Effects of Prenatal Paracetamol Exposure on the Development of Asthma and Wheezing in Childhood: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
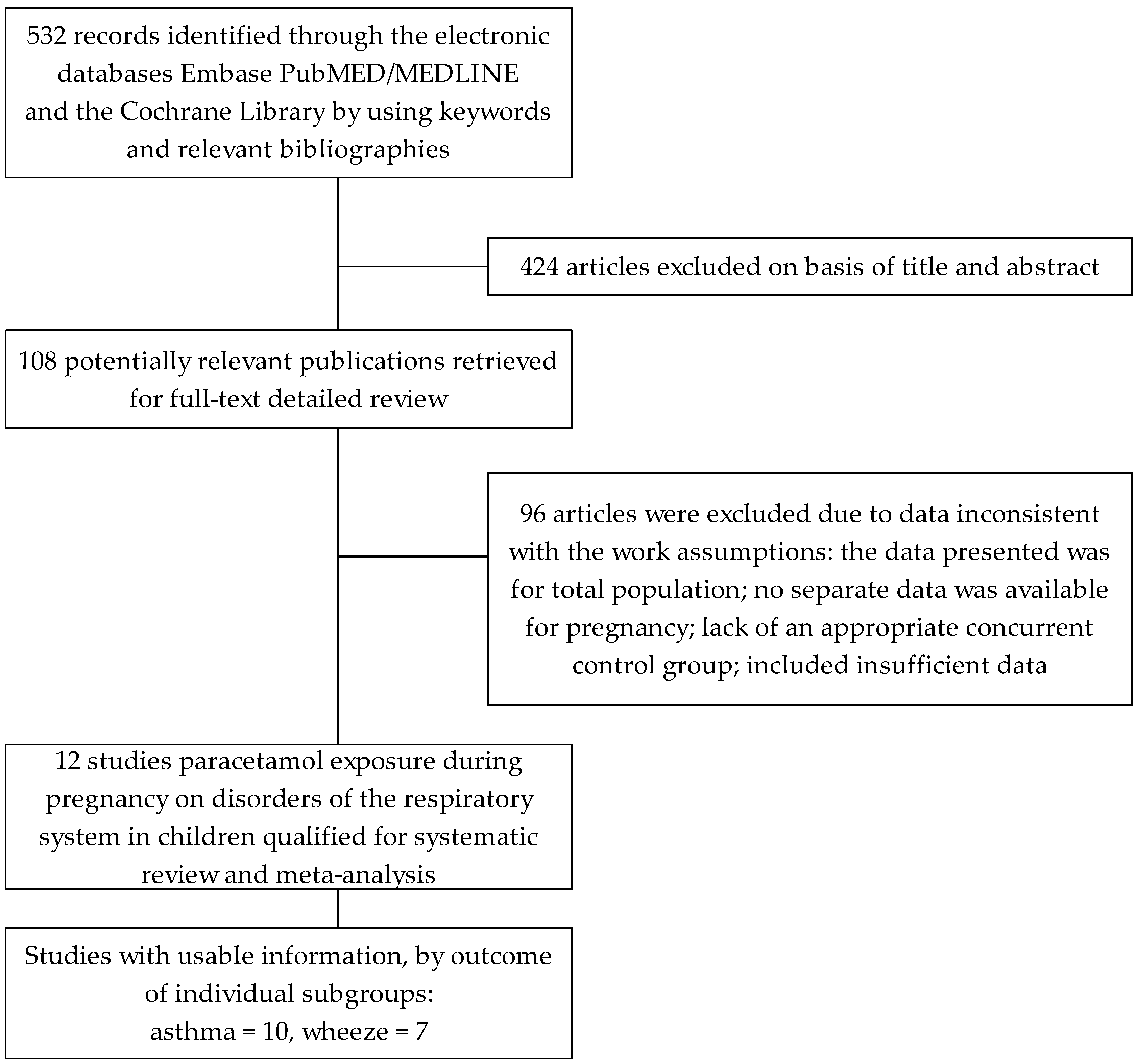
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Abstraction
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Sensitivity Analysis
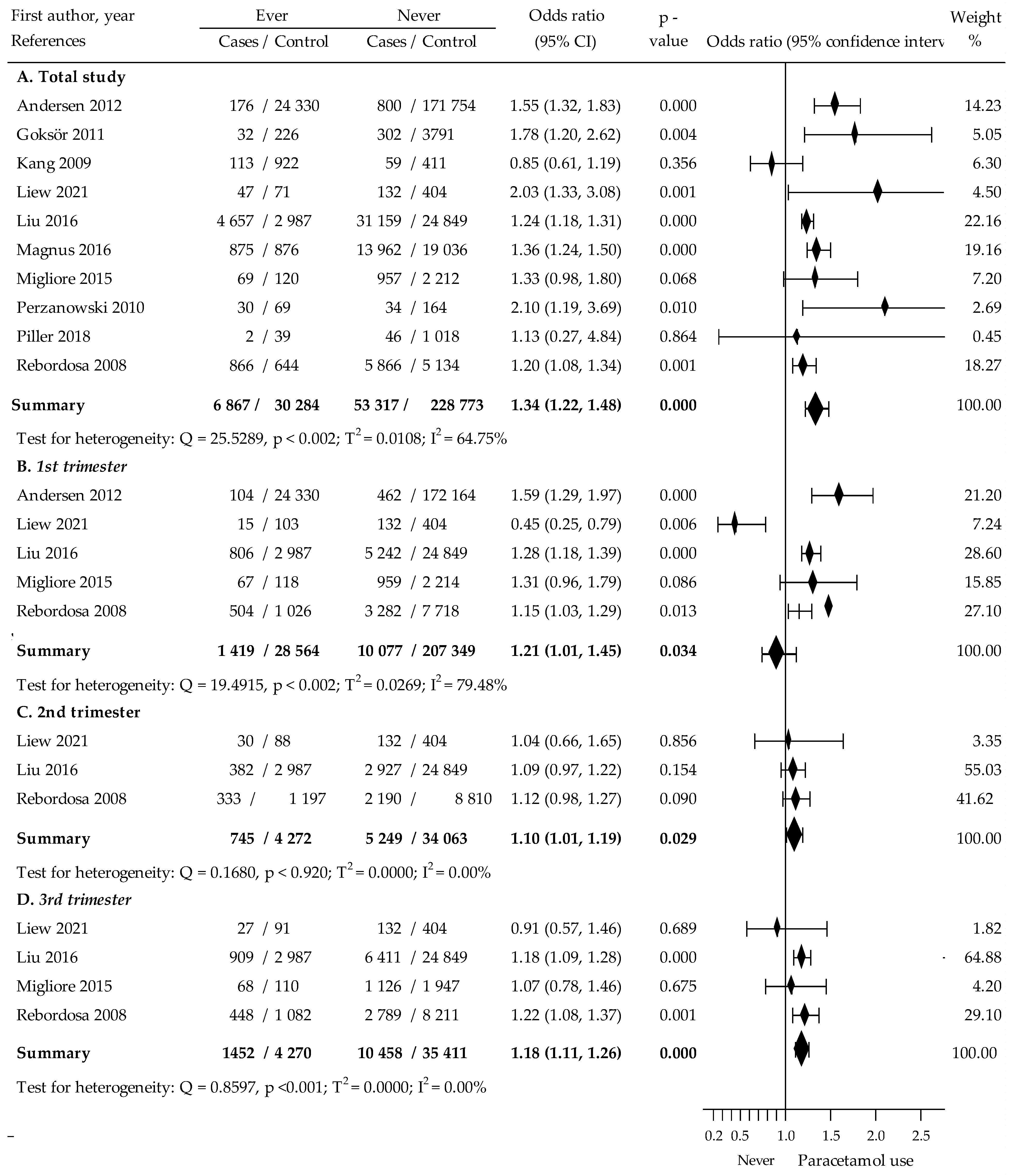
3.2. Association between Paracetamol Exposure during Pregnancy and Asthma in Children
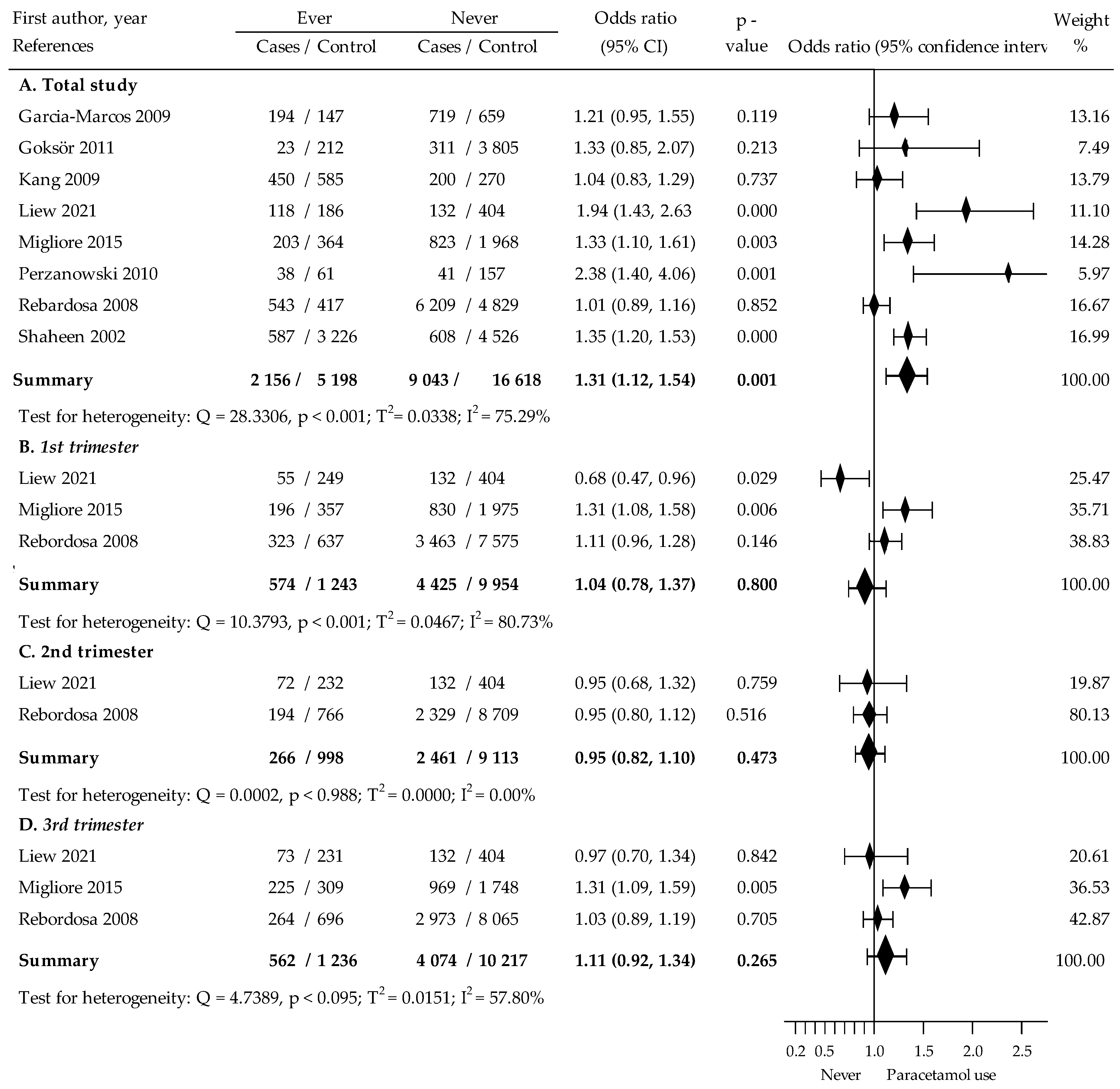
3.3. Association between Paracetamol Exposure during Pregnancy and Wheezing in Children
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mazaleuskaya, L.L.; Sangkuhl, K.; Thorn, C.F.; FitzGerald, G.A.; Altman, R.B.; Klein, T.E. PharmGKB summary: Pathways of acetaminophen metabolism at the therapeutic versus toxic doses. Pharm. Genom. 2015, 25, 416–426. [Google Scholar] [CrossRef] [PubMed]
- McCrae, J.C.; Morrison, E.E.; MacIntyre, I.M.; Dear, J.W.; Webb, D.J.B. Long-term adverse effects of paracetamol-a review. Br. J. Clin. Pharmacol. 2018, 84, 2218–2230. [Google Scholar] [CrossRef] [PubMed]
- Nuttall, S.L.; Khan, J.N.; Thorpe, G.H.; Langford, N.; Kendall, M.J. The impact of therapeutic doses of paracetamol on serum total antioxidant capacity. J. Clin. Pharm. Ther. 2003, 28, 289–294. [Google Scholar] [CrossRef]
- Williams, M.A. Pregnancy complications. In Reproductive and Perinatal Epidemiology; Louis, G.M.B., Platt, R.W., Eds.; Oxford University Press: London, UK, 2011; pp. 101–128. [Google Scholar]
- Lupattelli, A.; Spigset, O.; Twigg, M.J.; Zagorodnikova, K.; Mårdby, A.C.; Moretti, M.E.; Drozd, M.; Panchaud, A.; Hämeen-Anttila, K.; Rieutord, A.; et al. Medication use in pregnancy: A cross-sectional, multinational web-based study. BMJ Open 2014, 4, e004365. [Google Scholar] [CrossRef] [PubMed]
- Ishitsuka, Y.; Kondo, Y.; Kadowaki, D. Toxicological Property of Acetaminophen: The Dark Side of a Safe Antipyretic/Analgesic Drug? Biol. Pharm. Bull. 2020, 43, 195–206. [Google Scholar] [CrossRef] [PubMed]
- Ryu, R.; Hebert, M.F. Impact of pregnancy on maternal pharmacokinetics of medications. In Clinical Pharmacology during Pregnancy; Academic Press: Cambridge, MA, USA, 2022; pp. 19–46. [Google Scholar] [CrossRef]
- Pacifici, G.M.; Allegaert, K. Clinical Pharmacology of Paracetamol in Neonates: A Review. Curr. Ther. Res. 2015, 77, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Mian, P.; Allegaert, K.; Conings, S.; Annaert, P.; Tibboel, D.; Pfister, M.; van Calsteren, K.; Anker, J.N.V.D.; Dallmann, A. Integration of Placental Transfer in a Fetal–Maternal Physiologically Based Pharmacokinetic Model to Characterize Acetaminophen Exposure and Metabolic Clearance in the Fetus. Clin. Pharmacokinet. 2020, 59, 911–925. [Google Scholar] [CrossRef]
- Nitsche, J.F.; Patil, A.S.; Langman, L.J.; Penn, H.J.; Derleth, D.; Watson, W.J.; Brost, B.C. Transplacental Passage of Acetaminophen in Term Pregnancy. Am. J. Perinatol. 2017, 34, 541–543. [Google Scholar] [CrossRef]
- Chiew, A.L.; Gluud, C.; Brok, J.; Buckley, N.A. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst. Rev. 2018, 23, CD003328. [Google Scholar] [CrossRef]
- Rahman, I.; MacNee, W. Oxidative stress and regulation of glutathione in lung inflammation. Eur. Respir. J. 2000, 16, 534–554. [Google Scholar] [CrossRef]
- Hehua, Z.; Qing, C.; Shanyan, G.; Qijun, W.; Yuhong, Z. The impact of prenatal exposure to air pollution on childhood wheezing and asthma: A systematic review. Environ. Res. 2017, 159, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials revisited. Contemp. Clin. Trials 2015, 45, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Liew, Z.; Yuan, Y.; Meng, Q.; von Ehrenstein, O.S.; Cui, X.; Flores, M.E.S.; Ritz, B. Prenatal Exposure to Acetaminophen and Childhood Asthmatic Symptoms in a Population-Based Cohort in Los Angeles, California. Int. J. Environ. Res. Public Health 2021, 18, 10107. [Google Scholar] [CrossRef]
- Piler, P.; Švancara, J.; Kukla, L.; Pikhart, H. Role of combined prenatal and postnatal paracetamol exposure on asthma development: The Czech ELSPAC study. J. Epidemiol. Community Health 2018, 72, 349–355. [Google Scholar] [CrossRef]
- Magnus, M.C.; Karlstad, Ø.; Håberg, S.E.; Nafstad, P.; Smith, G.D.; Nystad, W. Prenatal and infant parace-tamol exposure and development of asthma: The Norwegian Mother and Child Cohort Study. Int. J. Epidemiol. 2016, 45, 512–522. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Liew, Z.; Olsen, J.; Pedersen, L.H.; Bech, B.H.; Agerbo, E.; Yuan, W.; Li, J. Association of prenatal exposure to acetaminophen and coffee with childhood asthma. Pharmacoepidemiol. Drug Saf. 2016, 25, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Migliore, E.; Zugna, D.; Galassi, C.; Merletti, F.; Gagliardi, L.; Rasero, L.; Trevisan, M.; Rusconi, F.; Richiardi, L. Prenatal Paracetamol Exposure and Wheezing in Childhood: Causation or Confounding? PLoS ONE 2015, 10, e0135775. [Google Scholar] [CrossRef] [PubMed]
- Andersen, A.B.; Farkas, D.K.; Mehnert, F.; Ehrenstein, V.; Erichsen, R. Use of prescription paracetamol during pregnancy and risk of asthma in children: A population-based Danish cohort study. Clin. Epidemiol. 2012, 4, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Goksör, E.; Thengilsdottir, H.; Alm, B.; Norvenius, G.; Wennergren, G. Prenatal paracetamol exposure and risk of wheeze at preschool age. Acta Paediatr. 2011, 100, 1567–1571. [Google Scholar] [CrossRef] [PubMed]
- Perzanowski, M.S.; Miller, R.L.; Tang, D.; Ali, D.; Garfinkel, R.S.; Chew, G.L.; Goldstein, I.F.; Perera, F.P.; Barr, R.G. Prenatal acetaminophen exposure and risk of wheeze at age 5 years in an urban low-income cohort. Thorax 2010, 65, 118–123. [Google Scholar] [CrossRef]
- Kang, E.M.; Lundsberg, L.S.; Illuzzi, J.L.; Bracken, M.B. Prenatal Exposure to Acetaminophen and Asthma in Children. Obstet. Gynecol. 2009, 114, 1295–1306. [Google Scholar] [CrossRef]
- Garcia-Marcos, L.; Sanchez-Solis, M.; Perez-Fernandez, V.; Pastor-Vivero, M.D.; Mondejar-Lopez, P.; Valverde-Molina, J. Is the effect of prenatal paracetamol exposure on wheezing in preschool children modified by asthma in the mother? Int. Arch. Allergy Immunol. 2009, 149, 33–37. [Google Scholar] [CrossRef]
- Rebordosa, C.; Kogevinas, M.; Sørensen, H.T.; Olsen, J. Pre-natal exposure to paracetamol and risk of wheezing and asthma in children: A birth cohort study. Int. J. Epidemiol. 2008, 37, 583–590. [Google Scholar] [CrossRef]
- Shaheen, S.O.; Newson, R.B.; Sherriff, A.; Henderson, A.J.; Heron, J.E.; Burney, P.G.J.; Golding, J.; ALSPAC Study Team. Paracetamol use in pregnancy and wheezing in early childhood. Thorax 2002, 57, 958–963. [Google Scholar] [CrossRef]
- Singh, M.; Varukolu, S.; Chauhan, A.; Jaiswal, N.; Pradhan, P.; Mathew, J.L.; Singh, M. Paracetamol exposure and asthma: What does the evidence say? An overview of systematic reviews. Pediatr. Pulmonol. 2021, 56, 3189–3199. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Wang, B.; Liu, C.; Li, D. Prenatal paracetamol use and asthma in childhood: A systematic review and meta-analysis. Allergol. Immunopathol. 2017, 45, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Eyers, S.; Weatherall, M.; Jefferies, S.; Beasley, R. Paracetamol in pregnancy and the risk of wheezing in offspring: A systematic review and meta-analysis. Clin. Exp. Allergy 2011, 41, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Sujan, A.C.; Quinn, P.D.; Rickert, M.E.; Wiggs, K.K.; Lichtenstein, P.; Larsson, H.; Almqvist, C.; Öberg, A.S.; D’Onofrio, B.M. Maternal prescribed opioid analgesic use during pregnancy and associations with adverse birth outcomes: A population-based study. PLoS Med. 2019, 16, e1002980. [Google Scholar] [CrossRef] [PubMed]
- de Fays, L.; Van Malderen, K.; De Smet, K.; Sawchik, J.; Verlinden, V.; Hamdani, J.; Dogné, J.-M.; Dan, B. Use of paracetamol during pregnancy and child neurological development. Dev. Med. Child Neurol. 2015, 57, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Arneja, J.; Hung, R.J.; Seeto, R.A.; Knight, J.A.; Hewko, S.L.; Bocking, A.; Lye, S.J.; Brooks, J.D. Association between maternal acetaminophen use and adverse birth outcomes in a pregnancy and birth cohort. Pediatr. Res. 2020, 87, 1263–1269. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.M.D.; Waldie, K.E.; Wall, C.R.; Murphy, R.; Mitchell, E.A.; ABC Study Group. Associations between Acetaminophen Use during Pregnancy and ADHD Symptoms Measured at Ages 7 and 11 Years. PLoS ONE 2014, 9, e108210. [Google Scholar] [CrossRef] [PubMed]
- Liew, Z.; Ritz, B.; Rebordosa, C.; Lee, P.-C.; Olsen, J. Acetaminophen Use during Pregnancy, Behavioral Problems, and Hyperkinetic Disorders. JAMA Pediatr. 2014, 168, 313–320. [Google Scholar] [CrossRef]
- Cooper, M.; Langley, K.; Thapar, A. Antenatal acetaminophen use and attention-deficit/hyperactivity disorder: An interesting observed association but too early to infer causality. JAMA Pediatr. 2014, 168, 306–307. [Google Scholar] [CrossRef]
- Bauer, A.Z.; Swan, S.H.; Kriebel, D.; Liew, Z.; Taylor, H.S.; Bornehag, C.-G.; Andrade, A.M.; Olsen, J.; Jensen, R.H.; Mitchell, R.T.; et al. Paracetamol use during pregnancy—A call for precautionary action. Nat. Rev. Endocrinol. 2021, 17, 757–766. [Google Scholar] [CrossRef]
| Author, Year Country | Study | Exposure Classification Research Period (Years) | The Children’s Respiratory Disorders | Age of Children’s Diagnosis | Population: Paracetamol Use | Child With Asthma or Wheezing | Outcome Period (Months) | Nos Scale | |
|---|---|---|---|---|---|---|---|---|---|
| Studies Included in Meta-Analysis | |||||||||
| 1. | Liew [22], 2021 USA | Environment and Pregnancy Outcomes Study Cohort study | Paracetamol use during pregnancy: 1st trimester, 2nd trimester, 3rd trimester, ever. 2003–2007 | Asthma: diagnosed by medical professional Wheezing | early childhood | 958 | Asthma: 118 Wheeze: 304 | 48 | 9 |
| 2. | Piler [23], 2018 Czech Republic/Brno and Znojmo regions | Czech European Longitudinal Study of Pregnancy and Childhood | Paracetamol use during pregnancy. 1991–1992 | Paediatrician-diagnosed asthma | 3, 5, 7 and 11 years | 1105 | Asthma: 41 | 132 | 9 |
| 3. | Magnus [24], 2016 Norway | Norwegian Mother and Child Cohort Study | Paracetamol use during pregnancy. 1999–2014 | Childhood asthma | 3 years; 7 years | 34,703 | Asthma: 1751 | 36 | 9 |
| 4. | Liu [25], 2016 Denmark | Danish National Birth Cohort | Paracetamol use during pregnancy: 1st trimester, 2nd trimester, 3rd trimester, ever. 1996–2010 | Asthma: at least two prescriptions for inhalants or cases diagnosed by a hospital doctor. | 3 years or later | 63,652 | Asthma: 7644 | 36 | 8 |
| 5. | Migliore [26], 2015 Italy | Nascita e INFanzia: Effeti dell Ambiente study | Paracetamol use during pregnancy: 1st trimester, 3rd trimester. 2005–2013 | Asthma: diagnosed by doctor Wheezing or whistling: at least one episode | 18 months | 3358 | Asthma: 185 Wheeze 535 | 18 | 7 |
| 6. | Andersen [27], 2012 Denmark | Danish Medical Birth Registry | Paracetamol use during pregnancy: 1st trimester, both 2nd and 3rd trimesters, ever. 1996–2008 | Asthma: hospital diagnosed, anti-asthmatic drug prescription | median—6.8 years | 197,060 | Asthma: 24,506 | ~82 | 8 |
| 7. | Goksör [28], 2011 Sweden | Swedish Medical Birth Register | Paracetamol use during pregnancy. 2003 | Asthma: Inhaled corticosteroid-treated Wheezing: three or more episodes | 6, 12 months and 4, 5 years | 4496 | Asthma: 258 Wheeze: 235 | 54 | 7 |
| 8. | Perzanowski [29], 2010 USA | Columbia Center for Children’s Environmental Health | Paracetamol used during pregnancy by low-income women. 1998–2006 | Asthma: self-reported Wheezing: self-reported | 5 years | 297 | Asthma: 99 Wheeze: 99 | 60 | 7 |
| 9. | Kang [30], 2009 USA | The Yale Study | Paracetamol used in 1st and 3rd trimesters pregnancy. 1997–2000 | Asthma: diagnosed by a doctor or health professional | 6 years +/− 3 months | 1505 | Asthma: 172 | 72 | 7 |
| 10. | Garcia-Marcos [31], 2009 Spain | Murcia (Spain) Study | Paracetamol use during pregnancy. | Wheezing: self-reported | 4.08 +/− 0.8 (3–4 years) | 1741 | Wheeze: 341 | 36–60 | 8 |
| 11. | Rebordosa [32], 2008 Denmark | Danish National Birth Cohort study | Paracetamol use during pregnancy: 1st trimester, 2nd trimester, 3rd trimester, ever. 1996–2003 | Asthma: symptoms reported, physician-diagnosedWheezing: self-reported | 18 months—wheeze; 7 years—asthma | 12,733 | Asthma: 12,530 Wheeze: 11,980 | 84 | 9 |
| 12. | Saheen [33], 2002 UK | Avon Longitudinal Study of Parents and Children | Paracetamol use during pregnancy. 1992–1999 | Wheezing: self-reported | 30–42 months | 8942 | Wheeze: 1195 | 30–42 | 9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barańska, A.; Kanadys, W.; Wdowiak, A.; Malm, M.; Błaszczuk, A.; Religioni, U.; Wdowiak-Filip, A.; Polz-Dacewicz, M. Effects of Prenatal Paracetamol Exposure on the Development of Asthma and Wheezing in Childhood: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 1832. https://doi.org/10.3390/jcm12051832
Barańska A, Kanadys W, Wdowiak A, Malm M, Błaszczuk A, Religioni U, Wdowiak-Filip A, Polz-Dacewicz M. Effects of Prenatal Paracetamol Exposure on the Development of Asthma and Wheezing in Childhood: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(5):1832. https://doi.org/10.3390/jcm12051832
Chicago/Turabian StyleBarańska, Agnieszka, Wiesław Kanadys, Artur Wdowiak, Maria Malm, Agata Błaszczuk, Urszula Religioni, Anita Wdowiak-Filip, and Małgorzata Polz-Dacewicz. 2023. "Effects of Prenatal Paracetamol Exposure on the Development of Asthma and Wheezing in Childhood: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 5: 1832. https://doi.org/10.3390/jcm12051832
APA StyleBarańska, A., Kanadys, W., Wdowiak, A., Malm, M., Błaszczuk, A., Religioni, U., Wdowiak-Filip, A., & Polz-Dacewicz, M. (2023). Effects of Prenatal Paracetamol Exposure on the Development of Asthma and Wheezing in Childhood: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(5), 1832. https://doi.org/10.3390/jcm12051832









