Return to Sport after Adolescent Idiopathic Scoliosis (AIS) Correction Surgery: A Retrospective Data Analysis
Abstract
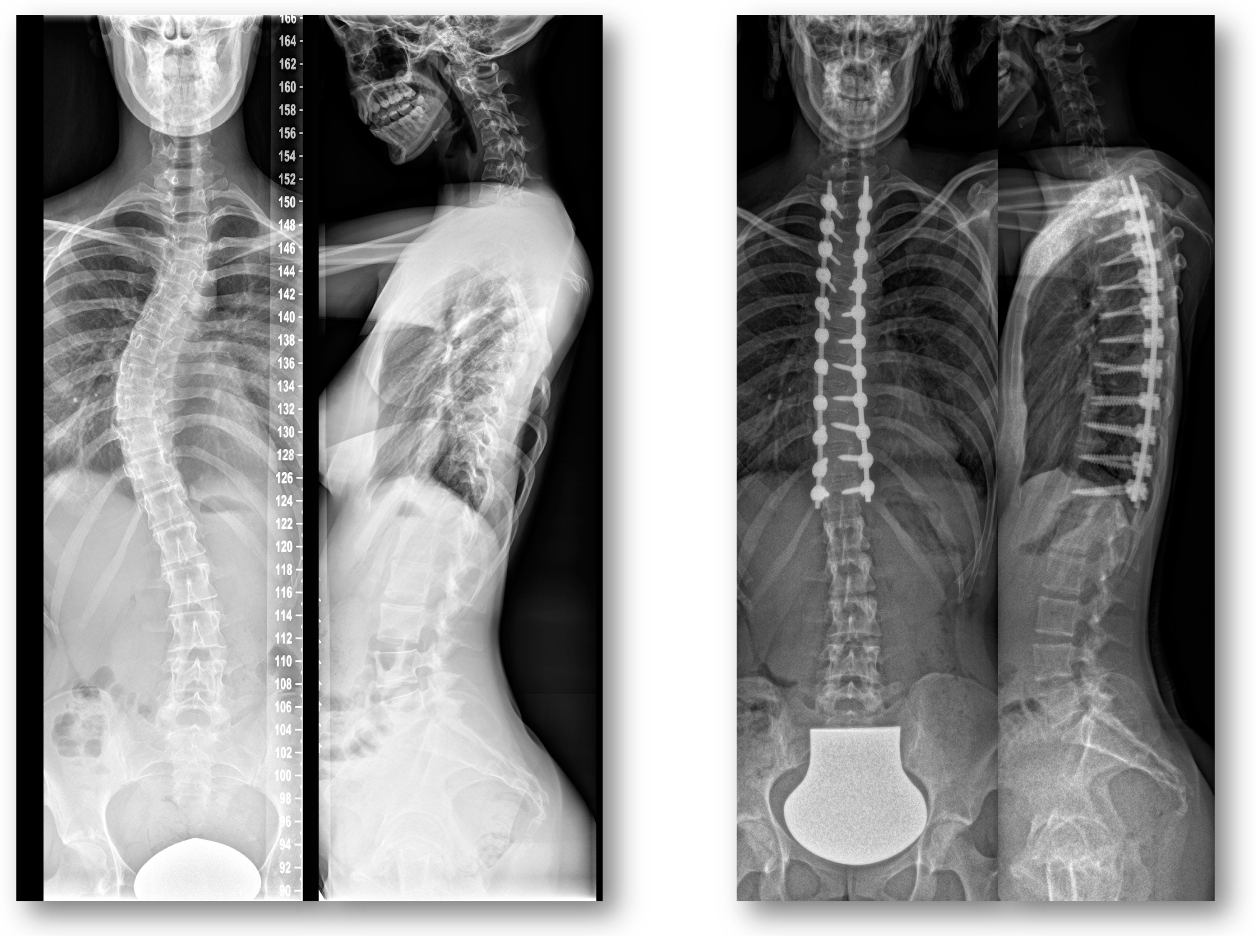
:1. Introduction
2. Materials and Methods
2.1. Study Cohort
2.2. Data Collection and Analysis
2.3. Radiographic Assessment
2.4. Patient Stratification
2.5. Statistical Analysis
3. Results
3.1. Global Analysis
3.2. Sport Activities and Returning to Sports after Surgery
3.3. Stratification by the Length and LIV of the Posterior Spondylodesis
3.4. Clinical Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- White, A.A. Clinical Biomechanics of Cervical Spine Implants. Spine 1989, 14, 1040–1045. [Google Scholar] [CrossRef]
- Bridwell, K.H. Surgical treatment of adolescent idiopathic scoliosis: The basics and the controversies. Spine (Phila Pa 1976) 1994, 19, 1095–1100. [Google Scholar] [CrossRef] [PubMed]
- Bridwell, K.H. Surgical Treatment of Idiopathic Adolescent Scoliosis. Spine 1999, 24, 2607–2616. [Google Scholar] [CrossRef] [PubMed]
- Dickson, R.A. Spinal Deformity—Adolescent Idiopathic Scoliosis. Spine 1999, 24, 2601–2606. [Google Scholar] [CrossRef]
- Maruyama, T.; Takeshita, K. Surgical treatment of scoliosis: A review of techniques currently applied. Scoliosis 2008, 3, 6. [Google Scholar] [CrossRef] [Green Version]
- Harrington, P.R. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J. Bone Joint Surg. Am. 1962, 44, 591–610. [Google Scholar] [CrossRef] [PubMed]
- Betz, R.R.; Harms, J.; Clements, D.H.; Lenke, L.G.; Lowe, T.G.; Shufflebarger, H.L.; Jeszenszky, D.; Beele, B. Comparison of Anterior and Posterior Instrume ntation for Correction of Adolescent Thoracic Idiopathic Scoliosis. Spine 1999, 24, 225–239. [Google Scholar] [CrossRef]
- Muschik, M.T.; Kimmich, H.; Demmel, T. Comparison of anterior and posterior double-rod instrumentation for thoracic idiopathic scoliosis: Results of 141 patients. Eur. Spine J. 2006, 15, 1128–1138. [Google Scholar] [CrossRef]
- Arlet, V. Anterior thoracoscopic spine release in deformity surgery: A meta-analysis and review. Eur. Spine J. 2000, 9, S017–S023. [Google Scholar] [CrossRef] [Green Version]
- Kaneda, K.; Shono, Y.; Satoh, S.; Abumi, K. New Anterior Instrumentation for the Management of Thoracolumbar and Lumbar Scoliosis. Spine 1996, 21, 1250–1261. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Shufflebarger, H.L.; Lenke, L.G.; Lowe, T.G.; Betz, R.R.; Bassett, G.S. Parents’ and patients’ preferences and concerns in idiopathic adolescent scoliosis: A cross-sectional preoperative analysis. Spine (Phila Pa 1976) 2000, 25, 2392–2399. [Google Scholar] [CrossRef]
- White, S.F.; Asher, M.A.; Lai, S.-M.; Burton, D.C. Patients’ Perceptions of Overall Function, Pain, and Appearance After Primary Posterior Instrumentation and Fusion for Idiopathic Scoliosis. Spine 1999, 24, 1693. [Google Scholar] [CrossRef]
- Hopf, C.; Felske-Adler, C.; Heine, J. Recommendations for participation in sports by patients with idiopathic scoliosis. Z. Orthop. Ihre. Grenzgeb. 1991, 129, 204–207. [Google Scholar] [CrossRef]
- Wright, A.; Ferree, B.; Tromanhauser, S. Spinal fusion in the athlete. Clin. Sports Med. 1993, 12, 599–602. [Google Scholar] [PubMed]
- Alsobrook, J.; Clugston, J.R. Return to play after surgery of the lumbar spine. Curr. Sport. Med. Rep. 2008, 7, 45–48. [Google Scholar] [CrossRef]
- Barile, F.; Ruffilli, A.; Manzetti, M.; Fiore, M.; Panciera, A.; Viroli, G.; Faldini, C. Resumption of sport after spinal fusion for adolescent idiopathic scoliosis: A review of the current literature. Spine Deform. 2021, 9, 1247–1251. [Google Scholar] [CrossRef]
- Sarwahi, V.; Wendolowski, S.; Gecelter, R.; Maguire, K.; Gambassi, M.; Orlando, D.; Lo, Y.; Amaral, T. When Do Patients Return to Physical Activities and Athletics After Scoliosis Surgery?: A Validated Patient Questionnaire Based Study. Spine 2018, 43, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Ruffilli, A.; Barile, F.; Viroli, G.; Manzetti, M.; Traversari, M.; Ialuna, M.; Bulzacki Bogucki, B.D.; Faldini, C. Return to sport after posterior spinal fusion for adolescent idiopathic scoliosis: What variables actually have an influence? A retrospective study. Spine Deform. 2022, 10, 1367–1374. [Google Scholar] [CrossRef] [PubMed]
- Lenke, L.G.; Edwards, C.C.; Bridwell, K.H. The Lenke classification of adolescent idiopathic scoliosis: How it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila Pa 1976) 2003, 28, S199–S207. [Google Scholar] [CrossRef]
- Fabricant, P.D.; Admoni, S.H.; Green, D.W.; Ipp, L.S.; Widmann, R.F. Return to athletic activity after posterior spinal fusion for adolescent idiopathic scoliosis: Analysis of independent predictors. J. Pediatr. Orthop. 2012, 32, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Lehman, R.A.; Kang, D.G.; Lenke, L.G.; Sucato, D.J.; Bevevino, A.J. Return to sports after surgery to correct adolescent idiopathic scoliosis: A survey of the Spinal Deformity Study Group. Spine J. 2015, 15, 951–958. [Google Scholar] [CrossRef] [PubMed]
- Parsch, D.; Gärtner, V.; Brocai, D.R.C.; Carstens, C.; Schmitt, H. Sports Activity of Patients with Idiopathic Scoliosis at Long-Term Follow-Up. Clin. J. Sport Med. 2002, 12, 95–98. [Google Scholar] [CrossRef]
- Cochran, T.; Irstam, L.; Nachemson, A. Long-Term Anatomic and Functional Changes in Patients with Adolescent Idiopathic Scoliosis Treated by Harrington Rod Fusion. Spine 1983, 8, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Chotigavanich, C.; Songcharoen, P.; Thanapipatsiri, S. Surgical treatment of adolescent idiopathic scoliosis using Harrington distraction rod combined with segmental sublaminar wiring. J. Med. Assoc. Thail. 1994, 77, 617–626. [Google Scholar]
- Mehta, H.; Santos, E.; Ledonio, C.; Sembrano, J.; Ellingson, A.; Pare, P.; Murrell, B.; Nuckley, D. Biomechanical analysis of pedicle screw thread differential design in an osteoporotic cadaver model. Clin. Biomech. 2012, 27, 234–240. [Google Scholar] [CrossRef]
- Liu, M.-Y.; Tsai, T.-T.; Lai, P.-L.; Hsieh, M.-K.; Chen, L.-H.; Tai, C.-L. Biomechanical comparison of pedicle screw fixation strength in synthetic bones: Effects of screw shape, core/thread profile and cement augmentation. PLoS ONE 2020, 15, e0229328. [Google Scholar] [CrossRef]
- Liljenqvist, U.; Witt, K.A.; Bullmann, V.; Steinbeck, J.; Völker, K. Recommendations on sport activities for patients with idiopathic scoliosis. Sport. Sportschaden 2006, 20, 36–42. [Google Scholar] [CrossRef]
- Rubery, P.T.; Bradford, D.S. Athletic activity after spine surgery in children and adolescents: Results of a survey. Spine (Phila Pa 1976) 2002, 27, 423–427. [Google Scholar] [CrossRef]
- Fekete, T.F.; Mannion, A.F.; Haschtmann, D.; Loibl, M.; Kleinstück, F.; Jeszenszky, D.J. Back Pain and Its Change After Surgery in Adolescents and Young Adults with Idiopathic Scoliosis. Spine Deform. 2019, 7, 754–758. [Google Scholar] [CrossRef]
- Djurasovic, M.; Glassman, S.D.; Sucato, D.J.; Lenke, L.G.; Crawford, C.H.; Carreon, L.Y. Improvement in Scoliosis Research Society-22R Pain Scores After Surgery for Adolescent Idiopathic Scoliosis. Spine 2018, 43, 127–132. [Google Scholar] [CrossRef]
- Bjerkreim, I.; Steen, H.; Brox, J.I. Idiopathic scoliosis treated with Cotrel-Dubousset instrumentation: Evaluation 10 years after surgery. Spine (Phila Pa 1976) 2007, 32, 2103–2110. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Burke, M.C.; Gagnier, J.; Caird, M.S.; Farley, F.A. Comparison of EOSQ-24 and SRS-22 Scores in Congenital Scoliosis: A Preliminary Study. J. Pediatr. Orthop. 2020, 40, e182–e185. [Google Scholar] [CrossRef] [PubMed]





| Pre-Op Contact | Pre-Op Contact/ Non-Contact | Pre-Op Non-Contact | Post-Op Contact | Post-Op Contact/ Non-Contact | Post-Op Non-Contact |
|---|---|---|---|---|---|
| Bicycle (n = 5) | Bicycle (n = 7) | ||||
| Fitness (n = 6) | Fitness (n = 37) | ||||
| Football (n = 11) | Football (n = 4) | ||||
| Horse riding (n = 5) | |||||
| Jogging (n = 7) | |||||
| School sports (n = 12) | School sports (n = 6) | ||||
| Swimming (n = 7) | Swimming (n = 13) | ||||
| Dancing (n = 14) | Dancing (n= 7) | ||||
| Walking (n = 5) | |||||
| Gymnastics (n = 4) |
| Curve Type | Quantity | Percentage |
|---|---|---|
| Main thoracic (Type 1) | 35 | 31.0% |
| Double thoracic (Type 2) | 28 | 24.8% |
| Double major (Type 3) | 20 | 17.7% |
| Triple major (Type 4) | 7 | 6.2% |
| Thoracolumbar/lumbar (Type 5) | 7 | 6.2% |
| Thoracolumbar–main thoracic (Type 6) | 16 | 14.1% |
| Total | 113 | 100.0% |
| UIV | Quantity | Percentage | LIV | Quantity | Percentage |
|---|---|---|---|---|---|
| T2 | 18 | 15.9% | |||
| T3 | 33 | 29.6% | T10 | 2 | 1.8% |
| T4 | 27 | 23.3% | T12 | 18 | 15.9% |
| T5 | 8 | 7.2% | L1 | 15 | 12.2% |
| T6 | 8 | 7.2% | L2 | 16 | 14.1% |
| T7 | 2 | 1.8% | L3 | 41 | 37.2% |
| T9 | 2 | 1.8% | L4 | 19 | 17% |
| T10 | 12 | 10.5% | L5 | 2 | 1.8% |
| T11 | 2 | 1.8% | |||
| T12 | 1 | 0.9% | |||
| Total | 113 | 100.0% | Total | 113 | 100.0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pepke, W.; Madathinakam, A.; Bruckner, T.; Renkawitz, T.; Hemmer, S.; Akbar, M. Return to Sport after Adolescent Idiopathic Scoliosis (AIS) Correction Surgery: A Retrospective Data Analysis. J. Clin. Med. 2023, 12, 1551. https://doi.org/10.3390/jcm12041551
Pepke W, Madathinakam A, Bruckner T, Renkawitz T, Hemmer S, Akbar M. Return to Sport after Adolescent Idiopathic Scoliosis (AIS) Correction Surgery: A Retrospective Data Analysis. Journal of Clinical Medicine. 2023; 12(4):1551. https://doi.org/10.3390/jcm12041551
Chicago/Turabian StylePepke, Wojciech, Abhilash Madathinakam, Tom Bruckner, Tobias Renkawitz, Stefan Hemmer, and Michael Akbar. 2023. "Return to Sport after Adolescent Idiopathic Scoliosis (AIS) Correction Surgery: A Retrospective Data Analysis" Journal of Clinical Medicine 12, no. 4: 1551. https://doi.org/10.3390/jcm12041551
APA StylePepke, W., Madathinakam, A., Bruckner, T., Renkawitz, T., Hemmer, S., & Akbar, M. (2023). Return to Sport after Adolescent Idiopathic Scoliosis (AIS) Correction Surgery: A Retrospective Data Analysis. Journal of Clinical Medicine, 12(4), 1551. https://doi.org/10.3390/jcm12041551








