Abstract
Background: Discontinuation of radiotherapy is rarely discussed in the scientific literature. The goal of this study was, therefore, to estimate the frequency of and reasons for treatment discontinuations in patients receiving radiotherapy for brain metastases from solid tumors and to identify factors predicting said discontinuations. Methods: All patients treated for brain metastases from solid tumors between 2010 and 2020 at our institution were retrospectively reviewed. In addition to collecting relevant patient characteristics, the Recursive Partitioning Analysis (RPA) and disease-specific Graded Prognostic Assessment (GPA) groups for each patient were calculated to assess the performance of these scores in predicting treatment discontinuations. Results: Out of 468 patients who underwent cranial radiotherapy, 35 treatments (7.5%) were discontinued. The most frequent reason was clinical deterioration, which was documented in 26 (74.3%) of discontinued treatments. Patients whose radiotherapy was discontinued had, on average, more leptomeningeal disease (20.0% vs. 12.6%), worse ECOG performance status (mean ECOG performance status 1.86 vs. 1.39), and more uncontrolled extracranial metastases (85.3% vs. 70.8%). The frequencies of treatment discontinuation increased with worse prognosis and differed significantly across RPA groups (p = 0.037) but not across GPA groups (p = 0.612). Conclusions: Treatment discontinuation occurred in 7.5% of cases, mostly due to clinical deterioration. Poor performance status, as well as more advanced disease and, in turn, poor prognosis, were associated with higher discontinuation rates.
1. Introduction
Treatment discontinuation in radiation oncology is rarely discussed in the scientific literature. A potential reason could be that a common cause of treatment discontinuation is the clinical deterioration of the patient and that, therefore, presenting cases of treatment discontinuation from one’s own institution might be viewed as a failure to perform good patient selection.
However, good patient selection is difficult, especially when treating brain metastases, where the prognosis varies greatly for different primary tumors and patient characteristics [1]. In addition, the improvement of CNS-active systemic therapies has contributed to improved survival in some but not all patients, with sometimes exceptional responses in patients with initially poor performance status, further complicating the issue [2,3]. However, good patient selection is crucial, especially since not every patient will derive a meaningful benefit, even from completing a course of brain radiotherapy, as illustrated by the QUARTZ trial that found only a marginal difference in overall survival and quality-adjusted life-years (QALYs) for whole-brain radiotherapy plus optimal supportive care compared to optimal supportive care alone [4].
Increasing the amount of data on the topic could potentially allow for better patient selection in the future. We, therefore, conducted a retrospective review of patients who were treated with cranial radiotherapy for brain metastases from solid tumors at our department. Our hypothesis was that treatment discontinuations would occur more frequently in patients with worse prognosis, and the goal was, in turn, to identify characteristics frequently associated with treatment discontinuation.
2. Materials and Methods
We retrospectively reviewed all patients who were treated with cranial radiotherapy for brain metastases from solid tumors in our department from 01/2010 to 12/2020. Patients who only received prophylactic cranial radiotherapy, had primary brain tumors, or hematologic malignancies were excluded. If a patient did not complete the number of therapy sessions that were prescribed at the start of the treatment, this was considered a case of treatment discontinuation.
Data were collected on age, sex, Eastern Cooperative Oncology Group (ECOG) performance status, the primary tumor site, the number of brain metastases, as well as the presence of leptomeningeal disease, other organs with metastases, whether the primary tumor and/or the extracranial metastases were controlled, which radiotherapy technique was used, and if the patient was taking steroids at the time of radiotherapy initiation. In addition to collecting relevant patient characteristics such as collecting the reasons for treatment discontinuation, we also computed the Recursive Partitioning Analysis (RPA) and disease-specific Graded Prognostic Assessment (GPA) groups for each patient where all the required information was available [5,6]. Due to the cohort going back to 2010, we used the executive summary report from 2012 instead of newer versions that would have required molecular markers that were not available for the whole cohort.
Chi-square tests were used to test the frequencies of treatment discontinuations across the different RPA and GPA groups.
Data preprocessing, analysis, and visualization were performed with Python (version 3.9.7) using the numpy (version 1.20.3), pandas (version 1.3.4), scikit-learn (version 0.24.2), scipy (version 1.10.0), matplotlib (version 3.4.3), and seaborn (version 0.11.2) packages. The full dataset, notebook, and environment file have been uploaded to a public repository (https://github.com/windisch-paul/rt-treatment-discontinuation).
Institutional review board approval was obtained from the ethical review committee of the canton of Zurich for a project (project number: BASEC 2020-02112) to analyze the effects and side effects of radiotherapy at our institution (ClinicalTrials.gov Identifier: NCT05192876). Written informed consent for the analysis of anonymized clinical and imaging data was obtained from all patients, and all data were gathered in accordance with the World Medical Association Declaration of Helsinki: Research involving human subjects.
3. Results
The patient characteristics are presented in Table 1, and the distributions of selected patient characteristics are presented in Figure 1A. Out of 468 patients who underwent cranial radiotherapy, 35 treatments (7.5%) were discontinued. The most frequent reason for treatment discontinuation was clinical deterioration, which was documented in 26 (74.3%) discontinued treatments. One patient died, one patient underwent surgery for his brain metastases, and one patient discontinued his radiotherapy in order to start another systemic therapy. In the six remaining patients, no definitive reason was documented.

Table 1.
Patient characteristics. RT = Radiotherapy, IQR = Interquartile range, ECOG = Eastern Cooperative Oncology Group, NSCLC = Non-small-cell lung cancer, SCLC = Small-cell lung cancer.
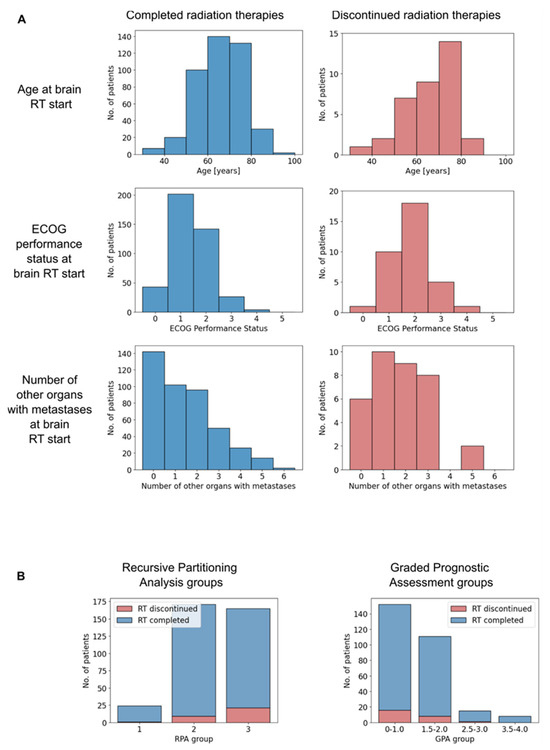
Figure 1.
(A) Histograms of selected patient characteristics depending on whether the radiotherapy was completed (left) or discontinued (right). (B) Histograms of completed and discontinued radiotherapies by Recursive Partitioning analysis (left) and Graded Prognostic Assessment group (right). RT = Radiotherapy, ECOG = Eastern Cooperative Oncology Group, RPA = Recursive Partitioning Analysis, GPA = Graded Prognostic Assessment.
Non-small-cell lung cancer accounted for the majority of primary tumors (n = 251), followed by breast (n = 67) and small-cell lung cancer (n = 50). This order was seen in both completed and discontinued treatments with a slightly higher share of breast cancer among discontinued treatments (13.6 vs. 22.9%, respectively).
Patients whose radiotherapy was discontinued had, on average, more leptomeningeal disease (20.0% vs. 12.6%), worse ECOG performance status (mean ECOG performance status 1.86 vs. 1.39), and more uncontrolled extracranial metastases (85.3% vs. 70.8%).
In addition, they were slightly older (median age 69 years vs. 66 years), more frequently diagnosed with three or more brain metastases (54.3% vs. 46.1%), more frequently under treatment with steroids (85.3% vs. 74.2%), and more frequently treated with whole-brain radiotherapy (84.7% vs. 71.8%) instead of stereotactic or partial-brain radiotherapy.
The distribution of RPA and GPA groups and the respective frequencies of treatment discontinuation are presented in Figure 1B. Most patients were classified into the RPA groups 2 and 3 (47.5% and 45.8%, respectively), which indicates an on-average poor prognosis of the patient collective. For the GPA, this was even more pronounced, with 64.0% of patients being classified in group 1, which is associated with the worst prognosis.
The frequencies of treatment discontinuation increased with worse prognosis and differed significantly across RPA groups (p = 0.037) but not across GPA groups (p = 0.612).
4. Discussion
Our analysis did not identify a singular factor that predicts the discontinuation of cranial radiotherapy for brain metastases from solid tumors. However, treatment discontinuations were more frequent in patients with generally poor performance status and more advanced or uncontrolled disease.
Due to the low number of treatment discontinuation events, we refrained from trying to build our own model to predict treatment discontinuation and instead attempted a validation of the performance of previously published prognostic models for the purpose of predicting treatment discontinuation.
As expected, we found an increase in rates of treatment discontinuation in the groups with worse prognosis for both the GPA and the RPA. This also fits in with clinical deterioration accounting for the majority of discontinued treatments. The fact that the frequency of treatment discontinuation across prognostic groups did not reach statistical significance for the GPA is likely due to the low number of discontinuation events combined with the higher number of classes compared to the RPA.
Searching PubMed for reports on radiotherapy discontinuation (query syntax: “((discontinuation[Title]) OR (stop[Title]) OR (termination[Title]) OR (abort[Title])) AND ((radiotherapy[Title]) OR (radiation[Title]))”) yielded 44 results, four of which were original articles discussing the permanent discontinuation of radiotherapy [7,8,9,10]. Lebwohl and colleagues analyzed treatment discontinuation during radiochemotherapy for rectal cancer and found a discontinuation rate of 5.3% [9]. Ramsey and colleagues found that 22% of Medicare-enrolled women did not complete their radiotherapy for non-metastatic breast cancer [10]. Puckett and colleagues analyzed 297 patients who received any kind of palliative radiotherapy and found that 60 (20.2%) did not complete their treatment. They also reported an association of worse performance status with increased discontinuation rates. Unsurprisingly, they also saw a correlation between treatment discontinuation and poor survival [8]. Lazarev and colleagues reported that 58 out of 1001 patients (5.7%) discontinued their curative radiotherapy for head and neck cancer due to a variety of different reasons, from patients’ decisions against medical advice (33%), over comorbidities (24%), toxicities (17%), social factors (17%) to disease progression (9%) [7]. The discrepancy between the reasons they found in a head and neck cohort compared to the reasons we identified in a brain metastases cohort suggests that reasons for treatment discontinuation and, in turn, factors predicting the risk of treatment discontinuation might vary greatly for different tumor sites and clinical scenarios. This adds to the complexity of the already difficult situation of counseling patients with brain metastases. While prognostic scores can and should be employed to support physicians with an objective assessment of the patient’s expected survival, they should not be the sole foundation for suggesting a plan to a patient as exceptional responses, both good and bad, occur. Therefore, clinical judgment, especially that of the patient’s willingness to continue treatment, is necessary to integrate prognostic scores into a sound management plan.
A question we could not answer is about the disease course of people in which a decision was made not to perform the treatment. Unfortunately, this information is usually not stored in a structured format and can happen in different situations, e.g., discussions with the patient outside of the radiation oncology institute, in the tumor board, etc., which makes it difficult to obtain comprehensive data.
The strengths of our article include the consecutive sampling and the publication of patient-level data so that interested researchers can replicate the results themselves or include them in future meta-analyses of the topic. The limitations of our article include the small number of treatment discontinuation events that prevented us from more sophisticated analyses or modeling. However, we instead validated existing prognostic models for the purpose of predicting treatment discontinuation. In addition, we did not capture additional sociodemographic data, e.g., on the care situation which could be interesting in the context of predicting discontinuations.
Another limitation is the fact that we did not use the most recent version of the GPA and that newer versions considering molecular alterations might exhibit a different performance for predicting treatment discontinuations.
5. Conclusions
Treatment discontinuation of palliative brain radiotherapy in patients with brain metastases occurred in 7.5% of cases, mostly due to clinical deterioration. Poor performance status, as well as more advanced disease and, in turn, poor prognosis, were associated with higher discontinuation rates.
Author Contributions
Conceptualization, P.W. and C.S.; methodology, P.W. and C.S.; formal analysis, P.W. and J.L.; data curation, P.W. and C.S.; writing—original draft preparation, P.W.; writing—review and editing, J.L., R.F., D.R.Z. and C.S.; supervision, R.F. and D.R.Z.; project administration, D.R.Z. All authors have read and agreed to the published version of the manuscript.
Funding
C.S. was supported by a personal grant from the “Filling the gap” program of the University of Zurich, Switzerland.
Institutional Review Board Statement
Institutional review board approval was obtained on 1 September 2020 from the ethical review committee of the canton of Zurich (Kantonale Ethikkommission) for a project (project number: BASEC 2020-02112) to analyze the effects and side effects of radiotherapy at our institution (ClinicalTrials.gov Identifier: NCT05192876, link: https://clinicaltrials.gov/study/NCT05192876).
Informed Consent Statement
Written informed consent for the analysis of anonymized clinical and imaging data was obtained from all patients, and all data were gathered in accordance with the World Medical Association Declaration of Helsinki: Research involving human subjects.
Data Availability Statement
All data and code used to obtain the results of this study have been uploaded to https://github.com/windisch-paul/rt-treatment-discontinuation.
Conflicts of Interest
P.W. has a patent application titled “Method for detection of neurological abnormalities” outside of the submitted work. The remaining authors declare no conflicts of interest.
References
- Lamba, N.; Wen, P.Y.; Aizer, A.A. Epidemiology of Brain Metastases and Leptomeningeal Disease. Neuro. Oncol. 2021, 23, 1447–1456. [Google Scholar] [CrossRef] [PubMed]
- Tawbi, H.A.; Forsyth, P.A.; Algazi, A.; Hamid, O.; Hodi, F.S.; Moschos, S.J.; Khushalani, N.I.; Lewis, K.; Lao, C.D.; Postow, M.A.; et al. Combined Nivolumab and Ipilimumab in Melanoma Metastatic to the Brain. N. Engl. J. Med. 2018, 379, 722–730. [Google Scholar] [CrossRef] [PubMed]
- Reungwetwattana, T.; Nakagawa, K.; Cho, B.C.; Cobo, M.; Cho, E.K.; Bertolini, A.; Bohnet, S.; Zhou, C.; Lee, K.H.; Nogami, N.; et al. CNS Response to Osimertinib Versus Standard Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Patients with Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2018, 36, JCO2018783118. [Google Scholar] [CrossRef] [PubMed]
- Mulvenna, P.; Nankivell, M.; Barton, R.; Faivre-Finn, C.; Wilson, P.; McColl, E.; Moore, B.; Brisbane, I.; Ardron, D.; Holt, T.; et al. Dexamethasone and Supportive Care with or without Whole Brain Radiotherapy in Treating Patients with Non-Small Cell Lung Cancer with Brain Metastases Unsuitable for Resection or Stereotactic Radiotherapy (QUARTZ): Results from a Phase 3, Non-Inferiority, Randomised Trial. Lancet 2016, 388, 2004–2014. [Google Scholar] [PubMed]
- Sperduto, P.W.; Kased, N.; Roberge, D.; Xu, Z.; Shanley, R.; Luo, X.; Sneed, P.K.; Chao, S.T.; Weil, R.J.; Suh, J.; et al. Summary Report on the Graded Prognostic Assessment: An Accurate and Facile Diagnosis-Specific Tool to Estimate Survival for Patients with Brain Metastases. J. Clin. Oncol. 2012, 30, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, L.; Scott, C.; Rotman, M.; Asbell, S.; Phillips, T.; Wasserman, T.; McKenna, W.G.; Byhardt, R. Recursive Partitioning Analysis (RPA) of Prognostic Factors in Three Radiation Therapy Oncology Group (RTOG) Brain Metastases Trials. Int. J. Radiat. Oncol. Biol. Phys. 1997, 37, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Lazarev, S.; Gupta, V.; Ghiassi-Nejad, Z.; Miles, B.; Scarborough, B.; Misiukiewicz, K.J.; Reckson, B.; Sheu, R.-D.; Bakst, R.L. Premature Discontinuation of Curative Radiation Therapy: Insights from Head and Neck Irradiation. Adv. Radiat. Oncol. 2018, 3, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Puckett, L.L.; Luitweiler, E.; Potters, L.; Teckie, S. Preventing Discontinuation of Radiation Therapy: Predictive Factors to Improve Patient Selection for Palliative Treatment. J. Oncol. Pract. 2017, 13, e782–e791. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, B.; Ballas, L.; Cao, Y.; Chan, G.; Grossman, R.; Sherr, D.L.; Woodhouse, S.; Neugut, A.I. Treatment Interruption and Discontinuation in Radiotherapy for Rectal Cancer. Cancer Investig. 2010, 28, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Ramsey, S.D.; Zeliadt, S.B.; Richardson, L.C.; Pollack, L.A.; Linden, H.; Blough, D.K.; Cheteri, M.K.; Tock, L.; Nagy, K.; Anderson, N. Discontinuation of Radiation Treatment among Medicaid-Enrolled Women with Local and Regional Stage Breast Cancer. Breast J. 2010, 16, 20–27. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).