Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subsection Literature Search and Study Selection
2.2. Data Extraction
2.3. Methodological Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Literature Search and Study Selection
3.2. Basic Characteristics of Included Studies
3.3. Outcomes and Measurements
3.4. Methodological Quality
3.5. Data Synthesis
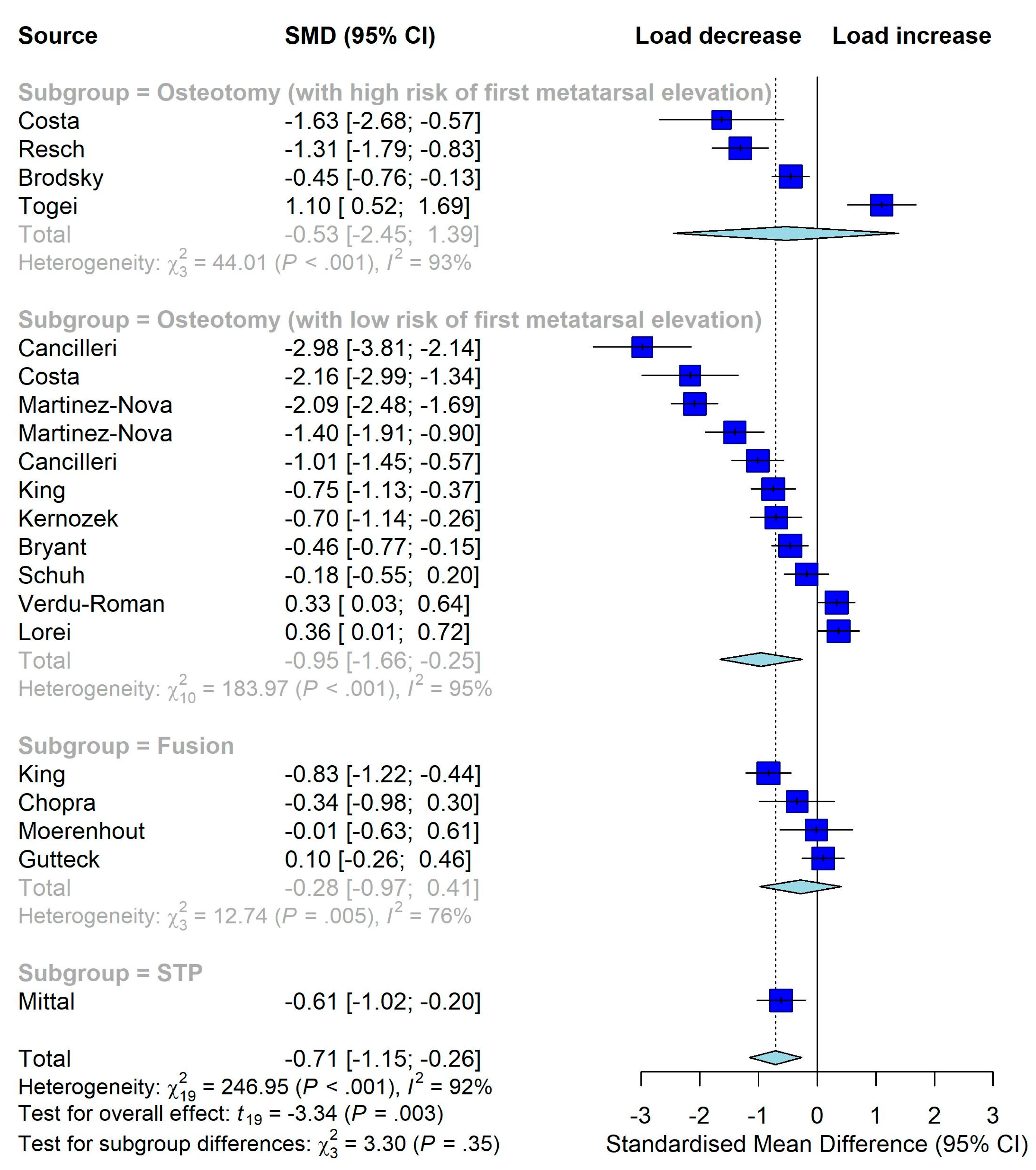
3.6. Subgroup Analyses
3.7. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nix, S.; Smith, M.; Vicenzino, B. Prevalence of hallux valgus in the general population: A systematic review and meta-analysis. J. Foot Ankle Res. 2010, 3, 21. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, R.; Yamaguchi, S.; Kimura, S.; Sadamasu, A.; Yamamoto, Y.; Muramatsu, Y.; Sato, Y.; Akagi, R.; Sasho, T.; Ohtori, S. Efficacy of foot orthoses as nonoperative treatment for hallux valgus: A 2-year follow-up study. J. Orthop. Sci. 2019, 24, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Morris, M.E. Footwear characteristics and foot problems in older people. Gerontology 2005, 51, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, E.B.; Svendsen, M.B.; Nørreslet, A.; Baldvinsson, H.K.; Heilskov-Hansen, T.; Larsen, P.K.; Alkjær, T.; Henriksen, M. Walking on high heels changes muscle activity and the dynamics of human walking significantly. J. Appl. Biomech. 2012, 28, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Roddy, E. Epidemiology and impact of hallux valgus: More than just bunions. J. Foot Ankle Res. 2011, 4, 1. [Google Scholar]
- Roan, L.-Y.; Tanaka, Y.; Taniguchi, A.; Tomiwa, K.; Kumai, T.; Cheng, Y.-M. Why do lesser toes deviate laterally in hallux valgus? A radiographic study. Foot Ankle Int. 2015, 36, 664–672. [Google Scholar] [CrossRef]
- Coughlin, M.J.; Anderson, R.B. Hallux Valgus. In Mann’s Surgery of the Foot and Ankle; Coughlin, M.J., Saltzman, C.L., Anderson, R.B., Eds.; Elsevier: Philadelphia, PA, USA, 2014; Volume 1, pp. 168–321. [Google Scholar]
- Partio, N.; Mäenpää, H.; Huttunen, T.; Haapasalo, H.; Laine, H.-J.; Mattila, V.M. Incidence of hallux valgus primary surgical treatment. Finnish nationwide data from 1997 to 2014. Foot Ankle Surg. 2019, 25, 761–765. [Google Scholar] [CrossRef]
- Miranda, M.A.M.; Martins, C.; Cortegana, I.M.; Campos, G.; Pérez, M.F.M.; Oliva, X.M. Complications on percutaneous hallux valgus surgery: A systematic review. J. Foot Ankle Surg. 2021, 60, 548–554. [Google Scholar] [PubMed]
- Malagelada, F.; Sahirad, C.; Dalmau-Pastor, M.; Vega, J.; Bhumbra, R.; Manzanares-Céspedes, M.C.; Laffenêtre, O. Minimally invasive surgery for hallux valgus: A systematic review of current surgical techniques. Int. Orthop. 2019, 43, 625–637. [Google Scholar]
- Trnka, H.-J. Percutaneous, MIS and open hallux valgus surgery. EFORT Open Rev. 2021, 6, 432–438. [Google Scholar]
- Lee, K.T.; Park, Y.U.; Jegal, H.; Lee, T.H. Deceptions in hallux valgus: What to look for to limit failures. Foot Ankle Clin. 2014, 19, 361–370. [Google Scholar]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [PubMed]
- Guyton, G.P. Theoretical limitations of the AOFAS scoring systems: An analysis using Monte Carlo modeling. Foot Ankle Int. 2001, 22, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Mayich, D.J. Life without the AOFAS score: A critical problem in a time of scarcity. Foot Ankle Int. 2012, 33, 689–691. [Google Scholar] [CrossRef]
- Raikin, S.M.; Miller, A.G.; Daniel, J. Recurrence of hallux valgus: A review. Foot Ankle Clin. 2014, 19, 259–274. [Google Scholar]
- Menz, H.B.; Lord, S.R. Gait instability in older people with hallux valgus. Foot Ankle Int. 2005, 26, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Geng, X.; Huang, D.; Wang, X.; Zhang, C.; Huang, J.; Ma, X.; Chen, L.; Wang, C.; Yang, J.; Wang, H. Loading pattern of postoperative hallux valgus feet with and without transfer metatarsalgia: A case control study. J. Orthop. Surg. Res. 2017, 12, 120. [Google Scholar]
- Abdul Razak, A.H.; Zayegh, A.; Begg, R.K.; Wahab, Y. Foot plantar pressure measurement system: A review. Sensors 2012, 12, 9884–9912. [Google Scholar]
- Deepashini, H.; Omar, B.; Paungmali, A.; Amaramalar, N.; Ohnmar, H.; Leonard, J. An insight into the plantar pressure distribution of the foot in clinical practice: Narrative review. Pol. Ann. Med. 2014, 21, 51–56. [Google Scholar]
- Wafai, L.; Zayegh, A.; Woulfe, J.; Aziz, S.M.; Begg, R. Identification of foot pathologies based on plantar pressure asymmetry. Sensors 2015, 15, 20392–20408. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, U.K.; Götze, M.; Wiesenreiter, K.; Müller, O.; Wünschel, M.; Mittag, F. Transfer of plantar pressure from the medial to the central forefoot in patients with hallux valgus. BMC Musculoskelet. Disord. 2019, 20, 149. [Google Scholar]
- Galica, A.M.; Hagedorn, T.J.; Dufour, A.B.; Riskowski, J.L.; Hillstrom, H.J.; Casey, V.A.; Hannan, M.T. Hallux valgus and plantar pressure loading: The Framingham foot study. J. Foot Ankle Res. 2013, 6, 42. [Google Scholar] [CrossRef]
- Lorei, T.J.; Kinast, C.; Klarner, H.; Rosenbaum, D. Pedographic, clinical, and functional outcome after scarf osteotomy. Clin. Orthop. Relat. Res. 2006, 451, 161–166. [Google Scholar] [CrossRef]
- Brodsky, J.W.; Beischer, A.D.; Robinson, A.H.; Westra, S.; Negrine, J.P.; Shabat, S. Surgery for hallux valgus with proximal crescentic osteotomy causes variable postoperative pressure patterns. Clin. Orthop. Relat. Res. 2006, 443, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Cheung, J.T.-M.; Wong, D.W.-C.; Cong, Y.; Zhang, M. Biomechanical simulation of high-heeled shoe donning and walking. J. Biomech. 2013, 46, 2067–2074. [Google Scholar]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). Available online: www.training.cochrane.org/handbook (accessed on 9 January 2023).
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar]
- Seki, H.; Oki, S.; Suda, Y.; Takeshima, K.; Kokubo, T.; Nagura, T.; Ishii, K. Three-dimensional analysis of the first metatarsal bone in minimally invasive distal linear metatarsal osteotomy for hallux valgus. Foot Ankle Int. 2020, 41, 84–93. [Google Scholar] [CrossRef]
- Borton, D.C.; Stephens, M.M. Basal metatarsal osteotomy for hallux valgus. J. Bone Jt. Surg. 1994, 76, 204–209. [Google Scholar] [CrossRef]
- Bryant, A.R.; Tinley, P.; Cole, J.H. Plantar pressure and radiographic changes to the forefoot after the Austin bunionectomy. J. Am. Podiatr. Med. Assoc. 2005, 95, 357–365. [Google Scholar] [CrossRef]
- Cancilleri, F.; Marinozzi, A.; Martinelli, N.; Ippolito, M.; Spiezia, F.; Ronconi, P.; Denaro, V. Comparison of plantar pressure, clinical, and radiographic changes of the forefoot after biplanar Austin osteotomy and triplanar Boc osteotomy in patients with mild hallux valgus. Foot Ankle Int. 2008, 29, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Chopra, S.; Moerenhout, K.; Crevoisier, X. Subjective versus objective assessment in early clinical outcome of modified Lapidus procedure for hallux valgus deformity. Clin. Biomech. 2016, 32, 187–193. [Google Scholar] [CrossRef]
- Costa, J.M.; Avila, A.O.V.; Kleinowski, D.N.; Kroth, L.M.; Contreras, M.E.K. Modified Chevron Osteotomy: Preliminary Analysis of Baropodometric Behavior. Acta Ortop. Bras. 2010, 18, 191–196. [Google Scholar] [CrossRef]
- Gutteck, N.; Savov, P.; Panian, M.; Wohlrab, D.; Zeh, A.; Delank, K.S. Preliminary results of a plantar plate for Lapidus arthrodesis. Foot Ankle Surg. 2018, 24, 383–388. [Google Scholar] [CrossRef]
- Jones, S.; Al Hussainy, H.A.; Ali, F.; Betts, R.P.; Flowers, M.J. Scarf osteotomy for hallux valgus. A prospective clinical and pedobarographic study. J. Bone Jt. Surg. Br. 2004, 86, 830–836. [Google Scholar] [CrossRef]
- Kernozek, T.W.; Sterriker, S.A. Chevron (Austin) distal metatarsal osteotomy for hallux valgus: Comparison of pre- and post-surgical characteristics. Foot Ankle Int. 2002, 23, 503–508. [Google Scholar] [CrossRef] [PubMed]
- Klemola, T.; Leppilahti, J.; Laine, V.; Pentikainen, I.; Ojala, R.; Ohtonen, P.; Savola, O. Effect of First Tarsometatarsal Joint Derotational Arthrodesis on First Ray Dynamic Stability Compared to Distal Chevron Osteotomy. Foot Ankle Int. 2017, 38, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Lipscombe, S.; Molloy, A.; Sirikonda, S.; Hennessy, M.S. Scarf osteotomy for the correction of hallux valgus: Midterm clinical outcome. J. Foot Ankle Surg. 2008, 47, 273–277. [Google Scholar] [CrossRef]
- Martinez-Nova, A.; Sanchez-Rodriguez, R.; Leal-Muro, A.; Pedrera-Zamorano, J.D. Dynamic Plantar Pressure Analysis and Midterm Outcomes in Percutaneous Correction for Mild Hallux Valgus. J. Orthop. Res. 2011, 29, 1700–1706. [Google Scholar] [CrossRef]
- Martínez-Nova, A.; Sánchez-Rodríguez, R.; Leal-Muro, A.; Sánchez-Barrado, E.; Pedrera-Zamorano, J.D. Percutaneous Distal Soft Tissue Release–Akin Procedure, Clinical and Podobarometric Assessment with the BioFoot In-Shoe System: A Preliminary Report. Foot Ankle Spec. 2008, 1, 222–230. [Google Scholar] [CrossRef]
- Mittal, D.; Raja, S.; Geary, N.P.J. The Modified McBride Procedure: Clinical, Radiological, and Pedobarographic Evaluations. J. Foot Ankle Surg. 2006, 45, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Moerenhout, K.; Chopra, S.; Crevoisier, X. Outcome of the modified Lapidus procedure for hallux valgus deformity during the first year following surgery: A prospective clinical and gait analysis study. Clin. Biomech. 2019, 61, 205–210. [Google Scholar] [CrossRef]
- Nyska, M.; Liberson, A.; McCabe, C.; Linge, K.; Klenerman, L. Plantar foot pressure distribution in patients with hallux valgus treated by distal soft tissue procedure and proximal metatarsal osteotomy. Foot Ankle Surg. 1998, 4, 35–41. [Google Scholar] [CrossRef]
- Resch, S.; Stenström, A. Evaluation of hallux valgus surgery with dynamic foot pressure registration with the Fscan system. Foot 1995, 5, 115–121. [Google Scholar] [CrossRef]
- Saro, C.; Andrén, B.; Felländer-Tsai, L.; Lindgren, U.; Arndt, A. Plantar pressure distribution and pain after distal osteotomy for hallux valgus. A prospective study of 22 patients with 12-month follow-up. Foot 2007, 17, 84–93. [Google Scholar] [CrossRef]
- Schuh, R.; Adams, S.; Hofstaetter, S.G.; Krismer, M.; Trnka, H.J. Plantar Loading After Chevron Osteotomy Combined with Postoperative Physical Therapy. Foot Ankle Int. 2010, 31, 980–986. [Google Scholar] [CrossRef]
- Schuh, R.; Hofstaetter, S.G.; Adams, S.B., Jr.; Pichler, F.; Kristen, K.H.; Trnka, H.J. Rehabilitation after hallux valgus surgery: Importance of physical therapy to restore weight bearing of the first ray during the stance phase. Phys. Ther. 2009, 89, 934–945. [Google Scholar] [CrossRef]
- Togei, K.; Shima, H.; Yasuda, T.; Tsujinaka, S.; Nakamura, G.; Neo, M. Plantar pressure distribution in hallux valgus feet after a first metatarsal proximal crescentic osteotomy with a lesser metatarsal proximal shortening osteotomy. Foot Ankle Surg. 2021, 27, 665–672. [Google Scholar] [CrossRef]
- Wong, D.W.C.; Wu, D.Y.; Man, H.S.; Leung, A.K.L. The use of a syndesmosis procedure for the treatment of hallux valgus: Good clinical and radiological results two years post-operatively. Bone Jt. J. 2014, 96, 502–507. [Google Scholar] [CrossRef]
- Yildiz, K.I.; Misir, A.; Kizkapan, T.B.; Cukurlu, M.; Aydin, C.G. Effect of Proximal Dome and Distal Chevron Osteotomies on Plantar Pressures and Radiographic and Functional Outcomes in Hallux Valgus Surgery a Retrospective Analysis. J. Am. Podiatr. Med. Assoc. 2021, 111. [Google Scholar]
- Verdu-Roman, C.; Sanz-Reig, J.; Martinez-Gimenez, E.; Carratala-Munuera, C.; Lopez-Pineda, A.; Quesada, J.A.; Gil-Guillen, V.F.; Orozco-Beltran, D. Plantar pressure improvement in moderate hallux valgus with modified chevron osteotomy: Clinical and radiographic outcomes. Foot Ankle Surg. 2020, 26, 205–208. [Google Scholar] [CrossRef] [PubMed]
- King, C.M.; Hamilton, G.A.; Ford, L.A. Effects of the lapidus arthrodesis and chevron bunionectomy on plantar forefoot pressures. J. Foot Ankle Surg. 2014, 53, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Garrow, A.P.; Papageorgiou, A.; Silman, A.J.; Thomas, E.; Jayson, M.I.; Macfarlane, G.J. The grading of hallux valgus: The Manchester Scale. J. Am. Podiatr. Med. Assoc. 2001, 91, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Piqué-Vidal, C.; Vila, J. A geometric analysis of hallux valgus: Correlation with clinical assessment of severity. J. Foot Ankle Res. 2009, 2, 15. [Google Scholar] [CrossRef] [PubMed]
- Zembsch, A.; Trnka, H.-J.; Ritschl, P. Correction of hallux valgus: Metatarsal osteotomy versus excision arthroplasty. Clin. Orthop. Relat. Res. 2000, 376, 183–194. [Google Scholar]
- Huerta, J.P.; Lorente, C.A.; Carmona, F.J.G. The Weil osteotomy: A comprehensive review. Rev. Española Podol. 2017, 28, e38–e51. [Google Scholar] [CrossRef]
- Perera, A.; Mason, L.; Stephens, M. The pathogenesis of hallux valgus. JBJS 2011, 93, 1650–1661. [Google Scholar]
- Wu, D.Y.; Lam, K. Osteodesis for hallux valgus correction: Is it effective? Clin. Orthop. Relat. Res. 2015, 473, 328–336. [Google Scholar]
- Ponnapula, P.; Wittock, R. Application of an interosseous suture and button device for hallux valgus correction: A review of outcomes in a small series. J. Foot Ankle Surg. 2010, 49, 159.e121–159.e126. [Google Scholar] [CrossRef]
- Polastri, M. Postoperative rehabilitation after hallux valgus surgery: A literature review. Foot Ankle Online J. 2011, 4, 4. [Google Scholar]
- Glasoe, W.M.; Nuckley, D.J.; Ludewig, P.M. Hallux valgus and the first metatarsal arch segment: A theoretical biomechanical perspective. Phys. Ther. 2010, 90, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Charen, D.A.; Markowitz, J.S.; Cheung, Z.B.; Matijakovich, D.J.; Chan, J.J.; Vulcano, E. Overview of metatarsalgia. Orthopedics 2019, 42, e138–e143. [Google Scholar] [CrossRef] [PubMed]
- Zeidan, H.; Ryo, E.; Suzuki, Y.; Iijima, H.; Kajiwara, Y.; Harada, K.; Nakai, K.; Shimoura, K.; Fujimoto, K.; Takahashi, M. Detailed analysis of the transverse arch of hallux valgus feet with and without pain using weightbearing ultrasound imaging and precise force sensors. PLoS ONE 2020, 15, e0226914. [Google Scholar]
- Kang, J.-H.; Chen, M.-D.; Chen, S.-C.; Hsi, W.-L. Correlations between subjective treatment responses and plantar pressure parameters of metatarsal pad treatment in metatarsalgia patients: A prospective study. BMC Musculoskelet. Disord. 2006, 7, 95. [Google Scholar]
- Wong, D.W.-C.; Wang, Y.; Zhang, M.; Leung, A.K.-L. Functional restoration and risk of non-union of the first metatarsocuneiform arthrodesis for hallux valgus: A finite element approach. J. Biomech. 2015, 48, 3142–3148. [Google Scholar] [CrossRef]
- Coughlin, M.J. Lesser Toe Deformities. In Mann’s Surgery of the Foot and Ankle; Coughlin, M.J., Saltzman, C.L., Anderson, R.B., Eds.; Elsevier: Philadelphia, PA, USA, 2014; Volume 1, pp. 322–424. [Google Scholar]
- Mickle, K.J.; Munro, B.J.; Lord, S.R.; Menz, H.B.; Steele, J.R. Gait, balance and plantar pressures in older people with toe deformities. Gait Posture 2011, 34, 347–351. [Google Scholar] [PubMed]
- Pasapula, C.; Al-Sukaini, A.; Band, H.; Fawi, H.; Cutts, S. Spring Ligament Insufficiency and Hallux Valgus as an independent risk factors for First Ray Instability. Foot 2021, 48, 101818. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.W.-C.; Zhang, M.; Yu, J.; Leung, A.K.-L. Biomechanics of first ray hypermobility: An investigation on joint force during walking using finite element analysis. Med. Eng. Phys. 2014, 36, 1388–1393. [Google Scholar]
- Biz, C.; Favero, L.; Stecco, C.; Aldegheri, R. Hypermobility of the first ray in ballet dancer. Muscles Ligaments Tendons J. 2012, 2, 282. [Google Scholar]
- Wong, D.W.-C.; Wang, Y.; Chen, T.L.-W.; Yan, F.; Peng, Y.; Tan, Q.; Ni, M.; Leung, A.K.-L.; Zhang, M. Finite element analysis of generalized ligament laxity on the deterioration of Hallux valgus deformity (bunion). Front. Bioeng. Biotechnol. 2020, 8, 1062. [Google Scholar] [CrossRef]
- Blackwood, S.; Gossett, L. Hallux valgus/medial column instability and their relationship with posterior tibial tendon dysfunction. Foot Ankle Clin. 2018, 23, 297–313. [Google Scholar] [CrossRef] [PubMed]
- Hagedorn, T.J.; Dufour, A.B.; Riskowski, J.L.; Hillstrom, H.J.; Menz, H.B.; Casey, V.A.; Hannan, M.T. Foot disorders, foot posture, and foot function: The Framingham foot study. PLoS ONE 2013, 8, e74364. [Google Scholar] [CrossRef] [PubMed]
- Heyes, G.J.; Vosoughi, A.R.; Weigelt, L.; Mason, L.; Molloy, A. Pes planus deformity and its association with hallux valgus recurrence following scarf osteotomy. Foot Ankle Int. 2020, 41, 1212–1218. [Google Scholar] [PubMed]
- Cobden, A.; Camurcu, Y.; Sofu, H.; Ucpunar, H.; Duman, S.; Kocabiyik, A. Evaluation of the Association Between Plantar Fasciitis and Hallux Valgus. J. Am. Podiatr. Med. Assoc. 2020, 110. [Google Scholar] [CrossRef]
- Wu, W.-L.; Liang, J.-M.; Cheng, Y.-M.; Huang, P.-J.; Wu, J.-H. The foot plantar pressures for patients with hallux valgus combines with or without claw toe. J. Foot Ankle Res. 2014, 7, A110. [Google Scholar] [CrossRef]
- Richie, D.H., Jr. First Ray Function, Metatarsalgia, and Hammertoes: How Are They Connected? In Hammertoes; Springer: Cham, Switzerland, 2019; pp. 33–55. [Google Scholar]
- Han, J.T.; Koo, H.M.; Jung, J.M.; Kim, Y.J.; Lee, J.H. Differences in plantar foot pressure and COP between flat and normal feet during walking. J. Phys. Ther. Sci. 2011, 23, 683–685. [Google Scholar] [CrossRef]
- Yamada, S.; Hirao, M.; Tsuboi, H.; Akita, S.; Matsushita, M.; Ohshima, S.; Saeki, Y.; Hashimoto, J. Involvement of valgus hindfoot deformity in hallux valgus deformity in rheumatoid arthritis. Mod. Rheumatol. 2014, 24, 851–854. [Google Scholar] [CrossRef]
- Chevalier, T.L.; Hodgins, H.; Chockalingam, N. Plantar pressure measurements using an in-shoe system and a pressure platform: A comparison. Gait Posture 2010, 31, 397–399. [Google Scholar]
- Liau, B.-Y.; Wu, F.-L.; Li, Y.; Lung, C.-W.; Mohamed, A.A.; Jan, Y.-K. Effect of Walking Speeds on Complexity of Plantar Pressure Patterns. Complexity 2021, 2021, 6571336. [Google Scholar]
- Lee, S.-Y.; Chou, C.-Y.; Hou, Y.-Y.; Wang, Y.-L.; Yang, C.-H.; Guo, L.-Y. The effects of changes in step width on plantar foot pressure patterns of young female subjects during walking. J. Mech. Med. Biol. 2011, 11, 1071–1083. [Google Scholar] [CrossRef]




| Source | Year | Intervention/Group | Subject | Feet | Age * | Deformity Angle | Severity |
|---|---|---|---|---|---|---|---|
| Borton and Stephens [31] | 1994 | Basal Chevron ost. | 31 (25 F/6 M) | 32 | 53.1 | IMA > 12° | Moderate to severe # |
| Brodsky, et al. [25] | 2006 | Mod. McBride proc. w/ prox. crescentic ost. | 32 (29 F/3 M) | 43 | 41.7 (10.1) | - | - |
| Bryant, et al. [32] | 2005 | Austin bunionectomy | 31 (27 F/4 M) | 44 | 50.5 (11.3) | HVA ≥ 20° | Moderate to severe # |
| Cancilleri, et al. [33] | 2008 | Austin ost. | 30 F | 30 | 56.2 | IMA < 15° | Mild |
| Boc ost. | 30 F | 30 | 59.1 | ||||
| Chopra, et al. [34] | 2016 | Mod. Lapidus proc. | 10 F | - | 51.3 (10.3) | - | Moderate to severe |
| Costa, et al. [35] | 2010 | Mod. distal Chevron ost. | 12 F | 19 | 49 (13) | HVA: 17°–44° IMA: 11°–18° | Mild to moderate |
| Mod. distal Chevron ost. w/ Weil proc. | 4 F | 8 | |||||
| Gutteck, et al. [36] | 2018 | 1st TMT arthrodesis | 28 | 30 | 52.5 | HVA: 35.9° (8.3°) IMA: 19.2° (3.2°) | Moderate to severe # |
| Jones, et al. [37] | 2004 | Scarf ost. w/ Akin closing-wedge ost. | 24 (21 F/3 M) | 35 | 46 | HVA: 24°–46°IMA: 10°–19° | Moderate to severe # |
| Kernozek and Sterriker [38] | 2002 | Chevron (Austin) ost. | 25 F | - | 43 | HVA: 31.7° (4.7°) IMA: 14.5° (1.7°) | Mild to moderate |
| King, et al. [54] | 2014 | Chevron bunionectomy | 34 (30 F/4 M) | 34 | 55.6 (11.8) | HVA: 24.4° (3.8°) IMA: 13.6° (2.9°) | Moderate # |
| Lapidus arthrodesis | 34 (32 F/2 M) | 34 | 52.6 (12.0) | HVA: 31.6° (7.0°) IMA: 15.6 ° (4.2°) | |||
| Klemola, et al. [39] | 2017 | Chevron ost. | 30 F | 30 | 37.6 (7.0) | HVA ≤ 50° IMA ≤ 21° | Mild to severe # |
| 1st TMT arthrodesis | 30 (29 F/1 M) | 30 | 51.3 (9.2) | Matched pair on HVA with Chevron group | |||
| Lipscombe, et al. [40] | 2008 | Scarf ost. | 22 (20 F/2 M) | 31 | 57 | HVA: 20°–40° IMA: 11°–18° | Moderate # |
| Lorei, et al. [24] | 2006 | Scarf ost. | 32 (31 F/1 M) | 32 | 54.1 (12.3) | HVA: 32.5° (7.2°) IMA: 15.5° (2.7°) | Moderate # |
| Martínez-Nova, et al. [42] | 2008 | PDSTR—Akin proc. | 26 F | 30 | 50.3 | HVA: 15°–30° IMA ≤ 13° | Mild |
| Martinez-Nova, et al. [41] | 2011 | PDSTR—Akin proc. | 79 F | 79 | 54.7 (12.5) | HVA: 15°–30°IMA ≤ 13° | Mild |
| Mittal, et al. [43] | 2006 | Mod. McBride proc. | 19 F | 27 | 49.7 | HVA ≥ 20° IMA ≥ 10° | Moderate to severe # |
| Moerenhout, et al. [44] | 2019 | Mod. Lapidus proc. | 10 F | - | 51.3 (8.2) | HVA > 20° IMA > 15° | Moderate to severe |
| Nyska, et al. [45] | 1998 | Distal soft tissue proc. w/ prox. ost. | 17 (15 F/2 M) | 29 | 47.8 | HVA: 29.6° (10.1°) IMA: 12.9° (4.3°) | Moderate # |
| Scarf ost. | 25 (23 F/2 M) | 51.0 | |||||
| Resch and Stenström [46] | 1995 | Chevron ost. | 24 (23 F/1 M) | 22 | 52 | HVA: 32° (8°) IMA: 13° (3°) | Moderate # |
| Proximal closing wedge ost. | 9 | HVA: 31° (7°) IMA: 12° (3°) | |||||
| Saro, et al. [47] | 2007 | Chevron ost. | 8 F | 8 | 49 (13) | HVA: 20°–44° IMA < 21° | Moderate to severe # |
| Lindgren ost. | 14 F | 14 | 49 (14) | ||||
| Schuh, et al. [49] | 2009 | Austin ost. | 30 (28 F/2 M) | - | 58.4 (13.8) | IMA < 16° | Mild to moderate |
| Scarf ost. | - | IMA > 16° | |||||
| Schuh, et al. [48] | 2010 | Chevron ost. | 29 (28 F/1 M) | - | 58 | HVA: 20°–50° IMA: 11°–18° | Mild to moderate |
| Togei, et al. [50] | 2020 | 1st MT prox. crescentic ost. w/ lesser MT prox. shortening ost. | 18 F | 18 | 60.4 (7.2) | HVA > 25° IMA > 12° | Moderate to severe |
| Verdu-Roman, et al. [53] | 2020 | Mod. Chevron ost. | 44 (35 F/9 M) | - | 56.1 (12.7) | HVA: 21°–40° | Moderate |
| Wong, et al. [51] | 2014 | Syndesmosis | 27 (26 F/1 M) | 54 | 46 | HVA: 24.3°–49.8° IMA: 10.2°–18.6° | Moderate to severe |
| Yildiz, et al. [52] | 2021 | Distal Chevron ost. | 26 (22 F/4 M) | - | 45.3 (15.2) | HVA: 31.4° (3.9°) IMA: 12.3° (2.6°) | Moderate # |
| Proximal Dome ost. | 22 (18 F/4 M) | - | 44.7 (15.1) | HVA: 38.5° (7.6°) IMA: 14.7° (3.7°) |
| Source | Intervention/Group | Surgery Class | Last F/U (Months) | Outcome |
|---|---|---|---|---|
| Borton and Stephens [31] | Basal Chevron ost. | Osteotomy (proximal) | 9.9 | MP |
| Brodsky, et al. [25] | Mod. McBride proc. w/ prox. crescentic ost. | Osteotomy (proximal) | 29 | PP, PTI |
| Bryant, et al. [32] | Austin bunionectomy | Osteotomy (distal) | 24 | PP |
| Cancilleri, et al. [33] | Austin ost. | Osteotomy (distal) | 24 | PP, PTI |
| Boc ost. | Osteotomy (distal) | |||
| Chopra, et al. [34] | Mod. Lapidus proc. | Fusion | 6 | PF, PP |
| Costa, et al. [35] | Mod. distal Chevron ost. | Osteotomy (distal) | 3 | PP, PTI |
| Mod. distal Chevron ost. w/ Weil proc. | Osteotomy (distal) | |||
| Gutteck, et al. [36] | 1st TMT arthrodesis | Fusion | 12 | PF, FTI |
| Jones, et al. [37] | Scarf ost. w/ Akin closing-wedge ost. | Osteotomy (distal) | 12 | PP |
| Kernozek and Sterriker [38] | Chevron (Austin) ost. | Osteotomy (distal) | 12 | PF, FTI, PP, PTI |
| King, et al. [54] | Chevron bunionectomy | Osteotomy (distal) | 7.7 | MP |
| Lapidus arthrodesis | Fusion | |||
| Klemola, et al. [39] | Chevron ost. | Osteotomy (distal) | 7.9 years | FTI |
| 1st TMT arthrodesis | Fusion | 5.1 years | ||
| Lipscombe, et al. [40] | Scarf ost. | Osteotomy (distal) | 12 | PP, PTI, FTI |
| Lorei, et al. [24] | Scarf ost. | Osteotomy (distal) | 33 | PF, PP, FTI |
| Martínez-Nova, et al. [42] | PDSTR—Akin proc. | Osteotomy (distal) | 12.1 | PP, MP |
| Martinez-Nova, et al. [41] | PDSTR—Akin proc. | Osteotomy (distal) | 28.1 | MP |
| Mittal, et al. [43] | Mod. McBride proc. | Soft Tissue proc. | 7 | PF, PP |
| Moerenhout, et al. [44] | Mod. Lapidus proc. | Fusion | 12 | PF, PP |
| Nyska, et al. [45] | Distal soft tissue proc. w/ prox. ost. | Osteotomy (proximal) | 18.2 | PF, PP, FTI, PTI |
| Scarf ost. | Osteotomy (distal) | |||
| Resch and Stenström [46] | Chevron ost. | Osteotomy (distal) | 25 | PP |
| Proximal closing wedge ost. | Osteotomy (proximal) | |||
| Saro, et al. [47] | Chevron ost. | Osteotomy (distal) | 12 | PP, MP |
| Lindgren ost. | Osteotomy (distal) | |||
| Schuh, et al. [49] | Austin ost. | Osteotomy (distal) | 6 | PF, PP, FTI |
| Scarf ost. | Osteotomy (distal) | |||
| Schuh, et al. [48] | Chevron ost. | Osteotomy (distal) | 12 | PF, FTI |
| Togei, et al. [50] | 1st MT prox. crescentic ost. w/ lesser MT prox. shortening ost. | Osteotomy (proximal) | 18.7 | PF, PP, FTI |
| Verdu-Roman, et al. [53] | Mod. Chevron ost. | Osteotomy (distal) | 12 | PP, MP |
| Wong, et al. [51] | Syndesmosis | Soft Tissue proc. | 26.4 | PF, FTI |
| Yildiz, et al. [52] | Distal Chevron ost. | Osteotomy (distal) | 12 | MP |
| Proximal Dome ost. | Osteotomy (proximal) |
| Load over Hx | Load over MMT | Load over CMT | ||||
|---|---|---|---|---|---|---|
| Effect (95%CI) | I2(%) | Effect (95%CI) | I2(%) | Effect (95%CI) | I2(%) | |
| Subgroup: Surgery | ||||||
| Osteotomy (high-elev.) | −0.53 (−2.45 to 1.39) | 93 | −0.40 (−0.98 to 0.18) | 64 | 0.14 (−1.24 to 1.51) | 93 |
| Osteotomy (low-elev.) | −0.95 (−1.66 to −0.25) * | 95 | −0.30 (−0.84 to 0.24) | 89 | −0.06 (−0.56 to 0.44) | 87 |
| Fusion | −0.28 (−0.97 to 0.41) | 76 | 0.17 (−0.04 to 0.38) | 0 | −0.29 (−0.88 to 0.29) | 54 |
| STP | −0.61 (01.02 to −0.20) | - | - | - | ||
| SGD | p = 0.35 | p = 0.004 | p = 0.56 | |||
| Subgroup: Age | ||||||
| <53 | −0.75 (−1.15 to −0.34) * | 81 | −0.15 (−0.45 to 0.15) | 76 | 0.06 (−0.29 to 0.40) | 82 |
| >=53 | −0.63 (−1.74 to −0.49) * | 96 | −0.37 (−1.19 to 0.45) | 91 | −0.29 (−1.12 to 0.55) | 91 |
| SGD | p = 0.81 | p = 0.55 | p = 0.38 | |||
| Subgroup: Follow-up period | ||||||
| >=12 months | −0.63 (−1.28 to 0.02) | 95 | −0.24 (−0.69 to 0.21) | 87 | −0.06 (−0.56 to 0.45) | 90 |
| <12 months | −0.81 (−1.40 to −0.21) * | 75 | −0.2 (−0.71 to 0.32) | 72 | −0.13 (−0.48 to 0.23) | 47 |
| SGD | p = 0.64 | p = 0.88 | p = 0.79 | |||
| Subgroup: Publication Year | ||||||
| <2010 | −0.81 (−1.41 to −0.20) * | 90 | −0.41 (−1.06 to 0.24) | 90 | −0.07 (−0.77 to 0.63) | 91 |
| >=2010 | −0.60 (−1.36 to 0.17) | 94 | −0.04 (−0.32 to 0.24) | 62 | −0.09 (−0.44 to 0.27) | 79 |
| SGD | p = 0.63 | p = 0.24 | p = 0.96 | |||
| Sensitivity Analysis | ||||||
| Overall | −0.71 (−1.15 to −0.26) * | 92 | −0.23 (−0.55 to 0.09) | 84 | −0.08 (−0.42 to 0.27) | 87 |
| RL | −0.71 (−1.17 to −0.25) * | 92 | 0.00 (−0.21 to 0.20) | 60 | 0.00 (−0.23 to 0.23) | 72 |
| Impulse over Hx | Impulse over MMT | Impulse over CMT | ||||
|---|---|---|---|---|---|---|
| Effect (95%CI) | I2(%) | Effect (95%CI) | I2(%) | Effect (95%CI) | I2(%) | |
| Subgroup: Surgery | ||||||
| Osteotomy (high-elev.) | −0.39 (−6.01 to 5.22) | 94 | −0.05 (−0.38 to 0.29) | 0 | −0.04 (−0.78 to 0.70) | 37 |
| Osteotomy (low-elev.) | −0.70 (−1.68 to 0.27) | 95 | −0.05 (−0.68 to 0.58) | 91 | 0.02 (−0.58 to 0.61) | 89 |
| Fusion | −0.22 (−2.48 to 2.04) | 45 | 0.25 (−3.97 to 4.48) | 84 | −0.08 (−1.04 to 0.89) | 0 |
| STP | - | - | - | |||
| SGD | p = 0.55 | p = 0.68 | p = 0.93 | |||
| Subgroup: Age | ||||||
| <53 | −0.80 (−1.63 to 0.02) | 85 | 0.01 (−0.44 to 0.46) | 76 | 0.07 (−0.18 to 0.32) | 41 |
| >=53 | −0.07 (−1.57 to 1.42) | 96 | 0.03 (−0.78 to 0.84) | 92 | −0.13 (−0.97 to 0.71) | 91 |
| SGD | p = 0.28 | p = 0.96 | p = 0.57 | |||
| Subgroup: Follow-up period | ||||||
| >=12 months | −0.33 (−1.09 to 0.44) | 93 | 0.02 (−0.37 to 0.40) | 85 | −0.13 (−0.53 to 0.26) | 83 |
| <12 months | −1.50 (−6.06 to 3.05) | 95 | 0.00 (−2.38 to 2.39) | 93 | 0.54 (0.12 to 0.95)* | 0 |
| SGD | p = 0.29 | p = 0.98 | p = 0.008 | |||
| Subgroup: Publication Year | ||||||
| <2010 | −0.64 (−1.78 to 0.49) | 95 | −0.04 (−0.82 to 0.74) | 92 | −0.18 (−0.96 to 0.59) | 90 |
| >=2010 | −0.40 (−1.74 to 0.94) | 93 | 0.07 (−0.40 to 0.55) | 77 | 0.14 (−0.17 to 0.46) | 58 |
| SGD | p = 0.73 | p = 0.75 | p = 0.32 | |||
| Sensitivity Analysis | ||||||
| Overall | −0.51 (−1.26 to 0.23) | 93 | 0.02 (−0.35 to 0.38) | 87 | 0 (−0.34 to 0.33) | 82 |
| RL | −0.47 (−1.48 to 0.54) | 92 | 0.19 (−0.26 to 0.65) | 80 | 0.27 (0 to 0.53) * | 56 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, D.W.-C.; Cheung, J.C.-W.; Zhao, J.-G.; Ni, M.; Yang, Z.-Y. Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement. J. Clin. Med. 2023, 12, 1384. https://doi.org/10.3390/jcm12041384
Wong DW-C, Cheung JC-W, Zhao J-G, Ni M, Yang Z-Y. Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement. Journal of Clinical Medicine. 2023; 12(4):1384. https://doi.org/10.3390/jcm12041384
Chicago/Turabian StyleWong, Duo Wai-Chi, James Chung-Wai Cheung, Jia-Guo Zhao, Ming Ni, and Zu-Yao Yang. 2023. "Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement" Journal of Clinical Medicine 12, no. 4: 1384. https://doi.org/10.3390/jcm12041384
APA StyleWong, D. W.-C., Cheung, J. C.-W., Zhao, J.-G., Ni, M., & Yang, Z.-Y. (2023). Forefoot Function after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis on Plantar Load Measurement. Journal of Clinical Medicine, 12(4), 1384. https://doi.org/10.3390/jcm12041384







