Impact of Post-Operative Infection after CABG on Long-Term Survival
Abstract
1. Introduction
2. Materials and Methods
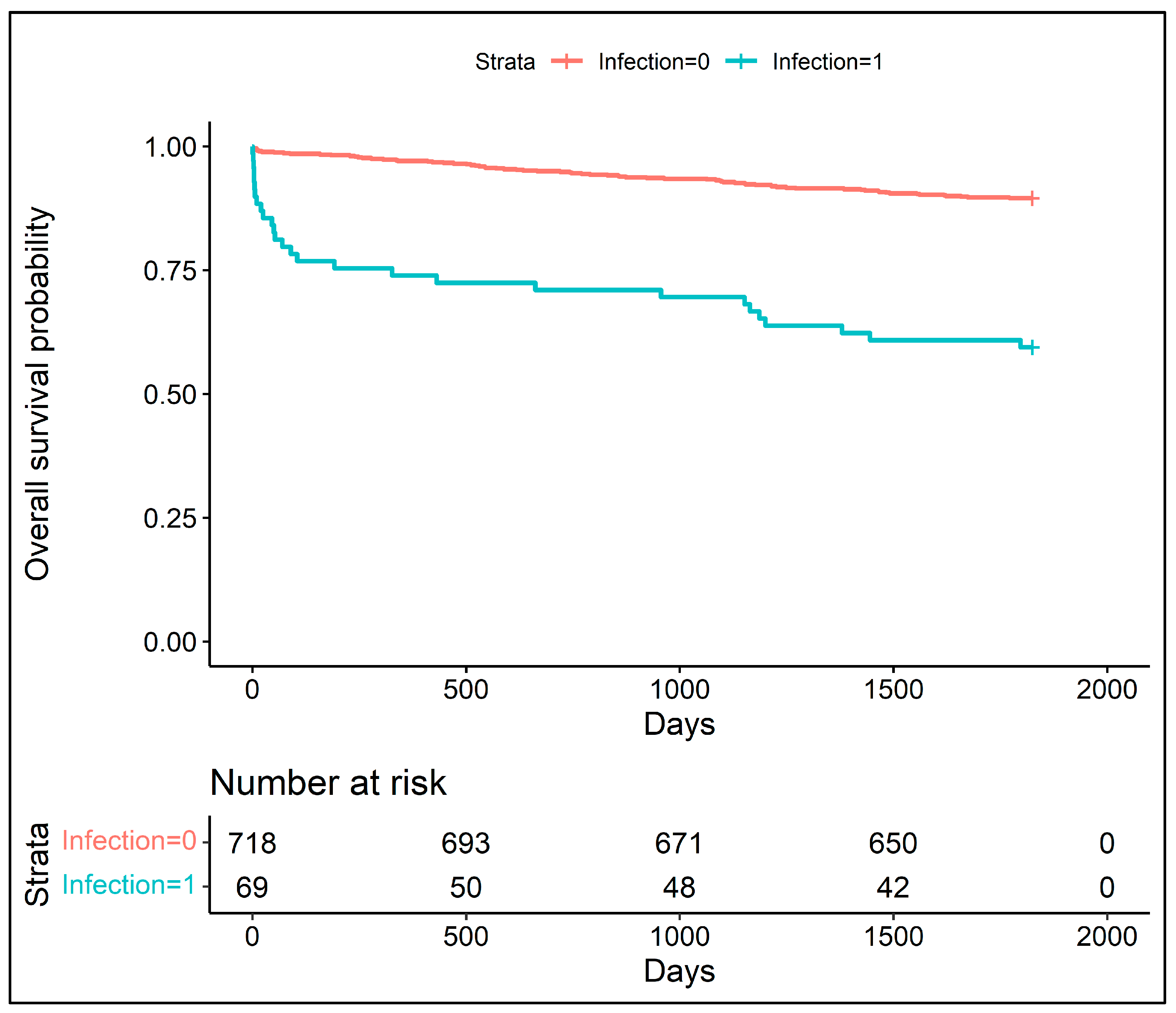
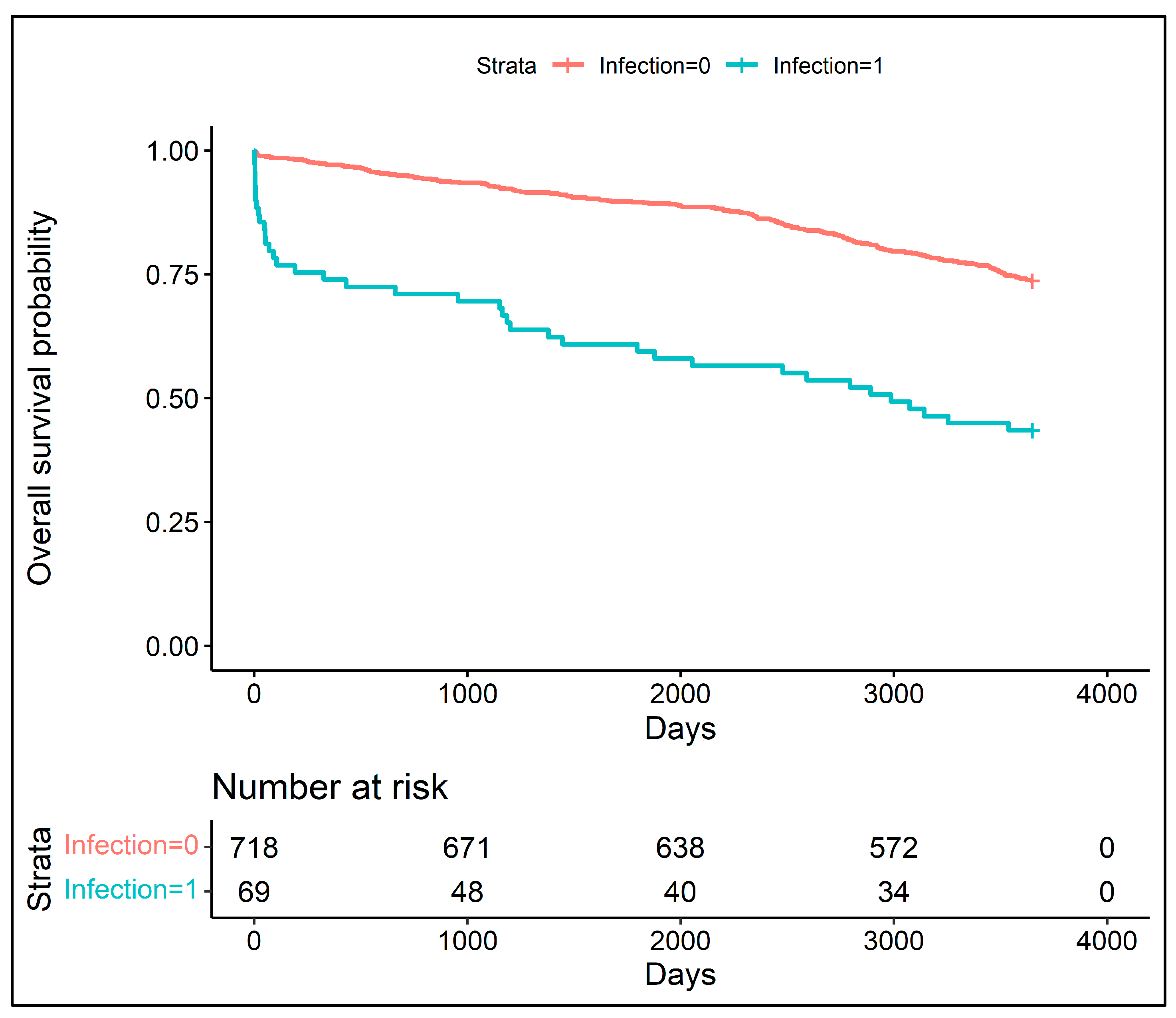
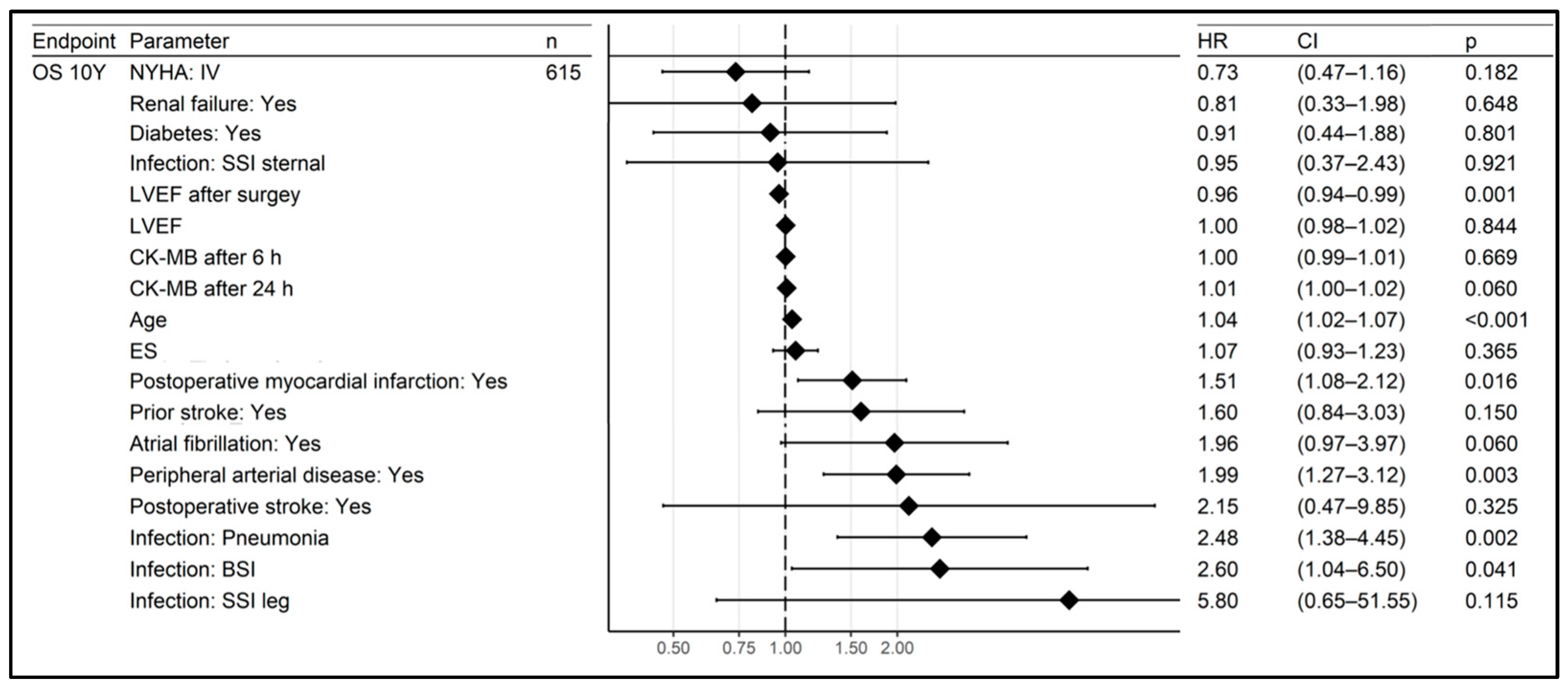
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caldonazo, T.; Kirov, H.; Riedel, L.L.; Gaudino, M.; Doenst, T. Comparing CABG and PCI across the globe based on current regional registry evidence. Sci. Rep. 2022, 12, 22164. [Google Scholar] [CrossRef] [PubMed]
- Bachar, B.J.; Manna, B. Coronary Artery Bypass Graft. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Pan, E.; Nielsen, S.J.; Mennander, A.; Björklund, E.; Martinsson, A.; Lindgren, M.; Hansson, E.C.; Pivodic, A.; Jeppsson, A. Statins for secondary prevention and major adverse events after coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 2022, 164, 1875–1886. [Google Scholar] [CrossRef] [PubMed]
- Magouliotis, D.E.; Fergadi, M.P.; Zotos, P.-A.; Rad, A.A.; Xanthopoulos, A.; Bareka, M.; Spiliopoulos, K.; Athanasiou, T. Differences in long-term survival outcomes after coronary artery bypass grafting using single vs multiple arterial grafts: A meta-analysis with reconstructed time-to-event data and subgroup analyses. Gen. Thorac. Cardiovasc. Surg. 2022, 71, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Talukder, S.; Dimagli, A.; Benedetto, U.; Gray, A.; Gerry, S.; Lees, B.; Krzych, L.; Gaudino, M.F.; Taggart, D.; Flather, M.D. A Systematic Review and Meta-analysis of Factors Associated with Long-Term Mortality in Adults After Coronary Artery Bypass Graft Surgery. Circulation 2022, 146 (Suppl. S1), A12626. [Google Scholar]
- Jain, S.S.; Li, D.; Dressler, O.; Kotinkaduwa, L.; Serruys, P.W.; Kappetein, A.P.; Sabik, J.F.; Morice, M.-C.; Puskas, J.; Kandzari, D.E.; et al. Impact of Periprocedural Adverse Events After PCI and CABG on 5-Year Mortality. JACC Cardiovasc. Interv. 2023, 16, 303–313. [Google Scholar] [CrossRef]
- Fallahzadeh, A.; Sheikhy, A.; Ajam, A.; Sadeghian, S.; Pashang, M.; Shirzad, M.; Bagheri, J.; Mansourian, S.; Momtahen, S.; Hosseini, K. Significance of preoperative left ventricular ejection fraction in 5-year outcome after isolated CABG. J. Cardiothorac. Surg. 2021, 16, 353. [Google Scholar] [CrossRef]
- Shawon, S.R.; Odutola, M.; Falster, M.O.; Jorm, L.R. Patient and hospital factors associated with 30-day readmissions after coronary artery bypass graft (CABG) surgery: A systematic review and meta-analysis. J. Cardiothorac. Surg. 2021, 16, 172. [Google Scholar] [CrossRef] [PubMed]
- Narayan, P.; Dimagli, A.; Fudulu, D.P.; Sinha, S.; Dong, T.; Chan, J.; Angelini, G.D. Risk Factors and Outcomes of Reoperative Surgical Aortic Valve Replacement in The United Kingdom. Ann. Thorac. Surg. 2023. published online ahead of print. [Google Scholar] [CrossRef]
- Perrault, L.P.; Kirkwood, K.A.; Chang, H.L.; Mullen, J.C.; Gulack, B.C.; Argenziano, M.; Gelijns, A.C.; Ghanta, R.K.; Whitson, B.A.; Williams, D.L.; et al. A Prospective Multi-Institutional Cohort Study of Mediastinal Infections after Cardiac Operations. Ann. Thorac. Surg. 2018, 105, 461–468. [Google Scholar] [CrossRef]
- Massart, N.; Mansour, A.; Ross, J.T.; Piau, C.; Verhoye, J.-P.; Tattevin, P.; Nesseler, N. Mortality due to hospital-acquired infection after cardiac surgery. J. Thorac. Cardiovasc. Surg. 2022, 163, 2131–2140. [Google Scholar] [CrossRef]
- Gómez-López, R.; Barge-Caballero, E.; Fernández-Ugidos, P.; Paniagua-Martin, M.J.; Barge-Caballero, G.; Couto-Mallón, D.; Solla-Buceta, M.; de Sierra, C.V.-G.; Aller-Fernández, V.; Fernández-Arias, L.; et al. In-Hospital Post-Operative Infection after Heart Transplantation: Epidemiology, Clinical Management, and Outcome. Surg. Infect. 2020, 21, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Mazzeffi, M.; Zivot, J.; Buchman, T.; Halkos, M. In-Hospital Mortality after Cardiac Surgery: Patient Characteristics, Timing, and Association with Postoperative Length of Intensive Care Unit and Hospital Stay. Ann. Thorac. Surg. 2014, 97, 1220–1225. [Google Scholar] [CrossRef] [PubMed]
- Ibañez, J.; Riera, M.; Amezaga, R.; Herrero, J.; Colomar, A.; Campillo-Artero, C.; De Ibarra, J.I.S.; Bonnin, O. Long-Term Mortality After Pneumonia in Cardiac Surgery Patients: A Propensity-Matched Analysis. J. Intensive Care Med. 2016, 31, 34–40. [Google Scholar] [CrossRef]
- Pahwa, S.; Bernabei, A.; Schaff, H.; Stulak, J.; Greason, K.; Pochettino, A.; Daly, R.; Dearani, J.; Bagameri, G.; King, K.; et al. Impact of postoperative complications after cardiac surgery on long-term survival. J. Card. Surg. 2021, 36, 2045–2052. [Google Scholar] [CrossRef] [PubMed]
- Ono, M.; Kawashima, H.; Hara, H.; Mancone, M.; Mack, M.J.; Holmes, D.R.; Morice, M.-C.; Kappetein, A.P.; Thuijs, D.J.; Noack, T.; et al. Impact of major infections on 10-year mortality after revascularization in patients with complex coronary artery disease. Int. J. Cardiol. 2021, 341, 9–12. [Google Scholar] [CrossRef]
- Tatsuishi, W.; Yamamoto, H.; Nakai, M.; Tanemoto, K.; Miyata, H.; Motomura, N. Incidence and outcomes of surgical site infection after cardiovascular surgery (complete republication). Gen. Thorac. Cardiovasc. Surg. 2022, 70, 1009–1014. [Google Scholar] [CrossRef]
- Sandner, S.; Redfors, B.; Angiolillo, D.J.; Audisio, K.; Fremes, S.E.; Janssen, P.W.; Kulik, A.; Mehran, R.; Peper, J.; Ruel, M.; et al. Association of dual antiplatelet therapy with ticagrelor with vein graft failure after coronary artery bypass graft surgery: A systematic review and meta-analysis. JAMA 2022, 328, 554–562. [Google Scholar] [CrossRef]
- Omran, A.S.; Karimi, A.; Ahmadi, S.H.; Davoodi, S.; Marzban, M.; Movahedi, N.; Abbasi, K.; Boroumand, M.A.; Davoodi, S.; Moshtaghi, N. Superficial and deep sternal wound infection after more than 9000 coronary artery bypass graft (CABG): Incidence, risk factors and mortality. BMC Infect. Dis. 2007, 7, 112. [Google Scholar]
- Mancone, M.; Cavalcante, R.; Modolo, R.; Falcone, M.; Biondi-Zoccai, G.; Frati, G.; Spitzer, E.; Benedetto, U.; Blackstone, E.H.; Onuma, Y.; et al. Major infections after bypass surgery and stenting for multivessel coronary disease in the randomised SYNTAX trial. Eurointervention 2020, 15, 1520–1526. [Google Scholar] [CrossRef]
- Biancari, F.; Gatti, G.; Rosato, S.; Mariscalco, G.; Pappalardo, A.; Onorati, F.; Faggian, G.; Salsano, A.; Santini, F.; Ruggieri, V.G.; et al. Preoperative risk stratification of deep sternal wound infection after coronary surgery. Infect. Control. Hosp. Epidemiol. 2020, 41, 444–451. [Google Scholar] [CrossRef]
- Hadaya, J.; Downey, P.; Tran, Z.; Sanaiha, Y.; Verma, A.; Shemin, R.J.; Benharash, P. Impact of Postoperative Infections on Readmission and Resource Use in Elective Cardiac Surgery. Ann. Thorac. Surg. 2022, 113, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Brescia, A.A.; Rankin, J.S.; Cyr, D.D.; Jacobs, J.P.; Prager, R.L.; Zhang, M.; Matsouaka, R.A.; Harrington, S.D.; Dokholyan, R.S.; Bolling, S.F.; et al. Determinants of Variation in Pneumonia Rates after Coronary Artery Bypass Grafting. Ann. Thorac. Surg. 2018, 105, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Head, S.J.; Davierwala, P.M.; Serruys, P.W.; Redwood, S.R.; Colombo, A.; Mack, M.J.; Morice, M.-C.; Holmes, D.R.; Feldman, T.E.; Ståhle, E.; et al. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: Final five-year follow-up of the SYNTAX trial. Eur. Heart J. 2014, 35, 2821–2830. [Google Scholar] [CrossRef]
- Head, S.J.; Milojevic, M.; Daemen, J.; Ahn, J.-M.; Boersma, E.; Christiansen, E.H.; Domanski, M.J.; Farkouh, M.E.; Flather, M.; Fuster, V.; et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: A pooled analysis of individual patient data. Lancet 2018, 391, 939–948. [Google Scholar] [CrossRef]
- Nuru, A.; Weltzien, J.A.H.; Sandvik, L.; Tønnessen, T.; Bjørnstad, J.L. Short-and long-term survival after isolated coronary artery bypass grafting, the impact of gender and age. Scand. Cardiovasc. J. 2019, 53, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Robich, M.P.; Sabik, J.F., III; Houghtaling, P.L.; Kelava, M.; Gordon, S.; Blackstone, E.H.; Koch, C.G. Prolonged effect of postoperative infectious complications on survival after cardiac surgery. Ann. Thorac. Surg. 2015, 99, 1591–1599. [Google Scholar] [CrossRef]

| Parameter | Survivors n = 560 | Non-Survivors n = 228 | p |
|---|---|---|---|
| Female (n. %) | 138/560 (25%) | 51/228 (22%) | 0.8974 |
| Age (years. mean ± SD) | 63 (9) | 69 (8) | <0.0001 |
| Weight (kg. mean ± SD) | 81 (13) | 80 (14) | 0.6957 |
| LVEF (%. mean ± SD) | 51 (10) | 46 (12) | 0.0001 |
| Insulin-dependent diabetes (n. %) | 6/553 (1.1%) | 2/228 (0.9%) | 1 |
| Insulin-non-dependent diabetes (n. %) | 159/553 (29%) | 92/228 (40%) | 0.0134 |
| Prior stroke (n. %) | 18/553 (3.3%) | 19/228 (8.3%) | 0.0178 |
| Myocardial infarction (n. %) | 169/552 (31%) | 96/228 (42%) | 0.0143 |
| Atrial fibrillation (n. %) | 12/553 (2.2%) | 14/228 (6.1%) | 0.0352 |
| NYHA functional class (n. %) | 0.0170 | ||
| 1 | 4/542 (0.7%) | 0/226 (0%) | |
| 2 | 122/542 (23%) | 28/226 (12%) | |
| 3 | 290/542 (54%) | 146/226 (65%) | |
| 4 | 126/542 (23%) | 52/226 (23%) | |
| ES (mean ± SD) | 3.36 (2.48) | 5.13 (2.81) | <0.0001 |
| ES log (mean ± SD) | 3.9 (4.2) | 7.2 (6.8) | <0.0001 |
| Peripheral arterial disease (n. %) | 43/553 (7.8%) | 44/228 (19%) | <0.0001 |
| Renal failure (n. %) | 13/553 (2.4%) | 21/228 (9.2%) | 0.0004 |
| CPB time (minutes. mean ± SD) | 50 (15) | 50 (15) | 0.8031 |
| Operation time (minutes. mean ± SD) | 153 (56) | 150 (26) | 0.8031 |
| LVEF day after surgery % | 53 (9) | 47 (11) | <0.0001 |
| CK-MB after 6 h | 37 (20) | 43 (38) | 0.5946 |
| CK-MB after 12 h | 42 (32) | 53 (70) | 0.2007 |
| CK-MB after 24 h | 44 (35) | 59 (100) | 0.1307 |
| Intraaortic balloon pump (n. %) | 2/548 (0.4%) | 2/227 (0.9%) | 0.98331 |
| Milrinone (n. %) | 11/541 (2.0%) | 9/222 (4.1%) | 0.48196 |
| TIA (n. %) | 5/551 (0.9%) | 0/227 (0%) | 0.63631 |
| Post-operative myocardial infarction (n. %) | 6/551 (1.1%) | 7/227 (3.1%) | 0.27267 |
| Post-operative stroke (n. %) | 2/551 (0.4%) | 5/227 (2.2%) | 0.13234 |
| Post-operative atrial fibrillation (n. %) | 119/551 (22%) | 58/227 (26%) | 0.55622 |
| Infection (n. %) | 30/559 (5.4%) | 39/228 (17%) | <0.0001 |
| Infection source (n. %) | <0.0001 | ||
| 0 | 529/559 (95%) | 189/228 (83%) | |
| BSI | 6/559 (1.1%) | 9/228 (3.9%) | |
| SSI sternal | 9/559 (1.6%) | 6/228 (2.6%) | |
| SSI leg | 2/559 (0.4%) | 1/228 (0.4%) | |
| Pneumonia | 13/559 (2.3%) | 23/228 (10%) | |
| Post-operative drainage (mL. mean ± SD) | 552 (353) | 530 (306) | 0.9020 |
| Red blood cells (mL. mean ± SD) | 124 (271) | 181 (326) | 0.0363 |
| Parameter | Infection (−) | Infection (+) | p |
|---|---|---|---|
| Female (n. %) | 176/718 (25%) | 13/69 (19%) | 0.6571 |
| Age (years. mean ± SD) | 65 (9) | 68 (9) | 0.0051 |
| Weight (kg. mean ± SD) | 81 (13) | 84 (13) | 0.06332 |
| LVEF (%. mean ± SD) | 50 (11) | 46 (12) | 0.0313 |
| ES (mean ± SD) | 3.71 (2.60) | 5.60 (3.12) | <0.0001 |
| ES log (mean ± SD) | 4.5 (4.7) | 8.3 (9.2) | <0.0001 |
| Insulin-dependent diabetes (n. %) | 7/713 (1.0%) | 1/67 (1.5%) | 1 |
| Insulin-non-dependent diabetes (n. %) | 218/713 (31%) | 32/67 (48%) | 0.0411 |
| Prior stroke (n. %) | 33/713 (4.6%) | 4/67 (6.0%) | 1 |
| Myocardial infarction (n. %) | 242/712 (34%) | 23/67 (34%) | 1 |
| Atrial fibrillation (n. %) | 22/713 (3.1%) | 4/67 (6.0%) | 0.6571 |
| Hypertension (n. %) | |||
| NYHA functional class (n. %) | 0.02625 | ||
| 1 | 4/700 (0.6%) | 0/67 (0%) | |
| 2 | 145/700 (21%) | 5/67 (7.5%) | |
| 3 | 400/700 (57%) | 36/67 (54%) | |
| 4 | 151/700 (22%) | 26/67 (39%) | |
| Peripheral arterial disease (n. %) | 75/713 (11%) | 12/67 (18%) | 0.3156 |
| Renal failure (n. %) | 29/713 (4.1%) | 5/67 (7.5%) | 0.6458 |
| Intraaortic balloon pump (n. %) | 2/709 (0.3%) | 2/65 (3.1%) | 0.1683 |
| Milrinone (n. %) | 11/696 (1.6%) | 9/66 (14%) | <0.0001 |
| TIA (n. %) | 4/711 (0.6%) | 1/66 (1.5%) | 1 |
| Post-operative myocardial infarction (n. %) | 8/711 (1.1%) | 5/66 (7.6%) | 0.0074 |
| Post-operative stroke (n. %) | 6/711 (0.8%) | 1/66 (1.5%) | 1 |
| Post-operative atrial fibrillation (n. %) | 160/711 (23%) | 16/66 (24%) | 1 |
| CPB time (minutes. mean ± SD) | 50 (14) | 52 (18) | 0.8494 |
| Operation time (minutes. mean ± SD) | 151 (50) | 157 (33) | 0.1689 |
| LVEF day after surgery % | 52 (10) | 45 (11) | <0.0001 |
| Chest drainage time (hours. mean ± SD) | 29 (15) | 31 (17) | 0.9266 |
| CK-MB after 6 h | 37 (21) | 56 (59) | 0.0373 |
| CK-MB after 12 h | 42 (33) | 71 (113) | 0.0212 |
| CK-MB after 24 h | 45 (38) | 82 (163) | 0.0068 |
| Post-operative drainage (mL. mean ± SD) | 544 (334) | 568 (403) | 0.8015 |
| Red blood cells (mL. mean ± SD) | 130 (278) | 251 (366) | 0.0058 |
| Time of in-hospital stay (days mean ± SD) | 7.2 (1.7) | 13.7 (13.4) | 0.0001 |
| ICU admission (n. %) | 4/718 (0.6) | 20/69 (28.9) | <0.0001 |
| In-hospital mortality (n. %) | 4/718 9(0.6) | 8/69 (11.6) | <0.0001 |
| Parameter | Survivors n = 560 | Non-survivors n = 228 | p |
|---|---|---|---|
| Female (n. %) | 138/560 (25%) | 51/228 (22%) | 0.8974 |
| Age (years. Mean ± SD) | 63 (9) | 69 (8) | <0.0001 |
| Weight (kg. mean ± SD) | 81 (13) | 80 (14) | 0.6957 |
| LVEF (%. Mean ± SD) | 51 (10) | 46 (12) | 0.0001 |
| Insulin-dependent diabetes (n. %) | 6/553 (1.1%) | 2/228 (0.9%) | 1 |
| Insulin-non-dependent diabetes (n. %) | 159/553 (29%) | 92/228 (40%) | 0.0134 |
| Prior stroke (n. %) | 18/553 (3.3%) | 19/228 (8.3%) | 0.0178 |
| Myocardial infarction (n. %) | 169/552 (31%) | 96/228 (42%) | 0.0143 |
| Atrial fibrillation (n. %) | 12/553 (2.2%) | 14/228 (6.1%) | 0.0352 |
| NYHA functional class (n. %) | 0.0170 | ||
| 1 | 4/542 (0.7%) | 0/226 (0%) | |
| 2 | 122/542 (23%) | 28/226 (12%) | |
| 3 | 290/542 (54%) | 146/226 (65%) | |
| 4 | 126/542 (23%) | 52/226 (23%) | |
| ES (mean ± SD) | 3.36 (2.48) | 5.13 (2.81) | <0.0001 |
| ES log (mean ± SD) | 3.9 (4.2) | 7.2 (6.8) | <0.0001 |
| Peripheral arterial disease (n. %) | 43/553 (7.8%) | 44/228 (19%) | <0.0001 |
| Renal failure (n. %) | 13/553 (2.4%) | 21/228 (9.2%) | 0.0004 |
| CPB time (minutes. Mean ± SD) | 50 (15) | 50 (15) | 0.8031 |
| Operation time (minutes. Mean ± SD) | 153 (56) | 150 (26) | 0.8031 |
| LVEF day after surgery % | 53 (9) | 47 (11) | <0.0001 |
| CK-MB after 6 h | 37 (20) | 43 (38) | 0.5946 |
| CK-MB after 12 h | 42 (32) | 53 (70) | 0.2007 |
| CK-MB after 24 h | 44 (35) | 59 (100) | 0.1307 |
| Intraaortic balloon pump (n. %) | 2/548 (0.4%) | 2/227 (0.9%) | 0.98331 |
| Milrinone (n. %) | 11/541 (2.0%) | 9/222 (4.1%) | 0.48196 |
| TIA (n. %) | 5/551 (0.9%) | 0/227 (0%) | 0.63631 |
| Post-operative myocardial infarction (n. %) | 6/551 (1.1%) | 7/227 (3.1%) | 0.27267 |
| Post-operative stroke (n. %) | 2/551 (0.4%) | 5/227 (2.2%) | 0.13234 |
| Post-operative atrial fibrillation (n. %) | 119/551 (22%) | 58/227 (26%) | 0.55622 |
| Infection (n. %) | 30/559 (5.4%) | 39/228 (17%) | <0.0001 |
| Infection source (n. %) | <0.0001 | ||
| 0 | 529/559 (95%) | 189/228 (83%) | |
| BSI | 6/559 (1.1%) | 9/228 (3.9%) | |
| SSI sternal | 9/559 (1.6%) | 6/228 (2.6%) | |
| SSI leg | 2/559 (0.4%) | 1/228 (0.4%) | |
| Pneumonia | 13/559 (2.3%) | 23/228 (10%) | |
| Post-operative drainage (mL. mean ± SD) | 552 (353) | 530 (306) | 0.9020 |
| Red blood cells (mL. mean ± SD) | 124 (271) | 181 (326) | 0.0363 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zukowska, A.; Kaczmarczyk, M.; Listewnik, M.; Zukowski, M. Impact of Post-Operative Infection after CABG on Long-Term Survival. J. Clin. Med. 2023, 12, 3125. https://doi.org/10.3390/jcm12093125
Zukowska A, Kaczmarczyk M, Listewnik M, Zukowski M. Impact of Post-Operative Infection after CABG on Long-Term Survival. Journal of Clinical Medicine. 2023; 12(9):3125. https://doi.org/10.3390/jcm12093125
Chicago/Turabian StyleZukowska, Agnieszka, Mariusz Kaczmarczyk, Mariusz Listewnik, and Maciej Zukowski. 2023. "Impact of Post-Operative Infection after CABG on Long-Term Survival" Journal of Clinical Medicine 12, no. 9: 3125. https://doi.org/10.3390/jcm12093125
APA StyleZukowska, A., Kaczmarczyk, M., Listewnik, M., & Zukowski, M. (2023). Impact of Post-Operative Infection after CABG on Long-Term Survival. Journal of Clinical Medicine, 12(9), 3125. https://doi.org/10.3390/jcm12093125






