Association between Early Immune-Related Adverse Events and Survival in Patients Treated with PD-1/PD-L1 Inhibitors
Abstract
1. Background
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Quality Assessment and Statistical Analyses
3. Results
3.1. Literature Search
3.2. Study Characteristics
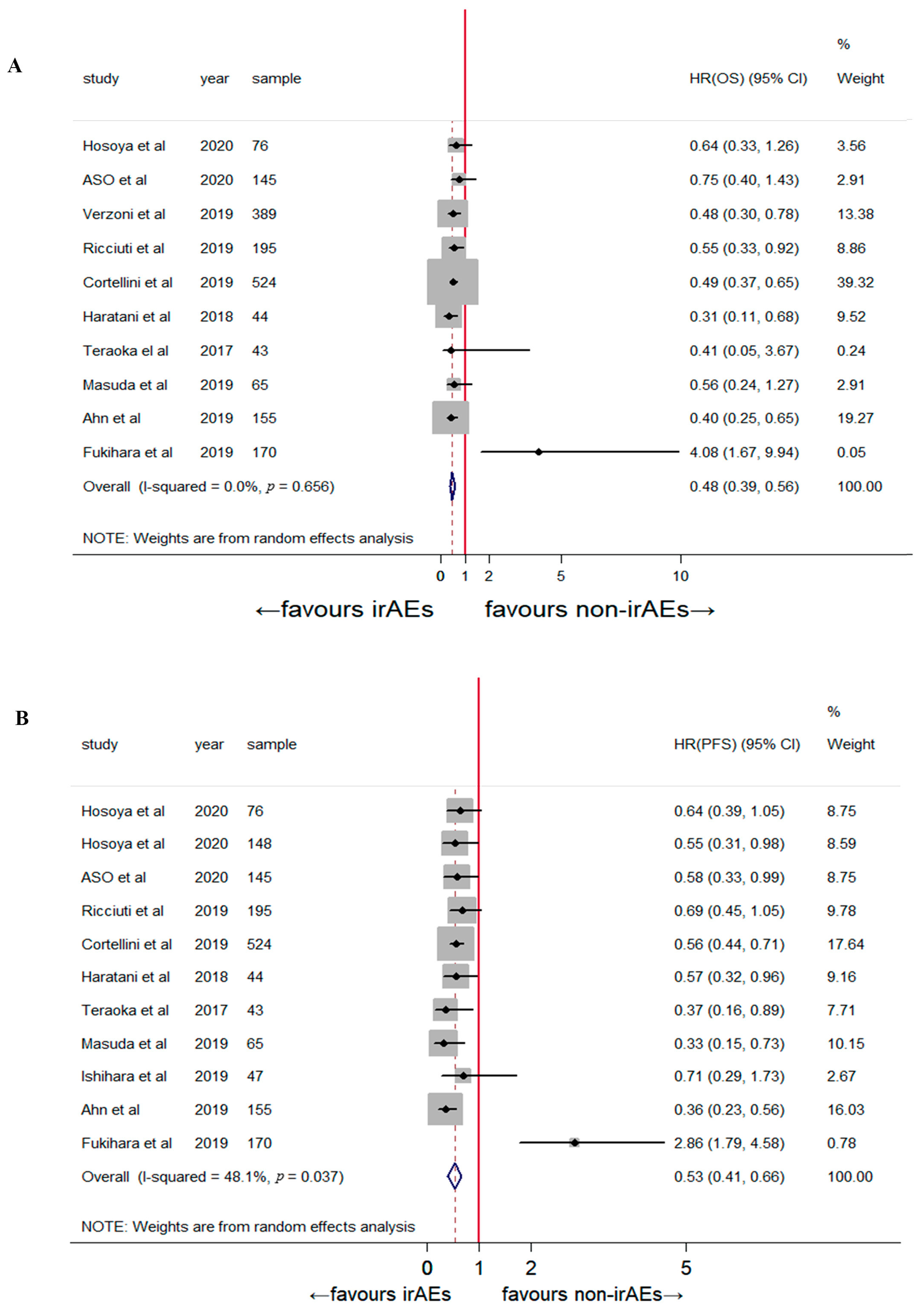
3.3. Correlation of Early irAEs and Treatment Efficacy
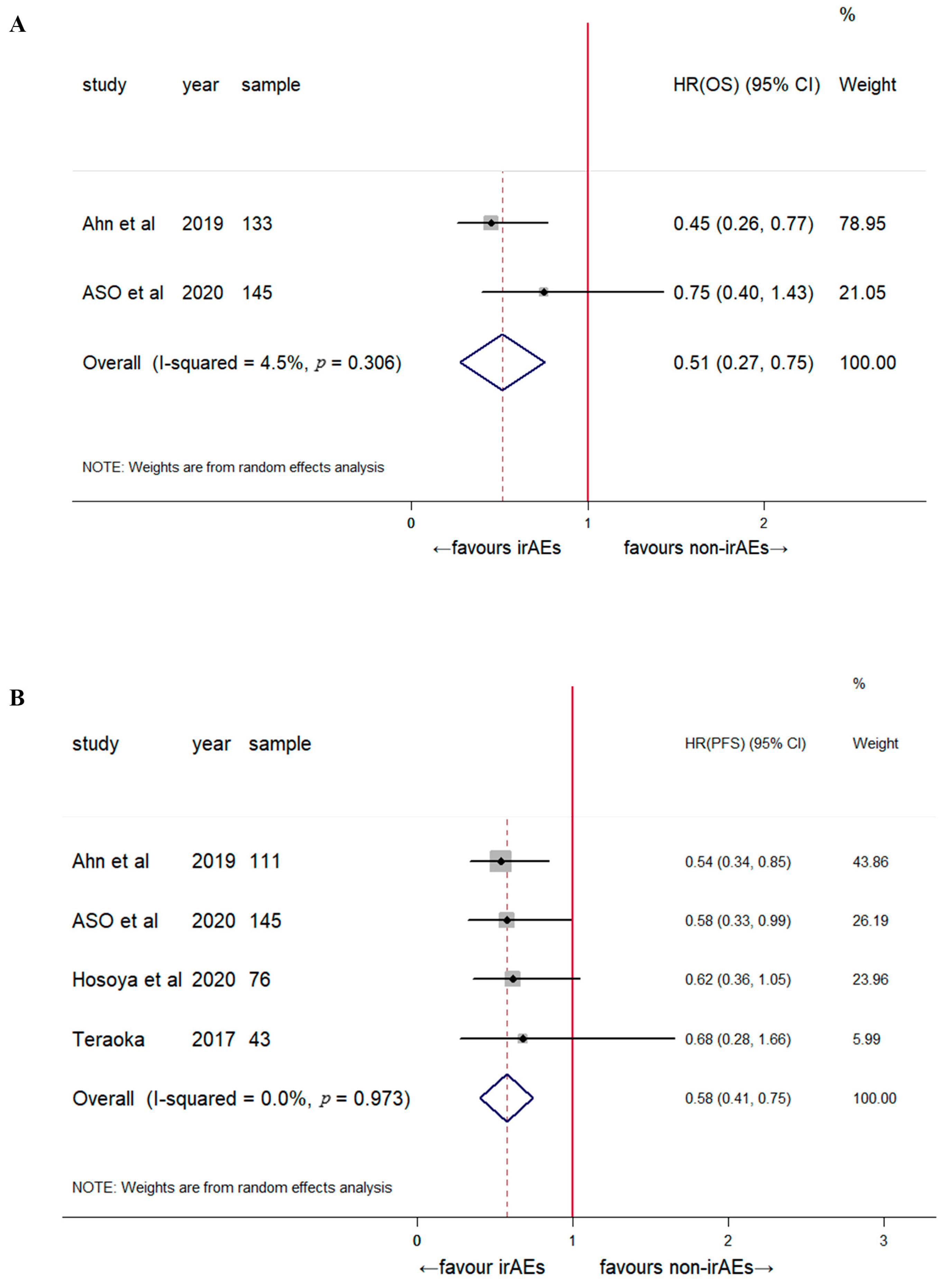
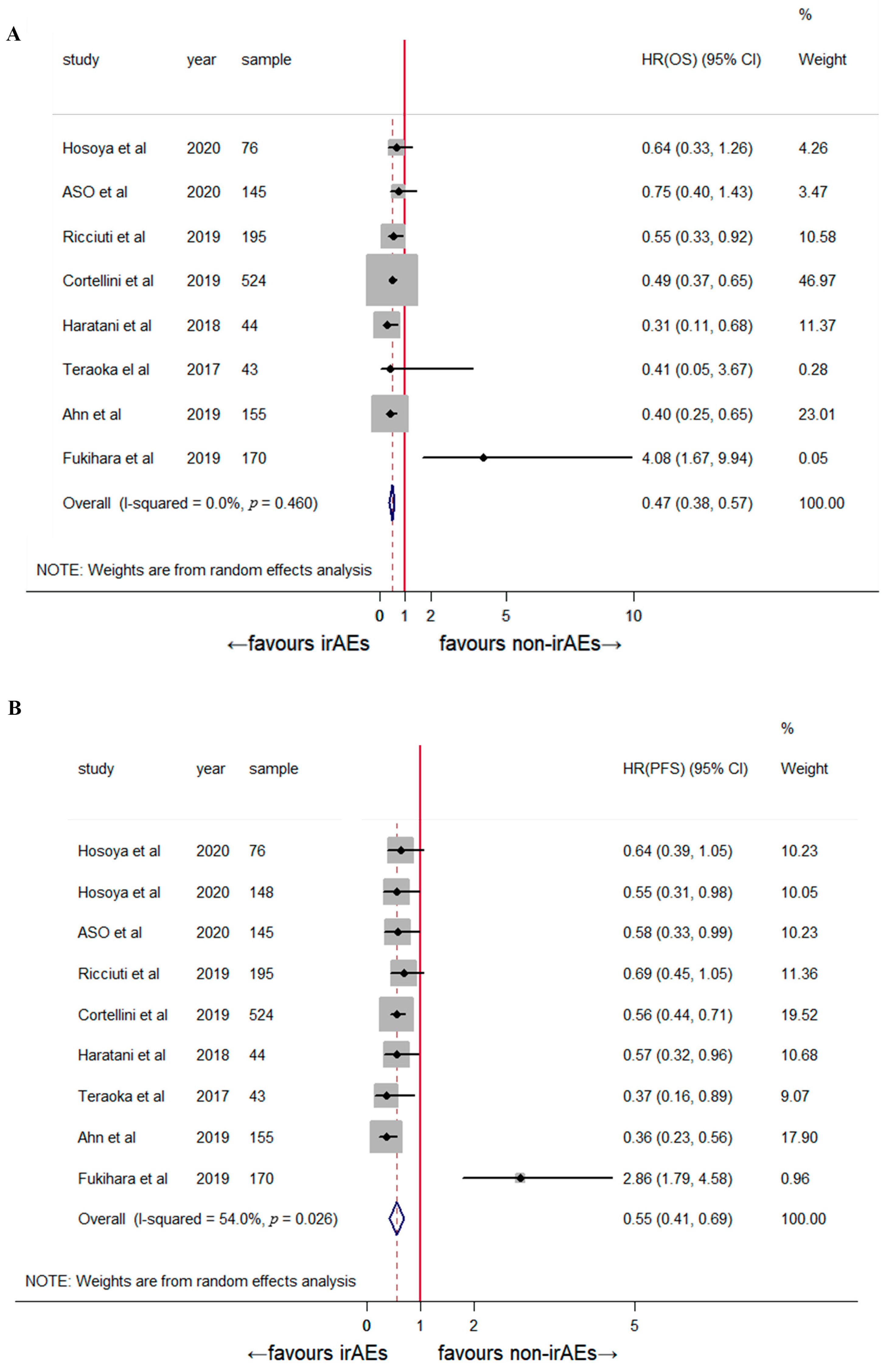
3.4. Subgroup and Sensitivity Analyses
3.5. Publication Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Myers G: Immune-related adverse events of immune checkpoint inhibitors: A brief review. Curr. Oncol. 2018, 25, 342–347. [CrossRef] [PubMed]
- Aso, M.; Toi, Y.; Sugisaka, J.; Aiba, T.; Kawana, S.; Saito, R.; Ogasawara, T.; Tsurumi, K.; Ono, K.; Shimizu, H.; et al. Association between Skin Reaction and Clinical Benefit in Patients Treated with Anti-Programmed Cell Death 1 Monotherapy for Advanced Non-Small Cell Lung Cancer. Oncologist 2020, 25, e536–e544. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.; Hwang, S.J.E.; Byth, K.; Kyaw, M.; Carlino, M.S.; Chou, S.; Fernandez-Penas, P. Survival and prognosis of individuals receiving programmed cell death 1 inhibitor with and without immunologic cutaneous adverse events. J. Am. Acad. Dermatol. 2020, 82, 311–316. [Google Scholar] [CrossRef]
- Das, S.; Ciombor, K.K.; Haraldsdottir, S.; Pumpalova, Y.; Sahin, I.H.; Pineda, G.; Shyr, Y.; Lin, E.P.; Hsu, C.Y.; Chu, S.K.; et al. Immune-Related Adverse Events and Immune Checkpoint Inhibitor Efficacy in Patients with Gastrointestinal Cancer with Food and Drug Administration-Approved Indications for Immunotherapy. Oncologist 2020, 25, 669–679. [Google Scholar] [CrossRef]
- Ezponda Casajús, A.; Calvo Imirizaldu, M.; de Torres Tajes, J.P.; García-Baizán, A.; Castañón Álvarez, E.; Cano Rafart, D.; Vivas Pérez, I.; Bastarrika Alemañ, G. Immune-related adverse events as predictors of response in cancer patients undergoing immunotherapy. Radiologia 2020, 62, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Colen, R.R.; Bilen, M.A.; Hess, K.R.; Hajjar, J.; Suarez-Almazor, M.E.; Alshawa, A.; Hong, D.S.; Tsimberidou, A.; Janku, F.; et al. Incidence of immune-related adverse events and its association with treatment outcomes: The MD Anderson Cancer Center experience. Investig. New Drugs 2018, 36, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Grangeon, M.; Tomasini, P.; Chaleat, S.; Jeanson, A.; Souquet-Bressand, M.; Khobta, N.; Bermudez, J.; Trigui, Y.; Greillier, L.; Blanchon, M.; et al. Association between Immune-related Adverse Events and Efficacy of Immune Checkpoint Inhibitors in Non-small-cell Lung Cancer. Clin. Lung Cancer 2019, 20, 201–207. [Google Scholar] [CrossRef]
- Haratani, K.; Hayashi, H.; Nakagawa, K. Association of immune-related adverse events with immune checkpoint inhibitor efficacy: Real or imaginary? BMC Med. 2020, 18, 111. [Google Scholar] [CrossRef]
- Das, S.; Johnson, D.B. Immune-related adverse events and anti-tumor efficacy of immune checkpoint inhibitors. J. Immunother. Cancer 2019, 7, 306. [Google Scholar] [CrossRef]
- Zhou, X.; Yao, Z.; Yang, H.; Liang, N.; Zhang, X.; Zhang, F. Are immune-related adverse events associated with the efficacy of immune checkpoint inhibitors in patients with cancer? A systematic review and meta-analysis. BMC Med. 2020, 18, 87. [Google Scholar] [CrossRef]
- Park, R.; Lopes, L.; Saeed, A. Anti-PD-1/L1-associated immune-related adverse events as harbinger of favorable clinical outcome: Systematic review and meta-analysis. Clin. Transl. Oncol. 2020, 23, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Grizzi, G.; Ghidini, M.; Ghidini, A.; Ratti, M.; Panni, S.; Cabiddu, M.; Ghilardi, M.; Borgonovo, K.; Parati, M.C.; et al. Immune-related Adverse Events and Survival in Solid Tumors Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. J. Immunother. 2020, 43, 1–7. [Google Scholar] [CrossRef]
- Cortellini, A.; Chiari, R.; Ricciuti, B.; Metro, G.; Perrone, F.; Tiseo, M.; Bersanelli, M.; Bordi, P.; Santini, D.; Giusti, R.; et al. Correlations between the Immune-related Adverse Events Spectrum and Efficacy of Anti-PD1 Immunotherapy in NSCLC Patients. Clin. Lung Cancer 2019, 20, 237–247.e231. [Google Scholar] [CrossRef] [PubMed]
- Teraoka, S.; Fujimoto, D.; Morimoto, T.; Kawachi, H.; Ito, M.; Sato, Y.; Nagata, K.; Nakagawa, A.; Otsuka, K.; Uehara, K.; et al. Early Immune-Related Adverse Events and Association with Outcome in Advanced Non–Small Cell Lung Cancer Patients Treated with Nivolumab: A Prospective Cohort Study. J. Thorac. Oncol. 2017, 12, 1798–1805. [Google Scholar] [CrossRef] [PubMed]
- Hosoya, K.; Fujimoto, D.; Morimoto, T.; Kumagai, T.; Tamiya, A.; Taniguchi, Y.; Yokoyama, T.; Ishida, T.; Hirano, K.; Matsumoto, H.; et al. Association between Early Immune-related Adverse Events and Clinical Outcomes in Patients with Non–Small Cell Lung Cancer Treated with Immune Checkpoint Inhibitors. Clin. Lung Cancer 2020, 21, e315–e328. [Google Scholar] [CrossRef]
- Ahn, B.C.; Pyo, K.H.; Xin, C.F.; Jung, D.; Shim, H.S.; Lee, C.Y.; Park, S.Y.; Yoon, H.I.; Hong, M.H.; Cho, B.C.; et al. Comprehensive analysis of the characteristics and treatment outcomes of patients with non-small cell lung cancer treated with anti-PD-1 therapy in real-world practice. J. Cancer Res. Clin. Oncol. 2019, 145, 1613–1623. [Google Scholar] [CrossRef]
- Fukihara, J.; Sakamoto, K.; Koyama, J.; Ito, T.; Iwano, S.; Morise, M.; Ogawa, M.; Kondoh, Y.; Kimura, T.; Hashimoto, N.; et al. Prognostic Impact and Risk Factors of Immune-Related Pneumonitis in Patients with Non-Small-Cell Lung Cancer Who Received Programmed Death 1 Inhibitors. Clin. Lung Cancer 2019, 20, 442–450.e444. [Google Scholar] [CrossRef]
- Ishihara, H.; Takagi, T.; Kondo, T.; Homma, C.; Tachibana, H.; Fukuda, H.; Yoshida, K.; Iizuka, J.; Kobayashi, H.; Okumi, M.; et al. Association between immune-related adverse events and prognosis in patients with metastatic renal cell carcinoma treated with nivolumab. Urol. Oncol. 2019, 37, e321–e355. [Google Scholar] [CrossRef]
- Ksienski, D.; Wai, E.S.; Croteau, N.; Fiorino, L.; Brooks, E.; Poonja, Z.; Fenton, D.; Geller, G.; Glick, D.; Lesperance, M. Efficacy of Nivolumab and Pembrolizumab in Patients with Advanced Non-Small-Cell Lung Cancer Needing Treatment Interruption Because of Adverse Events: A Retrospective Multicenter Analysis. Clin. Lung Cancer 2019, 20, e97–e106. [Google Scholar] [CrossRef]
- Masuda, K.; Shoji, H.; Nagashima, K.; Yamamoto, S.; Ishikawa, M.; Imazeki, H.; Aoki, M.; Miyamoto, T.; Hirano, H.; Honma, Y.; et al. Correlation between immune-related adverse events and prognosis in patients with gastric cancer treated with nivolumab. BMC Cancer 2019, 19, 974. [Google Scholar] [CrossRef]
- Ricciuti, B.; Genova, C.; De Giglio, A.; Bassanelli, M.; Dal Bello, M.G.; Metro, G.; Brambilla, M.; Baglivo, S.; Grossi, F.; Chiari, R. Impact of immune-related adverse events on survival in patients with advanced non-small cell lung cancer treated with nivolumab: Long-term outcomes from a multi-institutional analysis. J. Cancer Res. Clin. Oncol. 2019, 145, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Verzoni, E.; Cartenì, G.; Cortesi, E.; Giannarelli, D.; De Giglio, A.; Sabbatini, R.; Buti, S.; Rossetti, S.; Cognetti, F.; Rastelli, F.; et al. Real-world efficacy and safety of nivolumab in previously-treated metastatic renal cell carcinoma, and association between immune-related adverse events and survival: The Italian expanded access program. J. Immunother. Cancer 2019, 7, 99. [Google Scholar] [CrossRef] [PubMed]
- Haratani, K.; Hayashi, H.; Chiba, Y.; Kudo, K.; Yonesaka, K.; Kato, R.; Kaneda, H.; Hasegawa, Y.; Tanaka, K.; Takeda, M.; et al. Association of Immune-Related Adverse Events with Nivolumab Efficacy in Non-Small-Cell Lung Cancer. JAMA Oncol. 2018, 4, 374–378. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Parmar, M.K.; Torri, V.; Stewart, L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat. Med. 1998, 17, 2815–2834. [Google Scholar] [CrossRef]
- Giobbie-Hurder, A.; Gelber, R.D.; Regan, M.M. Challenges of guarantee-time bias. J. Clin. Oncol. 2013, 31, 2963–2969. [Google Scholar] [CrossRef] [PubMed]
- Yoest, J.M. Clinical features, predictive correlates, and pathophysiology of immune-related adverse events in immune checkpoint inhibitor treatments in cancer: A short review. Immunotargets Ther. 2017, 6, 73–82. [Google Scholar] [CrossRef]
- Berner, F.; Bomze, D.; Diem, S.; Ali, O.H.; Faessler, M.; Ring, S.; Niederer, R.; Ackermann, C.J.; Baumgaertner, P.; Pikor, N.; et al. Association of Checkpoint Inhibitor-Induced Toxic Effects with Shared Cancer and Tissue Antigens in Non-Small Cell Lung Cancer. JAMA Oncol. 2019, 5, 1043–1047. [Google Scholar] [CrossRef]
- Yang, H.; Yao, Z.; Zhou, X.; Zhang, W.; Zhang, X.; Zhang, F. Immune-related adverse events of checkpoint inhibitors: Insights into immunological dysregulation. Clin. Immunol. 2020, 213, 108377. [Google Scholar] [CrossRef]
- Passat, T.; Touchefeu, Y.; Gervois, N.; Jarry, A.; Bossard, C.; Bennouna, J. Physiopathological mechanisms of immune-related adverse events induced by anti-CTLA-4, anti-PD-1 and anti-PD-L1 antibodies in cancer treatment. Bull. Cancer 2018, 105, 1033–1041. [Google Scholar] [CrossRef]
- Chaput, N.; Lepage, P.; Coutzac, C.; Soularue, E.; Le Roux, K.; Monot, C.; Boselli, L.; Routier, E.; Cassard, L.; Collins, M.; et al. Baseline gut microbiota predicts clinical response and colitis in metastatic melanoma patients treated with ipilimumab. Ann. Oncol. 2019, 30, 2012. [Google Scholar] [CrossRef] [PubMed]


| Study | Cancer Type | Agents | Exposed Group/Total, No. | irAE Type | irAE Grade | Hazard Ratio (95% CI) | Landmark Analysis | Design |
|---|---|---|---|---|---|---|---|---|
| Aso, 2020 [2] | NSCLC | N/P | 51/155 | skin | 1–5 | PFS:0.58 (0.33–0.99) | 6 weeks | RC |
| OS:0.75 (0.40–1.43) | ||||||||
| Haratani, 2018 [8] | NSCLC | N | 69/134 | Global | 1–4 | PFS:0.57 (0.33–0.96) | 6 weeks | RC |
| OS:0.31 (0.11–0.68) | ||||||||
| Hosoya, 2020 [15] | NSCLC | N/P | 37/76 | Global | 1–4 | PFS:0.64 (0.39–1.05) | 6 weeks | PC |
| OS:0.64 (0.33–1.26) | ||||||||
| PFS:0.55 (0.31–0.98) | 3 weeks | RC | ||||||
| Ricciuti, 2019 [21] | NSCLC | N | 85/195 | Global | 1–4 | PFS:0.69 (0.45–1.05) | 6 weeks | RC |
| OS:0.55 (0.33–0.92) | ||||||||
| Cortellini, 2019 [13] | NSCLC | N/P | 231/559 | Global | 1–4 | PFS:0.56 (0.44–0.71) | 6 weeks | RC |
| OS:0.49 (0.37–0.65) | ||||||||
| Ahn, 2019 [16] | NSCLC | N/P | 55/155 | Global | 1–4 | PFS:0.36 (0.23–0.56) | 6 weeks | RC |
| OS:0.40 (0.25–0.65) | ||||||||
| Verzoni, 2019 [22] | RCC | N | 76/389 | Global | 1–4 | OS:0.48 (0.30–0.78) | 6 weeks | |
| Ishihara, 2019 [18] | RCC | N | 23/47 | Global | 1–4 | PFS:0.71 (0.29–1.73) | 2-cycle | RC |
| Masuda, 2019 [20] | AGC | N | 14/65 | Global | 1–4 | PFS:0.33 (0.15–0.73) | 2 months | RC |
| OS:0.56 (0.24–1.27) | ||||||||
| Teraoka, 2017 [14] | NSCLC | N | 19/43 | Global | 1–2 | PFS:0.37 (0.16–0.89) | 6 weeks | PC |
| OS:0.41 (0.05–3.67) | ||||||||
| Fukihara, 2019 [17] | NSCLC | N/P | 27/170 | pulmonary | 1–5 | PFS:2.86 (1.79–4.58) | 6 weeks | RC |
| OS:4.08 (1.67–9.94) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.-C.; Zhu, T.-C.; Nie, R.-C.; Lu, L.-H.; Xiang, Z.-C.; Xie, D.; Luo, R.-Z.; Cai, M.-Y. Association between Early Immune-Related Adverse Events and Survival in Patients Treated with PD-1/PD-L1 Inhibitors. J. Clin. Med. 2023, 12, 736. https://doi.org/10.3390/jcm12030736
Zhang Y-C, Zhu T-C, Nie R-C, Lu L-H, Xiang Z-C, Xie D, Luo R-Z, Cai M-Y. Association between Early Immune-Related Adverse Events and Survival in Patients Treated with PD-1/PD-L1 Inhibitors. Journal of Clinical Medicine. 2023; 12(3):736. https://doi.org/10.3390/jcm12030736
Chicago/Turabian StyleZhang, You-Cheng, Tian-Chen Zhu, Run-Cong Nie, Liang-He Lu, Zhi-Cheng Xiang, Dan Xie, Rong-Zhen Luo, and Mu-Yan Cai. 2023. "Association between Early Immune-Related Adverse Events and Survival in Patients Treated with PD-1/PD-L1 Inhibitors" Journal of Clinical Medicine 12, no. 3: 736. https://doi.org/10.3390/jcm12030736
APA StyleZhang, Y.-C., Zhu, T.-C., Nie, R.-C., Lu, L.-H., Xiang, Z.-C., Xie, D., Luo, R.-Z., & Cai, M.-Y. (2023). Association between Early Immune-Related Adverse Events and Survival in Patients Treated with PD-1/PD-L1 Inhibitors. Journal of Clinical Medicine, 12(3), 736. https://doi.org/10.3390/jcm12030736







