From Detection to Decision: How STIR Sequence MRI Influences Treatment Strategies for Osteoporotic Vertebral Fractures
Abstract
:1. Introduction
2. Materials and Methods
- Conservative treatment modification: If a CT scan showed a lumbar fracture alone but the MRI detected a thoracic vertebral fracture, the external orthosis was extended to cover the thoracic region.
- Surgical intervention modification: If the CT identified an unstable fracture (AO A3, A4) without adjacent fractures, but the MRI revealed fractures adjacent to the original site, bone cement was injected using the PVP method to prevent future collapse or, depending on the case, surgical fixation was extended.
- Conservative to surgery: If a CT indicated a stable fracture (AO A1, A2) but the MRI showed signal enhancement in the peduncles and arches of the vertebrae or a ligamentous injury, the treatment was shifted from conservative to surgical (PVP, surgical fixation).
3. Results
3.1. Fracture Detection and Statistical Analysis
3.2. Detailed Analysis of Fracture Types
3.3. Analysis of Fracture Adjacency
3.4. Impact on Treatment Plans
3.5. Case Highlights
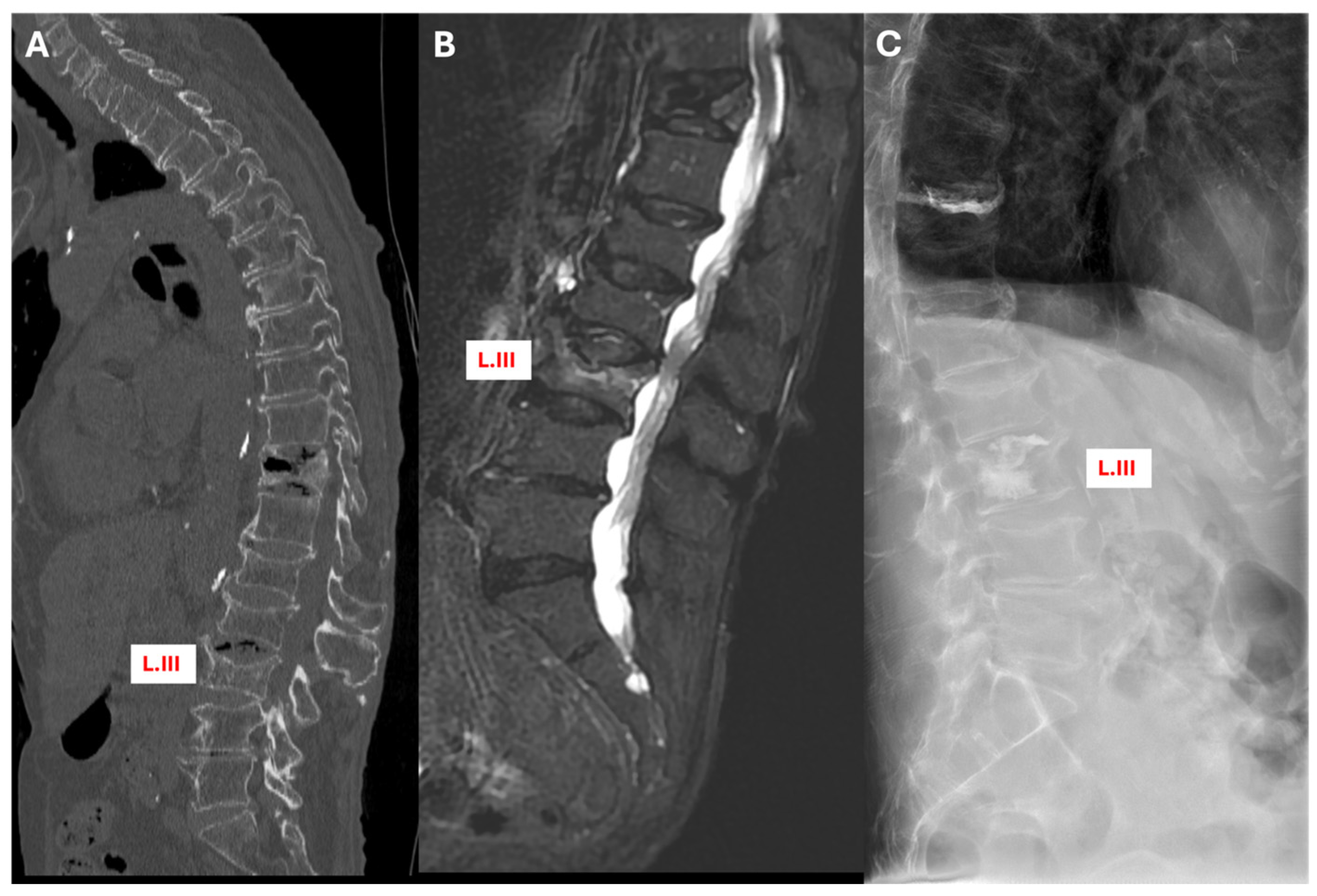
3.5.1. Case 1: Conservative Treatment Modification
3.5.2. Case 2: Surgical Treatment Modification
3.5.3. Case 3: Conversion from Conservative to Surgical Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vokó, Z.; Gáspár, K.; Inotai, A.; Horváth, C.; Bors, K.; Speer, G.; Kaló, Z. Osteoporotic Fractures May Impair Life as Much as the Complications of Diabetes. J. Eval. Clin. Pract. 2017, 23, 1375–1380. [Google Scholar] [CrossRef]
- Péntek, M.; Horváth, C.; Boncz, I.; Falusi, Z.; Tóth, E.; Sebestyén, A.; Májer, I.; Brodszky, V.; Gulácsi, L. Epidemiology of Osteoporosis Related Fractures in Hungary from the Nationwide Health Insurance Database, 1999–2003. Osteoporos. Int. 2008, 19, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Johnell, O.; Kanis, J.A. An Estimate of the Worldwide Prevalence and Disability Associated with Osteoporotic Fractures. Osteoporos. Int. 2006, 17, 1726–1733. [Google Scholar] [CrossRef]
- Riggs, B.L.; Melton, L.J. The Worldwide Problem of Osteoporosis: Insights Afforded by Epidemiology. Bone 1995, 17, 505S–511S. [Google Scholar] [CrossRef]
- Ballane, G.; Cauley, J.A.; Luckey, M.M.; El-Hajj Fuleihan, G. Worldwide Prevalence and Incidence of Osteoporotic Vertebral Fractures. Osteoporos. Int. 2017, 28, 1531–1542. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.D.; Osborne, J.R.; Gordon, W.T.; Hinkin, D.T.; Brinker, M.R. The Natural History of Bone Bruises. A Prospective Study of Magnetic Resonance Imaging-Detected Trabecular Microfractures in Patients with Isolated Medial Collateral Ligament Injuries. Am. J. Sports. Med. 1998, 26, 15–19. [Google Scholar] [CrossRef]
- Qaiyum, M.; Tyrrell, P.N.; McCall, I.W.; Cassar-Pullicino, V.N. MRI Detection of Unsuspected Vertebral Injury in Acute Spinal Trauma: Incidence and Significance. Skelet. Radiol. 2001, 30, 299–304. [Google Scholar] [CrossRef]
- Schoenfeld, A.J.; Bono, C.M.; McGuire, K.J.; Warholic, N.; Harris, M.B. Computed Tomography Alone versus Computed Tomography and Magnetic Resonance Imaging in the Identification of Occult Injuries to the Cervical Spine: A Meta-Analysis. J. Trauma 2010, 68, 109–113; discussion 113–114. [Google Scholar] [CrossRef] [PubMed]
- Kepler, C.K.; Bogner, E.A.; Herzog, R.J.; Huang, R.C. Anatomy of the Psoas Muscle and Lumbar Plexus with Respect to the Surgical Approach for Lateral Transpsoas Interbody Fusion. Eur. Spine J. 2011, 20, 550–556. [Google Scholar] [CrossRef]
- Terakado, A.; Orita, S.; Inage, K.; Kubota, G.; Kanzaki, T.; Mori, H.; Shinohara, Y.; Nakamura, J.; Matsuura, Y.; Aoki, Y.; et al. A Clinical Prospective Observational Cohort Study on the Prevalence and Primary Diagnostic Accuracy of Occult Vertebral Fractures in Aged Women with Acute Lower Back Pain Using Magnetic Resonance Imaging. Pain Res. Manag. 2017, 2017, 9265259. [Google Scholar] [CrossRef]
- Wang, Y.-F.; Teng, M.M.-H.; Chang, C.-Y.; Wu, H.-T.; Wang, S.-T. Imaging Manifestations of Spinal Fractures in Ankylosing Spondylitis. AJNR Am. J. Neuroradiol. 2005, 26, 2067–2076. [Google Scholar] [PubMed]
- Blattert, T.R.; Schnake, K.J.; Gonschorek, O.; Gercek, E.; Hartmann, F.; Katscher, S.; Mörk, S.; Morrison, R.; Müller, M.; Partenheimer, A.; et al. Nonsurgical and Surgical Management of Osteoporotic Vertebral Body Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob. Spine J. 2018, 8, 50S–55S. [Google Scholar] [CrossRef] [PubMed]
- Heynen, B.; Tamigneaux, C.; Pasoglou, V.; Malghem, J.; Vande Berg, B.; Kirchgesner, T. MRI Detection of Radiographically Occult Fractures of the Hip and Pelvis in the Elderly: Comparison of T2-Weighted Dixon Sequence with T1-Weighted and STIR Sequences. Diagn. Interv. Imaging 2019, 100, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Breitenseher, M.J.; Metz, V.M.; Gilula, L.A.; Gaebler, C.; Kukla, C.; Fleischmann, D.; Imhof, H.; Trattnig, S. Radiographically Occult Scaphoid Fractures: Value of MR Imaging in Detection. Radiology 1997, 203, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Fintelmann, F.J.; Kamath, R.S.; Kattapuram, S.V.; Rosenthal, D.I. Limited Magnetic Resonance Imaging of the Lumbar Spine Has High Sensitivity for Detection of Acute Fractures, Infection, and Malignancy. Skelet. Radiol. 2016, 45, 1687–1693. [Google Scholar] [CrossRef] [PubMed]
- Green, R.a.R.; Saifuddin, A. Whole Spine MRI in the Assessment of Acute Vertebral Body Trauma. Skeletal. Radiol. 2004, 33, 129–135. [Google Scholar] [CrossRef]
- Medical Advisory Secretariat. Percutaneous Vertebroplasty for Treatment of Painful Osteoporotic Vertebral Compression Fractures. Ont. Health Technol. Assess. Ser. 2010, 10, 1–45. [Google Scholar]
- Magerl, F.; Aebi, M.; Gertzbein, S.D.; Harms, J.; Nazarian, S. A Comprehensive Classification of Thoracic and Lumbar Injuries. Eur. Spine J. 1994, 3, 184–201. [Google Scholar] [CrossRef] [PubMed]
- Schnake, K.J.; Blattert, T.R.; Hahn, P.; Franck, A.; Hartmann, F.; Ullrich, B.; Verheyden, A.; Mörk, S.; Zimmermann, V.; Gonschorek, O.; et al. Classification of Osteoporotic Thoracolumbar Spine Fractures: Recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Glob. Spine J. 2018, 8, 46S–49S. [Google Scholar] [CrossRef]
- Yuan, W.-H.; Mu-Huo Teng, M.; Hsu, H.-C.; Sun, Y.-C.; Chang, C.-Y. Are Non-Contrast MR Images Enough for Detection of Fracture Levels Prior to Percutaneous Vertebroplasty in Patients with Osteoporosis? Interv. Neuroradiol. 2008, 14, 79–84. [Google Scholar] [CrossRef]
- Richards, P.J. Cervical Spine Clearance: A Review. Injury 2005, 36, 248–269; discussion 270. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.L.; Hardman, J.A.; Lyons, K. MR Imaging of Suspected Acute Spinal Instability. Injury 1998, 29, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Lenski, M.; Büser, N.; Scherer, M. Concomitant and Previous Osteoporotic Vertebral Fractures. Acta Orthop. 2017, 88, 192–197. [Google Scholar] [CrossRef]
- Grünhagen, J.; Egbers, H.-J.; Heller, M.; Reuter, M. Comparison of spine injuries by means of CT and MRI according to the classification of Magerl. Rofo 2005, 177, 828–834. [Google Scholar] [CrossRef] [PubMed]
- Atsina, K.-B.; Rozenberg, A.; Selvarajan, S.K. The Utility of Whole Spine Survey MRI in Blunt Trauma Patients Sustaining Single Level or Contiguous Spinal Fractures. Emerg. Radiol. 2019, 26, 493–500. [Google Scholar] [CrossRef]
- Kumar, Y.; Hayashi, D. Role of Magnetic Resonance Imaging in Acute Spinal Trauma: A Pictorial Review. BMC Musculoskelet. Disord. 2016, 17, 310. [Google Scholar] [CrossRef]
- Szaro, P.; Geijer, M.; Solidakis, N. Traumatic and Non-Traumatic Bone Marrow Edema in Ankle MRI: A Pictorial Essay. Insights Imaging 2020, 11, 97. [Google Scholar] [CrossRef]
- Himič, V.; Syrmos, N.; Ligarotti, G.K.I.; Kato, S.; Fehlings, M.G.; Ganau, M. The Role of Genetic and Epigenetic Factors in Determining the Risk of Spinal Fragility Fractures: New Insights in the Management of Spinal Osteoporosis. Quant. Imaging Med. Surg. 2023, 13, 7632–7645. [Google Scholar] [CrossRef]
- Ganau, M.; Kato, S.; Oshima, Y. Letter to the Editor Concerning “Osteoporotic Thoracolumbar Compression Fractures: Long-Term Retrospective Comparison between Vertebroplasty and Conservative Treatment” by K. Martikos et al. [Eur. Spine J. (2018) doi: 10.1007/S00586-018-5605-1]. Eur. Spine J. 2018, 27, 1662–1663. [Google Scholar] [CrossRef]



| Fracture Spine Level | Number of Fractures Diagnosed | |
|---|---|---|
| CT | STIR MRI | |
| C | 2 | 7 |
| Th | 73 | 128 |
| L | 85 | 129 |
| S | 1 | 2 |
| Total diagnosed fractures | 161 | 266 |
| Fracture Type | Patients with Single Fracture | Patients with Multiple Fractures | Total Number of Patients |
|---|---|---|---|
| Type of Imaging | |||
| CT | 17 | 47 | 64 |
| STIR MRI | 6 | 58 | 64 |
| Total | 23 | 105 | 128 (Grand Total) |
| Multiple Fractures Diagnosed | Patients Number with Multiple Fractures Diagnosed (%) | Total | |
|---|---|---|---|
| CT (n = 47) | STIR MRI (n = 58) | ||
| Patients with Adjacent Fracture | 35 | 51 | 86 |
| Patients with Non-Adjacent Fractures | 12 | 7 | 19 |
| Total | 47 | 58 | 105 (Grand Total) |
| Type of Treatment Modification | Image Findings | Resultant Change | Cases n = 43 (Percentage) | |
|---|---|---|---|---|
| CT | STIR MRI | |||
| Conservative treatment modification | Lumbar fracture alone | Additional fresh thoracic vertebral fracture | Extended external orthosis to cover the thoracic region | 25 instances (58%) |
| Surgical intervention modification | Unstable fracture (AO A3, A4) without adjacent fractures | Additional fresh fractures adjacent to the original site | Injected bone cement using the PVP method or extended surgical fixation | 13 instances (30%) |
| Conservative to surgery | Stable fracture (AO A1, A2) | Showed signal enhancement in the peduncles and arches of the vertebrae or a ligamentous injury | Shifted treatment from conservative to surgical (PVP, surgical fixation) | 5 instances (12%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Viola, R.; Aslan, S.; Al-Smadi, M.W.; Süvegh, D.; Viola, Á. From Detection to Decision: How STIR Sequence MRI Influences Treatment Strategies for Osteoporotic Vertebral Fractures. J. Clin. Med. 2024, 13, 3347. https://doi.org/10.3390/jcm13113347
Viola R, Aslan S, Al-Smadi MW, Süvegh D, Viola Á. From Detection to Decision: How STIR Sequence MRI Influences Treatment Strategies for Osteoporotic Vertebral Fractures. Journal of Clinical Medicine. 2024; 13(11):3347. https://doi.org/10.3390/jcm13113347
Chicago/Turabian StyleViola, Réka, Siran Aslan, Mohammad Walid Al-Smadi, Dávid Süvegh, and Árpád Viola. 2024. "From Detection to Decision: How STIR Sequence MRI Influences Treatment Strategies for Osteoporotic Vertebral Fractures" Journal of Clinical Medicine 13, no. 11: 3347. https://doi.org/10.3390/jcm13113347





