The Identification and Evaluation of Interleukin-7 as a Myokine Biomarker for Peripheral Artery Disease Prognosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Design
2.3. Patient Recruitment
2.4. Baseline Characteristics
2.5. Quantification of Plasma Myokine Levels
2.6. Follow-Up and Outcomes
2.7. Model Development and Evaluation
2.8. Statistical Analysis
3. Results
3.1. Patients
3.2. Plasma Concentrations of Myokines
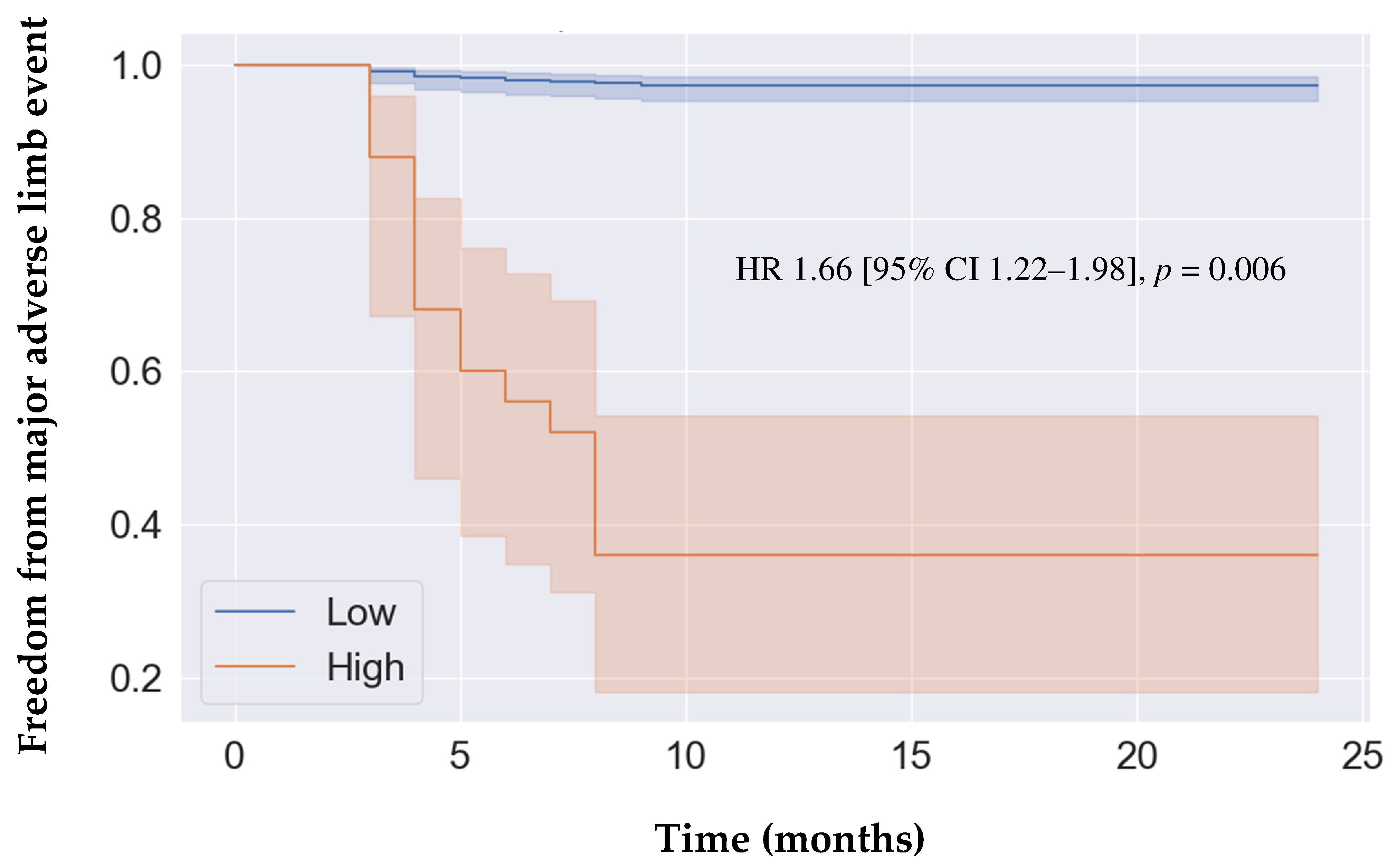
3.3. Adverse Limb Events
3.4. Model Performance
4. Discussion
4.1. Summary of Findings
4.2. Comparison to Existing Literature
4.3. Explanation of Findings
4.4. Implications
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zemaitis, M.R.; Boll, J.M.; Dreyer, M.A. Peripheral Arterial Disease. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Olin, J.W.; Sealove, B.A. Peripheral Artery Disease: Current Insight into the Disease and Its Diagnosis and Management. Mayo Clin. Proc. 2010, 85, 678–692. [Google Scholar] [CrossRef]
- Mehta, A.; Dhindsa, D.S.; Hooda, A.; Nayak, A.; Massad, C.S.; Rao, B.; Makue, L.F.; Rajani, R.R.; Alabi, O.; Quyyumi, A.A.; et al. Premature Atherosclerotic Peripheral Artery Disease: An Underrecognized and Undertreated Disorder with a Rising Global Prevalence. Trends Cardiovasc. Med. 2021, 31, 351–358. [Google Scholar] [CrossRef]
- Cooke, J.P.; Wilson, A.M. Biomarkers of Peripheral Arterial Disease. J. Am. Coll. Cardiol. 2010, 55, 2017–2023. [Google Scholar] [CrossRef]
- Zamzam, A.; Syed, M.H.; Rotstein, O.D.; Eikelboom, J.; Klein, D.J.; Singh, K.K.; Abdin, R.; Qadura, M. Validating Fatty Acid Binding Protein 3 as a Diagnostic and Prognostic Biomarker for Peripheral Arterial Disease: A Three-Year Prospective Follow-up Study. EClinicalMedicine 2023, 55, 101766. [Google Scholar] [CrossRef]
- Severinsen, M.C.K.; Pedersen, B.K. Muscle–Organ Crosstalk: The Emerging Roles of Myokines. Endocr. Rev. 2020, 41, 594–609. [Google Scholar] [CrossRef]
- Syed, M.H.; Zamzam, A.; Khan, H.; Singh, K.; Forbes, T.L.; Rotstein, O.; Abdin, R.; Eikelboom, J.; Qadura, M. Fatty Acid Binding Protein 3 Is Associated with Peripheral Arterial Disease. JVS-Vasc. Sci. 2020, 1, 168–175. [Google Scholar] [CrossRef]
- Li, B.; Zamzam, A.; Syed, M.H.; Jahanpour, N.; Jain, S.; Abdin, R.; Qadura, M. Urinary Fatty Acid Binding Protein 3 Has Prognostic Value in Peripheral Artery Disease. Front. Cardiovasc. Med. 2022, 9, 875244. [Google Scholar] [CrossRef]
- Li, B.; Zamzam, A.; Syed, M.H.; Djahanpour, N.; Jain, S.; Abdin, R.; Qadura, M. Fatty Acid Binding Protein 4 Has Prognostic Value in Peripheral Artery Disease. J. Vasc. Surg. 2023, 78, 719–726. [Google Scholar] [CrossRef]
- Zamzam, A.; Syed, M.H.; Harlock, J.; Eikelboom, J.; Singh, K.K.; Abdin, R.; Qadura, M. Urinary Fatty Acid Binding Protein 3 (uFABP3) Is a Potential Biomarker for Peripheral Arterial Disease. Sci. Rep. 2021, 11, 11061. [Google Scholar] [CrossRef]
- Li, B.; Djahanpour, N.; Zamzam, A.; Syed, M.H.; Jain, S.; Arfan, S.; Abdin, R.; Qadura, M. The Prognostic Capability of Inflammatory Proteins in Predicting Peripheral Artery Disease Related Adverse Events. Front. Cardiovasc. Med. 2022, 9, 1073751. [Google Scholar] [CrossRef]
- Li, B.; Zamzam, A.; Syed, M.H.; Jahanpour, N.; Jain, S.; Abdin, R.; Qadura, M. Urinary Cystatin C Has Prognostic Value in Peripheral Artery Disease. Biomolecules 2022, 12, 860. [Google Scholar] [CrossRef]
- Batra, J.; Buttar, R.S.; Kaur, P.; Kreimerman, J.; Melamed, M.L. FGF-23 and Cardiovascular Disease: Review of Literature. Curr. Opin. Endocrinol. Diabetes Obes. 2016, 23, 423–429. [Google Scholar] [CrossRef]
- Kuang, N.; Shu, B.; Yang, F.; Li, S.; Zhang, M. TRAIL or TRAIL-R2 as a Predictive Biomarker for Mortality or Cardiovascular Events: A Systematic Review and Meta-Analysis. J. Cardiovasc. Pharmacol. 2023, 81, 348–354. [Google Scholar] [CrossRef]
- Damås, J.K.; Waehre, T.; Yndestad, A.; Otterdal, K.; Hognestad, A.; Solum, N.O.; Gullestad, L.; Frøland, S.S.; Aukrust, P. Interleukin-7-Mediated Inflammation in Unstable Angina: Possible Role of Chemokines and Platelets. Circulation 2003, 107, 2670–2676. [Google Scholar] [CrossRef]
- Hoogeveen, R.C.; Morrison, A.; Boerwinkle, E.; Miles, J.S.; Rhodes, C.E.; Sharrett, A.R.; Ballantyne, C.M. Plasma MCP-1 Level and Risk for Peripheral Arterial Disease and Incident Coronary Heart Disease: Atherosclerosis Risk in Communities Study. Atherosclerosis 2005, 183, 301–307. [Google Scholar] [CrossRef]
- Berezin, A.E.; Berezin, A.A.; Lichtenauer, M. Myokines and Heart Failure: Challenging Role in Adverse Cardiac Remodeling, Myopathy, and Clinical Outcomes. Dis. Markers 2021, 2021, 6644631. [Google Scholar] [CrossRef]
- Boreskie, K.F.; Oldfield, C.J.; Hay, J.L.; Moffatt, T.L.; Hiebert, B.M.; Arora, R.C.; Duhamel, T.A. Myokines as Biomarkers of Frailty and Cardiovascular Disease Risk in Females. Exp. Gerontol. 2020, 133, 110859. [Google Scholar] [CrossRef]
- Walsh, K. Adipokines, Myokines and Cardiovascular Disease. Circ. J. Off. J. Jpn. Circ. Soc. 2009, 73, 13–18. [Google Scholar] [CrossRef]
- Chung, H.S.; Choi, K.M. Adipokines and Myokines: A Pivotal Role in Metabolic and Cardiovascular Disorders. Curr. Med. Chem. 2018, 25, 2401–2415. [Google Scholar] [CrossRef]
- Barbalho, S.M.; Prado Neto, E.V.; De Alvares Goulart, R.; Bechara, M.D.; Baisi Chagas, E.F.; Audi, M.; Guissoni Campos, L.M.; Landgraf Guiger, E.; Buchaim, R.L.; Buchaim, D.V.; et al. Myokines: A Descriptive Review. J. Sports Med. Phys. Fit. 2020, 60, 1583–1590. [Google Scholar] [CrossRef]
- Parvar, S.L.; Fitridge, R.; Dawson, J.; Nicholls, S.J. Medical and Lifestyle Management of Peripheral Arterial Disease. J. Vasc. Surg. 2018, 68, 1595–1606. [Google Scholar] [CrossRef]
- Cornejo Del Río, V.; Mostaza, J.; Lahoz, C.; Sánchez-Arroyo, V.; Sabín, C.; López, S.; Patrón, P.; Fernández-García, P.; Fernández-Puntero, B.; Vicent, D.; et al. Prevalence of Peripheral Artery Disease (PAD) and Factors Associated: An Epidemiological Analysis from the Population-Based Screening PRE-Diabetes and Type 2 DIAbetes (SPREDIA-2) Study. PLoS ONE 2017, 12, e0186220. [Google Scholar] [CrossRef]
- Duval, S.; Massaro, J.M.; Jaff, M.R.; Boden, W.E.; Alberts, M.J.; Califf, R.M.; Eagle, K.A.; D’Agostino, R.B.; Pedley, A.; Fonarow, G.C.; et al. An Evidence-Based Score to Detect Prevalent Peripheral Artery Disease (PAD). Vasc. Med. 2012, 17, 342–351. [Google Scholar] [CrossRef]
- Gouda, P.; Ramasundarahettige, C.; Anand, S.; Muhlhoffer, E.; Berkowitz, S.; Fox, K.A.; Eikelboom, J.; Welsh, R. Clinical Factors Associated with Peripheral Artery Disease in Patients with Documented Coronary Artery Disease: A Post Hoc Analysis of the COMPASS Trial. Atherosclerosis 2021, 331, 38–44. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Collins, G.S.; Moons, K.G.M.; Dhiman, P.; Riley, R.D.; Beam, A.L.; Calster, B.V.; Ghassemi, M.; Liu, X.; Reitsma, J.B.; van Smeden, M.; et al. TRIPOD+AI Statement: Updated Guidance for Reporting Clinical Prediction Models That Use Regression or Machine Learning Methods. BMJ 2024, 385, e078378. [Google Scholar] [CrossRef]
- Gul, F.; Janzer, S.F. Peripheral Vascular Disease. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. J. Am. Coll. Cardiol. 2019, 73, e285–e350. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E.; Collins, K.J.; Dennison, H.C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. J. Am. Coll. Cardiol. 2018, 71, e127–e248. [Google Scholar] [CrossRef]
- Luminex Assays, Multiplex Immunoassays. Available online: https://www.bio-techne.com/ (accessed on 6 May 2023).
- Kodama, H.; Fukuda, K.; Pan, J.; Makino, S.; Baba, A.; Hori, S.; Ogawa, S. Leukemia Inhibitory Factor, a Potent Cardiac Hypertrophic Cytokine, Activates the JAK/STAT Pathway in Rat Cardiomyocytes. Circ. Res. 1997, 81, 656–663. [Google Scholar] [CrossRef]
- Jougasaki, M.; Leskinen, H.; Larsen, A.M.; Cataliotti, A.; Chen, H.H.; Burnett, J.C. Leukemia Inhibitory Factor Is Augmented in the Heart in Experimental Heart Failure. Eur. J. Heart Fail. 2003, 5, 137–145. [Google Scholar] [CrossRef]
- Mohri, T.; Fujio, Y.; Maeda, M.; Ito, T.; Iwakura, T.; Oshima, Y.; Uozumi, Y.; Segawa, M.; Yamamoto, H.; Kishimoto, T.; et al. Leukemia Inhibitory Factor Induces Endothelial Differentiation in Cardiac Stem Cells. J. Biol. Chem. 2006, 281, 6442–6447. [Google Scholar] [CrossRef]
- Luminex Assays—CA. Available online: https://www.thermofisher.com/ca/en/home/life-science/antibodies/immunoassays/procartaplex-assays-luminex.html (accessed on 18 December 2021).
- MAGPIX® System|xMAP Instrument|Luminex Corporation. Available online: https://www.luminexcorp.com/magpix-system/ (accessed on 18 December 2021).
- xPONENT® Software for xMAP® Instruments. Luminex Corp. Available online: https://int.diasorin.com/en/luminex-ltg/reagents-accessories/software (accessed on 1 May 2024).
- Rigatti, S.J. Random Forest. J. Insur. Med. 2017, 47, 31–39. [Google Scholar] [CrossRef]
- Song, Y.-Y.; Lu, Y. Decision Tree Methods: Applications for Classification and Prediction. Shanghai Arch. Psychiatry 2015, 27, 130–135. [Google Scholar] [CrossRef]
- Elfanagely, O.; Toyoda, Y.; Othman, S.; Mellia, J.A.; Basta, M.; Liu, T.; Kording, K.; Ungar, L.; Fischer, J.P. Machine Learning and Surgical Outcomes Prediction: A Systematic Review. J. Surg. Res. 2021, 264, 346–361. [Google Scholar] [CrossRef]
- Bektaş, M.; Tuynman, J.B.; Costa Pereira, J.; Burchell, G.L.; van der Peet, D.L. Machine Learning Algorithms for Predicting Surgical Outcomes after Colorectal Surgery: A Systematic Review. World J. Surg. 2022, 46, 3100–3110. [Google Scholar] [CrossRef]
- Senders, J.T.; Staples, P.C.; Karhade, A.V.; Zaki, M.M.; Gormley, W.B.; Broekman, M.L.D.; Smith, T.R.; Arnaout, O. Machine Learning and Neurosurgical Outcome Prediction: A Systematic Review. World Neurosurg. 2018, 109, 476–486.e1. [Google Scholar] [CrossRef]
- Hicks, S.A.; Strümke, I.; Thambawita, V.; Hammou, M.; Riegler, M.A.; Halvorsen, P.; Parasa, S. On Evaluation Metrics for Medical Applications of Artificial Intelligence. Sci. Rep. 2022, 12, 5979. [Google Scholar] [CrossRef]
- Ruopp, M.D.; Perkins, N.J.; Whitcomb, B.W.; Schisterman, E.F. Youden Index and Optimal Cut-Point Estimated from Observations Affected by a Lower Limit of Detection. Biom. J. 2008, 50, 419–430. [Google Scholar] [CrossRef]
- SPSS Software. Available online: https://www.ibm.com/analytics/spss-statistics-software (accessed on 18 December 2021).
- Ross, E.G.; Jung, K.; Dudley, J.T.; Li, L.; Leeper, N.J.; Shah, N.H. Predicting Future Cardiovascular Events in Patients With Peripheral Artery Disease Using Electronic Health Record Data. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e004741. [Google Scholar] [CrossRef]
- Lorenzetti, B.B.; Veiga, F.H.; Canetti, C.A.; Poole, S.; Cunha, F.Q.; Ferreira, S.H. Cytokine-Induced Neutrophil Chemoattractant 1 (CINC-1) Mediates the Sympathetic Component of Inflammatory Mechanical Hypersensitivitiy in Rats. Eur. Cytokine Netw. 2002, 13, 456–461. [Google Scholar]
- Padgett, L.E.; Dinh, H.Q.; Wu, R.; Gaddis, D.E.; Araujo, D.J.; Winkels, H.; Nguyen, A.; McNamara, C.A.; Hedrick, C.C. Naive CD8+ T Cells Expressing CD95 Increase Human Cardiovascular Disease Severity. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 2845–2859. [Google Scholar] [CrossRef]
- Damås, J.K.; Boullier, A.; Waehre, T.; Smith, C.; Sandberg, W.J.; Green, S.; Aukrust, P.; Quehenberger, O. Expression of Fractalkine (CX3CL1) and Its Receptor, CX3CR1, Is Elevated in Coronary Artery Disease and Is Reduced during Statin Therapy. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 2567–2572. [Google Scholar] [CrossRef]
- Song, L.; Sun, J.; Söderholm, M.; Melander, O.; Orho-Melander, M.; Nilsson, J.; Borné, Y.; Engström, G. Association of TIM-1 (T-Cell Immunoglobulin and Mucin Domain 1) With Incidence of Stroke. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1777–1786. [Google Scholar] [CrossRef]
- Chen, D.; Tang, T.-X.; Deng, H.; Yang, X.-P.; Tang, Z.-H. Interleukin-7 Biology and Its Effects on Immune Cells: Mediator of Generation, Differentiation, Survival, and Homeostasis. Front. Immunol. 2021, 12, 747324. [Google Scholar] [CrossRef]
- Yan, M.; Yang, Y.; Zhou, Y.; Yu, C.; Li, R.; Gong, W.; Zheng, J. Interleukin-7 Aggravates Myocardial Ischaemia/Reperfusion Injury by Regulating Macrophage Infiltration and Polarization. J. Cell. Mol. Med. 2021, 25, 9939–9952. [Google Scholar] [CrossRef]
- Mihailovic, P.M.; Lio, W.M.; Yano, J.; Zhou, J.; Zhao, X.; Chyu, K.-Y.; Shah, P.K.; Cercek, B.; Dimayuga, P.C. IL-7R Blockade Reduces Post-Myocardial Infarction-Induced Atherosclerotic Plaque Inflammation in ApoE−/- Mice. Biochem. Biophys. Rep. 2019, 19, 100647. [Google Scholar] [CrossRef]
- Stoltzfus, J.C. Logistic Regression: A Brief Primer. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2011, 18, 1099–1104. [Google Scholar] [CrossRef]
- Kia, B.; Mendes, A.; Parnami, A.; George, R.; Mobley, K.; Ditto, W.L. Nonlinear Dynamics Based Machine Learning: Utilizing Dynamics-Based Flexibility of Nonlinear Circuits to Implement Different Functions. PLoS ONE 2020, 15, e0228534. [Google Scholar] [CrossRef]
- Chatterjee, P.; Cymberknop, L.J.; Armentano, R.L.; Chatterjee, P.; Cymberknop, L.J.; Armentano, R.L. Nonlinear Systems in Healthcare towards Intelligent Disease Prediction. In Nonlinear Systems—Theoretical Aspects and Recent Applications; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- Smith, B.J.; Silva-Costa, L.C.; Martins-de-Souza, D. Human Disease Biomarker Panels through Systems Biology. Biophys. Rev. 2021, 13, 1179–1190. [Google Scholar] [CrossRef]
- Couronné, R.; Probst, P.; Boulesteix, A.-L. Random Forest versus Logistic Regression: A Large-Scale Benchmark Experiment. BMC Bioinform. 2018, 19, 270. [Google Scholar] [CrossRef]
- Flores, A.M.; Demsas, F.; Leeper, N.J.; Ross, E.G. Leveraging Machine Learning and Artificial Intelligence to Improve Peripheral Artery Disease Detection, Treatment, and Outcomes. Circ. Res. 2021, 128, 1833–1850. [Google Scholar] [CrossRef]
- Nakar, S.; Vinker, S.; Neuman, S.; Kitai, E.; Yaphe, J. Baseline Tests or Screening: What Tests Do Family Physicians Order Routinely on Their Healthy Patients? J. Med. Screen. 2002, 9, 133–134. [Google Scholar] [CrossRef]
- Akbari, C.M.; Stone, L. Accreditation and Credentialing in the Vascular Laboratory. Semin. Vasc. Surg. 2002, 15, 178–181. [Google Scholar] [CrossRef]
- Burns, P.; Gough, S.; Bradbury, A.W. Management of Peripheral Arterial Disease in Primary Care. BMJ 2003, 326, 584–588. [Google Scholar] [CrossRef]
- Koh, C.E.; Walker, S.R. Vascular Surgery Consults: A Significant Workload. ANZ J. Surg. 2007, 77, 352–354. [Google Scholar] [CrossRef]
- Nishimiya, K.; Matsumoto, Y.; Shimokawa, H. Recent Advances in Vascular Imaging. Arterioscler. Thromb. Vasc. Biol. 2020, 40, e313–e321. [Google Scholar] [CrossRef]
- Eikelboom, J.W.; Connolly, S.J.; Bosch, J.; Dagenais, G.R.; Hart, R.G.; Shestakovska, O.; Diaz, R.; Alings, M.; Lonn, E.M.; Anand, S.S.; et al. Rivaroxaban with or without Aspirin in Stable Cardiovascular Disease. N. Engl. J. Med. 2017, 377, 1319–1330. [Google Scholar] [CrossRef]
- Farber, A.; Menard, M.T.; Conte, M.S.; Kaufman, J.A.; Powell, R.J.; Choudhry, N.K.; Hamza, T.H.; Assmann, S.F.; Creager, M.A.; Cziraky, M.J.; et al. Surgery or Endovascular Therapy for Chronic Limb-Threatening Ischemia. N. Engl. J. Med. 2022, 387, 2305–2316. [Google Scholar] [CrossRef]
- Caetano, A.P.; Conde Vasco, I.; Veloso Gomes, F.; Costa, N.V.; Luz, J.H.; Spaepen, E.; Formiga, A.; Coimbra, É.; Neves, J.; Bilhim, T. Successful Revascularization Has a Significant Impact on Limb Salvage Rate and Wound Healing for Patients with Diabetic Foot Ulcers: Single-Centre Retrospective Analysis with a Multidisciplinary Approach. Cardiovasc. Intervent. Radiol. 2020, 43, 1449–1459. [Google Scholar] [CrossRef]
- Margolis, J.; Barron, J.J.; Grochulski, W.D. Health Care Resources and Costs for Treating Peripheral Artery Disease in a Managed Care Population: Results from Analysis of Administrative Claims Data. J. Manag. Care Pharm. 2005, 11, 727–734. [Google Scholar] [CrossRef]
| Non-PAD (n = 164) | PAD (n = 312) | p | |
|---|---|---|---|
| Age, mean (SD) | 65 (12) | 71 (10) | <0.001 |
| Female sex | 67 (41) | 109 (35) | 0.204 |
| Hypertension | 96 (59) | 257 (82) | <0.001 |
| Dyslipidemia | 100 (61) | 263 (84) | <0.001 |
| Diabetes | 34 (21) | 131 (42) | <0.001 |
| Past smoking | 71 (43) | 171 (55) | 0.001 |
| Current smoking | 35 (21) | 78 (25) | 0.002 |
| Congestive heart failure | 4 (2) | 11 (4) | 0.519 |
| Coronary artery disease | 34 (21) | 118 (38) | <0.001 |
| Previous stroke | 13 (8) | 51 (16) | 0.011 |
| Acetylsalicylic acid | 99 (60) | 251 (80) | <0.001 |
| Statin | 93 (57) | 229 (73) | <0.001 |
| ACE-Is/ARBs | 74 (45) | 216 (66) | 0.001 |
| Beta blockers | 50 (30) | 134 (41) | 0.001 |
| Calcium channel blockers | 34 (21) | 82 (25) | 0.079 |
| Hydrochlorothiazide or furosemide | 17 (10) | 41 (13) | 0.190 |
| Oral antihyperglycemic agents | 8 (5) | 24 (8) | 0.201 |
| Insulin | 6 (4) | 22 (7) | 0.255 |
| Non-PAD (n = 164) | PAD (n = 312) | p | |
|---|---|---|---|
| Median (25%, 75% IQR) | Median (25%, 75% IQR) | ||
| FGF-23 | 12.19 (9.41, 17.39) | 15.33 (10.43, 23.67) | <0.001 |
| TRAIL R2 | 25.65 (19.40, 35.12) | 32.76 (24.37, 45.84) | <0.001 |
| IL-7 | 3.41 (2.88, 4.21) | 3.78 (3.14, 5.05) | 0.001 |
| MCP-1 | 88.27 (67.44, 115.88) | 98.66 (69.15, 124.90) | 0.031 |
| LIF | 10.54 (7.19, 14.40) | 10.89 (7.92, 14.58) | 0.246 |
| No CAD (n = 324) | CAD (n = 152) | p | |
|---|---|---|---|
| Median (25%, 75% IQR) | Median (25%, 75% IQR) | ||
| FGF-23 | 13.54 (9.46, 20.58) | 15.79 (10.42, 23.43) | 0.958 |
| TRAIL R2 | 28.19 (20.57, 40.15) | 33.38 (24.94, 46.22) | 0.440 |
| IL-7 | 3.63 (2.88, 4.60) | 3.69 (3.16, 4.66) | 0.593 |
| MCP-1 | 94.00 (67.18, 123.16) | 97.34 (70.18, 123.03) | 0.559 |
| LIF | 10.89 (7.92, 14.19) | 11.21 (8.12, 14.88) | 0.876 |
| Non-PAD (n = 164) | PAD (n = 312) | p | |
|---|---|---|---|
| Major adverse limb event | 0 (0) | 28 (9) | 0.001 |
| Vascular intervention | 0 (0) | 19 (6) | 0.001 |
| Major amputation | 0 (0) | 17 (5) | 0.002 |
| Acute limb ischemia | 0 (0) | 0 (0) | N/A |
| Hazard Ratio [95% CI] | p-Value | ||
|---|---|---|---|
| IL-7 | MALEs | 1.56 [1.12–1.88] | 0.007 |
| Vascular intervention | 1.10 [1.05–2.98] | 0.019 | |
| Major amputation | 1.02 [1.01–1.88] | 0.042 | |
| TRAIL-R2 | MALEs | 1.00 [0.87–1.33] | 0.635 |
| Vascular intervention | 1.01 [0.99–1.43] | 0.884 | |
| Major amputation | 1.01 [0.98–4.32] | 0.932 | |
| MCP-1 | MALEs | 1.04 [0.68–1.59] | 0.277 |
| Vascular intervention | 1.11 [0.83–3.29] | 0.550 | |
| Major amputation | 1.00 [0.99–1.12] | 0.980 | |
| FGF-23 | MALEs | 1.06 [0.99–1.22] | 0.484 |
| Vascular intervention | 1.02 [0.91–1.31] | 0.832 | |
| Major amputation | 1.01 [0.90–3.22] | 0.742 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, B.; Shaikh, F.; Zamzam, A.; Syed, M.H.; Abdin, R.; Qadura, M. The Identification and Evaluation of Interleukin-7 as a Myokine Biomarker for Peripheral Artery Disease Prognosis. J. Clin. Med. 2024, 13, 3583. https://doi.org/10.3390/jcm13123583
Li B, Shaikh F, Zamzam A, Syed MH, Abdin R, Qadura M. The Identification and Evaluation of Interleukin-7 as a Myokine Biomarker for Peripheral Artery Disease Prognosis. Journal of Clinical Medicine. 2024; 13(12):3583. https://doi.org/10.3390/jcm13123583
Chicago/Turabian StyleLi, Ben, Farah Shaikh, Abdelrahman Zamzam, Muzammil H. Syed, Rawand Abdin, and Mohammad Qadura. 2024. "The Identification and Evaluation of Interleukin-7 as a Myokine Biomarker for Peripheral Artery Disease Prognosis" Journal of Clinical Medicine 13, no. 12: 3583. https://doi.org/10.3390/jcm13123583





