Smoking Habit and Respiratory Function Predict Patients’ Outcome after Surgery for Lung Cancer, Irrespective of Histotype and Disease Stage
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Identification and Selection
Preoperative Studies
2.2. Surgical Techniques
Surgical, Postsurgical, and Follow-Up Data
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AS | atypical segmentectomy |
| CM-LDC | carbon monoxide lung diffusing capacity |
| COPD | chronic obstructive pulmonary disease |
| CT | computed tomography |
| DFS | disease-free survival |
| EBUS-TBNA | endobronchial ultrasound transbronchial needle aspiration |
| FEV1 | forced expiratory volume during the first second |
| DLCO | diffusing capacity of the lungs for carbon monoxide |
| NSCLC | non-small-cell lung cancer |
| OS | overall survival |
| PET | positron emission tomography |
| AT | typical segementectomy |
| VATS | videothoracoscopy |
References
- Dezube, A.R.; Jaklitsch, M.T. New evidence supporting lung cancer screening with low dose CT surgical implications. Eur. J. Surg. Oncol. 2020, 46, 982–990. [Google Scholar] [CrossRef] [PubMed]
- Hennon, M.; Landreneau, R.J. Role of Segmentectomy in Treatment of Early-Stage Non-Small Cell Lung Cancer. Ann. Surg. Oncol. 2018, 251, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Dai, C.; Shen, J.; Ren, Y.; Zhong, S.; Zheng, H.; He, J.; Xie, D.; Fei, K.; Liang, W.; Jiang, G.; et al. Choice of Surgical Procedure for Patients With Non-Small-Cell Lung Cancer ≤1 cm or >1 to 2 cm Among Lobectomy, Segmentectomy, and Wedge Resection: A Population-Based Study. J. Clin. Oncol. 2016, 34, 3175–3782. [Google Scholar] [CrossRef]
- Saji, H.; Okada, M.; Tsuboi, M.; Nakajima, R.; Suzuki, K.; Aokage, K.; Aoki, T.; Okami, J.; Yoshino, I.; Ito, H.; et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): A multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet 2022, 399, 1607–1617. [Google Scholar] [CrossRef] [PubMed]
- Altorki, N.K.; Wang, X.; Wigle, D.; Gu, L.; Darling, G.; Ashrafi, A.S.; Landrenau, R.; Miller, D.; Liberman, M.; Jones, D.R.; et al. Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: Post-hoc analysis of an international, randomised, phase 3 trial (CALGB/Alliance 140503). Lancet. Resp. Med. 2018, 6, 915–924. [Google Scholar] [CrossRef]
- Mitchell, K.G.; Antonoff, M.B. Encouraging early outcomes in cancer and leukemia group B (CALGB)/Alliance 140503: Patient selection, not extent of resection, is the key to perioperative success. Ann. Transl. Med. 2019, 7 (Suppl. 1), S50. [Google Scholar] [CrossRef]
- Cancer and Leukemia Group B 140503 (2022) A phase III randomized trial of lobectomy versus sublobar resection for small (≤2 cm) peripheral non-small cell lung cancer. Available online: https://clinicaltrials.gov/ct2/show/NCT00499330 (accessed on 31 January 2023).
- Bugge, A.; Lund, M.B.; Brunborg, C.; Solberg, S.; Kongerud, J. Survival After Surgical Resection for Lung Cancer in Patients With Chronic Obstructive Pulmonary Disease. Ann. Thorac. Surg. 2016, 101, 2125–2131. [Google Scholar] [CrossRef] [Green Version]
- Qiang, G.; Liang, C.; Xiao, F.; Yu, Q.; Wen, H.; Song, Z.; Tian, Y.; Shi, B.; Guo, Y.; Liu, D. Impact of chronic obstructive pulmonary disease on postoperative recurrence in patients with resected non-small-cell lung cancer. Int. J. Chron. Obstruct. Pulmon. Dis. 2015, 11, 43–49. [Google Scholar] [CrossRef] [Green Version]
- Sihoe, A.D.L. We Asked the Experts: Minimally Invasive Segmentectomy for Early Stage Lung Cancer-Will it Replace Lobectomy? World J. Surg. 2022. [Google Scholar] [CrossRef]
- Stamatis, G.; Leschber, G.; Schwarz, B.; Brintrup, D.L.; Flossdorf, S.; Passlick, B.; Hecker, E.; Kugler, C.; Eichhorn, M.; Krbek, T.; et al. Survival outcomes in a prospective randomized multicenter Phase III trial comparing patients undergoing anatomical segmentectomy versus standard lobectomy for non-small cell lung cancer up to 2 cm. Lung Cancer 2022, 172, 108–116. [Google Scholar] [CrossRef]
- Bedetti, B.; Bertolaccini, L.; Rocco, R.; Schmidt, J.; Solli, P.; Scarci, M. Segmentectomy versus lobectomy for stage I non-small cell lung cancer: A systematic review and meta-analysis. J. Thorac. Dis. 2017, 9, 1615–1623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, Y.; Wu, S.; Ma, S.; Lyu, Y.; Xu, H.; Deng, L.; Chen, X. Comparison Between Wedge Resection and Lobectomy/Segmentectomy for Early-Stage Non-small Cell Lung Cancer: A Bayesian Meta-analysis and Systematic Review. Ann. Surg. Oncol. 2022, 29, 1868–1879. [Google Scholar] [CrossRef] [PubMed]
- Kearney, D.J.; Lee, T.H.; Reilly, J.J.; DeCamp, M.M.; Sugarbaker, D. J Assessment of operative risk in patients undergoing lung resection. Importance of predicted pulmonary function. Chest 1994, 105, 753–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cukic, V. Preoperative prediction of lung function in pneumonectomy by spirometry and lung perfusion scintigraphy. Acta Inform. Med. 2012, 20, 221–225. [Google Scholar] [CrossRef] [Green Version]
- Mathew, B.; Nag, S.; Agrawal, A.; Ranganathan, P.; Purandare, N.C.; Shah, S.; Puranik, A.; Rangarajan, V. Comparison of predicted postoperative forced expiratory volume in the first second (FEV1) using lung perfusion scintigraphy with observed forced expiratory volume in the first second (FEV1) post lung resection. World J. Nucl. Med. 2020, 19, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Mineo, T.C.; Schillaci, O.; Pompeo, E.; Mineo, D.; Simonetti, G. Usefulness of lung perfusion scintigraphy before lung cancer resection in patients with ventilatory obstruction. Ann. Thorac. Surg. 2006, 82, 1828–1834. [Google Scholar] [CrossRef]
- Reeves, T.; Bates, S.; Sharp, T.; Richardson, K.; Bali, S.; Plumb, J.; Anderson, H.; Prentis, J.; Swart, M.; Levett, D.Z.H.; et al. Cardiopulmonary exercise testing (CPET) in the United Kingdom-a national survey of the structure, conduct, interpretation and funding. Perioper. Med. 2018, 7, 2. [Google Scholar] [CrossRef] [Green Version]
- Levett, D.Z.H.; Jack, S.; Swart, M.; Carlisle, J.; Wilson, J.; Snowden, C.; Riley, M.; Danjoux, G.; Ward, S.A.; Older, P.; et al. Perioperative cardiopulmonary exercise testing (CPET): Consensus clinical guidelines on indications, organization, conduct, and physiological interpretation. Br. J. Anaesth. 2018, 120, 484–500. [Google Scholar] [CrossRef] [Green Version]
- Older, P.O.; Levett, D.Z.H. Cardiopulmonary Exercise Testing and Surgery. Ann. Am. Thorac. Soc. 2017, 14 (Suppl. 1), S74–S83. [Google Scholar] [CrossRef]
- Kodia, K.; Nguyen, D.M.; Villamizar, N.R. Comprehensive narrative review of segmentectomy for lung cancer. Ame Med. J. 2021, 6, 19. [Google Scholar] [CrossRef]
- Jensik, R.J.; Faber, L.P.; Milloy, F.J.; Monson, D.O. Monson. Segmental resection for lung cancer: A fifteen-year experience. J. Thorac. Cardiovasc. Surg. 1973, 66, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Saracino, L.; Bortolotto, C.; Tomaselli, S.; Fraolini, E.; Bosio, M.; Accordino, G.; Agustoni, F.; Abbott, D.M.; Pozzi, E.; Eleftheriou, D.; et al. Integrating data from multidisciplinary Management of Malignant Pleural Mesothelioma: A cohort study. BMC Cancer 2021, 21, 762. [Google Scholar] [CrossRef] [PubMed]
- Swanson, S.J.; White, A. Sublobar resections for lung cancer: Finally, some answers and some more questions? J. Surg. Oncol. 2023, 127, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Godfrey, C.M.; Marmor, H.N.; Lambright, E.S.; Grogan, E.L. Minimally Invasive and Sublobar Resections for Lung Cancer. Surg. Clin. North Am. 2022, 102, 483–492. [Google Scholar] [CrossRef]
- Schlachtenberger, G.; Doerr, F.; Menghesha, H.; Hagmeyer, L.; Bennink, G.; Gaisendrees, C.; Wahlers, T.; Hekmat, K.; Heldwein, M.B. Sublobar resection without staging and lymphadenectomy for ≤2 cm Non-Small Cell Lung Cancer is no adequate therapy. Surg. Oncol. 2022, 44, 101840. [Google Scholar] [CrossRef] [PubMed]
- Smolle, E.; Pichler, M. Non-Smoking-Associated Lung Cancer: A distinct Entity in Terms of Tumor Biology, Patient Characteristics and Impact of Hereditary Cancer Predisposition. Cancers 2019, 11, 204. [Google Scholar] [CrossRef] [Green Version]
- Bonanno, L.; Calabrese, F.; Nardo, G.; Calistri, D.; Tebaldi, M.; Tedaldi, G.; Polo, V.; Vuljan, S.; Favaretto, A.; Conte, P.; et al. Morphological and genetic heterogeneity in multifocal lung adenocarcinoma: The case of a never-smoker woman. Lung Cancer 2016, 96, 52–55. [Google Scholar] [CrossRef]
- Yang, P. Lung cancer in never smokers. Semin. Respir. Crit. Care Med. 2011, 32, 10–21. [Google Scholar] [CrossRef] [Green Version]
- Hao, B.; Li, F.; Wan, X.; Pan, S.; Li, D.; Song, C.; Li, N.; Geng, Q. Squamous cell carcinoma predicts worse prognosis than adenocarcinoma in stage IA lung cancer patients: A population-based propensity score matching analysis. Front. Surg. 2022, 9, 944032. [Google Scholar] [CrossRef]
- Yang, Y.; Shen, C.; Shao, J.; Wang, Y.; Wang, G.; Shen, A. Based on the Development and Verification of a Risk Stratification Nomogram: Predicting the Risk of Lung Cancer-Specific Mortality in Stage IIIA-N2 Unresectable Large Cell Lung Neuroendocrine Cancer Compared With Lung Squamous Cell Cancer and Lung Adenocarcinoma. Front. Oncol. 2022, 12, 825598. [Google Scholar] [CrossRef]

| (A) | ||||||
|---|---|---|---|---|---|---|
| Lobectomy | % | Typical SG | % | Atypical SG | % | |
| Mean Age at Diagnosis (yrs) | 68.5 (9.02) | 70.8 (6.71) | 71.58 (8.98) | |||
| Males | 60 | 58.25% | 14 | 53.85% | 17 | 70.83% |
| Females | 43 | 41.75% | 12 | 46.15% | 7 | 29.17% |
| 103 | 100.00% | 26 | 100.00% | 24 | 100.00% | |
| Smokers | 85 | 82.52% | 22 | 84.62% | 23 | 95.83% |
| Never smokers | 18 | 17.48% | 4 | 15.38% | 1 | 4.17% |
| Comorbidities | ||||||
| Pneumopathy | 40 | 38.83% | 19 | 73.08% | 12 | 50.00% |
| Cardiopathy | 38 | 36.89% | 15 | 57.69% | 12 | 50.00% |
| Vasculopathy | 35 | 33.98% | 10 | 38.46% | 11 | 45.83% |
| Previous neoplastic disease | 27 | 26.21% | 9 | 34.62% | 10 | 41.67% |
| Previous hematologic cancer | 9 | 8.74% | 3 | 11.54% | 2 | 8.33% |
| Others | 51 | 49.51% | 9 | 34.62% | 10 | 41.67% |
| Disease stage | ||||||
| IA | 77 | 65.3% | 20 | 17% | 21 | 17.7% |
| IA1 | 26 | 18.45% | 6 | 7.69% | 3 | 16.67% |
| IA2 | 38 | 36.89% | 12 | 46.15% | 10 | 41.67% |
| IA3 | 20 | 19.42% | 6 | 23.08% | 7 | 29.17% |
| IB | 26 | 25.24% | 6 | 23.08% | 3 | 12.50% |
| 103 | 100.00% | 26 | 100.00% | 24 | 100.00% | |
| Histotype | ||||||
| Adenocarcinoma | 88 | 338.46% | 21 | 350.00% | 18 | 600.00% |
| Squamous cell carcinoma | 15 | 57.69% | 5 | 83.33% | 6 | 200.00% |
| 103 | 396.15% | 26 | 433.33% | 24 | 800.00% | |
| Relapses | ||||||
| IA | 10/77 | 13 | 4/20 | 20 | 6/21 | 28.6 |
| IB | 6/26 | 23 | 1/6 | 16.6 | 1/3 | 33.3 |
| 16/103 | 15.5% | 5/26 | 19.2% | 7/24 | 29.2% | |
| (B) | ||||||
| Year | 1 | 2 | 3 | 1 | 2 | 3 |
| Disease-Free Survival (DFS) % | Overall Survival (OS) % | |||||
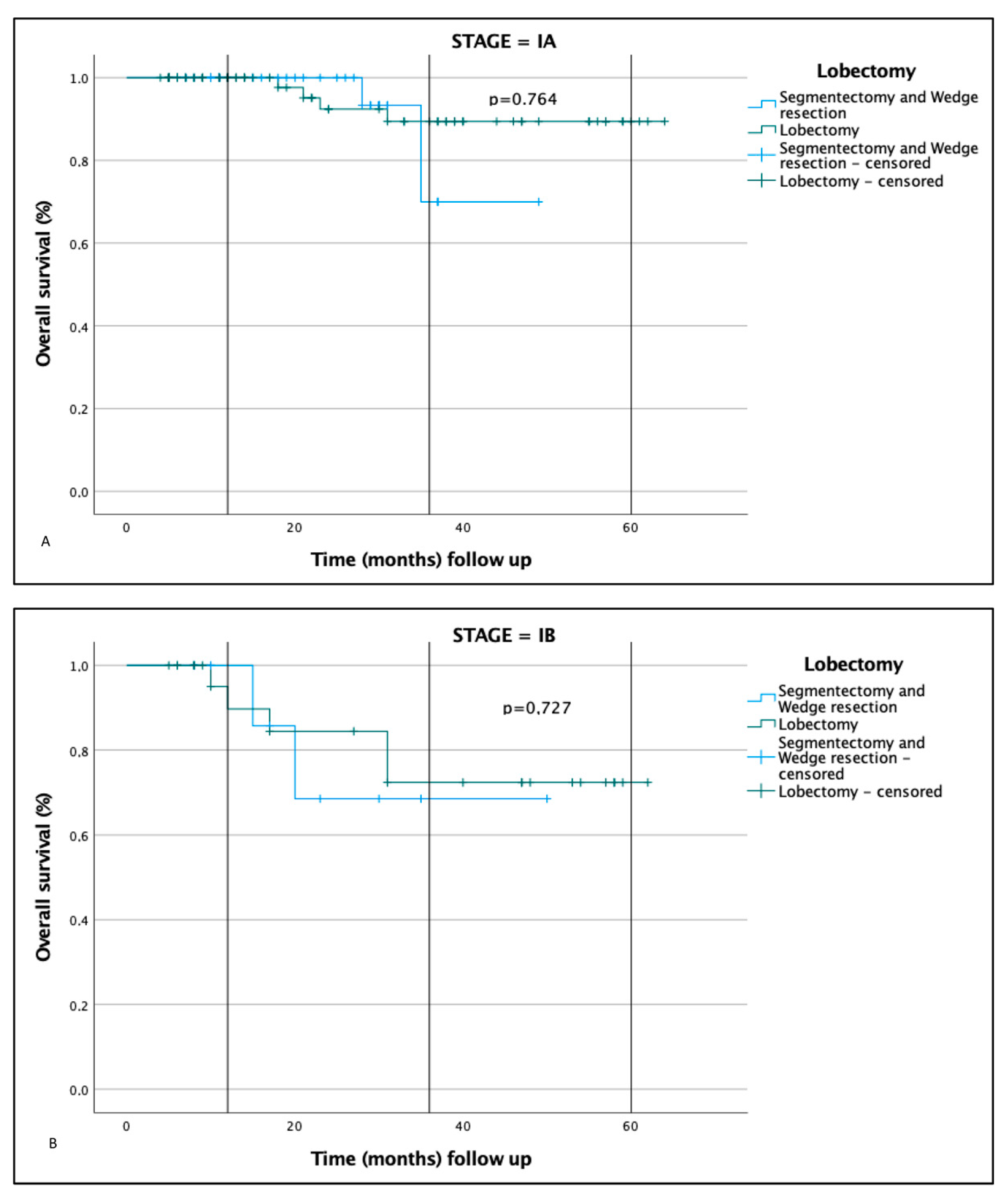
| Whole data | 91 | 77 | 57 | 97 | 83 | 83 |
| Stage | ||||||
| IA | 93 | 79 | 54 | 100 | 87.6 | 87.6 |
| IB | 90 | 69 | 69 | 96.4 | 70.5 | 70.5 |
| Surgery | ||||||
| Lobectomy | 97.5 | 81-4 | 62.2 | 97 | 84.5 | 84.5 |
| Segmentectomy | 82 | 77.7 | 60 | 100 | 94 | 94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piloni, D.; Bertuccio, F.R.; Primiceri, C.; Rinaldi, P.; Chino, V.; Abbott, D.M.; Sottotetti, F.; Bortolotto, C.; Agustoni, F.; Saddi, J.; et al. Smoking Habit and Respiratory Function Predict Patients’ Outcome after Surgery for Lung Cancer, Irrespective of Histotype and Disease Stage. J. Clin. Med. 2023, 12, 1561. https://doi.org/10.3390/jcm12041561
Piloni D, Bertuccio FR, Primiceri C, Rinaldi P, Chino V, Abbott DM, Sottotetti F, Bortolotto C, Agustoni F, Saddi J, et al. Smoking Habit and Respiratory Function Predict Patients’ Outcome after Surgery for Lung Cancer, Irrespective of Histotype and Disease Stage. Journal of Clinical Medicine. 2023; 12(4):1561. https://doi.org/10.3390/jcm12041561
Chicago/Turabian StylePiloni, Davide, Francesco R. Bertuccio, Cristiano Primiceri, Pietro Rinaldi, Vittorio Chino, David Michael Abbott, Federico Sottotetti, Chandra Bortolotto, Francesco Agustoni, Jessica Saddi, and et al. 2023. "Smoking Habit and Respiratory Function Predict Patients’ Outcome after Surgery for Lung Cancer, Irrespective of Histotype and Disease Stage" Journal of Clinical Medicine 12, no. 4: 1561. https://doi.org/10.3390/jcm12041561
APA StylePiloni, D., Bertuccio, F. R., Primiceri, C., Rinaldi, P., Chino, V., Abbott, D. M., Sottotetti, F., Bortolotto, C., Agustoni, F., Saddi, J., & Stella, G. M. (2023). Smoking Habit and Respiratory Function Predict Patients’ Outcome after Surgery for Lung Cancer, Irrespective of Histotype and Disease Stage. Journal of Clinical Medicine, 12(4), 1561. https://doi.org/10.3390/jcm12041561







