The Clinical Presentation of Endometriosis and Its Association to Current Surgical Staging
Abstract
:1. Introduction
2. Materials and Methods
2.1. Translation
2.2. Questionnaire Structure
2.3. Group Characteristics
2.4. Ethical Approval
2.5. Data Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nnoaham, K.E.; Hummelshoj, L.; Webster, P.; D’Hooghe, T.; De Cicco Nardone, F.; De Cicco Nardone, C.; Jenkinson, C.; Kennedy, S.H.; Zondervan, K.T. Impact of Endometriosis on Quality of Life and Work Productivity: A Multicenter Study across Ten Countries. Fertil. Steril. 2011, 96, 366–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Della Corte, L.; Di Filippo, C.; Gabrielli, O.; Reppuccia, S.; La Rosa, V.L.; Ragusa, R.; Fichera, M.; Commodari, E.; Bifulco, G.; Giampaolino, P. The Burden of Endometriosis on Women’s Lifespan: A Narrative Overview on Quality of Life and Psychosocial Wellbeing. Int. J. Environ. Res. Public Health 2020, 17, 4683. [Google Scholar] [CrossRef] [PubMed]
- Parasar, P.; Ozcan, P.; Terry, K.L. Endometriosis: Epidemiology, Diagnosis and Clinical Management. Curr. Obstet. Gynecol. Rep. 2017, 6, 34–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moradi, M.; Parker, M.; Sneddon, A.; Lopez, V.; Ellwood, D. Impact of Endometriosis on Women’s Lives: A Qualitative Study. BMC Women’S Health 2014, 14, 123. [Google Scholar] [CrossRef] [Green Version]
- Pugsley, Z.; Ballard, K. Management of Endometriosis in General Practice: The Pathway to Diagnosis. Br. J. Gen. Pract. 2007, 57, 470–476. [Google Scholar]
- Wahl, K.J.; Imtiaz, S.; Lisonek, M.; Joseph, K.; Smith, K.B.; Yong, P.J.; Cox, S.M. Dyspareunia in Their Own Words: A Qualitative Description of Endometriosis-Associated Sexual Pain. Sex. Med. 2021, 9, 100274. [Google Scholar] [CrossRef]
- Shahraki, Z.; Tanha, F.D.; Ghajarzadeh, M. Depression, Sexual Dysfunction and Sexual Quality of Life in Women with Infertility. BMC Womens Health 2018, 18, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Missmer, S.A.; Tu, F.F.; Agarwal, S.K.; Chapron, C.; Soliman, A.M.; Chiuve, S.; Eichner, S.; Flores-Caldera, I.; Horne, A.W.; Kimball, A.B.; et al. Taylor, and Sawsan As-Sanie. “Impact of Endometriosis on Life-Course Potential: A Narrative Review. Int. J. Gen. Med. 2021, 14, 9–25. [Google Scholar]
- Khong, S.Y.; Lam, A.; Luscombe, G. Is the 30-Item Endometriosis Health Profile (Ehp-30) Suitable as a Self-Report Health Status Instrument for Clinical Trials? Fertil. Steril. 2010, 94, 1928–1932. [Google Scholar] [CrossRef]
- Ashkenazi, M.S.; Huseby, O.L.; Kroken, G.; Soto-Mota, A.; Pents, M.; Loschiavo, A.; Lewandowska, R.; Tran, G.; Kwiatkowski, S. Covid-19 Pandemic and the Consequential Effect on Patients with Endometriosis. Hum. Reprod. Open 2022, 2022, hoac013. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Koo, Y.-J.; Lee, D.-H. Classification of Endometriosis. Yeungnam Univ. J. Med. 2021, 38, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Peter, A.W.; Adamson, G.D.; Al-Jefout, M.; Becker, C.M.; D’Hooghe, T.M.; Dunselman, G.A.J.; Fazleabas, A.; Giudice, L.C.; Horne, A.W.; Hull, M.L.; et al. Research Priorities for Endometriosis: Recommendations from a Global Consortium of Investigators in Endometriosis. Pap. Presented Reprod. Sci. 2017, 24, 202–226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Facchin, F.; Barbara, G.; Saita, E.; Mosconi, P.; Roberto, A.; Fedele, L.; Vercellini, P. Impact of Endometriosis on Quality of Life and Mental Health: Pelvic Pain Makes the Difference. J. Psychosom. Obstet. Gynecol. 2015, 36, 135–141. [Google Scholar] [CrossRef]
- As-Sanie, S.; Black, R.; Giudice, L.C.; Valbrun, T.G.; Gupta, J.; Jones, B.; Laufer, M.R.; Milspaw, A.T.; Missmer, S.A.; Norman, A.; et al. Assessing Research Gaps and Unmet Needs in Endometriosis. Am. J. Obstet. Gynecol. 2019, 221, 86–94. [Google Scholar]
- van Aken, M.A.; Oosterman, J.M.; van Rijn, C.; Ferdek, M.A.; Ruigt, G.S.; Peeters, B.; Braat, D.D.; Nap, A.W. Pain Cognition Versus Pain Intensity in Patients with Endometriosis: Toward Personalized Treatment. Fertil. Steril. 2017, 108, 679–686. [Google Scholar] [CrossRef] [Green Version]
- Leeners, B.; Imthurn, B. Psychosomatische Aspekte Der Endometriose-Aktueller Stand Der Wissenschaftlichen Kenntnisse Und Der Klinischen Erfahrungen. Gynakol.-Geburtshilfliche Rundsch. 2007, 47, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.; Barlow, D.; Jewell, D.; Kennedy, S. Do Gastrointestinal Symptoms Vary with the Menstrual Cycle? BJOG Int. J. Obstet. Gynaecol. 1998, 105, 1322–1325. [Google Scholar] [CrossRef]
- Warzecha, D.; Szymusik, I.; Wielgos, M.; Pietrzak, B. The Impact of Endometriosis on the Quality of Life and the Incidence of Depression—A Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 3641. [Google Scholar] [CrossRef]
- National Guideline, Alliance. National Institute for Health and Care Excellence: Guidelines. In Endometriosis: Diagnosis and Management; National Institute for Health and Care Excellence (NICE) ©: London, UK, 2017. [Google Scholar]
- Kennedy, S.; Bergqvist, A.; Chapron, C.; D’Hooghe, T.; Dunselman, G.; Greb, R.; Hummelshoj, L.; Prentice, A.; Saridogan, E. Eshre Guideline for the Diagnosis and Treatment of Endometriosis. Hum. Reprod. 2005, 20, 2698–2704. [Google Scholar] [CrossRef]
- McAllister, S.L.; McGinty, K.A.; Resuehr, D.; Berkley, K.J. Endometriosis-Induced Vaginal Hyperalgesia in the Rat: Role of the Ectopic Growths and Their Innervation. Pain 2009, 147, 255–264. [Google Scholar] [CrossRef] [Green Version]
- McAllister, S.L.; Dmitrieva, N.; Berkley, K.J. Sprouted Innervation into Uterine Transplants Contributes to the Development of Hyperalgesia in a Rat Model of Endometriosis. PLoS ONE 2012, 7, e31758. [Google Scholar] [CrossRef] [PubMed]
- Macer, M.L.; Taylor, H.S. Endometriosis and Infertility. A Review of the Pathogenesis and Treatment of Endometriosis-Associated Infertility. Obstet. Gynecol. Clin. N Am. 2012, 39, 535–549. [Google Scholar]
- Johnson, N.P.; Hummelshoj, L.; Adamson, G.D.; Keckstein, J.; Taylor, H.S.; Abrao, M.S.; Bush, D.; Kiesel, L.; Tamimi, R.; Sharpe-Timms, K.L.; et al. World Endometriosis Society Consensus on the Classification of Endometriosis. Hum. Reprod 2017, 32, 315–324. [Google Scholar] [CrossRef] [Green Version]
- Catelan, D.; Giangreco, M.; Biggeri, A.; Barbone, F.; Monasta, L.; Ricci, G.; Romano, F.; Rosolen, V.; Zito, G.; Ronfani, L. Spatial Patterns of Endometriosis Incidence. A Study in Friuli Venezia Giulia (Italy) in the Period 2004–2017. Int. J. Environ. Res. Public Health 2021, 18, 7175. [Google Scholar] [CrossRef] [PubMed]



| Variable | N/mean | SD/percentage | Min-Max | CI 95 | |
|---|---|---|---|---|---|
| Age (years) | 33.2 | 7.5 | 12–72 | 32.9–33.5 | |
| Age at diagnosis (years) | 27.7 | - | - | - | |
| Endometriosis stage | Stage 1 | 142 | 4.8% | - | - |
| Stage 2 | 267 | 9% | - | - | |
| Stage 3 | 435 | 14.7% | - | - | |
| Stage 4 | 910 | 30.7% | - | - | |
| Unknown | 1210 | 40.8% | - | - | |
| How often do you seek treatment? | Once a year | 668 | 22.5% | - | - |
| Once every 6 months | 1112 | 37.5% | - | - | |
| Multiple times during a half year | 762 | 25.7% | - | - | |
| Multiple times a month | 103 | 3.5% | - | - | |
| Other | 319 | 10.8% | - | - |
| Everyday Experience | Stage | n | % | Text | n tot. |
|---|---|---|---|---|---|
| Group A—Severe long-term effect on quality of life | Stage 1 (N = 141) | 34 | 24.11347518 | 24.1% | 1042 |
| Stage 2 (N = 267) | 93 | 34.83146067 | 34.8% | ||
| Stage 3 (N = 435) | 150 | 34.48275862 | 34.5% | ||
| Stage 4 (N = 907) | 385 | 42.44762955 | 42.4% | ||
| Undiagnosed (N = 1206) | 380 | 31.50912106 | 31.5% | ||
| Group B—Severe short-term effect on quality of life | Stage 1 (N = 141) | 9 | 6.382978723 | 6.4% | 345 |
| Stage 2 (N = 267) | 23 | 8.61423221 | 8.6% | ||
| Stage 3 (N = 435) | 49 | 11.26436782 | 11.3% | ||
| Stage 4 (N = 907) | 105 | 11.57662624 | 11.6% | ||
| Undiagnosed (N = 1206) | 159 | 13.1840796 | 13.2% | ||
| Group C—Mild effect on quality of life | Stage 1 (N = 141) | 78 | 55.31914894 | 55.3% | 1347 |
| Stage 2 (N = 267) | 128 | 47.94007491 | 47.9% | ||
| Stage 3 (N = 435) | 212 | 48.73563218 | 48.7% | ||
| Stage 4 (N = 907) | 359 | 39.58103638 | 39.6% | ||
| Undiagnosed (N = 1206) | 570 | 47.26368159 | 47.3% | ||
| Group D—No effect on quality of life | Stage 1 (N = 141) | 20 | 14.18439716 | 14.2% | 222 |
| Stage 2 (N = 267) | 23 | 8.61423221 | 8.6% | ||
| Stage 3 (N = 435) | 24 | 5.517241379 | 5.5% | ||
| Stage 4 (N = 907) | 58 | 6.394707828 | 6.4% | ||
| Undiagnosed (N = 1206) | 97 | 8.043117745 | 8% |
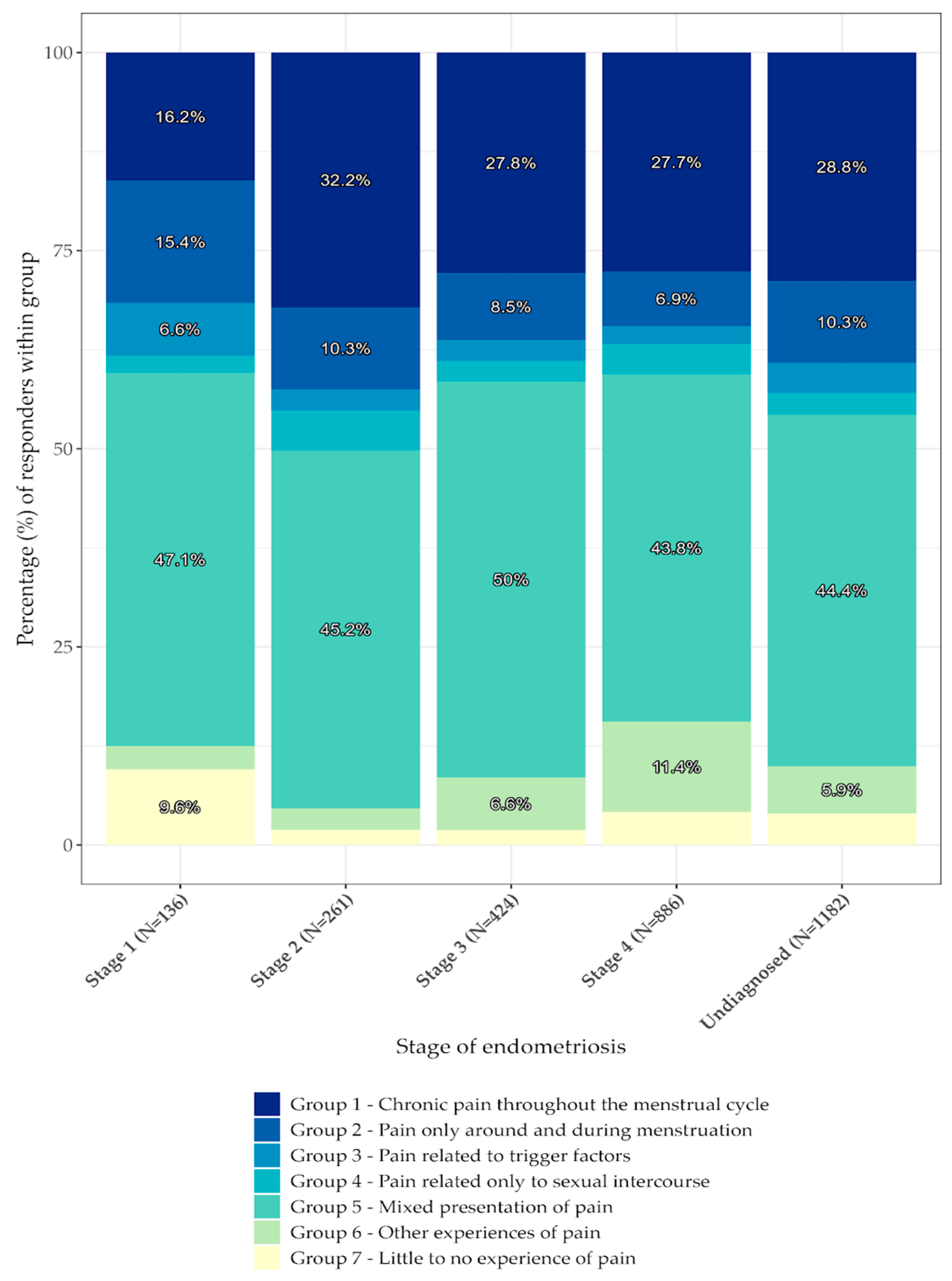
| Pain Experience | Stage | n | Tot | % | Text |
|---|---|---|---|---|---|
| Group 1—Chronic pain throughout the menstrual cycle | Stage 1 (N = 136) | 22 | 810 | 16.18 | 16.2% |
| Stage 2 (N = 261) | 84 | 32.18 | 32.2% | ||
| Stage 3 (N = 424) | 118 | 27.83 | 27.8% | ||
| Stage 4 (N = 886) | 245 | 27.65 | 27.7% | ||
| Undiagnosed (N = 1182) | 341 | 28.85 | 28.8% | ||
| Group 2—Pain only around and during menstruation | Stage 1 (N = 136) | 21 | 267 | 15.44 | 15.4% |
| Stage 2 (N = 261) | 27 | 10.34 | 10.3% | ||
| Stage 3 (N = 424) | 36 | 8.49 | 8.5% | ||
| Stage 4 (N = 886) | 61 | 6.88 | 6.9% | ||
| Undiagnosed (N = 1182) | 122 | 10.32 | 10.3% | ||
| Group 3—Pain related to trigger factors | Stage 1 (N = 136) | 9 | 92 | 6.62 | 6.6% |
| Stage 2 (N = 261) | 7 | 2.68 | 2.7% | ||
| Stage 3 (N = 424) | 11 | 2.59 | 2.6% | ||
| Stage 4 (N = 886) | 20 | 2.26 | 2.3% | ||
| Undiagnosed (N = 1182) | 45 | 3.81 | 3.8% | ||
| Group 4—Pain related only to sexual intercourse | Stage 1 (N = 136) | 3 | 93 | 2.21 | 2.2% |
| Stage 2 (N = 261) | 13 | 4.98 | 5% | ||
| Stage 3 (N = 424) | 11 | 2.59 | 2.6% | ||
| Stage 4 (N = 886) | 34 | 3.84 | 3.8% | ||
| Undiagnosed (N = 1182) | 32 | 2.71 | 2.7% | ||
| Group 5—Mixed presentation of pain | Stage 1 (N = 136) | 64 | 1307 | 47.06 | 47.1% |
| Stage 2 (N = 261) | 118 | 45.21 | 45.2% | ||
| Stage 3 (N = 424) | 212 | 50 | 50% | ||
| Stage 4 (N = 886) | 388 | 43.79 | 43.8% | ||
| Undiagnosed (N = 1182) | 525 | 44.41 | 44.4% | ||
| Group 6—Other experiences of pain | Stage 1 (N = 136) | 4 | 210 | 2.94 | 2.9% |
| Stage 2 (N = 261) | 7 | 2.68 | 2.7% | ||
| Stage 3 (N = 424) | 28 | 6.60 | 6.6% | ||
| Stage 4 (N = 886) | 101 | 11.40 | 11.4% | ||
| Undiagnosed (N = 1182) | 70 | 5.92 | 5.9% | ||
| Group 7—Little to no experience of pain | Stage 1 (N = 136) | 13 | 110 | 9.56 | 9.6% |
| Stage 2 (N = 261) | 5 | 1.92 | 1.9% | ||
| Stage 3 (N = 424) | 8 | 1.89 | 1.9% | ||
| Stage 4 (N = 886) | 37 | 4.18 | 4.2% | ||
| Undiagnosed (N = 1182) | 47 | 3.98 | 4% |
| Pain Experience | n Visits | n | % | Text |
|---|---|---|---|---|
| Group 1—Chronic pain throughout the menstrual cycle | Once a year (N = 649) | 140 | 21.57 | 21.6% |
| Once every 6 months (N = 1088) | 291 | 26.74 | 26.7% | |
| Multiple times during half year (N = 740) | 270 | 36.49 | 36.5% | |
| Multiple times a month (N = 99) | 34 | 34.34 | 34.3% | |
| Other (N = 313) | 75 | 23.96 | 24% | |
| Group 2—Pain only around and during menstruation | Once a year (N = 649) | 88 | 13.56 | 13.6% |
| Once every 6 months (N = 1088) | 106 | 9.74 | 9.7% | |
| Multiple times during half year (N = 740) | 41 | 5.54 | 5.5% | |
| Multiple times a month (N = 99) | 2 | 2.02 | 2% | |
| Other (N = 313) | 30 | 9.58 | 9.6% | |
| Group 3—Pain related to trigger factors | Once a year (N = 649) | 28 | 4.31 | 4.3% |
| Once every 6 months (N = 1088) | 35 | 3.22 | 3.2% | |
| Multiple times during half year (N = 740) | 18 | 2.43 | 2.4% | |
| Other (N = 313) | 11 | 3.51 | 3.5% | |
| Group 4—Pain related only to sexual intercourse | Once a year (N = 649) | 27 | 4.16 | 4.2% |
| Once every 6 months (N = 1088) | 28 | 2.57 | 2.6% | |
| Multiple times during half year (N = 740) | 22 | 2.97 | 3% | |
| Multiple times a month (N = 99) | 3 | 3.03 | 3% | |
| Other (N = 313) | 13 | 4.15 | 4.2% | |
| Group 5—Mixed presentation of pain | Once a year (N = 649) | 275 | 42.37 | 42.4% |
| Once every 6 months (N = 1088) | 513 | 47.15 | 47.2% | |
| Multiple times during half year (N = 740) | 343 | 46.35 | 46.4% | |
| Multiple times a month (N = 99) | 44 | 44.44 | 44.4% | |
| Other (N = 313) | 132 | 42.17 | 42.2% | |
| Group 6—Other experiences of pain | Once a year (N = 649) | 47 | 7.24 | 7.2% |
| Once every 6 months (N = 1088) | 72 | 6.62 | 6.6% | |
| Multiple times during half year (N = 740) | 38 | 5.14 | 5.1% | |
| Multiple times a month (N = 99) | 15 | 15.15 | 15.2% | |
| Other (N = 313) | 38 | 12.14 | 12.1% | |
| Group 7—Little to no experience of pain | Once a year (N = 649) | 44 | 6.78 | 6.8% |
| Once every 6 months (N = 1088) | 43 | 3.95 | 4% | |
| Multiple times during half year (N = 740) | 8 | 1.08 | 1.1% | |
| Multiple times a month (N = 99) | 1 | 1.01 | 1% | |
| Other (N = 649) | 14 | 4.47 | 4.5% |
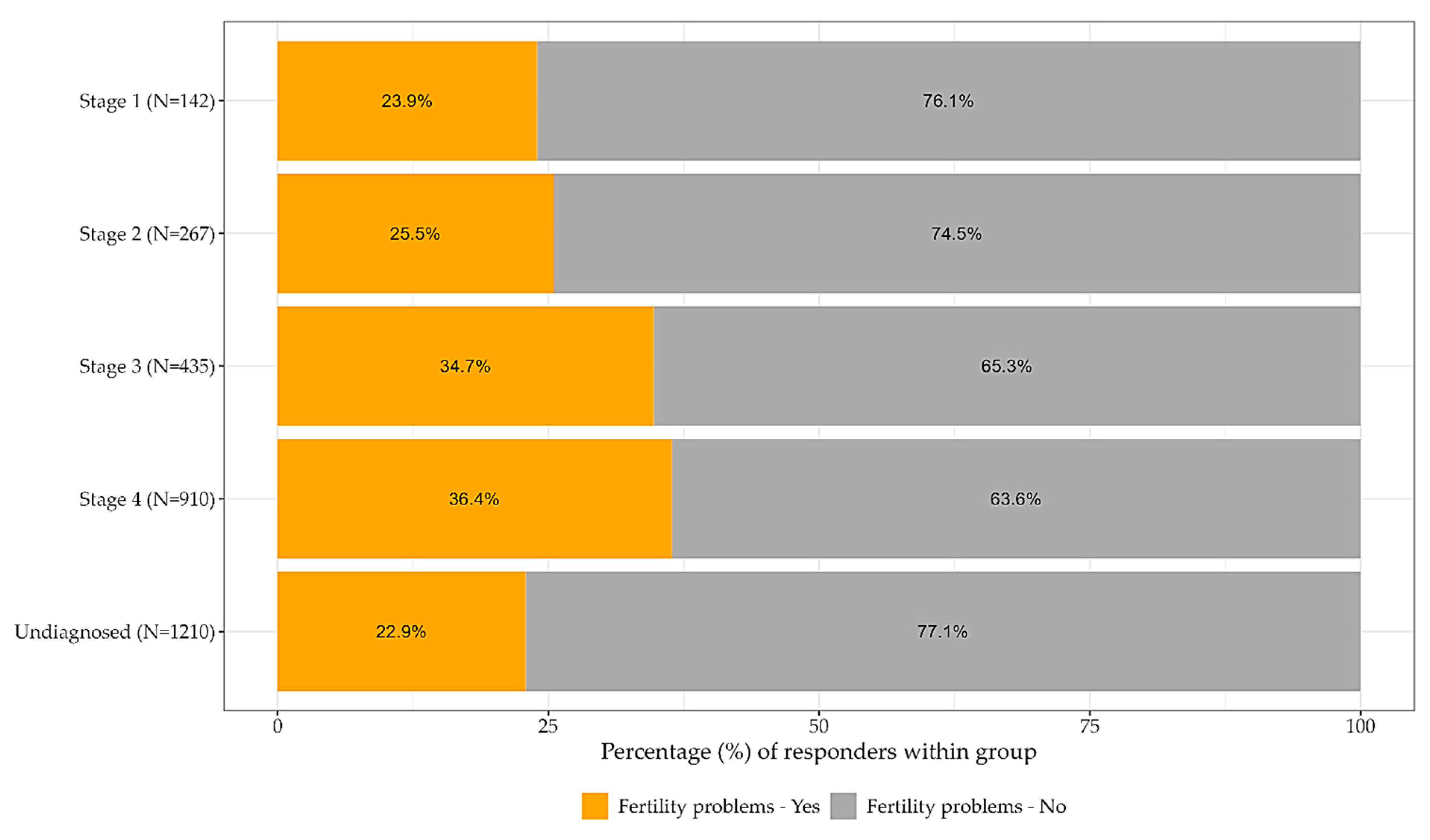
| Fertility Hardship | Stage | n | % | Text |
|---|---|---|---|---|
| Fertility related difficulties—Yes | Stage 1 (N = 142) | 34 | 23.94 | 23.9% |
| Stage 2 (N = 267) | 68 | 25.47 | 25.5% | |
| Stage 3 (N = 435) | 151 | 34.71 | 34.7% | |
| Stage 4 (N = 910) | 331 | 36.37 | 36.4% | |
| Undiagnosed (N = 1210) | 277 | 22.89 | 22.9% | |
| Fertility related difficulties—No | Stage 1 (N = 142) | 108 | 76.06 | 76.1% |
| Stage 2 (N = 267) | 199 | 74.53 | 74.5% | |
| Stage 3 (N = 435) | 284 | 65.29 | 65.3% | |
| Stage 4 (N = 910) | 579 | 63.63 | 63.6% | |
| Undiagnosed (N = 1210) | 933 | 77.11 | 77.1% |
| Pain Experience | Stage | Observed | Expected | Difference |
|---|---|---|---|---|
| Group 1—Chronic pain throughout the menstrual cycle | Stage 1 (N = 136) | 22 | 38.13 | −16.13 |
| Stage 2 (N = 261) | 84 | 73.178 | 10.82 | |
| Stage 3 (N = 424) | 118 | 118.88 | −0.88 | |
| Stage 4 (N = 886) | 245 | 248.41 | −3.41 | |
| Undiagnosed (N = 1182) | 341 | 331.40 | 9.60 | |
| Group 2—Pain only around and during menstruation | Stage 1 (N = 136) | 21 | 12.57 | 8.43 |
| Stage 2 (N = 261) | 27 | 24.12 | 2.88 | |
| Stage 3 (N = 424) | 36 | 39.19 | −3.19 | |
| Stage 4 (N = 886) | 61 | 81.88 | −20.88 | |
| Undiagnosed (N = 1182) | 122 | 109.24 | 12.76 | |
| Group 3—Pain related to trigger factors | Stage 1 (N = 136) | 9 | 4.33 | 4.67 |
| Stage 2 (N = 261) | 7 | 8.31 | −1.31 | |
| Stage 3 (N = 424) | 11 | 13.50 | −2.50 | |
| Stage 4 (N = 886) | 20 | 28.21 | −8.21 | |
| Undiagnosed (N = 1182) | 45 | 37.64 | 7.36 | |
| Group 4—Pain related only to sexual intercourse | Stage 1 (N = 136) | 3 | 4.38 | −1.38 |
| Stage 2 (N = 261) | 13 | 8.40 | 4.60 | |
| Stage 3 (N = 424) | 11 | 13.65 | −2.65 | |
| Stage 4 (N = 886) | 34 | 28.52 | 5.48 | |
| Undiagnosed (N = 1182) | 32 | 38.05 | −6.05 | |
| Group 5—Mixed presentation of pain | Stage 1 (N = 136) | 64 | 61.53 | 2.47 |
| Stage 2 (N = 261) | 118 | 118.08 | −0.08 | |
| Stage 3 (N = 424) | 212 | 191.82 | 20.18 | |
| Stage 4 (N = 886) | 388 | 400.83 | −12.83 | |
| Undiagnosed (N = 1182) | 525 | 534.74 | −9.74 | |
| Group 6—Other experiences of pain | Stage 1 (N = 136) | 4 | 9.89 | −5.89 |
| Stage 2 (N = 261) | 7 | 18.98 | −11.97 | |
| Stage 3 (N = 424) | 28 | 30.82 | −2.82 | |
| Stage 4 (N = 886) | 101 | 64.40 | 36.60 | |
| Undiagnosed (N = 1182) | 70 | 85.92 | −15.92 | |
| Group 7—Little to no experience of pain | Stage 1 (N = 136) | 13 | 5.18 | 7.82 |
| Stage 2 (N = 261) | 5 | 9.94 | −4.94 | |
| Stage 3 (N = 424) | 8 | 16.14 | −8.14 | |
| Stage 4 (N = 886) | 37 | 33.73 | 3.27 | |
| Undiagnosed (N = 1182) | 47 | 45.01 | 1.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashkenazi, M.S.; Huseby, O.L.; Kroken, G.; Trocha, M.; Henriksson, A.; Jasiak, H.; Cuartas, K.; Loschiavo, A.; Kuhn, I.; Støve, D.; et al. The Clinical Presentation of Endometriosis and Its Association to Current Surgical Staging. J. Clin. Med. 2023, 12, 2688. https://doi.org/10.3390/jcm12072688
Ashkenazi MS, Huseby OL, Kroken G, Trocha M, Henriksson A, Jasiak H, Cuartas K, Loschiavo A, Kuhn I, Støve D, et al. The Clinical Presentation of Endometriosis and Its Association to Current Surgical Staging. Journal of Clinical Medicine. 2023; 12(7):2688. https://doi.org/10.3390/jcm12072688
Chicago/Turabian StyleAshkenazi, Matilda Shaked, Ole Linvåg Huseby, Gard Kroken, Marcela Trocha, Aurora Henriksson, Hanna Jasiak, Karen Cuartas, Alessandra Loschiavo, Isabella Kuhn, Dina Støve, and et al. 2023. "The Clinical Presentation of Endometriosis and Its Association to Current Surgical Staging" Journal of Clinical Medicine 12, no. 7: 2688. https://doi.org/10.3390/jcm12072688
APA StyleAshkenazi, M. S., Huseby, O. L., Kroken, G., Trocha, M., Henriksson, A., Jasiak, H., Cuartas, K., Loschiavo, A., Kuhn, I., Støve, D., Grindahl, H., Latour, E., Melbø, M., Holstad, K., & Kwiatkowski, S. (2023). The Clinical Presentation of Endometriosis and Its Association to Current Surgical Staging. Journal of Clinical Medicine, 12(7), 2688. https://doi.org/10.3390/jcm12072688







