Discriminating Healthy Optic Discs and Visible Optic Disc Drusen on Fundus Autofluorescence and Color Fundus Photography Using Deep Learning—A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
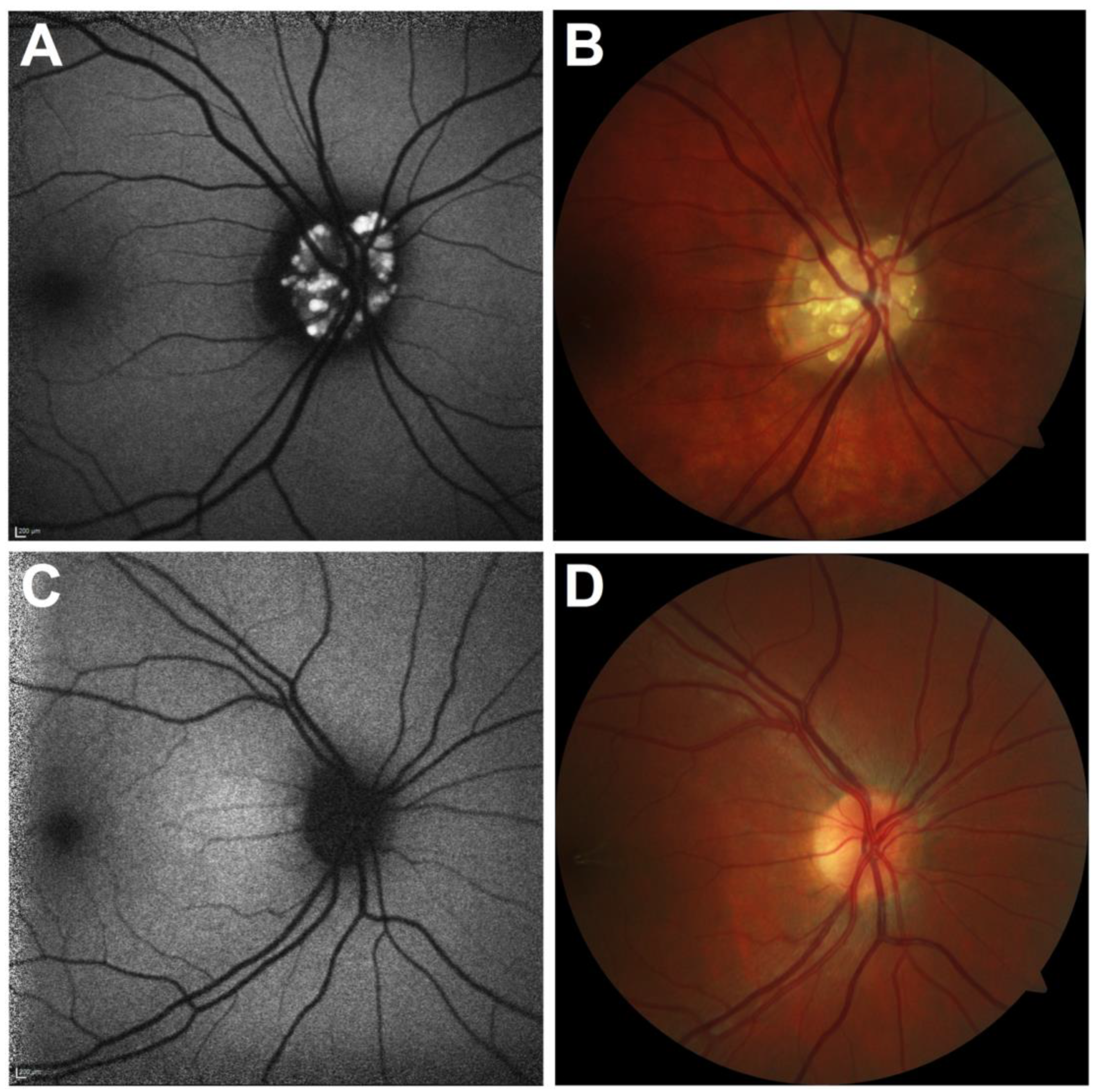
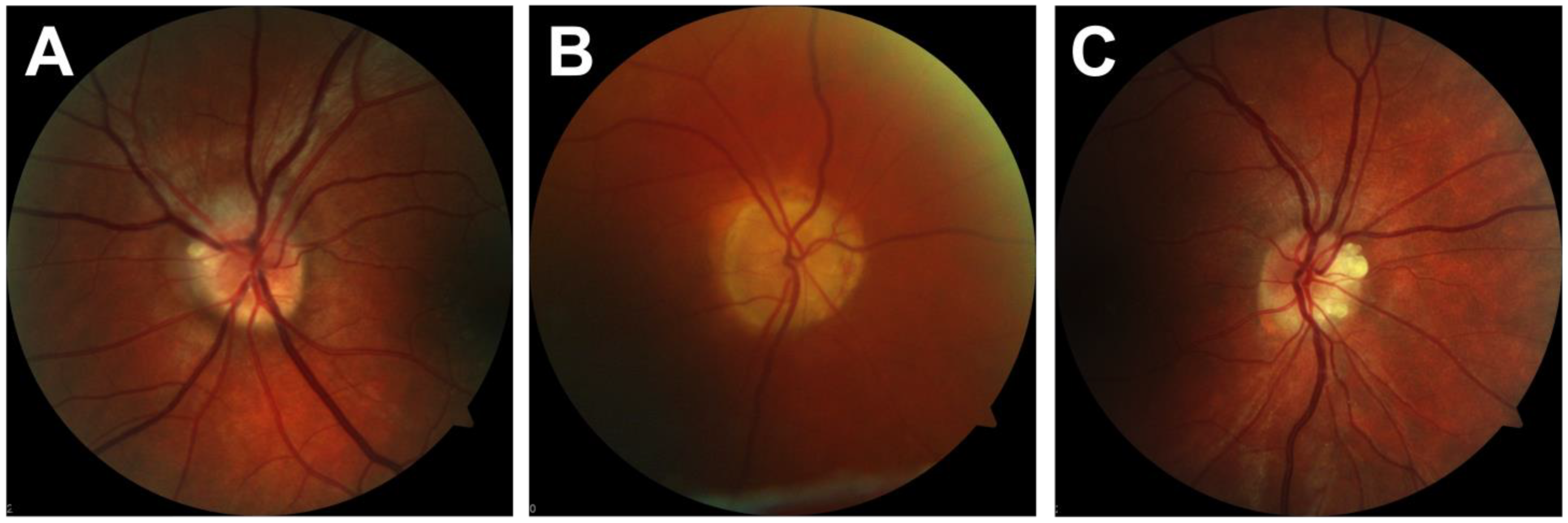
2.1. Patient and Image Selection
2.2. Deep Learning
2.3. Statistics
3. Results
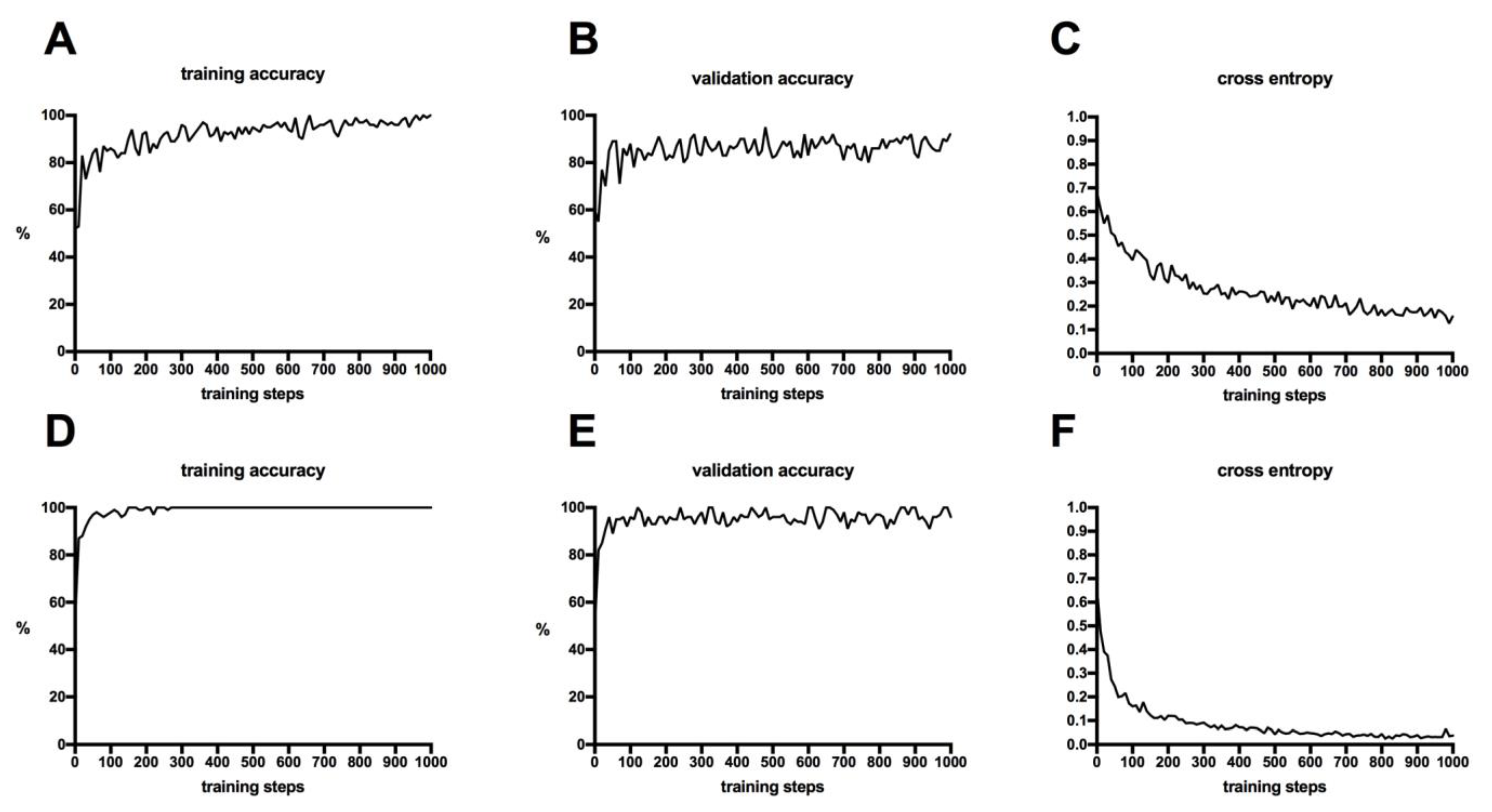
3.1. Performance of the Training Process
3.2. Testing of the Classifiers
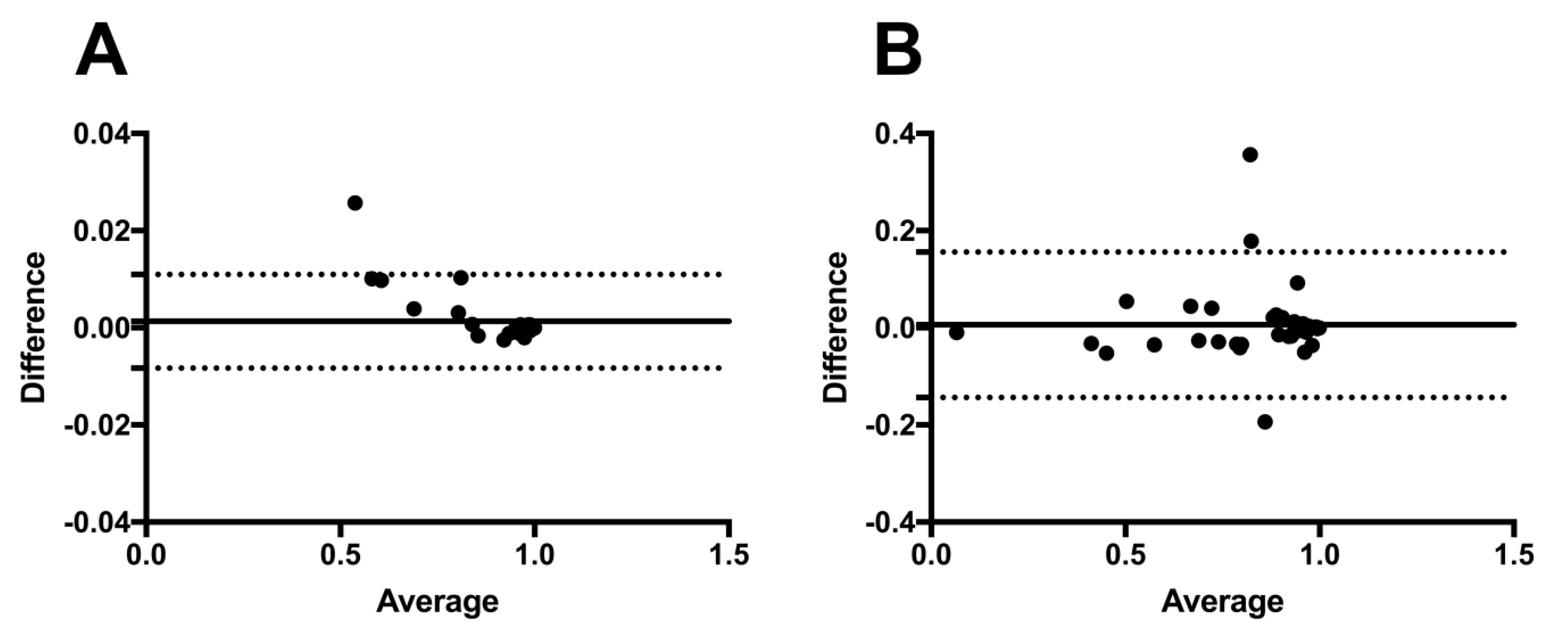
3.3. Repeatability and Precision
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Auw-Haedrich, C.; Staubach, F.; Witschel, H. Optic disk drusen. Surv. Ophthalmol. 2002, 47, 515–532. [Google Scholar] [CrossRef] [PubMed]
- Lorentzen, S.E. Drusen of the optic disk. A clinical and genetic study. Acta Ophthalmol. 1996, 90, 1–180. [Google Scholar]
- Baehring, J.M.; Biestek, J.S. Optic nerve head Drusen mimicking papilledema. J. Neuro-Oncol. 2005, 72, 47. [Google Scholar] [CrossRef] [PubMed]
- Hu, K.; Davis, A.; O’Sullivan, E. Distinguishing optic disc drusen from papilloedema. BMJ 2008, 337, a2360. [Google Scholar] [CrossRef]
- Palmer, E.; Gale, J.; Crowston, J.G.; Wells, A.P. Optic Nerve Head Drusen: An Update. Neuro-Ophthalmol. 2018, 42, 367–384. [Google Scholar] [CrossRef]
- Sim, P.Y.; Soomro, H.; Karampelas, M.; Barampouti, F. Enhanced Depth Imaging Optical Coherence Tomography of Optic Nerve Head Drusen in Children. J. Neuro-Ophthalmol. 2020, 40, 498–503. [Google Scholar] [CrossRef]
- Hamann, S.; Malmqvist, L.; Costello, F. Optic disc drusen: Understanding an old problem from a new perspective. Acta Ophthalmol. 2018, 96, 673–684. [Google Scholar] [CrossRef] [Green Version]
- Savino, P.J.; Glaser, J.S.; Rosenberg, M.A. A Clinical Analysis of Pseudopapilledema: II. Visual Field Defects. Arch. Ophthalmol. 1979, 97, 71–75. [Google Scholar] [CrossRef]
- Mustonen, E. Pseudopapilloedema with and without verified optic disc drusen. A clinical analysis II: Visual fields. Acta Ophthalmol. 1983, 61, 1057–1066. [Google Scholar] [CrossRef]
- Mistlberger, A.; Sitte, S.; Hommer, A.; Emesz, M.; Dengg, S.; Hitzl, W.; Grabner, G. Scanning Laser Polarimetry (SLP) for Optic Nerve Head Drusen. Int. Ophthalmol. 2001, 23, 233–237. [Google Scholar] [CrossRef]
- Malmqvist, L.; Wegener, M.; Sander, B.A.; Hamann, S. Peripapillary Retinal Nerve Fiber Layer Thickness Corresponds to Drusen Location and Extent of Visual Field Defects in Superficial and Buried Optic Disc Drusen. J. Neuro-Ophthalmol. 2016, 36, 41–45. [Google Scholar] [CrossRef]
- LeCun, Y.; Bengio, Y.; Hinton, G. Deep learning. Nature 2015, 521, 436–444. [Google Scholar] [CrossRef]
- Hekler, A.; Utikal, J.S.; Enk, A.H.; Solass, W.; Schmitt, M.; Klode, J.; Schadendorf, D.; Sondermann, W.; Franklin, C.; Bestvater, F.; et al. Deep learning outperformed 11 pathologists in the classification of histopathological melanoma images. Eur. J. Cancer 2019, 118, 91–96. [Google Scholar] [CrossRef] [Green Version]
- McBee, M.P.; Awan, O.A.; Colucci, A.T.; Ghobadi, C.W.; Kadom, N.; Kansagra, A.P.; Tridandapani, S.; Auffermann, W.F. Deep Learning in Radiology. Acad. Radiol. 2018, 25, 1472–1480. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Yang, D.M.; Rong, R.; Zhan, X.; Xiao, G. Pathology Image Analysis Using Segmentation Deep Learning Algorithms. Am. J. Pathol. 2019, 189, 1686–1698. [Google Scholar] [CrossRef] [Green Version]
- Ting, D.S.; Peng, L.; Varadarajan, A.V.; Keane, P.A.; Burlina, P.M.; Chiang, M.F.; Schmetterer, L.; Pasquale, L.R.; Bressler, N.M.; Webster, D.R.; et al. Deep learning in ophthalmology: The technical and clinical considerations. Prog. Retin. Eye Res. 2019, 72, 100759. [Google Scholar] [CrossRef]
- Li, F.; Yan, L.; Wang, Y.; Shi, J.; Chen, H.; Zhang, X.; Jiang, M.; Wu, Z.; Zhou, K. Deep learning-based automated detection of glaucomatous optic neuropathy on color fundus photographs. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 851–867. [Google Scholar] [CrossRef]
- Gulshan, V.; Peng, L.; Coram, M.; Stumpe, M.C.; Wu, D.; Narayanaswamy, A.; Venugopalan, S.; Widner, K.; Madams, T.; Cuadros, J.; et al. Development and Validation of a Deep Learning Algorithm for Detection of Diabetic Retinopathy in Retinal Fundus Photographs. JAMA 2016, 316, 2402–2410. [Google Scholar] [CrossRef]
- Peng, Y.; Dharssi, S.; Chen, Q.; Keenan, T.D.; Agrón, E.; Wong, W.T.; Chew, E.Y.; Lu, Z. DeepSeeNet: A Deep Learning Model for Automated Classification of Patient-based Age-related Macular Degeneration Severity from Color Fundus Photographs. Ophthalmology 2018, 126, 565–575. [Google Scholar] [CrossRef]
- Angermueller, C.; Pärnamaa, T.; Parts, L.; Stegle, O. Deep learning for computational biology. Mol. Syst. Biol. 2016, 12, 878. [Google Scholar] [CrossRef]
- Treder, M.; Eter, N. Deep Learning“ und neuronale Netzwerke in der Augenheilkunde. Ophthalmologe 2018, 115, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Szegedy, C.; Vanhoucke, V.; Ioffe, S.; Shlens, J.; Wojna, Z. Rethinking the Inception Architecture for Computer Vision. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Las Vegas, NV, USA, 27–30 June 2016; pp. 2818–2826. [Google Scholar]
- Chen, T.; Li, M.; Li, Y.; Lin, M.; Wang, N.; Wang, M.; Xiao, T.; Xu, B.; Zhang, C.; Zhang, Z. TensorFlow: Large-scale machine learning on heterogeneous distributed systems. arXiv 2015, arXiv:1512.01274. Available online: https://static.googleusercontent.com/media/research.google.com/en//pubs/archive/45166.pdf (accessed on 4 June 2017).
- TensorFlow. 2017. Available online: http://www.tensorflow.org/tutorials/image_recognition (accessed on 26 June 2017).
- Google Developers. 2017. Available online: https://codelabs.developers.google/.com/codelabs/tensorflow-for-poets/#0 (accessed on 4 July 2017).
- Deng, J.; Dong, W.; Socher, R.; Li, L.J.; Li, K.; Fei-Fei, L. ImageNet: A large-scale hierarchical image database. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Miami, FL, USA, 16–20 June 2009; pp. 248–255. [Google Scholar]
- Treder, M.; Lauermann, J.L.; Eter, N. Automated detection of exudative age-related macular degeneration in spectral domain optical coherence tomography using deep learning. Graefe’s Arch. Clin. Exp. Ophthalmol. 2017, 256, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Treder, M.; Lauermann, J.L.; Eter, N. Deep learning-based detection and classification of geographic atrophy using a deep convolutional neural network classifier. Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 256, 2053–2060. [Google Scholar] [CrossRef] [PubMed]
- Raman, R.; Srinivasan, S.; Virmani, S.; Sivaprasad, S.; Rao, C.; Rajalakshmi, R. Fundus photograph-based deep learning algorithms in detecting diabetic retinopathy. Eye 2018, 33, 97–109. [Google Scholar] [CrossRef] [Green Version]
- Burlina, P.M.; Joshi, N.; Pekala, M.; Pacheco, K.D.; Freund, D.E.; Bressler, N.M. Automated Grading of Age-Related Macular Degeneration From Color Fundus Images Using Deep Convolutional Neural Networks. JAMA Ophthalmol. 2017, 135, 1170–1176. [Google Scholar] [CrossRef]
- Treder, M.; Lauermann, J.L.; Alnawaiseh, M.; Eter, N. Using Deep Learning in Automated Detection of Graft Detachment in Descemet Membrane Endothelial Keratoplasty: A Pilot Study. Cornea 2018, 38, 157–161. [Google Scholar] [CrossRef]
- Shah, M.; Ledo, A.R.; Rittscher, J. Automated classification of normal and Stargardt disease optical coherence tomography images using deep learning. Acta Ophthalmol. 2020, 98, e715–e721. [Google Scholar] [CrossRef]
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. Imagenet classification with deep convolutional neural networks. Commun. ACM 2017, 60, 84–90. [Google Scholar] [CrossRef] [Green Version]
- Milea, D.; Najjar, R.P.; Jiang, Z.; Ting, D.; Vasseneix, C.; Xu, X.; Fard, M.A.; Fonseca, P.; Vanikieti, K.; Lagrèze, W.A.; et al. Artificial Intelligence to Detect Papilledema from Ocular Fundus Photographs. N. Engl. J. Med. 2020, 382, 1687–1695. [Google Scholar] [CrossRef]
| ODD Testing Group | Healthy Testing Group | |
|---|---|---|
| Positive | n = 20 | n = 0 |
| Negative | n = 0 | n = 20 |
| ODD Testing Group | Healthy Testing Group | |
|---|---|---|
| Positive | n = 17 | n = 0 |
| Negative | n = 3 | n = 20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diener, R.; Lauermann, J.L.; Eter, N.; Treder, M. Discriminating Healthy Optic Discs and Visible Optic Disc Drusen on Fundus Autofluorescence and Color Fundus Photography Using Deep Learning—A Pilot Study. J. Clin. Med. 2023, 12, 1951. https://doi.org/10.3390/jcm12051951
Diener R, Lauermann JL, Eter N, Treder M. Discriminating Healthy Optic Discs and Visible Optic Disc Drusen on Fundus Autofluorescence and Color Fundus Photography Using Deep Learning—A Pilot Study. Journal of Clinical Medicine. 2023; 12(5):1951. https://doi.org/10.3390/jcm12051951
Chicago/Turabian StyleDiener, Raphael, Jost Lennart Lauermann, Nicole Eter, and Maximilian Treder. 2023. "Discriminating Healthy Optic Discs and Visible Optic Disc Drusen on Fundus Autofluorescence and Color Fundus Photography Using Deep Learning—A Pilot Study" Journal of Clinical Medicine 12, no. 5: 1951. https://doi.org/10.3390/jcm12051951
APA StyleDiener, R., Lauermann, J. L., Eter, N., & Treder, M. (2023). Discriminating Healthy Optic Discs and Visible Optic Disc Drusen on Fundus Autofluorescence and Color Fundus Photography Using Deep Learning—A Pilot Study. Journal of Clinical Medicine, 12(5), 1951. https://doi.org/10.3390/jcm12051951






