Prognostic Role of OX40, LAG-3, TIM-3 and PD-L1 Expression in Bone and Soft Tissue Sarcomas
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Pathological Evaluation
2.2.1. PD-L1 Assessment
2.2.2. TIM-3 and LAG-3 Evaluation
2.2.3. OX40 Assessment
2.3. Statistical Analysis
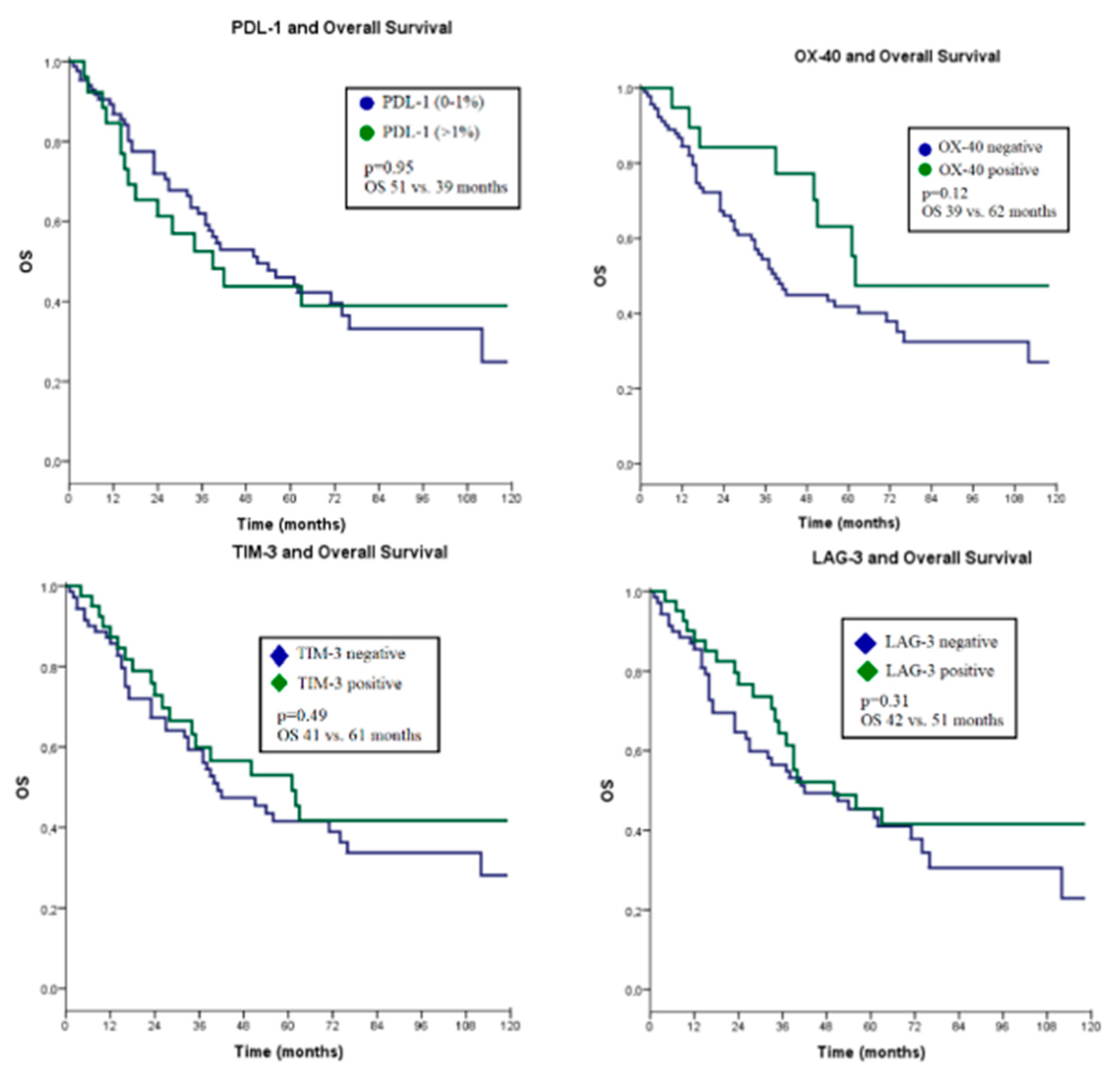
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nixon, N.; Blais, N.; Ernst, S.; Kollmannsberger, C.; Bebb, G.; Butler, M.; Smylie, M.; Verma, S. Current landscape of immunotherapy in the treatment of solid tumours, with future opportunities and challenges. Curr. Oncol. 2018, 25, 373–384. [Google Scholar] [CrossRef]
- Tawbi, H.A.; Burgess, M.; Bolejack, V.; Van Tine, B.A.; Schuetze, S.M.; Hu, J.; D’Angelo, S.; Attia, S.; Riedel, R.F.; Priebat, D.A. Pembrolizumab in advanced soft-tissue sarcoma and bone sarcoma (SARC028): A multicentre, two-cohort, single-arm, open-label, phase 2 trial. Lancet Oncol. 2017, 18, 1493–1501. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Ning, Q.; Yang, L.; Mo, Z.; Tang, S. Mechanisms of immune escape in the cancer immune cycle. Int. Immunopharmacol. 2020, 86, 106700. [Google Scholar] [CrossRef] [PubMed]
- Constantinidou, A.; Alifieris, C.; Trafalis, D.T. Targeting programmed cell death-1 (PD-1) and ligand (PD-L1): A new era in cancer active immunotherapy. Pharmacol. Ther. 2019, 194, 84–106. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; You, W.; Wan, P.; Jiang, X.; Chen, J.; Zheng, Y.; Li, W.; Tan, J.; Zhang, S. Clinicopathological and prognostic significance of PD-L1 expression in sarcoma: A systematic review and meta-analysis. Medicine 2018, 97, e11004. [Google Scholar] [CrossRef]
- Toulmonde, M.; Penel, N.; Adam, J.; Chevreau, C.; Blay, J.-Y.; Le Cesne, A.; Bompas, E.; Piperno-Neumann, S.; Cousin, S.; Grellety, T. Use of PD-1 targeting, macrophage infiltration, and IDO pathway activation in sarcomas: A phase 2 clinical trial. JAMA Oncol. 2018, 4, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Pollack, S.M.; Redman, M.W.; Baker, K.K.; Wagner, M.J.; Schroeder, B.A.; Loggers, E.T.; Trieselmann, K.; Copeland, V.C.; Zhang, S.; Black, G. Assessment of Doxorubicin and Pembrolizumab in Patients with Advanced Anthracycline-Naive Sarcoma: A Phase 1/2 Nonrandomized Clinical Trial. JAMA Oncol. 2020, 6, 1778–1782. [Google Scholar] [CrossRef]
- D’Angelo, S.P.; Mahoney, M.R.; Van Tine, B.A.; Atkins, J.; Milhem, M.M.; Jahagirdar, B.N.; Antonescu, C.R.; Horvath, E.; Tap, W.D.; Schwartz, G.K. Nivolumab with or without ipilimumab treatment for metastatic sarcoma (Alliance A091401): Two open-label, non-comparative, randomised, phase 2 trials. Lancet Oncol. 2018, 19, 416–426. [Google Scholar] [CrossRef] [PubMed]
- Asano, Y.; Kashiwagi, S.; Takada, K.; Ishihara, S.; Goto, W.; Morisaki, T.; Shibutani, M.; Tanaka, H.; Hirakawa, K.; Ohira, M. Clinical Significance of Expression of Immunoadjuvant Molecules (LAG-3, TIM-3, OX-40) in Neoadjuvant Chemotherapy for Breast Cancer. Anticancer Res. 2022, 42, 125–136. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, P.; Wang, H.; Wu, S.; Zhao, S.; He, Y.; Zhou, C.; Hirsch, F.R. The landscape of immune checkpoints expression in non-small cell lung cancer: A narrative review. Transl. Lung Cancer Res. 2021, 10, 1029. [Google Scholar] [CrossRef]
- Weinberg, A.D.; Rivera, M.-M.; Prell, R.; Morris, A.; Ramstad, T.; Vetto, J.T.; Urba, W.J.; Alvord, G.; Bunce, C.; Shields, J. Engagement of the OX-40 receptor in vivo enhances antitumor immunity. J. Immunol. 2000, 164, 2160–2169. [Google Scholar] [CrossRef] [PubMed]
- Melake, M.; Smith, H.; Mansfield, D.; Davies, E.; Dillon, M.; Wilkins, A.; Patin, E.; Pedersen, M.; Buus, R.; Melcher, A. OX40 and 4-1BB delineate distinct immune profiles in sarcoma. Oncoimmunology 2022, 11, 2066050. [Google Scholar] [CrossRef] [PubMed]
- Pardee, A.D.; McCurry, D.; Alber, S.; Hu, P.; Epstein, A.L.; Storkus, W.J. A therapeutic OX40 agonist dynamically alters dendritic, endothelial, and T cell subsets within the established tumor microenvironment. Cancer Res. 2010, 70, 9041–9052. [Google Scholar] [CrossRef] [PubMed]
- Reuter, D.; Staege, M.S.; Kühnöl, C.D.; Föll, J. Immunostimulation by OX40 ligand transgenic Ewing sarcoma cells. Front. Oncol. 2015, 5, 242. [Google Scholar] [CrossRef] [PubMed]
- Huard, B.; Prigent, P.; Tournier, M.; Bruniquel, D.; Triebel, F. CD4/major histocompatibility complex class II interaction analyzed with CD4-and lymphocyte activation gene-3 (LAG-3)-Ig fusion proteins. Eur. J. Immunol. 1995, 25, 2718–2721. [Google Scholar] [CrossRef] [PubMed]
- Shen, P.; Yue, R.; Tang, J.; Si, H.; Shen, L.; Guo, C.; Zhang, L.; Han, H.; Song, H.K.; Zhao, P. Preferential Tim-3 expression on treg and CD8+ T cells, supported by tumor-associated macrophages, is associated with worse prognosis in gastric cancer. Am. J. Transl. Res. 2016, 8, 3419. [Google Scholar]
- Dancsok, A.R.; Setsu, N.; Gao, D.; Blay, J.-Y.; Thomas, D.; Maki, R.G.; Nielsen, T.O.; Demicco, E.G. Expression of lymphocyte immunoregulatory biomarkers in bone and soft-tissue sarcomas. Mod. Pathol. 2019, 32, 1772–1785. [Google Scholar] [CrossRef] [PubMed]
- Burugu, S.; Dancsok, A.R.; Nielsen, T.O. Emerging targets in cancer immunotherapy. In Seminars in Cancer Biology; Elsevier: Amsterdam, The Netherlands, 2018; pp. 39–52. [Google Scholar]
- Ngiow, S.F.; Von Scheidt, B.; Akiba, H.; Yagita, H.; Teng, M.W.; Smyth, M.J. Anti-TIM3 Antibody Promotes T Cell IFN-γ–Mediated Antitumor Immunity and Suppresses Established TumorsMechanism of Anti-TIM3. Cancer Res. 2011, 71, 3540–3551. [Google Scholar] [CrossRef] [PubMed]
- Ceruso, M.S.; Albert, S.; Italiano, A.; Toulmonde, M.; Cousin, S.; Grellety, T.; Blay, J.; Verret, B.; Auzanneau, C.; Valade, V. 1527TiP CONGRATS-combination of nivolumab plus relatlimab in patients with advanced or metastatic soft-tissue sarcoma: A proof-of-concept randomized phase II study. Ann. Oncol. 2022, 33, S1243. [Google Scholar]
- Tang, F.; Tie, Y.; Wei, Y.-Q.; Tu, C.-Q.; Wei, X.-W. Targeted and immuno-based therapies in sarcoma: Mechanisms and advances in clinical trials. Biochim. Biophys. Acta (BBA)-Rev. Cancer 2021, 1876, 188606. [Google Scholar] [CrossRef]
- Tu, Q.; Hu, C.; Zhang, H.; Kong, M.; Peng, C.; Song, M.; Zhao, C.; Wang, Y.; Ma, X. Development and Validation of Novel Nomograms for Predicting Specific Distant Metastatic Sites and Overall Survival of Patients with Soft Tissue Sarcoma. Technol. Cancer Res. Treat. 2021, 20, 1533033821997828. [Google Scholar] [CrossRef] [PubMed]
- Van Glabbeke, M.; Van Oosterom, A.; Oosterhuis, J.; Mouridsen, H.; Crowther, D.; Somers, R.; Verweij, J.; Santoro, A.; Buesa, J.; Tursz, T. Prognostic factors for the outcome of chemotherapy in advanced soft tissue sarcoma: An analysis of 2,185 patients treated with anthracycline-containing first-line regimens-a European Organization for Research and Treatment of Cancer Soft Tissue and Bone Sarcoma Group Study. J. Clin. Oncol. 1999, 17, 150–157. [Google Scholar] [PubMed]
- Tap, W.D.; Wagner, A.J.; Schöffski, P.; Martin-Broto, J.; Krarup-Hansen, A.; Ganjoo, K.N.; Yen, C.-C.; Razak, A.R.A.; Spira, A.; Kawai, A. Effect of doxorubicin plus olaratumab vs doxorubicin plus placebo on survival in patients with advanced soft tissue sarcomas: The ANNOUNCE randomized clinical trial. Jama 2020, 323, 1266–1276. [Google Scholar] [CrossRef] [PubMed]
- Seddon, B.; Strauss, S.J.; Whelan, J.; Leahy, M.; Woll, P.J.; Cowie, F.; Rothermundt, C.; Wood, Z.; Benson, C.; Ali, N. Gemcitabine and docetaxel versus doxorubicin as first-line treatment in previously untreated advanced unresectable or metastatic soft-tissue sarcomas (GeDDiS): A randomised controlled phase 3 trial. Lancet Oncol. 2017, 18, 1397–1410. [Google Scholar] [CrossRef] [PubMed]
- Heymann, M.F.; Schiavone, K.; Heymann, D. Bone sarcomas in the immunotherapy era. Br. J. Pharmacol. 2021, 178, 1955–1972. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Kim, E.K.; Jung, H.; Chon, H.J.; Han, J.W.; Shin, K.-H.; Hu, H.; Kim, K.S.; Choi, Y.D.; Kim, S. Prognostic implications of PD-L1 expression in patients with soft tissue sarcoma. BMC Cancer 2016, 16, 434. [Google Scholar] [CrossRef] [PubMed]
- Bertucci, F.; Finetti, P.; Perrot, D.; Leroux, A.; Collin, F.; Le Cesne, A.; Coindre, J.-M.; Blay, J.-Y.; Birnbaum, D.; Mamessier, E. PDL1 expression is a poor-prognosis factor in soft-tissue sarcomas. Oncoimmunology 2017, 6, e1278100. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.R.; Moon, Y.J.; Kwon, K.S.; Bae, J.S.; Wagle, S.; Kim, K.M.; Park, H.S.; Lee, H.; Moon, W.S.; Chung, M.J. Tumor infiltrating PD1-positive lymphocytes and the expression of PD-L1 predict poor prognosis of soft tissue sarcomas. PLoS ONE 2013, 8, e82870. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, S.P.; Shoushtari, A.N.; Agaram, N.P.; Kuk, D.; Qin, L.-X.; Carvajal, R.D.; Dickson, M.A.; Gounder, M.; Keohan, M.L.; Schwartz, G.K. Prevalence of tumor-infiltrating lymphocytes and PD-L1 expression in the soft tissue sarcoma microenvironment. Hum. Pathol. 2015, 46, 357–365. [Google Scholar] [CrossRef]
- Peng, L.; Qin, B.-D.; Xiao, K.; Xu, S.; Yang, J.-S.; Zang, Y.-S.; Stebbing, J.; Xie, L.-P. A meta-analysis comparing responses of Asian versus non-Asian cancer patients to PD-1 and PD-L1 inhibitor-based therapy. Oncoimmunology 2020, 9, 1781333. [Google Scholar] [CrossRef]
- Ayers, K.L.; Mullaney, T.; Zhou, X.; Liu, J.J.; Lee, K.; Ma, M.; Jones, S.; Li, L.; Redfern, A.; Jappe, W. Analysis of real-world data to investigate the impact of race and ethnicity on response to programmed cell death-1 and programmed cell death-ligand 1 inhibitors in advanced non-small cell lung cancers. Oncologist 2021, 26, e1226–e1239. [Google Scholar] [CrossRef] [PubMed]
- Pollack, S.M.; He, Q.; Yearley, J.H.; Emerson, R.; Vignali, M.; Zhang, Y.; Redman, M.W.; Baker, K.K.; Cooper, S.; Donahue, B. T-cell infiltration and clonality correlate with programmed cell death protein 1 and programmed death-ligand 1 expression in patients with soft tissue sarcomas. Cancer 2017, 123, 3291–3304. [Google Scholar] [CrossRef]
- Que, Y.; Fang, Z.; Guan, Y.; Xiao, W.; Xu, B.; Zhao, J.; Chen, H.; Zhang, X.; Zeng, M.; Liang, Y. LAG-3 expression on tumor-infiltrating T cells in soft tissue sarcoma correlates with poor survival. Cancer Biol. Med. 2019, 16, 331. [Google Scholar]
- Petty, J.K.; He, K.; Corless, C.L.; Vetto, J.T.; Weinberg, A.D. Survival in human colorectal cancer correlates with expression of the T-cell costimulatory molecule OX-40 (CD134). Am. J. Surg. 2002, 183, 512–518. [Google Scholar] [CrossRef] [PubMed]
- Massarelli, E.; Lam, V.K.; Parra, E.R.; Rodriguez-Canales, J.; Behrens, C.; Diao, L.; Wang, J.; Blando, J.; Byers, L.A.; Yanamandra, N. High OX-40 expression in the tumor immune infiltrate is a favorable prognostic factor of overall survival in non-small cell lung cancer. J. Immunother. Cancer 2019, 7, 351. [Google Scholar] [CrossRef] [PubMed]
- Ozaniak, A.; Vachtenheim, J., Jr.; Lischke, R.; Bartunkova, J.; Strizova, Z. Novel Insights into the Immunotherapy of Soft Tissue Sarcomas: Do We Need a Change of Perspective? Biomedicines 2021, 9, 935. [Google Scholar] [CrossRef]
- Woo, S.-R.; Turnis, M.E.; Goldberg, M.V.; Bankoti, J.; Selby, M.; Nirschl, C.J.; Bettini, M.L.; Gravano, D.M.; Vogel, P.; Liu, C.L. Immune Inhibitory Molecules LAG-3 and PD-1 Synergistically Regulate T-cell Function to Promote Tumoral Immune EscapeLAG-3 and PD-1 Synergistically Prevent Antitumor Immunity. Cancer Res. 2012, 72, 917–927. [Google Scholar] [CrossRef]
- Yu, X.; Huang, X.; Chen, X.; Liu, J.; Wu, C.; Pu, Q.; Wang, Y.; Kang, X.; Zhou, L. Characterization of a novel anti-human lymphocyte activation gene 3 (LAG-3) antibody for cancer immunotherapy. In Mabs; Taylor & Francis: Abingdon, UK, 2019; pp. 1139–1148. [Google Scholar]
- Shayan, G.; Srivastava, R.; Li, J.; Schmitt, N.; Kane, L.P.; Ferris, R.L. Adaptive resistance to anti-PD1 therapy by Tim-3 upregulation is mediated by the PI3K-Akt pathway in head and neck cancer. Oncoimmunology 2017, 6, e1261779. [Google Scholar] [CrossRef] [PubMed]
- Leslie, M. High TMB predicts immunotherapy benefit. Cancer Discov. 2018, 8, 668. [Google Scholar]
- Hellmann, M.D.; Callahan, M.K.; Awad, M.M.; Calvo, E.; Ascierto, P.A.; Atmaca, A.; Rizvi, N.A.; Hirsch, F.R.; Selvaggi, G.; Szustakowski, J.D. Tumor mutational burden and efficacy of nivolumab monotherapy and in combination with ipilimumab in small-cell lung cancer. Cancer Cell 2018, 33, 853–861.e854. [Google Scholar] [CrossRef]
- Hellmann, M.D.; Ciuleanu, T.-E.; Pluzanski, A.; Lee, J.S.; Otterson, G.A.; Audigier-Valette, C.; Minenza, E.; Linardou, H.; Burgers, S.; Salman, P. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N. Engl. J. Med. 2018, 378, 2093–2104. [Google Scholar] [CrossRef] [PubMed]
- Siozopoulou, V.; Domen, A.; Zwaenepoel, K.; Van Beeck, A.; Smits, E.; Pauwels, P.; Marcq, E. Immune Checkpoint Inhibitory Therapy in Sarcomas: Is There Light at the End of the Tunnel? Cancers 2021, 13, 360. [Google Scholar] [CrossRef] [PubMed]
- Dufresne, A.; Meurgey, A.; Brahmi, M. Immunotherapy of heterogenous sarcomas: Questions and strategies. Curr. Opin. Oncol. 2019, 31, 304–309. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total (n = 111) No. Patients % | |
|---|---|---|
| Age | ||
| ≤60 | 84 | 76 |
| >60 | 27 | 24 |
| Gender | ||
| Male | 66 | 59.5 |
| Female | 45 | 40.5 |
| Histology | ||
| Soft tissue sarcoma | 68 | 61.3 |
| Bone sarcoma | 43 | 38.7 |
| Stage | ||
| Local | 100 | 90.1 |
| Metastatic | 11 | 9.9 |
| Tumor site | ||
| Head and neck | 13 | 11.7 |
| Chest | 12 | 10.8 |
| Abdomen | 32 | 28.8 |
| Limb | 54 | 48.6 |
| Tumor size | ||
| ≤5 cm | 35 | 31.5 |
| >5 cm | 76 | 68.5 |
| Grade | ||
| Low–intermediate | 23 | 20.7 |
| High | 88 | 79.3 |
| Median overall survival | Months (IQR) | |
| Whole group | 35 (15–63) | |
| Metastatic disease group | 10 (4–17) | |
| Types | Frequency | Percent |
|---|---|---|
| Leiomyosarcoma | 18 | 16.2 |
| Liposarcoma | 12 | 10.8 |
| Rhabdomyosarcoma | 8 | 7.2 |
| Osteosarcoma | 35 | 31.5 |
| Chondrosarcoma | 8 | 7.2 |
| Synovial sarcoma | 7 | 6.3 |
| Undifferentiated pleomorphic sarcoma | 9 | 8.1 |
| Others | 14 | 12.6 |
| Total | 111 | 100.0 |
| OX40 (Positive%) | TİM-3 (Positive%) | LAG-3 (Positive%) | PD-L1 (>1%) | |
|---|---|---|---|---|
| Leiomyosarcoma | 22.2% | 38.8% | 44.4% | 16.6% |
| Liposarcoma | 41.6% | 41.6% | 25% | 0% |
| Rhabdomyosarcoma | 50% | 75% | 50% | 37.5% |
| Osteosarcoma | 0% | 20% | 25.7% | 20% |
| Chondrosarcoma | 12.5% | 12.5% | 37.5% | 25% |
| Synovial sarcoma | 14.3% | 14.3% | 14.3% | 14.3% |
| Undifferentiated pleomorphic sarcoma | 33.3% | 55.5% | 66.6% | 33.3% |
| Total | 18% | 36% | 36.9% | 76.6% |
| Variable | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age | 0.92 | 0.50–1.67 | 0.79 | |||
| ≤60 years old | ||||||
| >60 years old | ||||||
| Gender | 0.74 | 0.44–1.26 | 0.27 | |||
| Male | ||||||
| Female | ||||||
| Histology | 1.35 | 0.80–2.28 | 0.25 | |||
| Soft tissue sarcoma | ||||||
| Bone sarcoma | ||||||
| Stage at diagnosis | 4.7 | 2.3–9.4 | <0.001 * | 7.40 | 3.46–15.8 | <0.001 * |
| Local | ||||||
| Metastatic | ||||||
| Tumor site | 1.15 | 0.85–1.56 | 0.36 | |||
| Head and neck | ||||||
| Chest | ||||||
| Abdomen | ||||||
| Limb | ||||||
| Tumor size | 0.83 | 0.50–1.41 | 0.50 | |||
| ≤5 cm | ||||||
| >5 cm | ||||||
| Grade | 1.81 | 1.19–2.77 | 0.001 * | 4.3 | 1.34–3.25 | 0.001 * |
| Low–intermediate | ||||||
| High | ||||||
| Pathological staining | 1.01 | 0.56–1.83 | 0.95 | 0.70 | 0.34–1.46 | 0.34 |
| PDL-1 | ||||||
| 0–1% | ||||||
| <1% | ||||||
| OX40 | 0.56 | 0.26–1.18 | 0.10 | 0.33 | 0.14–0.76 | 0.009 * |
| Negative | ||||||
| Positive | ||||||
| LAG-3 | 0.76 | 0.44–1.30 | 0.31 | 0.71 | 0.36–1.40 | 0.32 |
| Negative | ||||||
| Positive | ||||||
| TİM-3 | 0.83 | 0.48–1.42 | 0.49 | 1.81 | 0.94–3.44 | 0.074 |
| Negative | ||||||
| Positive | ||||||
| PDL-1 (%) | p Value | ||
|---|---|---|---|
| 0–1% | >1% | ||
| OX40 | |||
| Negative n (%) | 72 (84.7%) | 19 (73.1%) | |
| Positive n (%) | 13 (15.3%) | 7 (26.9%) | 0.17 |
| TIM-3 | |||
| Negative n (%) | 61 (71.8%) | 10 (38.5%) | |
| Positive n (%) | 24 (28.2%) | 16 (61.5%) | 0.002 * |
| LAG-3 | |||
| Negative n (%) | 63 (74.1%) | 7 (26.9%) | |
| Positive n (%) | 22 (25.9%) | 19 (73.1%) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurt İnci, B.; Acar, E.; Gürler, F.; İlhan, A.; Yıldız, F.; Ardıç, F.; Öksüzoğlu, B.; Özdemir, N.; Özet, A.; Esendağlı, G.; et al. Prognostic Role of OX40, LAG-3, TIM-3 and PD-L1 Expression in Bone and Soft Tissue Sarcomas. J. Clin. Med. 2024, 13, 3620. https://doi.org/10.3390/jcm13123620
Kurt İnci B, Acar E, Gürler F, İlhan A, Yıldız F, Ardıç F, Öksüzoğlu B, Özdemir N, Özet A, Esendağlı G, et al. Prognostic Role of OX40, LAG-3, TIM-3 and PD-L1 Expression in Bone and Soft Tissue Sarcomas. Journal of Clinical Medicine. 2024; 13(12):3620. https://doi.org/10.3390/jcm13123620
Chicago/Turabian StyleKurt İnci, Bediz, Elif Acar, Fatih Gürler, Ayşegül İlhan, Fatih Yıldız, Fisun Ardıç, Berna Öksüzoğlu, Nuriye Özdemir, Ahmet Özet, Güldal Esendağlı, and et al. 2024. "Prognostic Role of OX40, LAG-3, TIM-3 and PD-L1 Expression in Bone and Soft Tissue Sarcomas" Journal of Clinical Medicine 13, no. 12: 3620. https://doi.org/10.3390/jcm13123620





