.; Khoury, J.G.; Kishan, S.; Browne, R.H.; Mooney, J.F., III; Arnold, K.D.; McConnell, S.J.; Bauman, J.A.; Finegold, D.N. Predicting scoliosis progression from skeletal maturity: A simplified classification during adolescence. J. Bone Joint Surg. Am. 2008, 90, 540–553. [Google Scholar] [CrossRef]
- Capek, V.; Westin, O.; Brisby, H.; Wessberg, P. Providence nighttime brace is as effective as fulltime Boston brace for female patients with adolescent idiopathic scoliosis: A retrospective analysis of a randomized cohort. N. Am. Spine Soc. J. 2022, 12, 100178. [Google Scholar] [CrossRef] [PubMed]
- Buyuk, A.F.; Truong, W.H.; Morgan, S.J.; Snyder, A.J.; Miller, D.J.; Nolin, K.K.; Smith, K.J. Is nighttime bracing effective in the treatment of adolescent idiopathic scoliosis? A meta-analysis and systematic review based on scoliosis research society guidelines. Spine Deform. 2021, 10, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Karol, L.A.; Virostek, D.; Felton, K.; Jo, C.; Butler, L. The Effect of the Risser Stage on Bracing Outcome in Adolescent Idiopathic Scoliosis. J. Bone Joint Surg. Am. 2016, 98, 1253–1259. [Google Scholar] [CrossRef] [PubMed]
- Charles, Y.P.; Canavese, F.; Dimeglio, A. Curve progression risk in a mixed series of braced and nonbraced patients with idiopathic scoliosis related to skeletal maturity assessment on the olecranon. J. Pediatr. Orthop. B 2017, 26, 240–244. [Google Scholar] [CrossRef]
- Aulisa, A.G.; Giordano, M.; Falciglia, F.; Marzetti, E.; Poscia, A.; Guzzanti, V. Correlation between compliance and brace treatment in juvenile and adolescent idiopathic scoliosis: SOSORT 2014 award winner. Scoliosis 2014, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.O.; Newton, P.O.; Browne, R.H.; Katz, D.E.; Birch, J.G.; Herring, J.A. Bracing for idiopathic scoliosis: How many patients require treatment to prevent one surgery? J. Bone Joint Surg. Am. 2014, 96, 649–653. [Google Scholar] [CrossRef]
- Morton, A.; Riddle, R.; Buchanan, R.; Katz, D.; Birch, J. Accuracy in the prediction and estimation of adherence to bracewear before and during treatment of adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2008, 28, 336–341. [Google Scholar] [CrossRef]
- Takemitsu, M.; Bowen, J.R.; Rahman, T.; Glutting, J.J.; Scott, C.B. Compliance monitoring of brace treatment for patients with idiopathic scoliosis. Spine 2004, 29, 2070–2074; discussion 2074. [Google Scholar] [CrossRef]
- Rahman, T.; Borkhuu, B.; Littleton, A.G.; Sample, W.; Moran, E.; Campbell, S.; Rogers, K.; Bowen, J.R. Electronic monitoring of scoliosis brace wear compliance. J. Child. Orthop. 2010, 4, 343–347. [Google Scholar] [CrossRef]
- Donzelli, S.; Zaina, F.; Negrini, S. In defense of adolescents: They really do use braces for the hours prescribed, if good help is provided. Results from a prospective everyday clinic cohort using thermobrace. Scoliosis 2012, 7, 12. [Google Scholar] [CrossRef]
- Miller, D.J.; Franzone, J.M.; Matsumoto, H.; Gomez, J.A.; Avendano, J.; Hyman, J.E.; Roye, D.P., Jr.; Vitale, M.G. Electronic monitoring improves brace-wearing compliance in patients with adolescent idiopathic scoliosis: A randomized clinical trial. Spine 2012, 37, 717–721. [Google Scholar] [CrossRef] [PubMed]
- Hasler, C.C.; Wietlisbach, S.; Buchler, P. Objective compliance of adolescent girls with idiopathic scoliosis in a dynamic SpineCor brace. J. Child. Orthop. 2010, 4, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Vandal, S.; Rivard, C.H.; Bradet, R. Measuring the compliance behavior of adolescents wearing orthopedic braces. Issues Compr. Pediatr. Nurs. 1999, 22, 59–73. [Google Scholar] [CrossRef] [PubMed]

| Total (n = 358) | Providence (n = 249) | Boston (n = 109) | p | Effect Size | |
|---|---|---|---|---|---|
| Age at bracing | 13.41 (1.28) 13.42 (12.53; 14.35) | 13.42 (1.32) 13.43 (12.50;14.38) | 13.41 (1.21) 13.38 (12.57; 14.28) | 0.49 | 0.003 |
| Gender | |||||
| Female | 314 (87.7%) | 215 (86.3%) | 99 (90.8%) | ||
| Male | 44 (12.3%) | 34 (13.7%) | 10 (9.2%) | 0.30 | 0.06 |
| Initial Cobb angle main curve | 31.1 (4.7) 31 (27; 35) | 30.7 (4.5) 30 (27; 34) | 32.1 (4.9) 32.5 (28; 36) | 0.006 | −0.29 |
| Delay to bracing (years) | 0.20 (0.08) 0.19 (0.15; 0.24) | 0.20 (0.06) 0.19 (0.15; 0.24) | 0.19 (0.11) 0.17 (0.13; 0.23) | 0.56 | 0.08 |
| Time spent in brace (years) * | 1.91(0.94) 1.81 (1.28; 2.42) n = 295 | 1.87 (0.90) 1.69 (1.28; 2.31) n = 195 | 2.00 (1.01) 1.98 (1.34; 2.53) n = 100 | 0.12 | −0.15 |
| Follow up after finishing bracing (years) * | 1.45 (0.73) 1.19 (1.02; 1.64) n = 295 | 1.39 (0.66) 1.15 (1.00; 1.53) n = 195 | 1.56 (0.86) 1.25 (1.04; 1.94) n = 100 | 0.045 | −0.23 |
| Initial modified Sanders stage | |||||
| 2 | 7 (2.0%) | 3 (1.2%) | 4 (3.7%) | ||
| 3 | 48 (13.4%) | 31 (12.4%) | 17 (15.6%) | ||
| 4 | 109 (30.4%) | 74 (29.7%) | 35 (32.1%) | ||
| 5 | 58 (16.2%) | 37 (14.9%) | 21 (19.3%) | ||
| 6 | 135 (37.7%) | 104 (41.8%) | 31 (28.4%) | ||
| 7 | 1 (0.3%) | 0 (0.0%) | 1 (0.9%) | 0.042 | |
| Risser 0 | 164 (45.8%) | 109 (43.8%) | 55 (50.5%) | ||
| Risser > 0 | 194 (54.2%) | 140 (56.2%) | 54 (49.5%) | 0.25 | 0.062 |
| Main curve size | |||||
| Cobb 20–29° | 142 (39.7%) | 106 (42.6%) | 36 (33.0%) | ||
| Cobb 30–40° | 216 (60.3%) | 143 (57.4%) | 73 (67%) | 0.10 | 0.089 |
| Type of curve | |||||
| MT (Lenke 1) | 169 (47.5%) | 125 (50.2%) | 44 (40.4%) | ||
| DT (Lenke 2) | 29 (8.1%) | 18 (7.5%) | 11 (10.1%) | ||
| DM (Lenke 3) | 37 (10.3%) | 22 (8.8%) | 15 (13.8%) | ||
| TM (Lenke 4) | 1 (0.3%) | 1 (0.4%) | 0 (0.0%) | ||
| TL/L (Lenke 5 and 6) | 122 (34.1%) | 83 (33.3%) | 39 (35.8%) | 0.32 | 0.11 |
| Menarche at bracing | |||||
| Pre-menarche | 173 (55.6%) | 119 (55.9%) | 54 (55.1%) | ||
| Post-menarche | 138 (44.4%) n = 311 | 94 (44.1%) n = 213 | 44 (44.9%) n = 98 | 0.90 | 0.007 |
| In-brace main curve correction (%) | 54.7 (23.8) 55.8 (38.5; 71.4) | 63.3 (20.2) 64.0 (50.0; 76.7) | 34.9 (19.2) 33.3 (19.2; 46.9) | <0.0001 | −1.4 |
| Providence | Boston | Adjusted Analysis | |||||
|---|---|---|---|---|---|---|---|
| Mean D (95% CI) | p Value | OR (95% CI) | p Value * | Effect Size ** | |||
| Total, n | 249 | 109 | |||||
| Failure, n | 135 (54.2%) | 45 (41.3%) | 12.9% (1.8, 24.0) | 0.029 | 1.91 (1.19, 3.05) | 0.007 | 0.12 |
| Success, n | 114 (45.8%) | 64 (58.7%) | −12.9% (−24.0, −1.8) | ||||
| Surgery | |||||||
| Yes | 72 (28.9%) | 25 (22.9%) | 6% (−3.7,15.7) | 0.30 | 1.93 (1.08, 3.42) | 0.025 | 0.06 |
| No | 177 (71.1%) | 84 (77.1%) | −6% (−15.7,3.7) | ||||
| Providence | Boston | |||||||
|---|---|---|---|---|---|---|---|---|
| Crude Mean (SD) Median (IQR) | Adjusted Means * (95% CI) | Crude Mean (SD) Median (IQR) | Adjusted Means * (95% CI) | p | Adjusted p * | Difference between Groups Adjusted Means (95% CI) | Effect Size ** | |
| Cobb angle change (°) of main curve | 7.3 (9.3) 6.0 (0.5; 12.5) n = 249 | 7.4 (6.2, 8.5) n = 249 | 4.5 (9.1) 3.0 (−2; 10) n = 109 | 4.3 (2.6, 6.0) n = 109 | 0.009 | 0.002 | 3.1 (1.1, 5.1) | 0.30 |
| Failure SRS Rates | Adjusted Increase in Cobb Angle | |||||||
|---|---|---|---|---|---|---|---|---|
| Selected Subgroup | Brace Group | Proportion of Failures | Mean Difference between Groups [95% CI] | OR [95% CI] * | p * | Within Groups Mean (°) [95% CI] ** | Difference between Groups Adjusted Means [95% CI] ** | p ** |
| Females | Providence n = 215 | 117 (54.4%) | 15.0% [3.3, 24.7] | 2.0 [1.2, 3.3] | 0.005 | 7.1 (5.9, 8.3) | 3.2 (1.1, 5.2) | 0.002 |
| Boston n = 99 | 39 (39.4%) | 3.9 (2.2, 5.7) | ||||||
| Males | Providence n = 34 | 18 (52.9%) | −7.1% [−41.8, 27.6] | 1.1 [0.2, 5.3] | 0.88 | 9.0 (5.2, 12.7) | 1.3 (−8.3, 10.9) | 0.79 |
| Boston n = 10 | 6 (60.0%) | 7.7 (0.3, 15.0) | ||||||
| Pre-menarche | Providence n = 119 | 78 (65.5%) | 17.4% [1.6, 33.2] | 2.2 [1.1, 4.3] | 0.02 | 9.8 (8.1, 11.5) | 4.8 (1.8, 7.8) | 0.002 |
| Boston n = 54 | 26 (48.1%) | 5.0 (2.4, 7.6) | ||||||
| Post-menarche | Providence n = 94 | 38 (40.4%) | 13.1% [−3.4, 29.6] | 2.0 [0.9, 4.4] | 0.095 | 3.7 (2.3, 5.1) | 1.3 (−1.5, 4.1) | 0.34 |
| Boston n = 44 | 12 (27.3%) | 2.4 (0.3, 4.5) | ||||||
| Thoracic curve | Providence n = 155 | 96 (61.9%) | 18.0% [3.8, 32.2] | 2.4 [1.3, 4.3] | 0.005 | 8.8 (7.3, 10.4) | 3.6 (0.9, 6.2) | 0.008 |
| Boston n = 66 | 29 (43.9%) | 5.3 (3.0, 7.6) | ||||||
| Lumbar curve | Providence n = 94 | 39 (41.5%) | 4.3% [−13.2, 21.8] | 1.3 [0.6, 2.8] | 0.47 | 4.9 (3.3, 6.5) | 2.2 (−0.8, 5.1) | 0.15 |
| Boston n = 43 | 16 (37.2%) | 2.8 (0.4, 5.2) | ||||||
| Curves 20–29° | Providence n = 106 | 55 (51.9%) | 13.0% (−5.6, 31.6) | 2.3 (1.0, 5.4) | 0.05 | 8.1 (6.3, 9.9) | 3.8 (0.3, 7.3) | 0.034 |
| Boston n = 36 | 14 (38.9%) | 4.3 (1.1, 7.4) | ||||||
| Curves 30–40° | Providence n = 143 | 80 (55.9%) | 13.4% (−0.6, 27.4) | 1.9 (1.04, 3.3) | 0.036 | 6.9 (5.4, 8.3) | 2.7 (0.2, 5.2) | 0.035 |
| Boston n = 73 | 31 (42.5%) | 4.2 (2.2, 6.2) | ||||||
| Providence (n = 243) | Boston (n = 109) | p | |
|---|---|---|---|
| Compliance | |||
| Excellent | 180 (74.1%) | 60 (55.0%) | |
| Good | 32 (13.2%) | 15 (13.8%) | |
| Fair | 15 (6.2%) | 18 (16.5%) | |
| Poor | 16 (6.6%) | 16 (14.7%) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capek, V.; Baranto, A.; Brisby, H.; Westin, O. Nighttime versus Fulltime Brace Treatment for Adolescent Idiopathic Scoliosis: Which Brace to Choose? A Retrospective Study on 358 Patients. J. Clin. Med. 2023, 12, 7684. https://doi.org/10.3390/jcm12247684
Capek V, Baranto A, Brisby H, Westin O. Nighttime versus Fulltime Brace Treatment for Adolescent Idiopathic Scoliosis: Which Brace to Choose? A Retrospective Study on 358 Patients. Journal of Clinical Medicine. 2023; 12(24):7684. https://doi.org/10.3390/jcm12247684
Chicago/Turabian StyleCapek, Vojtech, Adad Baranto, Helena Brisby, and Olof Westin. 2023. "Nighttime versus Fulltime Brace Treatment for Adolescent Idiopathic Scoliosis: Which Brace to Choose? A Retrospective Study on 358 Patients" Journal of Clinical Medicine 12, no. 24: 7684. https://doi.org/10.3390/jcm12247684
APA StyleCapek, V., Baranto, A., Brisby, H., & Westin, O. (2023). Nighttime versus Fulltime Brace Treatment for Adolescent Idiopathic Scoliosis: Which Brace to Choose? A Retrospective Study on 358 Patients. Journal of Clinical Medicine, 12(24), 7684. https://doi.org/10.3390/jcm12247684






