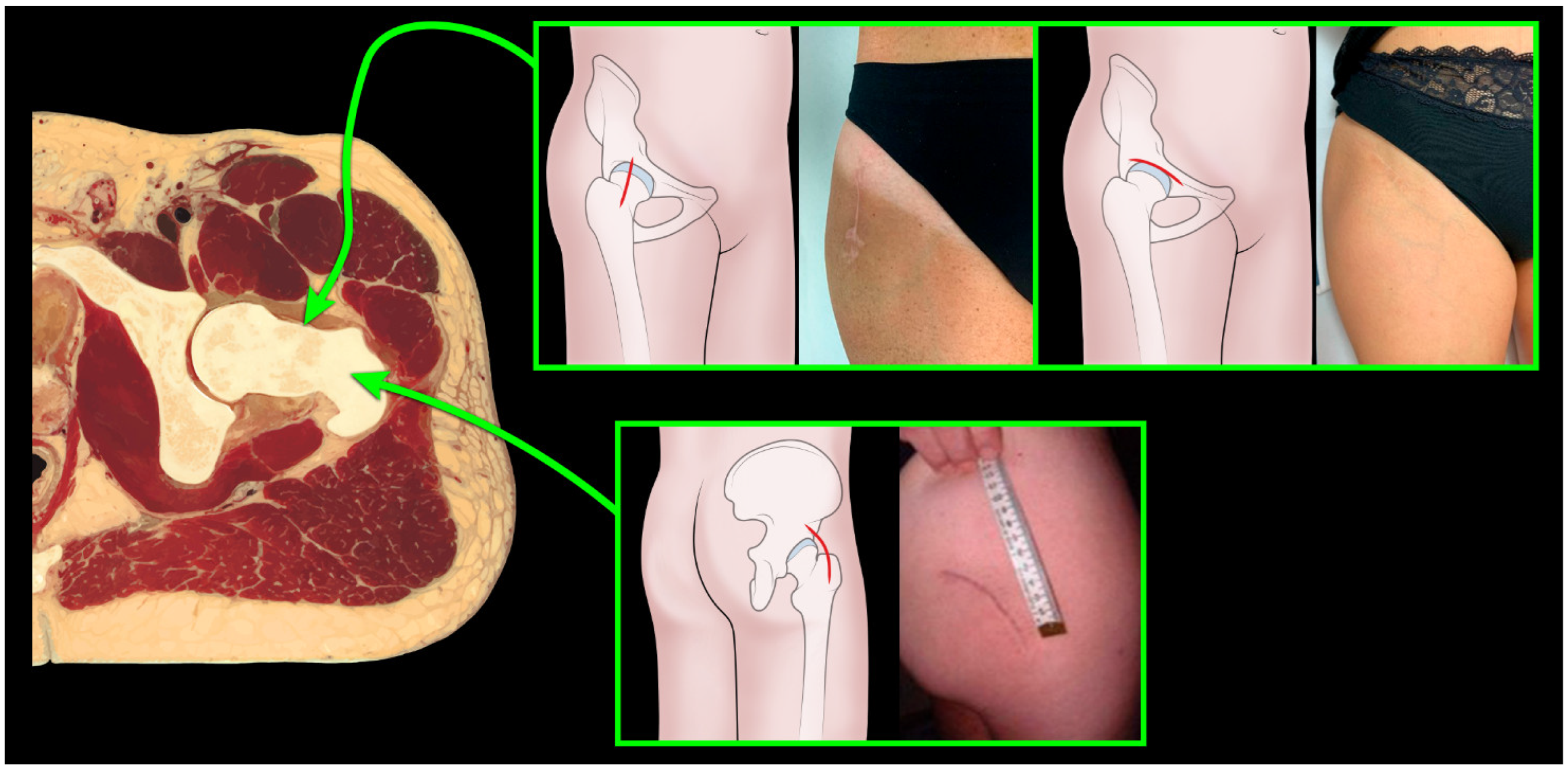
Aesthetic Results, Functional Outcome and Radiographic Analysis in THA by Direct Anterior, Bikini and Postero-Lateral Approach: Is It Worth the Hassle?
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Patient and Observer Scar Assessment Scale (POSAS)
2.2. Radiological Evaluation
2.3. Statistical Analysis
3. Results
3.1. Patients’ Demographics and Characteristics
3.2. Radiographic Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Putananon, C.; Tuchinda, H.; Arirachakaran, A.; Wongsak, S.; Narinsorasak, T.; Kongtharvonskul, J. Comparison of Direct Anterior, Lateral, Posterior and Posterior-2 Approaches in Total Hip Arthroplasty: Network Meta-Analysis. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 255–267. [Google Scholar] [CrossRef] [PubMed]
- Nambiar, M.; Cheng, T.E.; Onggo, J.R.; Maingard, J.; Troupis, J.; Pope, A.; Armstrong, M.S.; Singh, P.J. No Difference in Functional, Radiographic, and Survivorship Outcomes Between Direct Anterior or Posterior Approach THA: 5-Year Results of a Randomized Trial. Clin. Orthop. Relat. Res. 2021, 479, 2621–2629. [Google Scholar] [CrossRef] [PubMed]
- Wojciechowski, P.; Kusz, D.; Kopeć, K.; Borowski, M. Minimally invasive approaches in total hip arthroplasty. Ortop. Traumatol. Rehabil. 2007, 9, 1–7. [Google Scholar] [PubMed]
- Rachbauer, F.; Nogler, M.; Mayr, E.; Krismer, M. Minimally Invasive Single-Incision Anterior Approach for Total Hip Arthroplasty-Early Results. In Minimally Invasive Total Joint Arthroplasty; Hozack, W.J., Krismer, M., Nogler, M., Bonutti, P.M., Rachbauer, F., Schaffer, J.L., Donnelly, W.J., Eds.; Springer: Berlin/Heidelberg, Germany, 2004; pp. 54–59. ISBN 978-3-642-59298-0. [Google Scholar]
- Post, Z.D.; Orozco, F.; Diaz-Ledezma, C.; Hozack, W.J.; Ong, A. Direct Anterior Approach for Total Hip Arthroplasty: Indications, Technique, and Results. J. Am. Acad. Orthop. Surg. 2014, 22, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Sculco, T.P.; Jordan, L.C. The Mini-Incision Approach to Total Hip Arthroplasty. Instr. Course Lect. 2004, 53, 141–147. [Google Scholar] [PubMed]
- Corten, K.; Holzapfel, B.M. Direct Anterior Approach for Total Hip Arthroplasty Using the “Bikini Incision”. Oper. Orthop. Traumatol. 2021, 33, 318–330. [Google Scholar] [CrossRef]
- Butler, J.; Singleton, A.; Miller, R.; Morse, B.; Naylor, B.; DeCook, C. Bikini Incision vs. Longitudinal Incision for Anterior Total Hip Arthroplasty: A Systematic Review. Arthroplast. Today 2022, 17, 1–8. [Google Scholar] [CrossRef]
- Faldini, C.; Mazzotti, A.; Perna, F.; Stefanini, N.; Panciera, A.; Pilla, F.; Ruffilli, A.; Neonakis, E.M.; Traina, F. Modified Minimally Invasive Direct Anterior Approach through a Bikini Incision for Total Hip Arthroplasty: Technique and Results in Young Female Patients. J. Biol. Regul. Homeost. Agents 2017, 31, 83–89. [Google Scholar]
- Dettoni, F.; Pellegrino, P.; La Russa, M.R.; Bonasia, D.E.; Blonna, D.; Bruzzone, M.; Castoldi, F.; Rossi, R. Validation and Cross Cultural Adaptation of the Italian Version of the Harris Hip Score. Hip Int. 2015, 25, 91–97. [Google Scholar] [CrossRef]
- Vercelli, S.; Ferriero, G.; Bravini, E.; Stissi, V.; Ciceri, M.; Rossetti, S.; Bianchi, S.; Sartorio, F. Cross-Cultural Adaptation, Reproducibility and Validation of the Italian Version of the Patient and Observer Scar Assessment Scale (POSAS). Int. Wound J. 2017, 14, 1262–1268. [Google Scholar] [CrossRef]
- Leunig, M.; Faas, M.; von Knoch, F.; Naal, F.D. Skin Crease ‘Bikini’ Incision for Anterior Approach Total Hip Arthroplasty: Surgical Technique and Preliminary Results. Clin. Orthop. Relat. Res. 2013, 471, 2245–2252. [Google Scholar] [CrossRef] [Green Version]
- Leunig, M.; Hutmacher, J.E.; Ricciardi, B.F.; Impellizzeri, F.M.; Rüdiger, H.A.; Naal, F.D. Skin Crease “bikini” Incision for the Direct Anterior Approach in Total Hip Arthroplasty: A Two- to Four-Year Comparative Study in 964 Patients. Bone Jt. J. 2018, 100, 853–861. [Google Scholar] [CrossRef]
- Wang, Q.; Yue, Y.; Yang, Z.; Chen, L.; Li, Q.; Kang, P. Comparison of Postoperative Outcomes Between Traditional Longitudinal Incision and Bikini Incision in Total Hip Arthroplasty via Direct Anterior Approach: A Randomized Controlled Trial. J. Arthroplast. 2021, 36, 222–230. [Google Scholar] [CrossRef]
- Manrique, J.; Paskey, T.; Tarabichi, M.; Restrepo, C.; Foltz, C.; Hozack, W.J. Total Hip Arthroplasty Through the Direct Anterior Approach Using a Bikini Incision Can Be Safely Performed in Obese Patients. J. Arthroplast. 2019, 34, 1723–1730. [Google Scholar] [CrossRef]
- Islam, R.; Lanting, B.; Somerville, L.; Hunter, S.W. Evaluating the Functional and Psychological Outcomes Following Periprosthetic Femoral Fracture After Total Hip Arthroplasty. Arthroplast. Today 2022, 18, 57–62. [Google Scholar] [CrossRef]
- Göbel, P. Financing of Complex Replacement Surgery. Orthopadie 2022, 51, 646–651. [Google Scholar] [CrossRef]
- González-Martín, D.; Pais-Brito, J.L.; González-Casamayor, S.; Guerra-Ferraz, A.; González-Pérez, J.M.; Jiménez-Sosa, A.; Herrera-Pérez, M. Economic Impact of Periprosthetic Hip Fractures. Rev. Esp. Cir. Ortop. Traumatol. 2022, 66, T59–T66. [Google Scholar] [CrossRef]
- Crutcher, J.P.; Tompkins, G.; Rollier, G.; Sypher, K.; Valderrama, R.; Duwelius, P.J. The Economic Impact of Lower Extremity Periprosthetic Fractures in a Large Hospital System. J. Arthroplast. 2022, 37, S439–S443. [Google Scholar] [CrossRef]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after Total Hip-Replacement Arthroplasties. JBJS 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Dorr, L.; Callaghan, J. Death of the Lewinnek “Safe Zone”. J. Arthroplast. 2019, 34, 1–2. [Google Scholar] [CrossRef]
- Jia, F.; Guo, B.; Xu, F.; Hou, Y.; Tang, X.; Huang, L. A Comparison of Clinical, Radiographic and Surgical Outcomes of Total Hip Arthroplasty between Direct Anterior and Posterior Approaches: A Systematic Review and Meta-Analysis. HIP Int. 2019, 29, 584–596. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J.A.; Deshmukh, A.J.; Rathod, P.A.; Greiz, M.L.; Deshmane, P.P.; Hepinstall, M.S.; Ranawat, A.S. Does the Direct Anterior Approach in THA Offer Faster Rehabilitation and Comparable Safety to the Posterior Approach? Clin. Orthop. Relat. Res. 2014, 472, 455–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| DAA | BK | PL | |
|---|---|---|---|
| Number of patients | 58 | 52 | 50 |
| Age at surgery (years) | 59.8 | 56.9 | 60.2 |
| BMI | 25.6 ± 5.32 | 24.5 ± 2.7 | 27 ± 4.1 |
| Surgical Time (minutes) | 87.76 ± 22.1 | 84.3 ± 12.8 | 87.37 ± 22.1 |
| Intradermal suture | 63.8% | 69% | 64% |
| Hospitalization time (days) | 10 ± 3 | 8.5 ± 1.5 | 10 ± 2 |
| HHS pre-surgery | 49.9 ± 17.3 | 48.9 ± 9 | 52.3 ± 15 |
| HHS post-surgery | 92.8 ± 7.48 | 92.8 ± 9.53 | 92.7 ± 5.2 |
| Complications | DAA | BK | PL | Total |
|---|---|---|---|---|
| Femoral-cutaneous nerve apraxia | - | 3/52 (5.77%) | - | 3/160 (1.87%) |
| Intraoperative femur fracture | - | - | 1/50 (2%) | 1/160 (0.62%) |
| Dislocation | 1/58 (1.7%) | - | - | 1/160 (0.62%) |
| Aseptic mobilization | - | 1/52 (1.92%) | - | 1/160 (0.62%) |
| Total | 2/93 (1.7%) | 4/52 (7.69%) | 1/50 (2%) | 7/160 (4.37%) |
| POSAS Patient Scale Results | DAA | BK | PL |
|---|---|---|---|
| Pain | 1.2 | 1.9 | 1.5 |
| Itching | 1.3 | 2.4 | 1.5 |
| Colour | 3.3 | 1.9 | 2.5 |
| Stiffness | 2.2 | 1.3 | 2.4 |
| Thickness | 2.5 | 1.4 | 2.5 |
| Irregular | 1.5 | 1.5 | 1.5 |
| Opinion | 2.1 | 1.3 | 2.6 |
| Total | 14.1 | 11.7 | 14.5 |
| Cup Inclination | DAA | BK | PL |
|---|---|---|---|
| Mean | 35.3 | 38.4 | 37.8 |
| Standard deviation | 7.1 | 4.2 | 9.6 |
| Minimum | 25 | 27 | 23 |
| Maximum | 49 | 48 | 61 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Martino, A.; Brunello, M.; Rossomando, V.; Pederiva, D.; Schilardi, F.; Stefanini, N.; Geraci, G.; Faldini, C. Aesthetic Results, Functional Outcome and Radiographic Analysis in THA by Direct Anterior, Bikini and Postero-Lateral Approach: Is It Worth the Hassle? J. Clin. Med. 2023, 12, 1072. https://doi.org/10.3390/jcm12031072
Di Martino A, Brunello M, Rossomando V, Pederiva D, Schilardi F, Stefanini N, Geraci G, Faldini C. Aesthetic Results, Functional Outcome and Radiographic Analysis in THA by Direct Anterior, Bikini and Postero-Lateral Approach: Is It Worth the Hassle? Journal of Clinical Medicine. 2023; 12(3):1072. https://doi.org/10.3390/jcm12031072
Chicago/Turabian StyleDi Martino, Alberto, Matteo Brunello, Valentino Rossomando, Davide Pederiva, Francesco Schilardi, Niccolò Stefanini, Giuseppe Geraci, and Cesare Faldini. 2023. "Aesthetic Results, Functional Outcome and Radiographic Analysis in THA by Direct Anterior, Bikini and Postero-Lateral Approach: Is It Worth the Hassle?" Journal of Clinical Medicine 12, no. 3: 1072. https://doi.org/10.3390/jcm12031072
APA StyleDi Martino, A., Brunello, M., Rossomando, V., Pederiva, D., Schilardi, F., Stefanini, N., Geraci, G., & Faldini, C. (2023). Aesthetic Results, Functional Outcome and Radiographic Analysis in THA by Direct Anterior, Bikini and Postero-Lateral Approach: Is It Worth the Hassle? Journal of Clinical Medicine, 12(3), 1072. https://doi.org/10.3390/jcm12031072








