Association of Sonographic Sarcopenia and Falls in Older Adults Presenting to the Emergency Department
Abstract
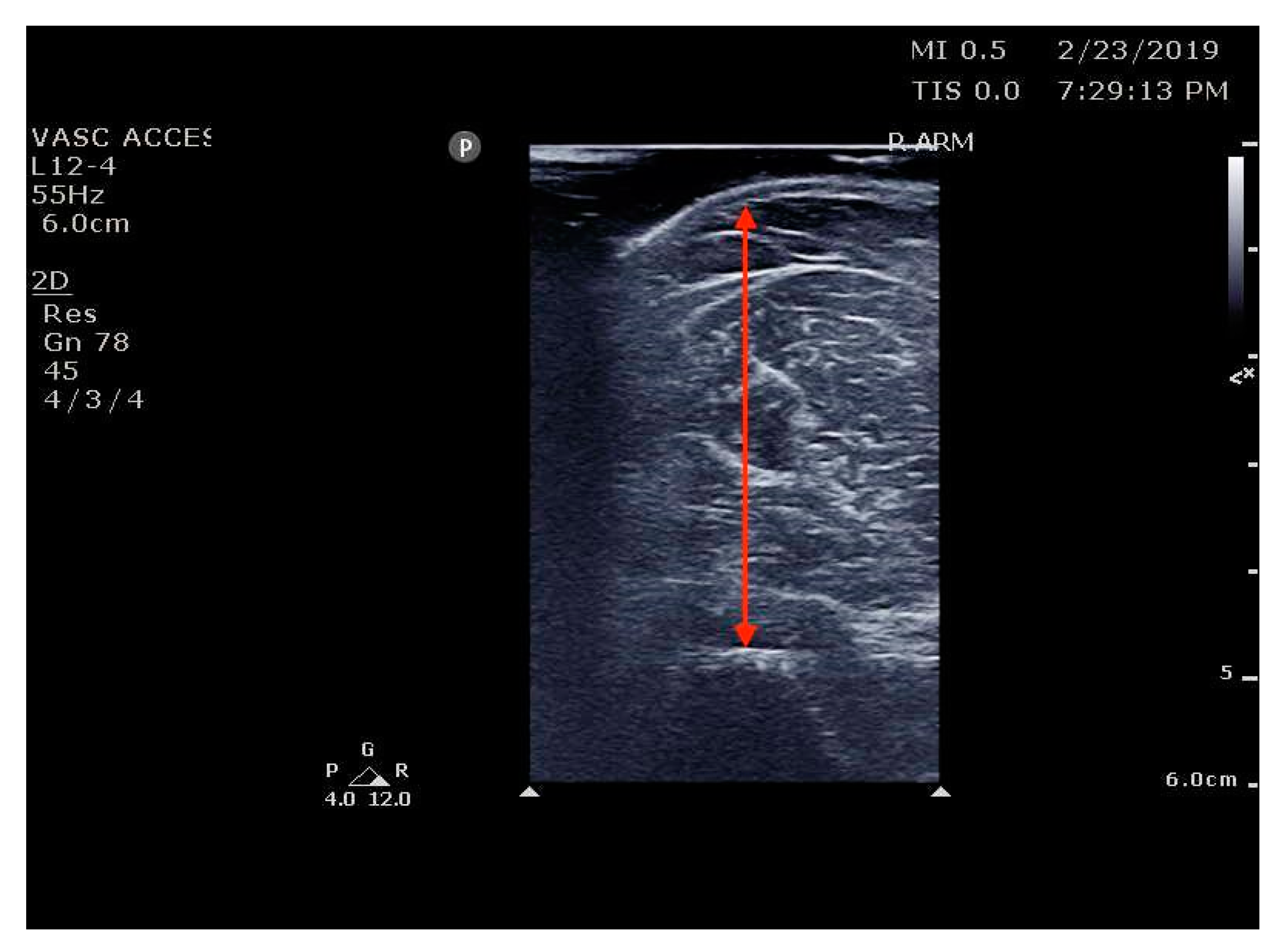
:1. Introduction
2. Method
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McCarthy, M. Falls are leading cause of injury deaths among older people, US study finds. BMJ 2016, 354, i5190. [Google Scholar] [CrossRef]
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and Fall Injuries Among Adults Aged ≥65 Years—United States, 2014. MMWR Morb. Mortal Wkly Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef]
- Florence, C.S.; Bergen, G.; Atherly, A.; Burns, E.; Stevens, J.; Drake, C. Medical Costs of Fatal and Nonfatal Falls in Older Adults: Medical Costs of Falls. J. Am. Geriatr. Soc. 2018, 66, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Shankar, K.; Liu, S.; Ganz, D. Trends and Characteristics of Emergency Department Visits for Fall-Related Injuries in Older Adults, 2003–2010. West J. Emerg. Med. 2017, 18, 785–793. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Williams, C.S. Falls, Injuries Due to Falls, and the Risk of Admission to a Nursing Home. N. Engl. J. Med. 1997, 337, 1279–1284. [Google Scholar] [CrossRef]
- LeLaurin, J.H.; Shorr, R.I. Preventing Falls in Hospitalized Patients. Clin. Geriatr. Med. 2019, 35, 273–283. [Google Scholar] [CrossRef] [PubMed]
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef]
- Liu-Ambrose, T.; Davis, J.C.; Best, J.R.; Dian, L.; Madden, K.; Cook, W.; Hsu, C.L.; Khan, K.M. Effect of a Home-Based Exercise Program on Subsequent Falls Among Community-Dwelling High-Risk Older Adults After a Fall: A Randomized Clinical Trial. JAMA 2019, 321, 2092. [Google Scholar] [CrossRef]
- Esquivel, M.K. Nutritional Assessment and Intervention to Prevent and Treat Malnutrition for Fall Risk Reduction in Elderly Populations. Am. J. Lifestyle Med. 2018, 12, 107–112. [Google Scholar] [CrossRef]
- Schneider, D.A.; Trence, D.L. Possible Role of Nutrition in Prevention of Sarcopenia and Falls. Endocr. Pract. 2019, 25, 1184–1190. [Google Scholar] [CrossRef]
- Sieber, C.C. Malnutrition and sarcopenia. Aging Clin. Exp. Res. 2019, 31, 793–798. [Google Scholar] [CrossRef]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patet, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Benzeval, M.; Deary, I.J.; Dennison, E.M.; Der, G.; Gale, C.R.; Inskip, H.M.; Jagger, C. Grip Strength across the Life Course: Normative Data from Twelve British Studies. Vina J, ed. PLoS ONE 2014, 9, e113637. [Google Scholar] [CrossRef]
- Stringer, H.J.; Wilson, D. The Role of Ultrasound as a Diagnostic Tool for Sarcopenia. J. Frailty Aging 2018, 7, 1–4. [Google Scholar] [CrossRef]
- Ismail, C.; Zabal, J.; Hernandez, H.J.; Woletz, P.; Manning, H.; Teixeira, C.; DiPietro, L.; Blackman, M.R.; Harris-Love, M.O. Diagnostic ultrasound estimates of muscle mass and muscle quality discriminate between women with and without sarcopenia. Front. Physiol. 2015, 6, 302. [Google Scholar] [CrossRef] [PubMed]
- Mueller, N.; Murthy, S.; Tainter, C.R.; Lee, J.; Riddell, K.; Fintelmann, F.J.; Grabitz, S.D.; Timm, F.P.; Levi, B.; Kurth, T. Can Sarcopenia Quantified by Ultrasound of the Rectus Femoris Muscle Predict Adverse Outcome of Surgical Intensive Care Unit Patients as well as Frailty? A Prospective, Observational Cohort Study. Ann. Surg. 2016, 264, 1116–1124. [Google Scholar] [CrossRef]
- Abe, T.; Loenneke, J.P.; Thiebaud, R.S.; Fukunaga, T. Age-related site-specific muscle wasting of upper and lower extremities and trunk in Japanese men and women. Age 2014, 36, 813–821. [Google Scholar] [CrossRef] [PubMed]
- Hida, T.; Ando, K.; Kobayashi, K.; Ito, K.; Tsushima, M.; Kobayakawa, T.; Morozumi, M.; Tanaka, S.; Machino, M.; Ota, K.; et al. Ultrasound measurement of thigh muscle thickness for assessment of sarcopenia. Nagoya J. Med. Sci. 2018, 80, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.P.; Penn, K.; Kaplan, S.J.; Vrablik, M.; Jablonowski, K.; Pham, T.N.; Reed, M.J. Comparison of bedside screening methods for frailty assessment in older adult trauma patients in the emergency department. Am. J. Emerg. Med. 2019, 37, 12–18. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [Green Version]
- Sallinen, J.; Stenholm, S.; Rantanen, T.; Heliövaara, M.; Sainio, P.; Koskinen, S. Hand-Grip Strength Cut Points to Screen Older Persons at Risk for Mobility Limitation: Hand-Grip Cut Points for Mobility Limitation. J. Am. Geriatr. Soc. 2010, 58, 1721–1726. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.; Patel, T.; Costa, A.; Bryce, E.; Hillier, L.M.; Slonim, K.; Hunter, S.W.; Heckman, G.; Molnar, F. Screening for frailty in primary care: Accuracy of gait speed and hand-grip strength. Can. Fam. Physician 2017, 63, e51–e57. [Google Scholar]
- Madden, K.M.; Feldman, B.; Arishenkoff, S.; Meneilly, G.S. A rapid point-of-care ultrasound marker for muscle mass and muscle strength in older adults. Age Ageing 2021, 50, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Hogenbirk, R.N.M.; Viddeleer, A.R.; Hentzen, J.E.K.R.; van der Plas, W.Y.; van der Schans, C.P.; de Bock, G.H.; Kruijff, S.; Klaase, J.M. Thickness of Biceps and Quadriceps Femoris Muscle Measured Using Point-of-Care Ultrasound as a Representation of Total Skeletal Muscle Mass. J. Clin. Med. 2022, 11, 6606. [Google Scholar] [CrossRef] [PubMed]
- Nijholt, W.; Scafoglieri, A.; Jager-Wittenaar, H.; Hobbelen, J.S.M.; van der Schans, C.P. The reliability and validity of ultrasound to quantify muscles in older adults: A systematic review: Muscle ultrasound in older adults. J. Cachexia Sarcopenia Muscle 2017, 8, 702–712. [Google Scholar] [CrossRef] [PubMed]
- Ticinesi, A.; Meschi, T.; Narici, M.V.; Lauretani, F.; Maggio, M. Muscle Ultrasound and Sarcopenia in Older Individuals: A Clinical Perspective. J. Am. Med. Dir. Assoc. 2017, 18, 290–300. [Google Scholar] [CrossRef]
- Abe, T.; Loenneke, J.P.; Young, K.C.; Thiebaud, R.S.; Nahar, V.K.; Hollaway, K.M.; Stover, C.D.; Ford, M.A.; Bass, M.A.; Loftin, M. Validity of Ultrasound Prediction Equations for Total and Regional Muscularity in Middle-aged and Older Men and Women. Ultrasound Med. Biol. 2015, 41, 557–564. [Google Scholar] [CrossRef]
- Sanz-Paris, A.; González-Fernandez, M.; Hueso-Del Río, L.E.; Ferrer-Lahuerta, E.; Monge-Vazquez, A.; Losfablos-Callau, F.; Sanclemente-Hernández, T.; Sanz-Arque, A.; Arbones-Mainar, J. Muscle Thickness and Echogenicity Measured by Ultrasound Could Detect Local Sarcopenia and Malnutrition in Older Patients Hospitalized for Hip Fracture. Nutrients 2021, 13, 2401. [Google Scholar] [CrossRef]
- Perkisas, S.; Bastijns, S.; Baudry, S.; Bauer, J.; Beaudart, C.; Beckwée, D.; Cruz-Jentoft, A.; Gasowski, J.; Hobbelen, H.; Jager-Wittenaar, H.; et al. Application of ultrasound for muscle assessment in sarcopenia: 2020 SARCUS update. Eur. Geriatr. Med. 2021, 12, 45–59. [Google Scholar] [CrossRef]
- Baracos, V.E. Psoas as a sentinel muscle for sarcopenia: A flawed premise: Editorial. J. Cachexia Sarcopenia Muscle 2017, 8, 527–528. [Google Scholar] [CrossRef]
- Rutten, I.J.G.; Ubachs, J.; Kruitwagen, R.F.P.M.; Beets-Tan, R.G.H.; Olde Damink, S.W.M.; Van Gorp, T. Psoas muscle area is not representative of total skeletal muscle area in the assessment of sarcopenia in ovarian cancer: Psoas muscle for assessment of sarcopenia in ovarian cancer. J. Cachexia Sarcopenia Muscle 2017, 8, 630–638. [Google Scholar] [CrossRef] [Green Version]
- Gadelha, A.B.; Neri, S.G.R.; Nóbrega, O.T.; Pereira, J.C.; Bottaro, M.; Fonsêca, A.; Lima, R.M. Muscle quality is associated with dynamic balance, fear of falling, and falls in older women. Exp. Gerontol. 2018, 104, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Benton, E.; Liteplo, A.S.; Shokoohi, H.; Loesche, M.A.; Yacoub, S.; Thatphet, P.; Wongtangman, T.; Liu, S.W. A pilot study examining the use of ultrasound to measure sarcopenia, frailty and fall in older patients. Am. J. Emerg. Med. 2021, 46, 310–316. [Google Scholar] [CrossRef]
- O’Sullivan, D.; O’Regan, N.A.; Timmons, S. Validity and Reliability of the 6-Item Cognitive Impairment Test for Screening Cognitive Impairment: A Review. Dement. Geriatr. Cogn. Disord. 2016, 42, 42–49. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Gong, G.; Wan, W.; Zhang, X.; Liu, Y.; Liu, X.; Yin, J. Correlation between the Charlson comorbidity index and skeletal muscle mass/physical performance in hospitalized older people potentially suffering from sarcopenia. BMC Geriatr. 2019, 19, 367. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, S.S.; Shati, M.; Keshtkar, A.; Malakouti, S.K.; Bazargan, M.; Assari, S. Defining polypharmacy in the elderly: A systematic review protocol. BMJ Open 2016, 6, e010989. [Google Scholar] [CrossRef] [PubMed]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef]
- Kim, J.; Parish, A.L. Polypharmacy and Medication Management in Older Adults. Nurs. Clin. North. Am. 2017, 52, 457–468. [Google Scholar] [CrossRef]
- Perkisas, S.; Baudry, S.; Bauer, J.; Beckwée, D.; De Cock, A.-M.; Hobbelen, H.; Jager-Wittenaar, H.; Kasiukiewicz, A.; Landi, F.; Marco, E.; et al. Application of ultrasound for muscle assessment in sarcopenia: Towards standardized measurements. Eur. Geriatr. Med. 2018, 9, 739–757. [Google Scholar] [CrossRef]
- Galindo Martín, C.A.; Monares Zepeda, E.; Lescas Méndez, O.A. Bedside Ultrasound Measurement of Rectus Femoris: A Tutorial for the Nutrition Support Clinician. J. Nutr. Metab. 2017, 2017, 2767232. [Google Scholar] [CrossRef]
- Delaney, S.; Worsley, P.; Warner, M.; Taylor, M.; Stokes, M. Assessing contractile ability of the quadriceps muscle using ultrasound imaging: Contractile Ability of Quadriceps. Muscle Nerve 2010, 42, 530–538. [Google Scholar] [CrossRef]
- Dodds, R.M.; Syddall, H.E.; Cooper, R.; Kuh, D.; Cooper, C.; Sayer, A.A. Global variation in grip strength: A systematic review and meta-analysis of normative data. Age Ageing 2016, 45, 209–216. [Google Scholar] [CrossRef]
- WHO. Falls. 26 April 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 28 May 2021).
- Bischoff, H.A. Identifying a cut-off point for normal mobility: A comparison of the timed “up and go” test in community-dwelling and institutionalised elderly women. Age Ageing 2003, 32, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk Factors for Falls among Elderly Persons Living in the Community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef] [PubMed]
- Desforges, J.F.; Tinetti, M.E.; Speechley, M. Prevention of Falls among the Elderly. N. Engl. J. Med. 1989, 320, 1055–1059. [Google Scholar] [CrossRef]
- Nevitt, M.C.; Cummings, S.R.; Kidd, S.; Black, D. Risk Factors for Recurrent Nonsyncopal Falls: A Prospective Study. JAMA 1989, 261, 2663. [Google Scholar] [CrossRef]
- Sai, A.; Tanaka, K.; Ohashi, Y.; Kushiyama, A.; Tanaka, Y.; Motonishi, S.; Sakai, K.; Hara, S.; Ozawa, T. Quantitative sonographic assessment of quadriceps muscle thickness for fall injury prediction in patients undergoing maintenance hemodialysis: An observational cohort study. BMC Nephrol. 2021, 22, 191. [Google Scholar] [CrossRef] [PubMed]
- Özkal, Ö.; Kara, M.; Topuz, S.; Kaymak, B.; Bakı, A.; Özçakar, L. Assessment of core and lower limb muscles for static/dynamic balance in the older people: An ultrasonographic study. Age Ageing 2019, 48, 881–887. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Li, H.; Hu, Y.; Zhu, S.; Xu, Z.; Zhang, Q.; Yang, Y.; Wang, Z.; Xu, J. Ultrasound for Measuring the Cross-Sectional Area of Biceps Brachii Muscle in Sarcopenia. Int. J. Med. Sci. 2020, 17, 2947–2953. [Google Scholar] [CrossRef] [PubMed]
- Fleischman, W. Study: Older Patients Vulnerable to Functional Decline Following ED Visit. ED Manag. Mon. Update Emerg. Dep. Manag. 2017, 29, 58–59. [Google Scholar]
- Tirrell, G.; Sri-on, J.; Lipsitz, L.A.; Camargo, C.A.; Kabrhel, C.; Liu, S.W. Evaluation of Older Adult Patients With Falls in the Emergency Department: Discordance With National Guidelines. Acad. Emerg. Med. 2015, 22, 461–467. [Google Scholar] [CrossRef]
- Paniagua, M.A.; Malphurs, J.E.; Phelan, E.A. Older patients presenting to a county hospital ED after a fall: Missed opportunities for prevention. Am. J. Emerg. Med. 2006, 24, 413–417. [Google Scholar] [CrossRef]
- Granacher, U.; Muehlbauer, T.; Zahner, L.; Gollhofer, A.; Kressig, R.W. Comparison of Traditional and Recent Approaches in the Promotion of Balance and Strength in Older Adults. Sports Med. 2011, 41, 377–400. [Google Scholar] [CrossRef]
- Society, A.G.; Society, G.; Of, A.A. On Falls Prevention OSP. Guideline for the Prevention of Falls in Older Persons. J. Am. Geriatr. Soc. 2001, 49, 664–672. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Josephson, K.R. The epidemiology of falls and syncope. Clin. Geriatr. Med. 2002, 18, 141–158. [Google Scholar] [CrossRef]
- Rosenblatt, N.J.; Madigan, M.L. Exploring the Association Between Measures of Obesity and Measures of Trip-induced Fall Risk Among Older Adults. Arch. Phys. Med. Rehabil. 2021, 102, 2362–2368. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.Y.; Seo, D.C.; Lin, H.C.; Lohrmann, D.K.; Chomistek, A.K. BMI and Central Obesity With Falls Among Community-Dwelling Older Adults. Am. J. Prev. Med. 2018, 54, e59–e66. [Google Scholar] [CrossRef] [PubMed]
- Lv, D.; Shen, S.; Chen, X. Association Between Dynapenic Abdominal Obesity and Fall Risk in Older Adults. Clin. Interv. Aging 2022, 17, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Deandrea, S.; Lucenteforte, E.; Bravi, F.; Foschi, R.; La Vecchia, C.; Negri, E. Risk Factors for Falls in Community-dwelling Older People: A Systematic Review and Meta-analysis. Epidemiology 2010, 21, 658–668. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | History of Fall (in the Prior 12 Months) | p-Value | ||
|---|---|---|---|---|
| Total Group N = 199 | Yes N = 91 | No N = 108 | ||
| Age (Mean, SD) | 77.3 (8.3) | 77.9 (8.2) | 76.8 (8.4) | 0.33 |
| 65–74 years (N, %) | 79 (39.5%) | 34 (37%) | 45 (42%) | |
| 75–84 years (N, %) | 77 (39.0%) | 35 (38%) | 42 (39%) | 0.69 |
| ≥85 years (N, %) | 43 (21.5%) | 22 (24%) | 21 (19%) | |
| Gender | 0.6 | |||
| Female (N, %) | 108 (54%) | 51 (56%) | 57 (53%) | |
| Male (N, %) | 91 (46%) | 40 (44%) | 51 (47%) | |
| BMI (cm/kg, median/IQR) | 27.6 (24.6–31.1) | 27.7 (24.8–30.1) | 27.7 (24.4–32.1) | 0.9 |
| Charlson Comorbidity Index (CCI) | 0.91 | |||
| 0–6 (N, %) | 158 (79%) | 73 (80%) | 85 (79%) | |
| >6 (N, %) | 41 (21%) | 18 (20%) | 23 (21%) | |
| Polypharmacy (>4) | N = 190 | 0.35 | ||
| Yes (N, %) | 179 (94%) | 83 (97%) | 96 (92%) | |
| No (N, %) | 11 (6%) | 3 (3%) | 8 (8%) | |
| Variable | All Participants N = 199 | History of Fall (in Past 12 Months) | |
|---|---|---|---|
| Yes (N = 91) | No (N = 108) | ||
| Biceps muscle thickness cm (Median/IQR) | 2.22 (1.87–2.74) | 2.22 (1.94–2.78) | 2.23 (1.79–2.69) |
| Thigh muscle thickness cm (Median/IQR) | 2.91 (2.40–3.49) | 2.76 (2.27–3.26) | 3.11 (2.55–3.68) |
| Grip strength | |||
| Normal [43] (≥16 kg in females, ≥27 in males) | N = 120 | 47 | 73 |
| Low [43] (<16 kg in females, <27 in males) | N = 79 | 44 | 35 |
| Variables | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Age | 1.02 | 0.98–1.05 |
| Sex (Female vs. Male) | 1.14 | 0.65–2.00 |
| Biceps muscle thickness | 0.97 | 0.65–1.44 |
| Thigh muscle thickness | 0.67 | 0.47–0.95 |
| Grip Strength | 0.52 | 0.29–0.93 |
| Timed Up and Go test result > 12 s | 2.73 | 0.72–10.27 |
| Charlson Comorbidity Index score > 6 | 0.91 | 0.46–1.82 |
| Polypharmacy | 2.31 | 0.59–8.97 |
| Variables | Adjusted Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Age | 1.00 | 0.96–1.04 |
| Sex (Female vs. Male) | 1.02 | 0.53–1.96 |
| Biceps muscle thickness | 1.47 | 0.85–2.54 |
| Thigh muscle thickness | 0.59 | 0.38–0.91 |
| Grip Strength | 0.59 | 0.31–1.14 |
| Charlson Comorbidity Index score > 6 | 0.9 | 0.43–1.90 |
| Polypharmacy | 3.07 | 0.60–15.63 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wongtangman, T.; Thatphet, P.; Shokoohi, H.; McFadden, K.; Ma, I.; Al Saud, A.; Vivian, R.; Hines, R.; Gullikson, J.; Morone, C.; et al. Association of Sonographic Sarcopenia and Falls in Older Adults Presenting to the Emergency Department. J. Clin. Med. 2023, 12, 1251. https://doi.org/10.3390/jcm12041251
Wongtangman T, Thatphet P, Shokoohi H, McFadden K, Ma I, Al Saud A, Vivian R, Hines R, Gullikson J, Morone C, et al. Association of Sonographic Sarcopenia and Falls in Older Adults Presenting to the Emergency Department. Journal of Clinical Medicine. 2023; 12(4):1251. https://doi.org/10.3390/jcm12041251
Chicago/Turabian StyleWongtangman, Thiti, Phraewa Thatphet, Hamid Shokoohi, Kathleen McFadden, Irene Ma, Ahad Al Saud, Rachel Vivian, Ryan Hines, Jamie Gullikson, Christina Morone, and et al. 2023. "Association of Sonographic Sarcopenia and Falls in Older Adults Presenting to the Emergency Department" Journal of Clinical Medicine 12, no. 4: 1251. https://doi.org/10.3390/jcm12041251
APA StyleWongtangman, T., Thatphet, P., Shokoohi, H., McFadden, K., Ma, I., Al Saud, A., Vivian, R., Hines, R., Gullikson, J., Morone, C., Parente, J., Perkisas, S., & Liu, S. W. (2023). Association of Sonographic Sarcopenia and Falls in Older Adults Presenting to the Emergency Department. Journal of Clinical Medicine, 12(4), 1251. https://doi.org/10.3390/jcm12041251







