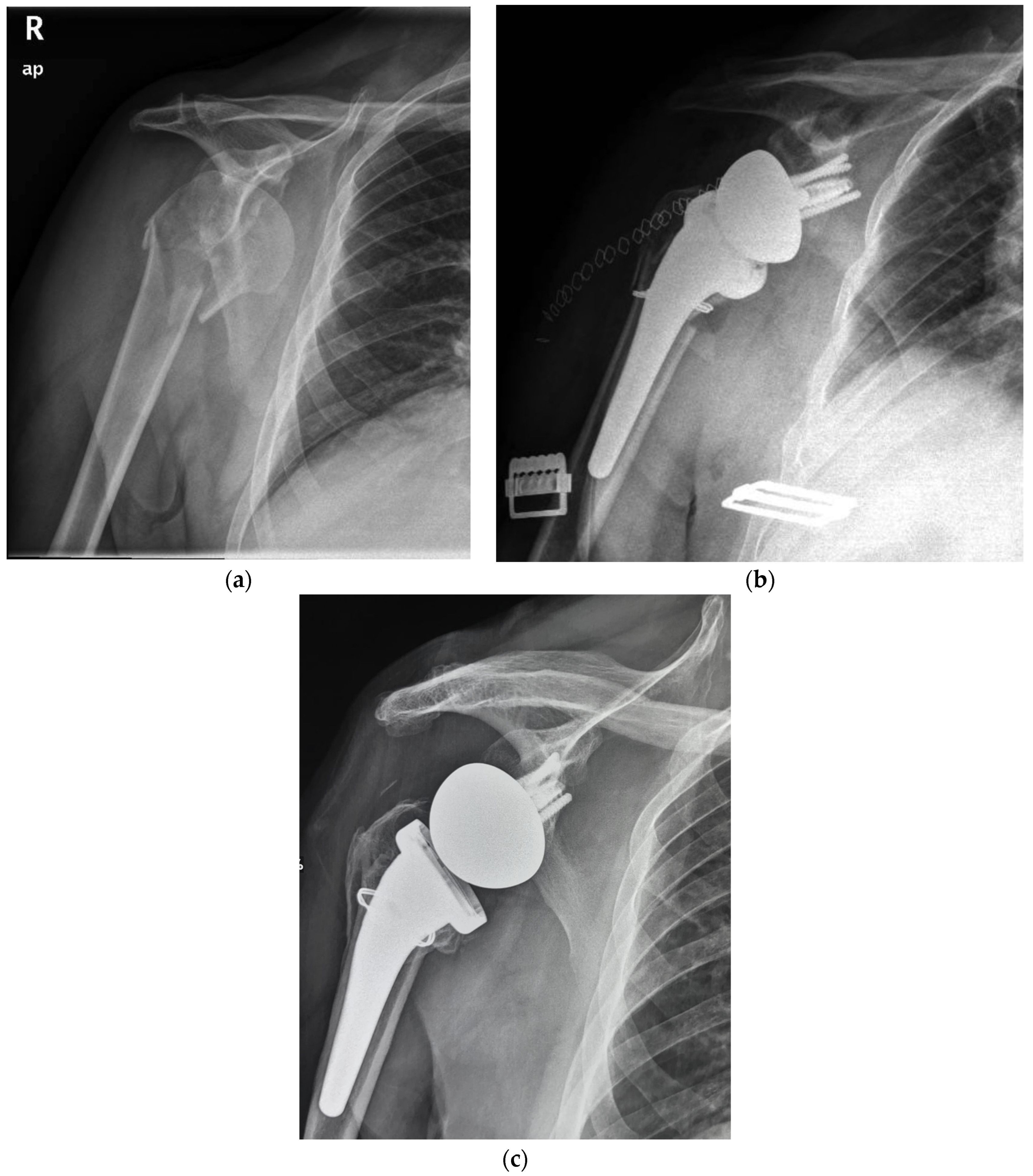
Reverse Total Shoulder Arthroplasty with a Cementless and Metaphyseal Stem Fixation Is a Viable Option for the Treatment of Proximal Humeral Fractures with Calcar Involvement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Implant
2.2. Surgical Technique
2.3. Postoperative Care
2.4. Radiological Assessment and Examination
2.5. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bell, J.E.; Leung, B.C.; Spratt, K.F.; Koval, K.J.; Weinstein, J.D.; Goodman, D.C.; Tosteson, A.N. Trends.and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J. Bone Jt. Surg. Am. 2011, 93, 121–131. [Google Scholar] [CrossRef]
- Miyamura, S.; Lans, J.; Min, K.S.; Waryasz, G.R.; Murase, T.; Chen, N.C. Bone resorption of the greater tuberosity after open reduction and internal fixation of complex proximal humeral fractures: Fragment characteristics and intraoperative risk factors. J. Shoulder Elbow Surg. 2021, 30, 1626–1635. [Google Scholar] [CrossRef]
- Yahuaca, B.I.; Simon, P.; Christmas, K.N.; Patel, S.; Gorman, R.A.; Mighell, M.A., 2nd; Frankle, M.A. Acute surgical management of proximal humerus fractures: ORIF vs. hemiarthroplasty vs. reverse shoulder arthroplasty. J. Shoulder Elbow Surg. 2020, 29, S32–S40. [Google Scholar] [CrossRef] [PubMed]
- Dillon, M.T.; Prentice, H.A.; Burfeind, W.E.; Chan, P.H.; Navarro, R.A. The increasing role of reverse total shoulder arthroplasty in the treatment of proximal humerus fractures. Injury 2019, 50, 676–680. [Google Scholar] [CrossRef] [PubMed]
- Mighell, M.A.; Kolm, G.P.; Collinge, C.A.; Frankle, M.A. Outcomes of hemiarthroplasty for fractures of the proximal humerus. J. Shoulder Elbow Surg. 2003, 12, 569–577. [Google Scholar] [CrossRef]
- Boileau, P.; Krishnan, S.G.; Tinsi, L.; Walch, G.; Coste, J.S.; Mole, D. Tuberosity malposition and migration: Reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J. Shoulder Elbow Surg. 2002, 11, 401–412. [Google Scholar] [CrossRef]
- Sebastia-Forcada, E.; Cebrian-Gomez, R.; Lizaur-Utrilla, A.; Gil-Guillen, V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J. Shoulder Elbow Surg. 2014, 23, 1419–1426. [Google Scholar] [CrossRef] [PubMed]
- Choo, A.; Sobol, G.; Maltenfort, M.; Getz, C.; Abboud, J. Prevalence of rotator cuff tears in operative proximal humerus fractures. Orthopedics 2014, 37, e968–e974. [Google Scholar] [CrossRef]
- Savin, D.D.; Zamfirova, I.; Iannotti, J.; Goldberg, B.A.; Youderian, A.R. Survey study suggests that reverse total shoulder arthroplasty is becoming the treatment of choice for four-part fractures of the humeral head in the elderly. Int. Orthop. 2016, 40, 1919–1925. [Google Scholar] [CrossRef]
- Hao, K.A.; Patch, D.A.; Reed, L.A.; Spitler, C.A.; Horneff, J.G.; Ahn, J.; Strelzow, J.A.; Herbert-Davies, J.; Little, M.T.M.; Krause, P.C.; et al. Factors Influencing Surgical Management of Proximal Humerus Fractures: Do Shoulder and Trauma Surgeons Differ? J. Shoulder Elbow Surg 2021, 31, e259–e269. [Google Scholar] [CrossRef]
- Boyle, M.J.; Youn, S.M.; Frampton, C.M.; Ball, C.M. Functional outcomes of reverse shoulder arthroplasty compared with hemiarthroplasty for acute proximal humeral fractures. J. Shoulder Elbow Surg. 2013, 22, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Gunst, S.; Louboutin, L.; Swan, J.; Lustig, S.; Servien, E.; Nove-Josserand, L. Does healing of both greater and lesser tuberosities improve functional outcome after reverse shoulder arthroplasty for fracture? A retrospective study of twenty-eight cases with a computed tomography scan at a minimum of one-year follow-up. Int. Orthop. 2021, 45, 681–687. [Google Scholar] [CrossRef]
- Rossi, L.A.; Tanoira, I.; Ranalletta, M.; Kunze, K.N.; Farivar, D.; Perry, A.; Chahla, J. Cemented vs. Uncemented Reverse Shoulder Arthroplasty for Proximal Humeral Fractures: A Systematic Review and Meta-analysis. J. Shoulder Elbow Surg. 2021, 31, e101–e119. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Kotha, S.; Huang, C.H.; Mason, J.; Yakimicki, D.; Hawkins, M. Finite element thermal analysis of bone cement for joint replacements. J. Biomech. Eng. 2003, 125, 315–322. [Google Scholar] [CrossRef]
- Eriksson, A.R.; Albrektsson, T. Temperature threshold levels for heat-induced bone tissue injury: A vital-microscopic study in the rabbit. J. Prosthet. Dent. 1983, 50, 101–107. [Google Scholar] [CrossRef]
- Cil, A.; Veillette, C.J.; Sanchez-Sotelo, J.; Sperling, J.W.; Schleck, C.; Cofield, R.H. Revision of the humeral component for aseptic loosening in arthroplasty of the shoulder. J. Bone Jt. Surg. Br. 2009, 91, 75–81. [Google Scholar] [CrossRef]
- Keener, J.D.; Chalmers, P.N.; Yamaguchi, K. The Humeral Implant in Shoulder Arthroplasty. J. Am. Acad. Orthop. Surg. 2017, 25, 427–438. [Google Scholar] [CrossRef]
- Farley, K.X.; Wilson, J.M.; Kumar, A.; Gottschalk, M.B.; Daly, C.; Sanchez-Sotelo, J.; Wagner, E.R. Prevalence of Shoulder Arthroplasty in the United States and the Increasing Burden of Revision Shoulder Arthroplasty. JBJS Open Access 2021, 6, e20.00156. [Google Scholar] [CrossRef]
- Phadnis, J.; Huang, T.; Watts, A.; Krishnan, J.; Bain, G.I. Cemented or cementless humeral fixation in reverse total shoulder arthroplasty? a systematic review. Bone Jt. J. 2016, 98, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Schoch, B.; Aibinder, W.; Walters, J.; Sperling, J.; Throckmorton, T.; Sanchez-Sotelo, J.; Duquin, T. Outcomes of Uncemented Versus Cemented Reverse Shoulder Arthroplasty for Proximal Humerus Fractures. Orthopedics 2019, 42, e236–e241. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.O.; Ho, A.; Kalma, J.; Koueiter, D.; Esterle, J.; Marcantonio, D.; Wiater, J.M.; Wiater, B. Uncemented Reverse Total Shoulder Arthroplasty as Initial Treatment for Comminuted Proximal Humerus Fractures. J. Orthop. Trauma. 2019, 33, e263–e269. [Google Scholar] [CrossRef]
- Youn, S.M.; Deo, S.; Poon, P.C. Functional and radiologic outcomes of uncemented reverse shoulder arthroplasty in proximal humeral fractures: Cementing the humeral component is not necessary. J. Shoulder Elbow Surg. 2016, 25, e83–e89. [Google Scholar] [CrossRef] [PubMed]
- Lo, E.Y.; Rizkalla, J.; Montemaggi, P.; Majekodunmi, T.; Krishnan, S.G. Clinical and radiographic outcomes of cementless reverse total shoulder arthroplasty for proximal humeral fractures. J. Shoulder Elbow Surg. 2021, 30, 1949–1956. [Google Scholar] [CrossRef]
- Rossi, L.A.; Guillermina, B.M.; Buljubasich, M.; Atala, N.; Tanoira, I.; Bongiovanni, S.; Ranalletta, M. Cemented versus uncemented reverse shoulder arthroplasty for acute proximal humeral fractures. J. Shoulder Elbow Surg. 2021, 31, 261–268. [Google Scholar] [CrossRef]
- Neer, C.S., 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J. Bone Jt. Surg. Am. 1970, 52, 1077–1089. [Google Scholar] [CrossRef]
- Boileau, P.; Alta, T.D.; Decroocq, L.; Sirveaux, F.; Clavert, P.; Favard, L.; Chelli, M. Reverse shoulder arthroplasty for acute fractures in the elderly: Is it worth reattaching the tuberosities? J. Shoulder Elbow Surg. 2019, 28, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Sperling, J.W.; Cofield, R.H.; O’Driscoll, S.W.; Torchia, M.E.; Rowland, C.M. Radiographic assessment of ingrowth total shoulder arthroplasty. J. Shoulder Elbow Surg. 2000, 9, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Sirveaux, F.; Favard, L.; Oudet, D.; Huquet, D.; Walch, G.; Mole, D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J. Bone Jt. Surg. Br. 2004, 86, 388–395. [Google Scholar] [CrossRef]
- Gallinet, D.; Clappaz, P.; Garbuio, P.; Tropet, Y.; Obert, L. Three or four parts complex proximal humerus fractures: Hemiarthroplasty versus reverse prosthesis: A comparative study of 40 cases. Orthop. Traumatol. Surg. Res. 2009, 95, 48–55. [Google Scholar] [CrossRef]
- Candela, V.; Gumina, S. Independent destiny of the two tuberosities in patients with complex humeral fractures treated with reverse shoulder arthroplasty and interposition autologous graft. Semin. Arthroplast. JSES 2021, 31, 72–80. [Google Scholar] [CrossRef]
- Harris, T.E.; Jobe, C.M.; Dai, Q.G. Fixation of proximal humeral prostheses and rotational micromotion. J. Shoulder Elbow Surg. 2000, 9, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Van de Kleut, M.L.; Yuan, X.; Athwal, G.S.; Teeter, M.G. Are Short Press-Fit Stems Comparable to Standard Length Cemented Stems in Reverse Shoulder Arthroplasty? A Prospective Randomized Clinical Trial. J. Shoulder Elbow Surg. 2021, 31, 580–590. [Google Scholar] [CrossRef] [PubMed]
- Eyberg, B.A.; Walker, J.B.; Harmsen, S.M.; Gobezie, R.; Denard, P.J.; Lederman, E.S. Suture cerclage for stabilizing the humeral shaft during shoulder arthroplasty. JSES Int. 2020, 4, 688–693. [Google Scholar] [CrossRef]
- Kriechling, P.; Hasler, A.; Passaplan, C.; Wieser, K. Is suture cerclage fixation a valid treatment for intraoperative nondisplaced calcar fractures in reverse total shoulder arthroplasties? JSES Int. 2021, 5, 673–678. [Google Scholar] [CrossRef]
- Michel, P.A.; Katthagen, J.C.; Schliemann, B.; Wilkens, S.; Frank, A.; Heilmann, L.F.; Dyrna, F.; Raschke, M.J. Biomechanical Value of a Protective Proximal Humeral Cerclage in Reverse Total Shoulder Arthroplasty. J. Clin. Med. 2021, 10, 4600. [Google Scholar] [CrossRef]
- Razfar, N.; Reeves, J.M.; Langohr, D.G.; Willing, R.; Athwal, G.S.; Johnson, J.A. Comparison of proximal humeral bone stresses between stemless, short stem, and standard stem length: A finite element analysis. J. Shoulder Elbow Surg. 2016, 25, 1076–1083. [Google Scholar] [CrossRef]
- Peduzzi, L.; Goetzmann, T.; Wein, F.; Roche, O.; Sirveaux, F.; Mole, D.; Jacquot, A. Proximal humeral bony adaptations with a short uncemented stem for shoulder arthroplasty: A quantitative analysis. JSES Open Access 2019, 3, 278–286. [Google Scholar] [CrossRef]
- Denard, P.J.; Noyes, M.P.; Walker, J.B.; Shishani, Y.; Gobezie, R.; Romeo, A.A.; Lederman, E. Proximal stress shielding is decreased with a short stem compared with a traditional-length stem in total shoulder arthroplasty. J. Shoulder Elbow Surg. 2018, 27, 53–58. [Google Scholar] [CrossRef] [PubMed]

| Patients Demographic Characteristics | ||
|---|---|---|
| Data | ||
| With Calcar Fragment | Without Calcar Fragment | |
| Overall, N | 18 | 50 |
| Age, mean ± SD, yr | 69.5 | 70.1 |
| Sex: male/female, n (%) | 3/15 | 17/33 |
| Time from injury to arthroplasty, mean, days | 7.4 | 6.7 |
| Operated side: left/right, n (%) | 7/11 (38/62%) | 24/26 (48/52%) |
| Follow-up, mean, years ± SD | 5.5 ± 0.5 | 6.9 ± 0.7 |
| Comparative Analysis of Postoperative Clinical Outcomes in Proximal Humeral Fractures “With Calcar Fragment” vs. “Without Calcar Fragment” | ||||
|---|---|---|---|---|
| Group A | Group B | |||
| “With Calcar Fragment” | “Without Calcar Fragment” | p Value | ||
| AE | 141° (15°) | 145° (10°) | 0.67 | |
| ER 1 | 49° (15°) | 53° (13°) | 0.55 | |
| ER 2 | 35° (5°) | 33° (5°) | 0.89 | |
| IR | 5 (2) | 6 (2) | 0.97 | |
| NRS pain score | 0.8 (2) | 0.5 (1.5) | 0.58 | |
| SST score | 91.1 (11) | 90.4 (10) | 0.49 | |
| ASES shoulder score | 89.2 (10) | 91.6 (9) | 0.23 | |
| Number and Type of Postoperative Complications Following Reverse Total Shoulder Arthroplasty with Cementless and Metaphyseal Stem’s Fixation for Proximal Humeral Fractures “With Calcar Fragment” vs. “Without Calcar Fragment” | ||||
|---|---|---|---|---|
| Total (n = 19) | “With Calcar Fragment” (n = 5) | “Without Calcar Fragment” (n = 12) | ||
| Tuberosity healing Subsidence | 10 3 | 3 1 | 7 2 | |
| Humeral radiolucency | 2 | 1 | 1 | |
| Scapular notching | 2 | 1 | 1 | |
| Heterotopic ossification | 1 | 0 | 1 | |
| Superficial infection | 1 | 0 | 1 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garofalo, R.; Fontanarosa, A.; Lassandro, N.; De Crescenzo, A. Reverse Total Shoulder Arthroplasty with a Cementless and Metaphyseal Stem Fixation Is a Viable Option for the Treatment of Proximal Humeral Fractures with Calcar Involvement. J. Clin. Med. 2023, 12, 1443. https://doi.org/10.3390/jcm12041443
Garofalo R, Fontanarosa A, Lassandro N, De Crescenzo A. Reverse Total Shoulder Arthroplasty with a Cementless and Metaphyseal Stem Fixation Is a Viable Option for the Treatment of Proximal Humeral Fractures with Calcar Involvement. Journal of Clinical Medicine. 2023; 12(4):1443. https://doi.org/10.3390/jcm12041443
Chicago/Turabian StyleGarofalo, Raffaele, Alberto Fontanarosa, Nunzio Lassandro, and Angelo De Crescenzo. 2023. "Reverse Total Shoulder Arthroplasty with a Cementless and Metaphyseal Stem Fixation Is a Viable Option for the Treatment of Proximal Humeral Fractures with Calcar Involvement" Journal of Clinical Medicine 12, no. 4: 1443. https://doi.org/10.3390/jcm12041443
APA StyleGarofalo, R., Fontanarosa, A., Lassandro, N., & De Crescenzo, A. (2023). Reverse Total Shoulder Arthroplasty with a Cementless and Metaphyseal Stem Fixation Is a Viable Option for the Treatment of Proximal Humeral Fractures with Calcar Involvement. Journal of Clinical Medicine, 12(4), 1443. https://doi.org/10.3390/jcm12041443





