Endodontic Treatment Outcomes in Cone Beam Computed Tomography Images—Assessment of the Diagnostic Accuracy of AI
Abstract
:1. Introduction
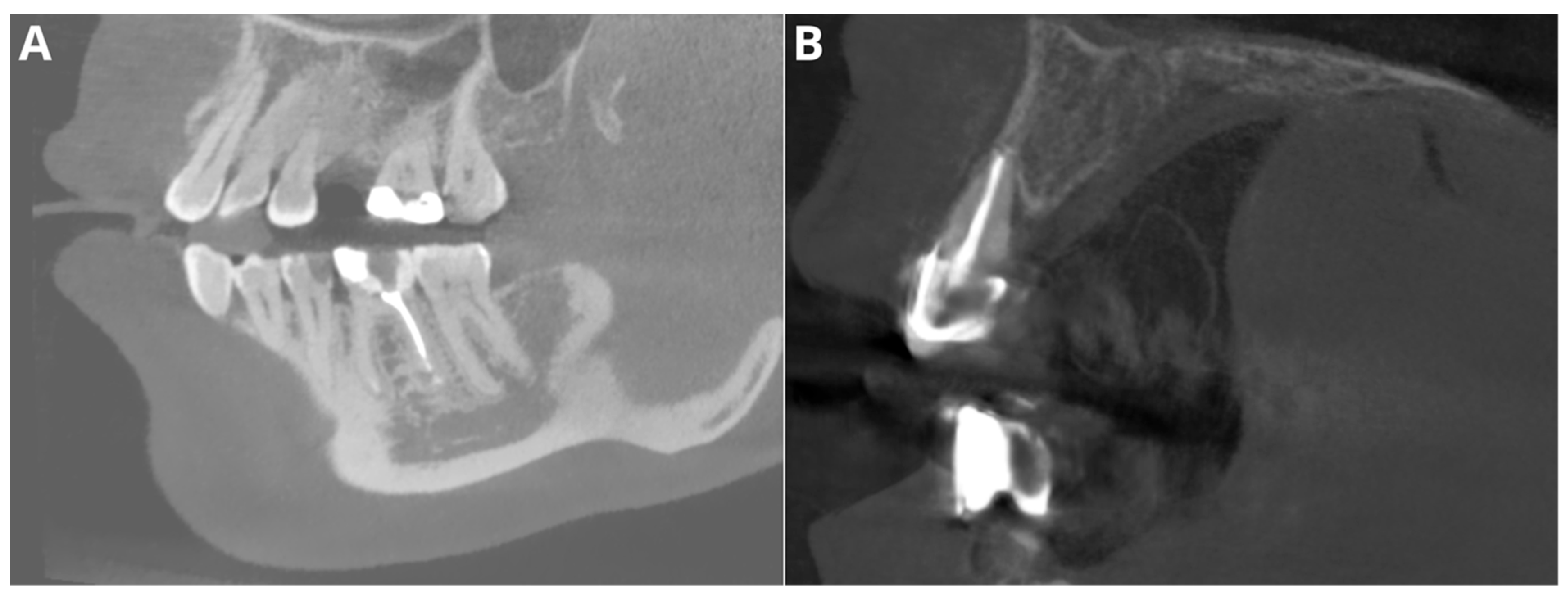
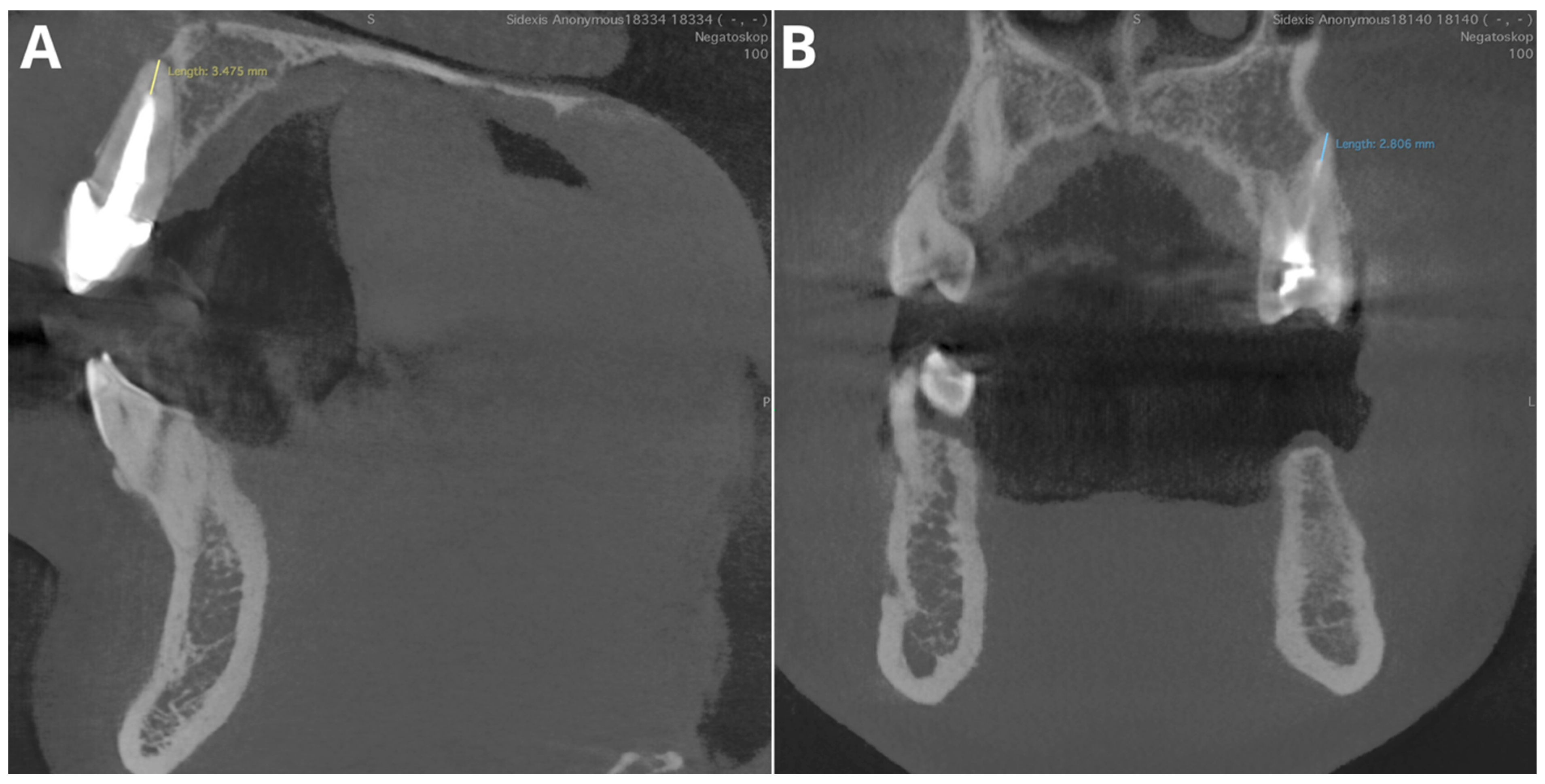
2. Materials and Methods
2.1. Patients
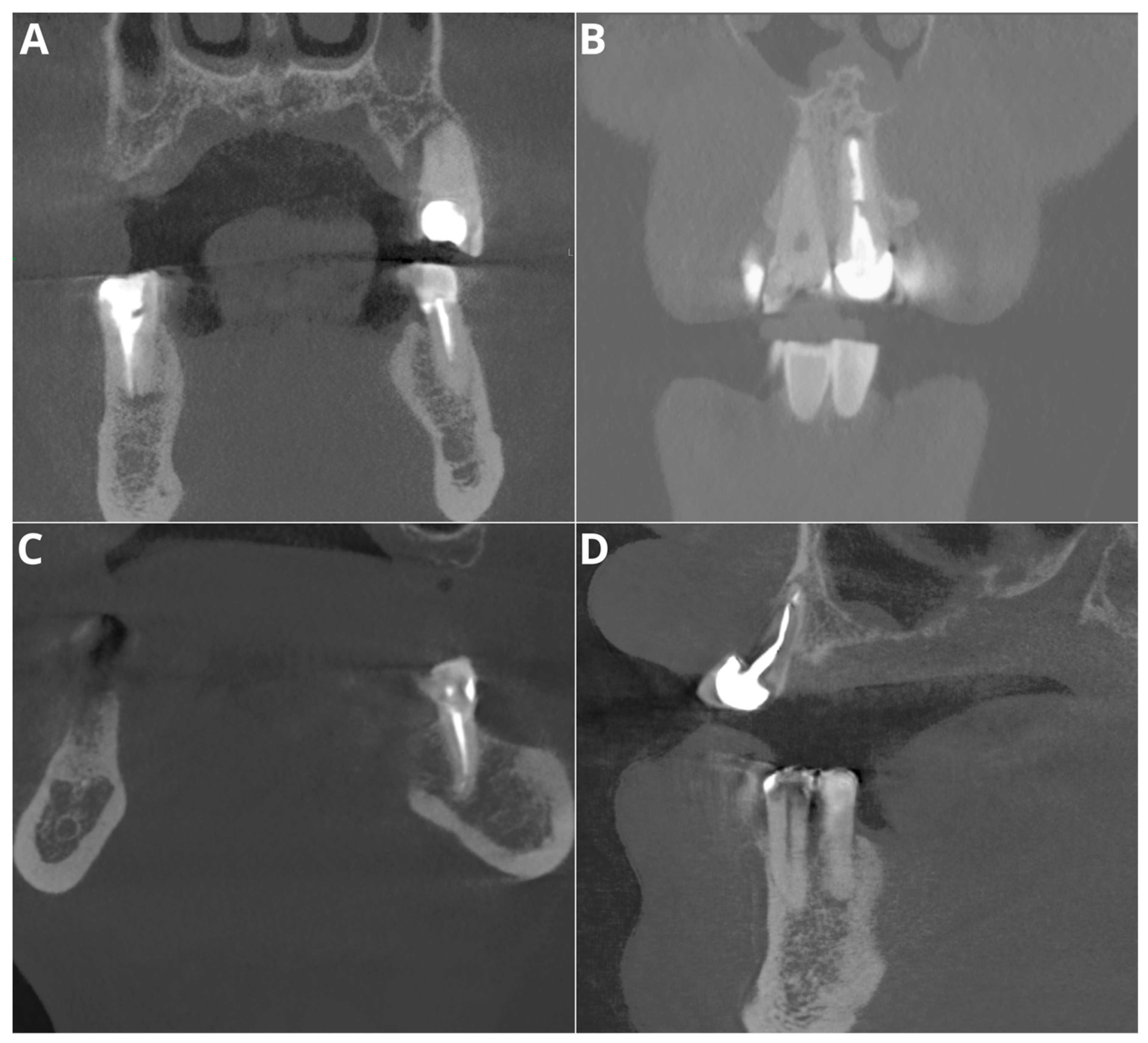
2.2. Image Acquisition and Postprocessing
2.3. AI Evaluation
- Probability of filling
- Adequate obturation
- Adequate density
- Overfilling
- Voids in filling
- Short filling
- Root canal number
2.4. Human Reader Evaluation
- Probability of filling—evaluation of the presence of radiopaque material within the tooth canals.
- Adequate obturation—assessment of the extent of the filling material up to the apex of the root, verification of material density and consistency through the canal.
- Adequate density—evaluation of the radiopacity and homogeneity of the filling material and identification of areas with lower density indicating voids or inadequate filling.
- Overfilling—examination of any filling material extending beyond the apex of the tooth.
- Voids in filling—identification of radiolucent areas within the filling that indicate the presence of voids.
- Short filling—assessment of the extent of the filling material if it falls short of the tooth apex.
2.5. Statistical Evaluation
3. Results
3.1. Patients
3.2. Diagnostic Accuracy Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fleming, C.H.; Litaker, M.S.; Alley, L.W.; Eleazer, P.D. Comparison of Classic Endodontic Techniques versus Contemporary Techniques on Endodontic Treatment Success. J. Endod. 2010, 36, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Van Nieuwenhuysen, J.-P.; Aouar, M.; D’hoore, W. Retreatment or Radiographic Monitoring in Endodontics. Int. Endod. J. 1994, 27, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Fernández, R.; Cadavid, D.; Zapata, S.M.; Álvarez, L.G.; Restrepo, F.A. Impact of Three Radiographic Methods in the Outcome of Nonsurgical Endodontic Treatment: A Five-Year Follow-Up. J. Endod. 2013, 39, 1097–1103. [Google Scholar] [CrossRef] [PubMed]
- Setzer, F.C.; Lee, S.-M. Radiology in Endodontics. Dent. Clin. N. Am. 2021, 65, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Petersson, A.; Axelsson, S.; Davidson, T.; Frisk, F.; Hakeberg, M.; Kvist, T.; Norlund, A.; Mejàre, I.; Portenier, I.; Sandberg, H.; et al. Radiological Diagnosis of Periapical Bone Tissue Lesions in Endodontics: A Systematic Review. Int. Endod. J. 2012, 45, 783–801. [Google Scholar] [CrossRef] [PubMed]
- Nur, M.; Kayipmaz, S.; Bayram, M.; Celikoglu, M.; Kilkis, D.; Sezgin, O.S. Conventional Frontal Radiographs Compared with Frontal Radiographs Obtained from Cone Beam Computed Tomography. Angle Orthod. 2012, 82, 579–584. [Google Scholar] [CrossRef]
- Olmez, H.; Gorgulu, S.; Akin, E.; Bengi, A.O.; Tekdemir, I.; Ors, F. Measurement Accuracy of a Computer-Assisted Three-Dimensional Analysis and a Conventional Two-Dimensional Method. Angle Orthod. 2011, 81, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Park, C.S.; Park, J.K.; Kim, H.; Han, S.S.; Jeong, H.G.; Park, H. Comparison of Conventional Lateral Cephalograms with Corresponding CBCT Radiographs. Imaging Sci. Dent. 2012, 42, 201–205. [Google Scholar] [CrossRef]
- Kaasalainen, T.; Ekholm, M.; Siiskonen, T.; Kortesniemi, M. Dental Cone Beam CT: An Updated Review. Phys. Medica 2021, 88, 193–217. [Google Scholar] [CrossRef] [PubMed]
- Wikner, J.; Hanken, H.; Eulenburg, C.; Heiland, M.; Gröbe, A.; Assaf, A.T.; Riecke, B.; Friedrich, R.E. Linear Accuracy and Reliability of Volume Data Sets Acquired by Two CBCT-Devices and an MSCT Using Virtual Models: A Comparative in-Vitro Study. Acta Odontol. Scand. 2016, 74, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Heo, M.-S.; Kim, J.-E.; Hwang, J.-J.; Han, S.-S.; Kim, J.-S.; Yi, W.-J.; Park, I.-W. Artificial Intelligence in Oral and Maxillofacial Radiology: What Is Currently Possible? Dentomaxillofacial Radiol. 2021, 50, 20200375. [Google Scholar] [CrossRef] [PubMed]
- Karobari, M.I.; Adil, A.H.; Basheer, S.N.; Murugesan, S.; Savadamoorthi, K.S.; Mustafa, M.; Abdulwahed, A.; Almokhatieb, A.A. Evaluation of the Diagnostic and Prognostic Accuracy of Artificial Intelligence in Endodontic Dentistry: A Comprehensive Review of Literature. Comput. Math. Methods Med. 2023, 2023, 7049360. [Google Scholar] [CrossRef] [PubMed]
- Ramezanzade, S.; Laurentiu, T.; Bakhshandah, A.; Ibragimov, B.; Kvist, T.; Bjørndal, L.; Bjørndal, L.; Dawson, V.S.; Fransson, H.; Frisk, F.; et al. The Efficiency of Artificial Intelligence Methods for Finding Radiographic Features in Different Endodontic Treatments—A Systematic Review. Acta Odontol. Scand. 2023, 81, 422–435. [Google Scholar] [PubMed]
- Jihed, M.; Dallel, I.; Tobji, S.; Amor, A. Ben The Impact of Artificial Intelligence on Contemporary Orthodontic Treatment Planning—A Systematic Review and Meta-Analysis. Sch. J. Dent. Sci. 2022, 9, 70–87. [Google Scholar] [CrossRef]
- Aminoshariae, A.; Kulild, J.; Nagendrababu, V. Artificial Intelligence in Endodontics: Current Applications and Future Directions. J. Endod. 2021, 47, 1352–1357. [Google Scholar] [CrossRef] [PubMed]
- Khanagar, S.B.; Alfadley, A.; Alfouzan, K.; Awawdeh, M.; Alaqla, A.; Jamleh, A. Developments and Performance of Artificial Intelligence Models Designed for Application in Endodontics: A Systematic Review. Diagnostics 2023, 13, 414. [Google Scholar] [CrossRef] [PubMed]
- Hicks, S.A.; Strümke, I.; Thambawita, V.; Hammou, M.; Riegler, M.A.; Halvorsen, P.; Parasa, S. On Evaluation Metrics for Medical Applications of Artificial Intelligence. Sci. Rep. 2022, 12, 5979. [Google Scholar] [CrossRef] [PubMed]
- Issa, J.; Riad, A.; Olszewski, R.; Dyszkiewicz-Konwińska, M. The Influence of Slice Thickness, Sharpness, and Contrast Adjustments on Inferior Alveolar Canal Segmentation on Cone-Beam Computed Tomography Scans: A Retrospective Study. J. Pers. Med. 2023, 13, 1518. [Google Scholar] [CrossRef] [PubMed]
- Mazzi-Chaves, J.F.; Camargo, R.V.; Borges, A.F.; Silva, R.G.; Pauwels, R.; Silva-Sousa, Y.T.C.; Sousa-Neto, M.D. Cone-Beam Computed Tomography in Endodontics—State of the Art. Curr. Oral. Health Rep. 2021, 8, 9–22. [Google Scholar] [CrossRef]
- Venskutonis, T.; Plotino, G.; Juodzbalys, G.; Mickevičiene, L. The Importance of Cone-Beam Computed Tomography in the Management of Endodontic Problems: A Review of the Literature. J. Endod. 2014, 40, 1895–1901. [Google Scholar] [CrossRef] [PubMed]
- Patel, S. New Dimensions in Endodontic Imaging: Part 2. Cone Beam Computed Tomography. Int. Endod. J. 2009, 42, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Durack, C.; Abella, F.; Roig, M.; Shemesh, H.; Lambrechts, P.; Lemberg, K. European Society of Endodontology Position Statement: The Use of CBCT in Endodontics. Int. Endod. J. 2014, 47, 502–504. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; Dawood, A.; Pitt Ford, T.; Whaites, E. The Potential Applications of Cone Beam Computed Tomography in the Management of Endodontic Problems. Int. Endod. J. 2007, 40, 818–830. [Google Scholar] [CrossRef]
- Lo Giudice, R.; Nicita, F.; Puleio, F.; Alibrandi, A.; Cervino, G.; Lizio, A.S.; Pantaleo, G. Accuracy of Periapical Radiography and CBCT in Endodontic Evaluation. Int. J. Dent. 2018, 2018, 2514243. [Google Scholar] [CrossRef] [PubMed]
- Keerthana, G.; Singh, N.; Yadav, R.; Duhan, J.; Tewari, S.; Gupta, A.; Sangwan, P.; Mittal, S. Comparative Analysis of the Accuracy of Periapical Radiography and Cone-Beam Computed Tomography for Diagnosing Complex Endodontic Pathoses Using a Gold Standard Reference—A Prospective Clinical Study. Int. Endod. J. 2021, 54, 1448–1461. [Google Scholar] [CrossRef]
- Orhan, K.; Belgin, C.A.; Manulis, D.; Golitsyna, M.; Bayrak, S.; Aksoy, S.; Sanders, A.; Önder, M.; Ezhov, M.; Shamshiev, M.; et al. Determining the Reliability of Diagnosis and Treatment Using Artificial Intelligence Software with Panoramic Radiographs. Imaging Sci. Dent. 2023, 53, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Zadrożny, Ł.; Regulski, P.; Brus-Sawczuk, K.; Czajkowska, M.; Parkanyi, L.; Ganz, S.; Mijiritsky, E. Artificial Intelligence Application in Assessment of Panoramic Radiographs. Diagnostics 2022, 12, 224. [Google Scholar] [CrossRef]
- Kazimierczak, W.; Wajer, R.; Wajer, A.; Kalka, K.; Kazimierczak, N.; Serafin, Z. Evaluating the Diagnostic Accuracy of an AI-Driven Platform for Assessing Endodontic Treatment Outcomes Using Panoramic Radiographs: A Preliminary Study. J. Clin. Med. 2024, 13, 3401. [Google Scholar] [CrossRef] [PubMed]
- Szabó, V.; Szabo, B.T.; Orhan, K.; Veres, D.S.; Manulis, D.; Ezhov, M.; Sanders, A. Validation of Artificial Intelligence Application for Dental Caries Diagnosis on Intraoral Bitewing and Periapical Radiographs. J. Dent. 2024, 2024, 105105. [Google Scholar] [CrossRef] [PubMed]
- Kazimierczak, W.; Wajer, R.; Wajer, A.; Kiian, V.; Kloska, A.; Kazimierczak, N.; Janiszewska-Olszowska, J.; Serafin, Z. Periapical Lesions in Panoramic Radiography and CBCT Imaging—Assessment of AI’s Diagnostic Accuracy. J. Clin. Med. 2024, 13, 2709. [Google Scholar] [CrossRef] [PubMed]
- Ezhov, M.; Gusarev, M.; Golitsyna, M.; Yates, J.M.; Kushnerev, E.; Tamimi, D.; Aksoy, S.; Shumilov, E.; Sanders, A.; Orhan, K. Clinically Applicable Artificial Intelligence System for Dental Diagnosis with CBCT. Sci. Rep. 2021, 11, 15006. [Google Scholar] [CrossRef] [PubMed]
- Alves dos Santos, G.N.; Faria-e-Silva, A.L.; Ribeiro, V.L.; Pelozo, L.L.; Candemil, A.P.; Oliveira, M.L.; Lopes-Olhê, F.C.; Mazzi-Chaves, J.F.; Sousa-Neto, M.D. Is the Quality of Root Canal Filling Obtained by Cone-Beam Computed Tomography Associated with Periapical Lesions? A Systematic Review and Meta-Analysis. Clin. Oral. Investig. 2022, 26, 5105–5116. [Google Scholar] [CrossRef] [PubMed]
- Orhan, K.; Bayrakdar, I.S.; Ezhov, M.; Kravtsov, A.; Özyürek, T. Evaluation of Artificial Intelligence for Detecting Periapical Pathosis on Cone-Beam Computed Tomography Scans. Int. Endod. J. 2020, 53, 680–689. [Google Scholar] [CrossRef] [PubMed]
- Issa, J.; Jaber, M.; Rifai, I.; Mozdziak, P.; Kempisty, B.; Dyszkiewicz-Konwińska, M. Diagnostic Test Accuracy of Artificial Intelligence in Detecting Periapical Periodontitis on Two-Dimensional Radiographs: A Retrospective Study and Literature Review. Medicina 2023, 59, 768. [Google Scholar] [CrossRef] [PubMed]
- Fayad, M.I.; Nair, M.; Levin, M.D.; Benavides, E.; Rubinstein, R.A.; Barghan, S.; Hirschberg, C.S.; Ruprecht, A. AAE and AAOMR Joint Position Statement Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 1393–1396. [Google Scholar]
- Berkhout, W.E.R. The ALARA-Principle. Backgrounds and Enforcement in Dental Practices. Ned. Tijdschr. Tandheelkd. 2015, 122, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Frush, D.P. Justification and Optimization of CT in Children: How Are We Performing? Pediatr. Radiol. 2011, 41 (Suppl. S2), 467–471. [Google Scholar] [CrossRef] [PubMed]
- Waller, J.; O’connor, A.; Rafaat, E.; Amireh, A.; Dempsey, J.; Martin, C.; Umair, M. Applications and Challenges of Artificial Intelligence in Diagnostic and Interventional Radiology. Pol. J. Radiol. 2022, 87, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Chino, Y. AI in Medicine: Creating a Safe and Equitable Future. Lancet 2023, 402, 503. [Google Scholar] [CrossRef] [PubMed]
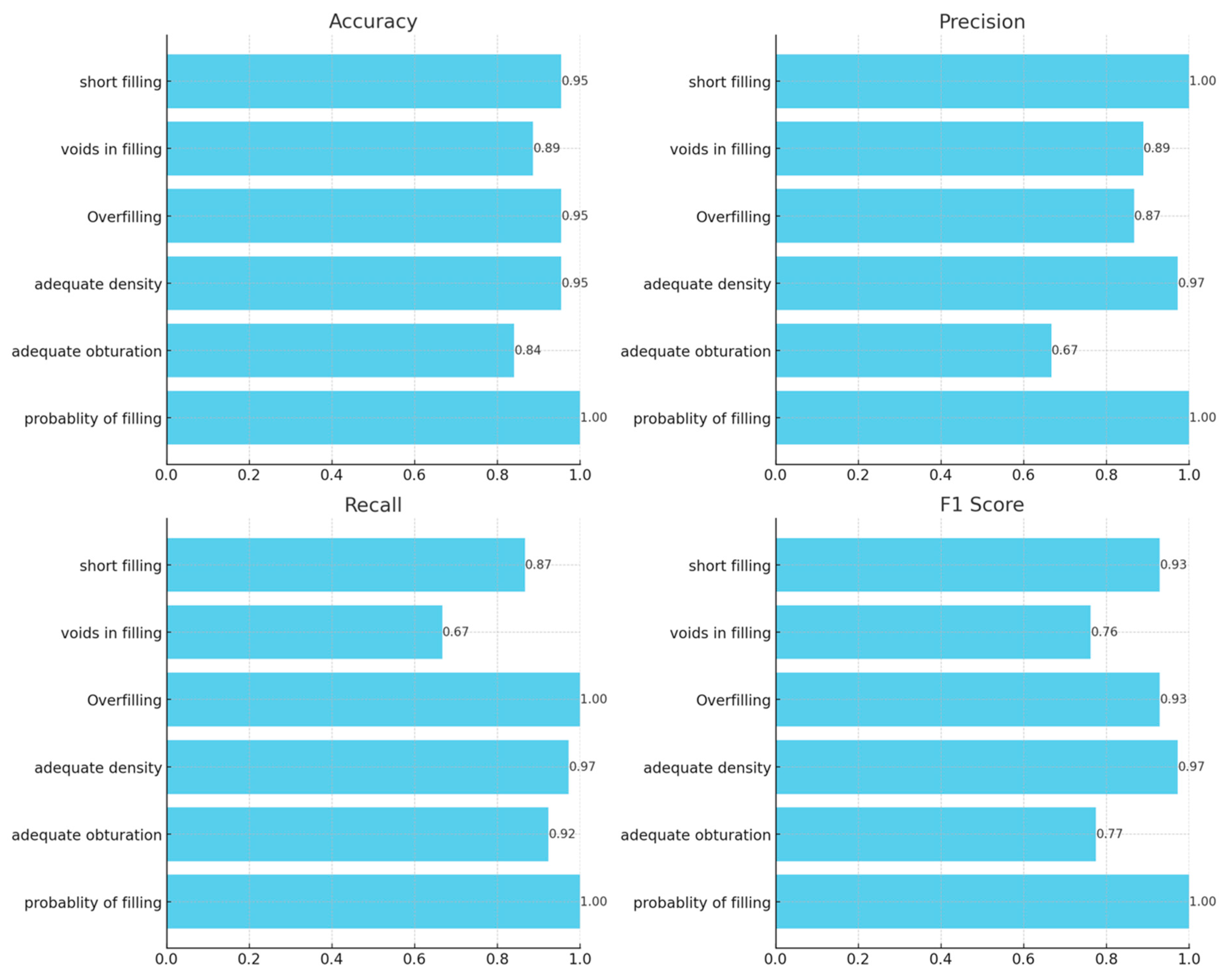
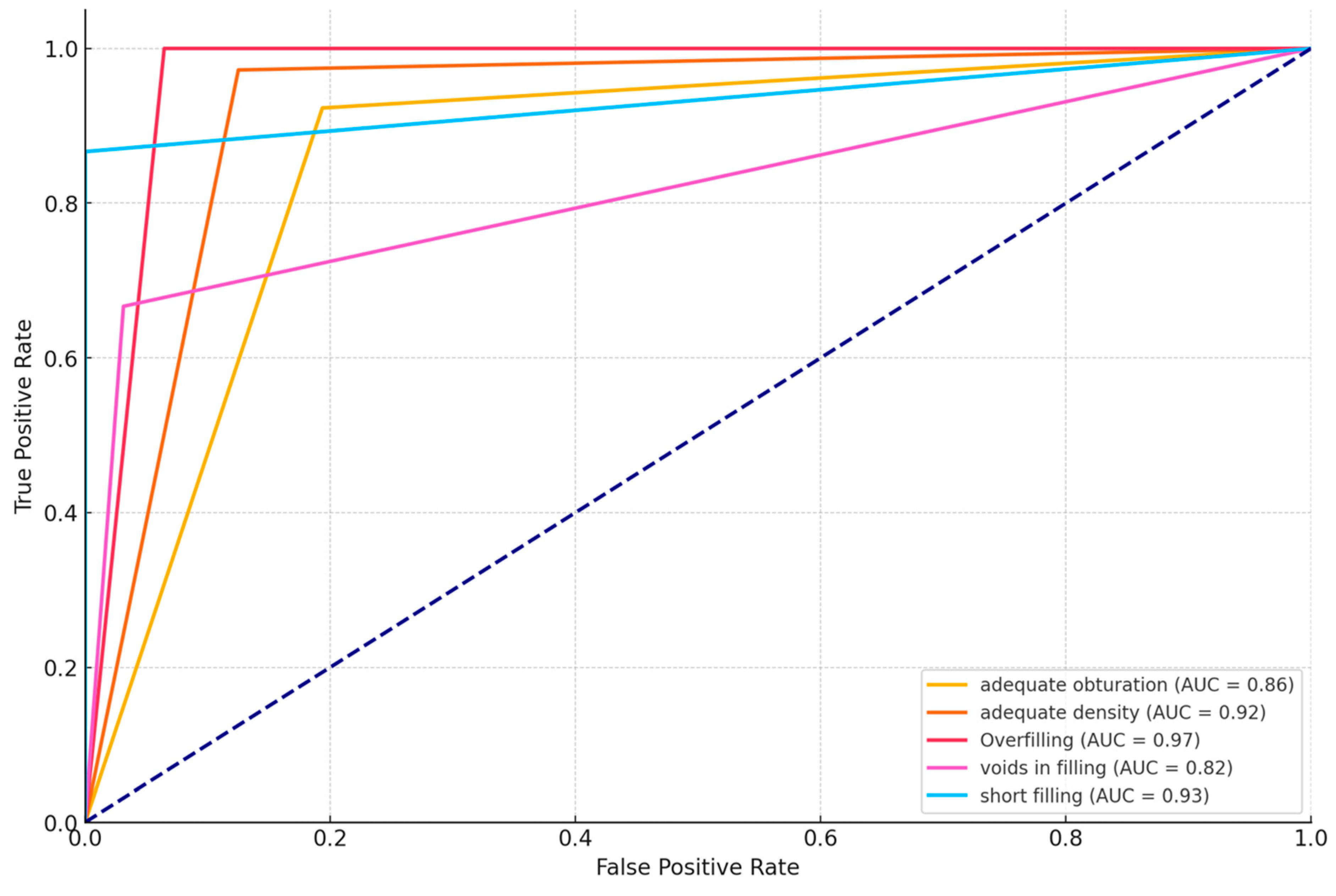
| Parameter | Accuracy | Precision | Recall | F1 Score |
|---|---|---|---|---|
| Probability of filling | 100% | 100% | 100% | 100% |
| Adequate obturation | 84.1% | 66.7% | 92,3% | 77.4% |
| Adequate density | 95.5% | 97.2% | 97.2% | 97.2% |
| Overfilling | 95.5% | 86.7% | 100% | 92.9% |
| Voids in filling | 88.6% | 88.9% | 66.7% | 76.2% |
| Short fillings | 95.5% | 100% | 86.7% | 92.9% |
| Parameter | ICC | 95% CI | Agreement (Cicchetti) | Agreement (Koo and Li) | |
|---|---|---|---|---|---|
| Root canals number | 0.958 | 0.941 | 0.971 | Excellent | Excellent |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kazimierczak, W.; Kazimierczak, N.; Issa, J.; Wajer, R.; Wajer, A.; Kalka, S.; Serafin, Z. Endodontic Treatment Outcomes in Cone Beam Computed Tomography Images—Assessment of the Diagnostic Accuracy of AI. J. Clin. Med. 2024, 13, 4116. https://doi.org/10.3390/jcm13144116
Kazimierczak W, Kazimierczak N, Issa J, Wajer R, Wajer A, Kalka S, Serafin Z. Endodontic Treatment Outcomes in Cone Beam Computed Tomography Images—Assessment of the Diagnostic Accuracy of AI. Journal of Clinical Medicine. 2024; 13(14):4116. https://doi.org/10.3390/jcm13144116
Chicago/Turabian StyleKazimierczak, Wojciech, Natalia Kazimierczak, Julien Issa, Róża Wajer, Adrian Wajer, Sandra Kalka, and Zbigniew Serafin. 2024. "Endodontic Treatment Outcomes in Cone Beam Computed Tomography Images—Assessment of the Diagnostic Accuracy of AI" Journal of Clinical Medicine 13, no. 14: 4116. https://doi.org/10.3390/jcm13144116








