Doctor, When Should I Start Walking? Revisiting Postoperative Rehabilitation and Weight-Bearing Protocols in Operatively Treated Acetabular Fractures: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction and Outcome Measures
2.4. Assessment of the Risk of Bias
2.5. Statistical Analysis
3. Results
3.1. Selection of Studies
3.2. Characteristics of the Studies
3.3. Sample Demographics
3.4. Perioperative Parameters and Form of Treatment
3.5. Quality of Reduction
3.6. Postoperative Rehabilitation Protocol
3.7. Outcome Measurements and Complications
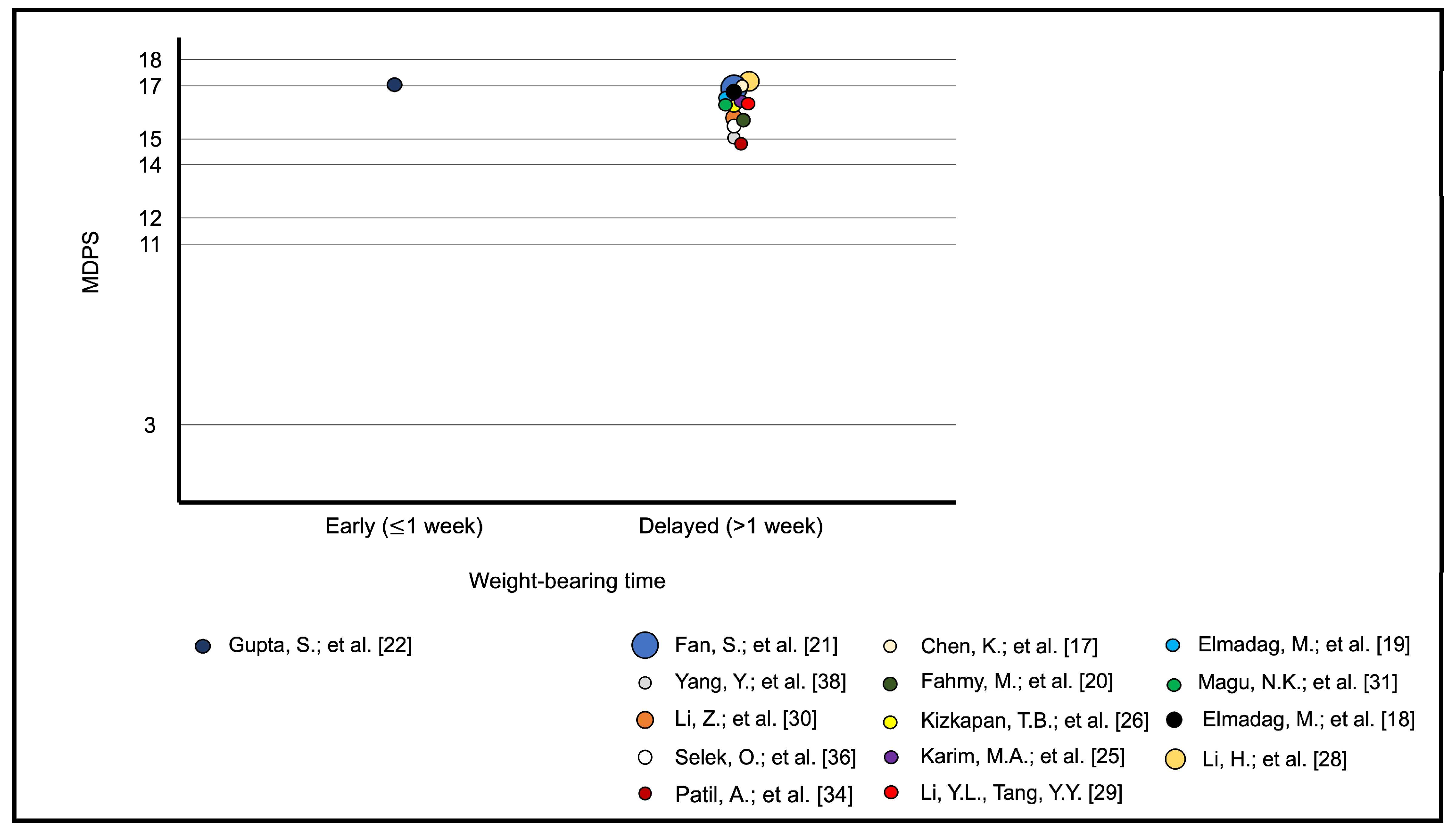
3.8. Meta-Analytic Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Giordano, V.; Pecegueiro do Amaral, N.; Franklin, C.E.; Pallottino, A.; Pires E Albuquerque, R.; Giordano, M. Functional outcome after operative treatment of displaced fractures of the acetabulum: A 12-month to 5-year follow-up investigation. Eur. J. Trauma Emerg. Surg. 2007, 33, 520–527. [Google Scholar] [CrossRef]
- Ziran, N.; Soles, G.L.S.; Matta, J.M. Outcomes after surgical treatment of acetabular fractures: A review. Patient Saf. Surg. 2019, 13, 16. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Grotz, M.R.; Papakostidis, C.; Dinopoulos, H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J. Bone Jt. Surg. Br. 2005, 87, 2–9. [Google Scholar] [CrossRef]
- Tannast, M.; Najibi, S.; Matta, J.M. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J. Bone Jt. Surg. Am. 2012, 94, 1559–1567. [Google Scholar] [CrossRef]
- Kelly, J.; Ladurner, A.; Rickman, M. Surgical management of acetabular fractures—A contemporary literature review. Injury 2020, 51, 2267–2277. [Google Scholar] [CrossRef] [PubMed]
- Fairhall, N.J.; Dyer, S.M.; Mak, J.C.; Diong, J.; Kwok, W.S.; Sherrington, C. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst. Rev. 2022, 9, CD001704. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, J.B.; Ferreira, N.; Domingos, J.; Ferreira, R.; Amador, C.; Pardal, N.; Castro, C.; Simões, A.; Fernandes, S.; Bernardes, C.; et al. Health professionals’ motivational strategies to enhance adherence in the rehabilitation of people with lower limb fractures: Scoping review. Int. J. Environ. Res. Public Health 2023, 20, 7050. [Google Scholar] [CrossRef]
- Asplin, G.; Carlsson, G.; Zidén, L.; Kjellby-Wendt, G. Early coordinated rehabilitation in acute phase after hip fracture—A model for increased patient participation. BMC Geriatr. 2017, 17, 240. [Google Scholar] [CrossRef] [PubMed]
- Chudyk, A.M.; Jutai, J.W.; Petrella, R.J.; Speechley, M. Systematic review of hip fracture rehabilitation practices in the elderly. Arch. Phys. Med. Rehabil. 2009, 90, 246–262. [Google Scholar] [CrossRef]
- Lee, K.J.; Um, S.H.; Kim, Y.H. Postoperative rehabilitation after hip fracture: A literature review. Hip Pelvis 2020, 32, 125–131. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Judet, R.; Judet, J.; Letournel, E. Fractures of the acetabulum: Classification and surgical approaches for open reduction. Preliminary report. J. Bone Jt. Surg. Am. 1964, 46, 1615–1646. [Google Scholar] [CrossRef]
- Letournel, E. Acetabulum fractures: Classification and management. J. Orthop. Trauma 2019, 33 (Suppl. S2), S1–S2. [Google Scholar] [CrossRef]
- Wright, J.G.; Swiontkowski, M.F.; Heckman, J.D. Introducing levels of evidence to the journal. J. Bone Jt. Surg. Am. 2003, 85, 1–3. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Chen, K.; Ji, Y.; Huang, Z.; Navinduth, R.; Yang, F.; Sun, T.; Xiong, Z.; Yao, S.; Ahn, J.; Guo, X. Single modified ilioinguinal approach for the treatment of acetabular fractures involving both columns. J. Orthop. Trauma 2018, 32, e428-34. [Google Scholar] [CrossRef]
- Elmadağ, M.; Güzel, Y.; Acar, M.A.; Uzer, G.; Arazi, M. The Stoppa approach versus the ilioinguinal approach for anterior acetabular fractures: A case control study assessing blood loss complications and function outcomes. Orthop. Traumatol. Surg. Res. 2014, 100, 675–680. [Google Scholar] [CrossRef]
- Elmadağ, M.; Guzel, Y.; Aksoy, Y.; Arazi, M. Surgical treatment of displaced acetabular fractures using a modified Stoppa approach. Orthopedics 2016, 39, e340–e345. [Google Scholar] [CrossRef]
- Fahmy, M.; Abdel Karim, M.; Khaled, S.A.; Khaled, S.A.; Abdelazeem, A.H.; Elnahal, W.A.; Elnahal, A. Single versus double column fixation in transverse fractures of the acetabulum: A randomised controlled trial. Injury 2018, 49, 1291–1296. [Google Scholar] [CrossRef]
- Fan, S.; Mai, Q.; Li, T.; Wang, H.; Yang, C.; Huang, H.; Liao, J.; Zhang, Y. Design and application of an acetabular integrative anatomic plate: A retrospective study of 178 cases with complex acetabular fractures. Orthop. Surg. 2023, 15, 2523–2531. [Google Scholar]
- Gupta, S.; Singh, J.; Virk, J.S. The role of trochanteric flip osteotomy in fixation of certain acetabular fractures. Chin. J. Traumatol. 2017, 20, 161–165. [Google Scholar] [CrossRef]
- Hammad, A.S.; El-Khadrawe, T.A.; Waly, A.H.; Abu-Sheasha, G.A. The efficacy of posterior plating and anterior column screw fixation in the management of T-shaped acetabular fractures—CART analysis of prospective cohort study. Injury 2017, 48, 680–686. [Google Scholar] [CrossRef]
- Hue, A.G.; Gauthé, R.; Tobenas-Dujardin, A.C.; Vallée, A.; Mouton, J.; Dujardin, F. Complex fractures of the acetabulum: Should the enlarged iliofemoral approach be abandoned? Results at 20 years’ follow-up. Orthop. Traumatol. Surg. Res. 2018, 104, 465–468. [Google Scholar] [CrossRef]
- Karim, M.A.; Abdelazeem, A.H.; Youness, M.; El Nahal, W.A. Fixation of quadrilateral plate fractures of the acetabulum using the buttress screw: A novel technique. Injury 2017, 48, 1813–1818. [Google Scholar] [CrossRef]
- Kizkapan, T.B.; Misir, A.; Uzun, E.; Ozcamdalli, M.; Yurdakul, E.; Argun, M. Comparison of acetabulum posterior wall fractures and fracture dislocations: Dislocation does not affect clinical and radiological outcomes. Acta Orthop. Belg. 2018, 84, 117–120. [Google Scholar]
- Kojima, K.E.; Munari, B.M.; Kubota, B.S.; Zanesco, L.; Proença, D.S.; Leonhardt, M.C.; Silva, J.D.S. Radiographic evaluation of immediate loading safety after surgical reduction in acetabular fractures: A comparative-retrospective study. Acta Ortop. Bras. 2022, 30, e256907. [Google Scholar] [CrossRef]
- Li, H.; Yang, H.; Wang, D.; Xu, Y.; Min, J.; Xu, X.; Li, Z.; Yuan, Y. Fractures of the posterior wall of the acetabulum: Treatment using internal fixation of two parallel reconstruction plates. Injury 2014, 45, 709–714. [Google Scholar] [CrossRef]
- Li, Y.L.; Tang, Y.Y. Displaced acetabular fractures in the elderly: Results after open reduction and internal fixation. Injury 2014, 45, 1908–1913. [Google Scholar] [CrossRef]
- Li, Z.; Li, J.; Li, Z.; Nie, S.; Zhang, H.; Li, M.; Liu, J.; Liu, Z.; Xu, G.; Zhang, L.; et al. Comparative study of anatomical locking plate and reconstruction plate in treating acetabular fractures. Int. Orthop. 2021, 45, 2727–2734. [Google Scholar] [CrossRef]
- Magu, N.K.; Gogna, P.; Singh, A.; Singla, R.; Rohilla, R.; Batra, A.; Mukhopadhyay, R. Long term results after surgical management of posterior wall acetabular fractures. J. Orthop. Traumatol. 2014, 15, 173–179. [Google Scholar] [CrossRef]
- Maini, L.; Batra, S.; Arora, S.; Singh, S.; Kumar, S.; Gautam, V.K. Surgical dislocation of the hip for reduction of acetabular fracture and evaluation of chondral damage. J. Orthop. Surg. 2014, 22, 18–23. [Google Scholar] [CrossRef]
- Park, K.S.; Chan, C.K.; Lee, G.W.; Ahn, H.W.; Yoon, T.R. Outcome of alternative approach to displaced acetabular fractures. Injury 2017, 48, 388–393. [Google Scholar] [CrossRef]
- Patil, A.; Attarde, D.S.; Haphiz, A.; Sancheti, P.; Shyam, A. A single approach for management of fractures involving both columns of the acetabulum: A case series of 23 patients. Strateg. Trauma Limb Reconstr. 2021, 16, 152–160. [Google Scholar] [CrossRef]
- Schwabe, P.; Altintas, B.; Schaser, K.D.; Druschel, C.; Kleber, C.; Haas, N.P.; Maerdian, S. Three-dimensional fluoroscopy-navigated percutaneous screw fixation of acetabular fractures. J. Orthop. Trauma 2014, 28, 700–706, discussion 706. [Google Scholar] [CrossRef]
- Selek, O.; Tosun, B.; Sarlak, A.Y. A new method for reduction quality assessment in acetabular fractures: Acetabular congruency measurement. Hip Int. 2021, 31, 435–439. [Google Scholar] [CrossRef]
- Uchida, K.; Kokubo, Y.; Yayama, T.; Nakajima, H.; Miyazaki, T.; Negoro, K.; Takeno, K.; Sawaguchi, T.; Watanabe, S.; Sugita, D.; et al. Fracture of the acetabulum: A retrospective review of ninety-one patients treated at a single institution. Eur. J. Orthop. Surg. Traumatol. 2013, 23, 155–163. [Google Scholar] [CrossRef]
- Yang, Y.; Sun, J.; Xiang, Z. The short- and mid-term follow-up of single-column fixation in transverse and posterior wall acetabular fractures. Orthop. Surg. 2022, 14, 65–72. [Google Scholar]
- Matta, J.M. Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J. Bone Jt. Surg. Am. 1996, 78, 1632–1645. [Google Scholar] [CrossRef]
- Matta, J.M.; Mehne, D.K.; Rom, R. Fractures of the acetabulum: Early results of a prospective study. Clin. Orthop. Relat. Res. 1986, 205, 241–250. [Google Scholar] [CrossRef]
- Haller, J.M.; Potter, M.Q.; Kubiak, E.N. Weight bearing after a periarticular fracture: What is the evidence? Orthop. Clin. N. Am. 2013, 44, 509–519. [Google Scholar] [CrossRef]
- Braun, B.J.; Histing, T.; Rollmann, M.F.R.; Menger, M.M.; Osche, D.; Orth, M.; Pohlemann, T.; Herath, S.C. Weight-bearing restrictions after acetabular fracture, necessity or false hope? A brief observational study. Acta Chir. Orthop. Traumatol. Cechoslov. 2022, 89, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Murena, L.; Canton, G.; Hoxhaj, B.; Sborgia, A.; Fattori, R.; Gulli, S.; Vaienti, E. Early weight bearing in acetabular and pelvic fractures. Acta Biomed. 2021, 92, e2021236. [Google Scholar] [CrossRef]
- Heare, A.; Kramer, N.; Salib, C.; Mauffrey, C. Early versus late weight-bearing protocols for surgically managed posterior wall acetabular fractures. Orthopedics 2017, 40, e652–e657. [Google Scholar] [CrossRef]
- Yoshida, H.; Faust, A.; Wilckens, J.; Kitagawa, M.; Fetto, J.; Chao, E.Y. Three-dimensional dynamic hip contact area and pressure distribution during activities of daily living. J. Biomech. 2006, 39, 1996–2004. [Google Scholar] [CrossRef]
- Bergmann, G.; Deuretzbacher, G.; Heller, M.; Graichen, F.; Rohlmann, A.; Strauss, J.; Duda, G.N. Hip contact forces and gait patterns from routine activities. J. Biomech. 2001, 34, 859–871. [Google Scholar] [CrossRef]
- Long, H.T.; Deng, Z.H.; Zou, M.; Lin, Z.Y.; Zhu, J.X.; Zhu, Y. Effects of the acetabular fracture index and other factors of posterior wall acetabular fracture on functional outcome. J. Int. Med. Res. 2017, 45, 1394–1405. [Google Scholar] [CrossRef]
- Kazemi, N.; Archdeacon, M.T. Immediate full weight bearing after percutaneous fixation of anterior column acetabulum fractures. J. Orthop. Trauma 2012, 26, 73–79. [Google Scholar] [CrossRef]
- Black, J.D.; Bhavikatti, M.; Al-Hadithy, N.; Hakmi, A.; Kitson, J. Early weight-bearing in operatively fixed ankle fractures: A systematic review. Foot (Edinb) 2013, 23, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Bouman, A.I.; Hemmen, B.; Evers, S.M.; van de Meent, H.; Ambergen, T.; Vos, P.E.; Brink, P.R.; Seelen, H.A. Effects of an integrated ‘Fast Track’ rehabilitation service for multi-trauma patients: A non-randomized clinical trial in the Netherlands. PLoS ONE 2017, 12, e0170047. [Google Scholar] [CrossRef] [PubMed]
- Heiman, E.; Menken, L.G.; Tang, A.; Vialonga, M.; Jankowski, J.M.; Liporace, F.A.; Yoon, R.S. Early versus standard weight bearing following operative treatment of tibial plateau fractures: Do we really have to wait so long? J. Knee Surg. 2024, 37, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Iliopoulos, E.; Galanis, N. Physiotherapy after tibial plateau fracture fixation: A systematic review of the literature. SAGE Open Med. 2020, 8, 2050312120965316. [Google Scholar] [CrossRef] [PubMed]
- Chiodo, C.P.; Macaulay, A.A.; Palms, D.A.; Smith, J.T.; Bluman, E.M. Patient compliance with postoperative lower-extremity non-weight-bearing restrictions. J. Bone Jt. Surg. Am. 2016, 98, 1563–1567. [Google Scholar] [CrossRef] [PubMed]
- Kalmet, P.; Maduro, C.; Verstappen, C.; Meys, G.; van Horn, Y.; van Vugt, R.; Janzing, H.; van der Veen, A.; Jaspars, C.; Sintenie, J.B.; et al. Effectiveness of permissive weight bearing in surgically treated trauma patients with peri- and intra-articular fractures of the lower extremities: A prospective comparative multicenter cohort study. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 1363–1371. [Google Scholar] [CrossRef] [PubMed]
- Bo, A.P.L.; Casas, L.; Cucho-Padin, G.; Hayashibe, m.; Elias, D. Control strategies for gait tele-rehabilitation system based on parallel robotics. Appl. Sci. 2021, 11, 11095. [Google Scholar] [CrossRef]
- Ciobanu, I.; Stanculescu, D.I.; Iliescu, A.; Popescu, A.M.; Seiciu, P.L.; Mikolajczyk, T.; Moldovan, F.; Berteanu, M. The usability pilot study of a mechatronic system for gait rehabilitation. Procedia Manuf. 2018, 22, 864–871. [Google Scholar] [CrossRef]
- Yiou, E.; Caderby, T.; Delafontaine, A.; Fourcade, P.; Honeine, J.L. Balance control during gait initiation: State-of-the-art and research perspectives. World J. Orthop. 2017, 8, 815–828. [Google Scholar] [CrossRef] [PubMed]
- Andrzejowski, P.; Holch, P.; Giannoudis, P.V. Measuring functional outcomes in major trauma: Can we do better? Eur. J. Trauma Emerg. Surg. 2022, 48, 1683–1698. [Google Scholar] [CrossRef]
- Jayakumar, P.; Heng, M.; Okelana, B.; Vrahas, M.; Rodriguez-Villalon, A.; Joeris, A. Patient-reported outcome measurement in orthopaedic trauma. J. Am. Acad. Orthop. Surg. 2023, 31, e906–e919. [Google Scholar] [CrossRef]
- Joeris, A.; Knoll, C.; Kalampoki, V.; Blumenthal, A.; Gaskell, G. Patient-reported outcome measurements in clinical routine of trauma, spine and craniomaxillofacial surgeons: Between expectations and reality: A survey among 1212 surgeons. BMJ Open 2018, 8, e020629. [Google Scholar] [CrossRef]
- Smerina, M.; Dumitrascu, A.G.; Spaulding, A.C.; Manz, J.W.; Chirila, R.M. Expanding the role of the surgical preoperative evaluation clinic: Impact on risk and quality outcome measures. Mayo Clin. Proc. Innov. Qual. Outcomes 2023, 7, 462–469. [Google Scholar] [CrossRef] [PubMed]




| Author(s) | Journal | Year Published | Grade of Recommendation/Level of Evidence | Methodological Index for Non-Randomized Studies (MINORS) Criteria |
|---|---|---|---|---|
| Fan, S. et al. [19] | Orthop Surg | 2023 | B/2b (individual cohort study or low-quality randomized control studies) | 12 (non-comparative study) |
| Kojima, K.E. et al. [25] | Acta Ortop Bras | 2022 | C/4 (case series, low-quality cohort, or case-control studies) | 20 (comparative study) |
| Yang, Y. et al. [36] | Orthop Surg | 2022 | C/4 (case series, low-quality cohort, or case-control studies) | 12 (non-comparative study) |
| Patil, A. et al. [32] | Strategies Trauma Limb Reconstr | 2021 | C/4 (case series, low-quality cohort, or case-control studies) | 12 (non-comparative study) |
| Li, Z. et al. [28] | Int Orthop | 2021 | C/4 (case series, low-quality cohort, or case-control studies) | 21 (comparative study) |
| Selek, O. et al. [34] | HIP International | 2019 | C/4 (case series, low-quality cohort, or case-control studies) | 13 (non-comparative study) |
| Chen, K. et al. [15] | J Orthop Trauma | 2018 | C/4 (case series, low-quality cohort, or case-control studies) | 12 (non-comparative study) |
| Hue, A.G. et al. [22] | Orthop Traumatol Surg Res | 2018 | C/4 (case series, low-quality cohort, or case-control studies) | 10 (non-comparative study) |
| Fahmy, M. et al. [18] | Injury | 2018 | B/2b (individual cohort study or low-quality randomized control studies) | 15 (non-comparative study) |
| Kizkapan, T.B. et al. [24] | Acta Orthop Belg | 2018 | C/4 (case series, low-quality cohort, or case-control studies) | 19 (comparative study) |
| Karin, M.A. et al. [23] | Injury | 2017 | C/4 (case series, low-quality cohort, or case-control studies) | 13 (non-comparative study) |
| Gupta, S. et al. [20] | Chin J Traumatol | 2017 | C/4 (case series, low-quality cohort, or case-control studies) | 11 (non-comparative study) |
| Hammad, A.S. et al. [21] | Injury | 2017 | B/2b (individual cohort study or low-quality randomized control studies) | 13 (non-comparative study) |
| Park, K.S. et al. [31] | Injury | 2017 | C/4 (case series, low-quality cohort, or case-control studies) | 13 (non-comparative study) |
| Elmadağ, M. et al. [17] | Orthopedics | 2016 | C/4 (case series, low-quality cohort, or case-control studies) | 15 (non-comparative study) |
| Li, Y.L. and Tang, Y.Y. [27] | Injury | 2014 | C/4 (case series, low-quality cohort, or case-control studies) | 15 (non-comparative study) |
| Magu, N.K. et al. [29] | J Orthop Traumatol | 2014 | C/4 (case series, low-quality cohort, or case-control studies) | 13 (non-comparative study) |
| Elmadağ, M. et al. [16] | Orthop Traumatol Surg Res | 2014 | C/4 (case series, low-quality cohort, or case-control studies) | 18 (comparative study) |
| Maini, L. et al. [30] | J Orthop Surg | 2014 | C/4 (case series, low-quality cohort, or case-control studies) | 9 (non-comparative study) |
| Schwabe, P. et al. [33] | J Orthop Trauma | 2014 | C/4 (case series, low-quality cohort, or case-control studies) | 15 (non-comparative study) |
| Li, H. et al. [26] | Injury | 2013 | C/4 (case series, low-quality cohort, or case-control studies) | 13 (non-comparative study) |
| Uchida, K. et al. [35] | Eur J Orthop Surg Traumatol | 2013 | C/4 (case series, low-quality cohort, or case-control studies) | 15 (non-comparative study) |
| Parameter | ||
|---|---|---|
| Male:female ratio * | 721:207 (77.6%:22.3%) | p = 0.0005 |
| Average age ± SD ** | 42.8 ± 10.9 years | |
| Letournel classification *** | 401 elementary fractures 614 associated fractures | p = 0.21 |
| Associated injuries | 236 skeletal injuries 32 non-skeletal (excluding neurological) injuries 11 peripheral nerve injuries 8 non-specified multiple traumas | p = 0.09 |
| Author(s) | Time to Surgery Mean ± SD (days) | Surgical Approach | Surgical Time Mean ± SD (minutes) | Blood Loss Mean ± SD (mL) |
|---|---|---|---|---|
| Fan, S. et al. [19] | 8.7 ± 2.6 (range: 5–21) | Lateral-rectus | 75 ± 29 (range: 35–150) | 440 ± 153 (range: 250–1400) |
| Kojima, K.E. et al. [25] | N/A | N/A | N/A | N/A |
| Yang, Y. et al. [36] | 7.1 | Kocher–Langenbeck | 135.8 (range: 90–230) | 405.4 (range: 200–650) |
| Patil, A. et al. [32] | 2.8 | Kocher–Langenbeck (n = 15), iliofemoral (n = 1), or modified anterior intrapelvic approach (n = 7) | N/A | N/A |
| Li, Z. et al. [28] | N/A | Kocher–Langenbeck (n = 35) or N/A (n = 48) | 154.97 ± 17.00 | 334.59 ± 23.73 |
| Selek, O. et al. [34] | N/A | N/A | N/A | N/A |
| Chen, K. et al. [15] | 9.2 ± 4.9 (range: 4–21) | Single modified ilioilioinguinal | 182 ± 40 | 793 ± 228 (range: 500–1500) |
| Hue, A.G. et al. [22] | 12 (range: 8–17) | Extended iliofemoral | 240 (range: 180–360) | N/A |
| Fahmy, M. et al. [18] | 8 ± 3 (range: 2–17) | Kocher–Langenbeck | N/A | range: 500–1000 |
| Kizkapan, T.B. et al. [24] | 2.3 (range: 1–6) | Kocher–Langenbeck | N/A | N/A |
| Karin, M.A. et al. [23] | 5.4 (range: 1–18) | Ilioinguinal (n = 36), modified Stoppa (n = 4), and additional Kocher–Langenbeck (n = 7) | 148.5 ± 33.8 | 741.2 ± 203.8 |
| Gupta, S. et al. [20] | 4.6 (range: 1–26) | Kocher–Langenbeck with trochanteric flip osteotomy | N/A | N/A |
| Hammad, A.S. et al. [21] | 6.5 | Kocher–Langenbeck | N/A | N/A |
| Park, K.S. et al. [31] | 5.7 (range: 3–15) | Kocher–Langenbeck and additional mini iliofemoral | 160 (range: 75–320) | N/A |
| Elmadağ, M. et al. [17] | N/A | Modified Stoppa | N/A | 970 (range: 800–1250) |
| Li, Y.L. and Tang, Y.Y. [27] | 6.6 (range: 2–15) | Ilioinguinal (n = 14), Kocher–Langenbeck (n = 11), and Ilioinguinal + Kocher–Langenbeck (n = 27) | N/A | N/A |
| Magu, N.K. et al. [29] | N/A | Kocher–Langenbeck with additional digastric trochanteric flip osteotomy (n = 3) | N/A | N/A |
| Elmadağ, M. et al. [16] | 3.7 | Ilioinguinal (n = 19) and modified Stoppa (n = 17) | N/A | 1140 (range: 450–2150) |
| Maini, L. et al. [30] | Within 3 weeks of injury | Kocher–Langenbeck with digastric trochanteric flip osteotomy | 150 (range: 90–240) | 800 (range: 350–1800) |
| Schwabe, P. et al. [33] | N/A | Percutaneous | N/A | N/A |
| Li, H. et al. [26] | 7.2 (range: 0–14) | Kocher–Langenbeck | 120 (range: 105–180) | 246 (range: 150–450) |
| Uchida, K. et al. [35] | 10 (range: 1–32) | Ilioinguinal (n = 19), Kocher–Langenbeck (n = 33), ilioinguinal + Kocher–Langenbeck (n = 13), and others (Smith-Peterson (2) and iliofemoral (4)) (n = 6) | N/A | N/A |
| Author(s) | Quality of Reduction | Postoperative Rehabilitation Protocol | Outcome Measurement |
|---|---|---|---|
| Fan, S. et al. [19] | Excellent in 131 cases, good in 31 cases, and poor in 16 cases | Isometric contraction training of lower limb muscles carried out 24 h after operation, toe-touch weight-bearing permitted 6–10 weeks after surgery, and full weight-bearing depending on the patient’s general condition and fracture healing state. | Excellent in 125 cases, good in 26 cases, and fair in 27 cases (MDPS) |
| Kojima, K.E. et al. [25] | Satisfactory in 61 cases in the non-weight-bearing group and 59 cases in the immediate weight-bearing group | 71 patients underwent rehabilitation with a non-weight-bearing protocol, while 66 patients underwent rehabilitation with immediate weight-bearing as tolerated. | N/A |
| Yang, Y. et al. [36] | Anatomic in 17 cases, imperfect in 3 cases, and poor in 4 cases | Physical therapy with isometric quadriceps- and abductor-strengthening exercises on the first postoperative day, passive hip movement at 2–3 days postoperatively, and active hip movement without weight-bearing at 3–4 weeks postoperatively. Patients with traumatic posterior hip dislocation maintained skeletal traction for 2–4 weeks before hip functional exercise. Partial weight-bearing gradually initiated at 8–12 weeks according to fracture healing. | Excellent in 10 cases, good in 6 cases, fair in 5 cases, and poor in 3 cases (MDPS) |
| Patil, A. et al. [32] | Acceptable in 23 cases | Patients were kept in bed for 2 weeks, followed by non-weight-bearing mobilization with the help of a walker for another 2 weeks. Partial weight-bearing was started at 1 month, which was increased to full weight-bearing at 4 months. | Mean modified MDPS of 14.95 (±3.46) and average HHS of 85.48 (±2.97) |
| Li, Z. et al. [28] | Excellent in 38 cases, good in 25 cases, fair in 17 cases, and poor in 3 cases | Isometric contraction training of the lower limbs was allowed right after the patient awoke from anesthesia. All patients remained non-weight-bearing for four weeks, and progressive weight-bearing was allowed after radiological evidence of fracture healing. | Excellent in 26 cases, good in 36 cases, fair in 13 cases, and poor in 8 cases (MDPS) |
| Selek, O. et al. [34] | Excellent in 20 cases, good in 24 cases, fair in 6 cases, and poor in 5 cases | Passive ROM exercises of the hip, including isotonic and isometric strengthening exercises applied just after the operation, and toe-touch weight-bearing from 6 to 12 weeks. | Excellent in 16 cases, good in 26 cases, fair in 10 cases, and poor in 3 cases (MDPS) |
| Chen, K. et al. [15] | Excellent in 17 cases, good in 4 cases, and poor in 1 case | Non-weight-bearing exercises were performed in bed within 4 weeks postoperatively, and patients were allowed to walk with a pair of crutches 4–6 weeks after operation and with a single crutch 6–12 weeks after operation. | Excellent in 14 cases, good in 6 cases, and poor in 2 cases (MDPS) |
| Hue, A.G. et al. [22] | Anatomic in all cases | Strict bedrest with continuous transtibial traction for 6 weeks. Passive mobilization of the hip after day 10. Raise from bed with 2 forearm crutches at week 6, with progressive painless resumption of weight-bearing. | N/A |
| Fahmy, M. et al. [18] | Anatomic in 24 cases and imperfect in 6 cases | Early ROM exercises and non-weight-bearing regimen on the affected limb for 6 weeks, followed by partial weight-bearing until 12 weeks, finally progressing to full weight-bearing at 12 weeks. | Excellent to good in 26 patients and fair to poor in 4 patients (MDPS) |
| Kizkapan, T.B. et al. [24] | Excellent in 6 cases, good in 13 cases, fair in 2 cases, and poor in 5 cases | All patients were allowed partial weight-bearing 3 months postoperatively and started full weight-bearing at 4–6 months postoperatively. | Excellent in 6 cases, good in 15 cases, and fair in 5 cases (MDPS) |
| Karin, M.A. et al. [23] | Anatomic in 23 cases, imperfect in 9 cases, and poor in 3 cases | ROM started from postoperative day 1, with weight-bearing delayed until full radiological and clinical unions were evident. | Excellent in 13 cases, good in 23 cases, fair in 3 cases, and poor in 1 case (MDPS) |
| Gupta, S. et al. [20] | N/A | Patients allowed for sitting, side turning, and pelvic lifting exercises on postoperative day 1, with toe-touch weight-bearing allowed within the first week and full weight-bearing allowed at the end of 3 months. | Excellent in 16 cases, good in 6 cases, and fair in 2 cases (MDPS) |
| Hammad, A.S. et al. [21] | Anatomic in 21 cases, imperfect in 4 cases, and poor in 9 cases | Non-weight bearing for 4 weeks, protected weight-bearing for 8 weeks, and full-weight bearing after 12 weeks. | Excellent to good in 25 cases and fair to poor in 9 cases (MDPS) |
| Park, K.S. et al. [31] | Anatomic in 12 cases, imperfect in 6 cases, and poor in 5 cases | Active ROM started the day after surgery, non-weight-bearing walking with two crutches from postoperative day 3, partial weight-bearing at 6 weeks, and full weight-bearing at 12 weeks. | Excellent in 15 cases, good in 5 cases, fair in 1 case, and poor in 2 cases (HHS) |
| Elmadağ, M. et al. [17] | Anatomic in 29 cases, imperfect in 5 cases, and poor in 2 cases | Flat-footed weight-bearing for 12 weeks. | Excellent in 14 cases, good in 12 cases, fair in 5 cases, and poor in 5 cases (HHS); excellent in 13 cases, good in 20 cases, fair in 2 cases, and poor in 1 case (MDPS) |
| Li, Y.L. and Tang, Y.Y. [27] | Excellent in 22 cases, good in 15 cases, fair in 6 cases, and poor in 9 cases | Sit up in bed on the first postoperative day with active and passive functional exercises on the operated hip and progressive resistance exercises of the hip adductors, quadriceps, and hamstrings. Patients encouraged to use walkers between 1 and 6 weeks and crutches between 6 and 12 weeks. Full weight-bearing according to tolerance after 12 weeks. | Excellent in 24 cases, good in 19 cases, fair in 2 cases, and poor in 7 cases (HHS); excellent in 14 cases, good in 29 cases, fair in 2 cases, and poor in 7 cases (MDPS) |
| Magu, N.K. et al. [29] | Excellent in 10 cases, good in 8 cases, fair in 5 cases, and poor in 3 cases | Intermittent, pain-free quadriceps, hip, and knee flexion exercises with traction starting on the second postoperative day, partial weight-bearing permitted 6 weeks after surgery, and gradually progressing to full weight-bearing at 12 weeks. | Excellent in 14 cases, good in 6 cases, fair in 3 cases, and poor in 3 cases (MDPS) |
| Elmadağ, M. et al. [16] | N/A | Crutches used for 6 weeks with weight-bearing not permitted, followed by one crutch for 6 more weeks, with partial weight-bearing allowed. Active and passive ROM exercises started in the early postoperative period. | Excellent in 21 cases, good in 12 cases, and fair in 3 cases (HHS); excellent in 18 cases, good in 14 cases, and fair in 4 cases (MDPS) |
| Maini, L. et al. [30] | Anatomic in 6 cases and satisfactory in 16 cases | Skeletal traction for 3 weeks, non-weight-bearing status for 6–12 weeks, depending on stability and fixation of the joint, and full weight-bearing after 12–20 weeks. | Extremely good in 6 cases, good in 13 cases, medium in 2 cases, and fair in 1 case |
| Schwabe, P. et al. [33] | Anatomic in all cases | Supervised mobilization with 30 kg of weight-bearing on the ipsilateral extremity with crutches or a mobile walking device started during the first day after the operation, with full weight-bearing after 6 weeks postoperatively. | Excellent in 8 patients and good in 4 patients (HHS) |
| Li, H. et al. [26] | Excellent in 45 cases, good in 10 cases, and fair in 2 cases | Joint exercise recommended as tolerated by pain, activities limited for an average of 12 weeks before partial weight-bearing was permitted, depending on the fracture stability, and full weight-bearing only after confirmed clinical and radiological fracture union. | Excellent or extremely good in 45 cases, good in 8 cases, fair in 2 cases, and poor in 2 cases |
| Uchida, K. et al. [35] | Anatomic in 42 cases, satisfactory in 27 cases, and unsatisfactory in 2 cases | Patients enrolled in physical therapy program on the third postoperative day, starting with hip (affected side) abduction and flexion, followed by isometric and then isotonic exercise, allowing sitting from 1 week and walking using a single cane without orthosis from 10 weeks. | N/A |
| Parameter | ||
|---|---|---|
| Follow-up | From 6 weeks to 9 years | |
| Complication(s) | None in 12 cases | |
| Heterotopic ossification in 52 cases | 5.1% | |
| Posttraumatic hip arthritis in 41 cases | 4.0% | |
| AVN of femoral head in 17 cases | 1.6% | |
| Thromboembolic complications in 24 cases | 2.3% | |
| Postoperative peripheral nerve injuries in 28 cases | 2.7% | |
| Sciatic nerve palsy in 14 cases | ||
| Lateral femoral cutaneous nerve palsy in 13 cases | ||
| Obturator nerve palsy in 1 case | ||
| Others | 4.1% | |
| Partial iliac vein damage in 1 case | ||
| Massive bleeding in 3 cases | ||
| Persistent drainage in 5 cases | ||
| Wound infection in 13 cases | ||
| Incisional hernia with mild symptoms 1 year after surgery in 1 case | ||
| Implant loosening or irritation in 4 cases | ||
| Loss of reduction in 12 cases | ||
| Delayed union in 2 cases | ||
| Femoroacetabular pincer-type impingement in 1 case |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giordano, V.; Pires, R.E.; Faria, L.P.G.d.; Temtemples, I.; Macagno, T.; Freitas, A.; Joeris, A.; Giannoudis, P.V. Doctor, When Should I Start Walking? Revisiting Postoperative Rehabilitation and Weight-Bearing Protocols in Operatively Treated Acetabular Fractures: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 3570. https://doi.org/10.3390/jcm13123570
Giordano V, Pires RE, Faria LPGd, Temtemples I, Macagno T, Freitas A, Joeris A, Giannoudis PV. Doctor, When Should I Start Walking? Revisiting Postoperative Rehabilitation and Weight-Bearing Protocols in Operatively Treated Acetabular Fractures: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(12):3570. https://doi.org/10.3390/jcm13123570
Chicago/Turabian StyleGiordano, Vincenzo, Robinson Esteves Pires, Luiz Paulo Giorgetta de Faria, Igor Temtemples, Tomas Macagno, Anderson Freitas, Alexander Joeris, and Peter V. Giannoudis. 2024. "Doctor, When Should I Start Walking? Revisiting Postoperative Rehabilitation and Weight-Bearing Protocols in Operatively Treated Acetabular Fractures: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 12: 3570. https://doi.org/10.3390/jcm13123570
APA StyleGiordano, V., Pires, R. E., Faria, L. P. G. d., Temtemples, I., Macagno, T., Freitas, A., Joeris, A., & Giannoudis, P. V. (2024). Doctor, When Should I Start Walking? Revisiting Postoperative Rehabilitation and Weight-Bearing Protocols in Operatively Treated Acetabular Fractures: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 13(12), 3570. https://doi.org/10.3390/jcm13123570








