Contemporary Concepts of Adhesive Cementation of Glass-Fiber Posts: A Narrative Review
Abstract
1. Introduction
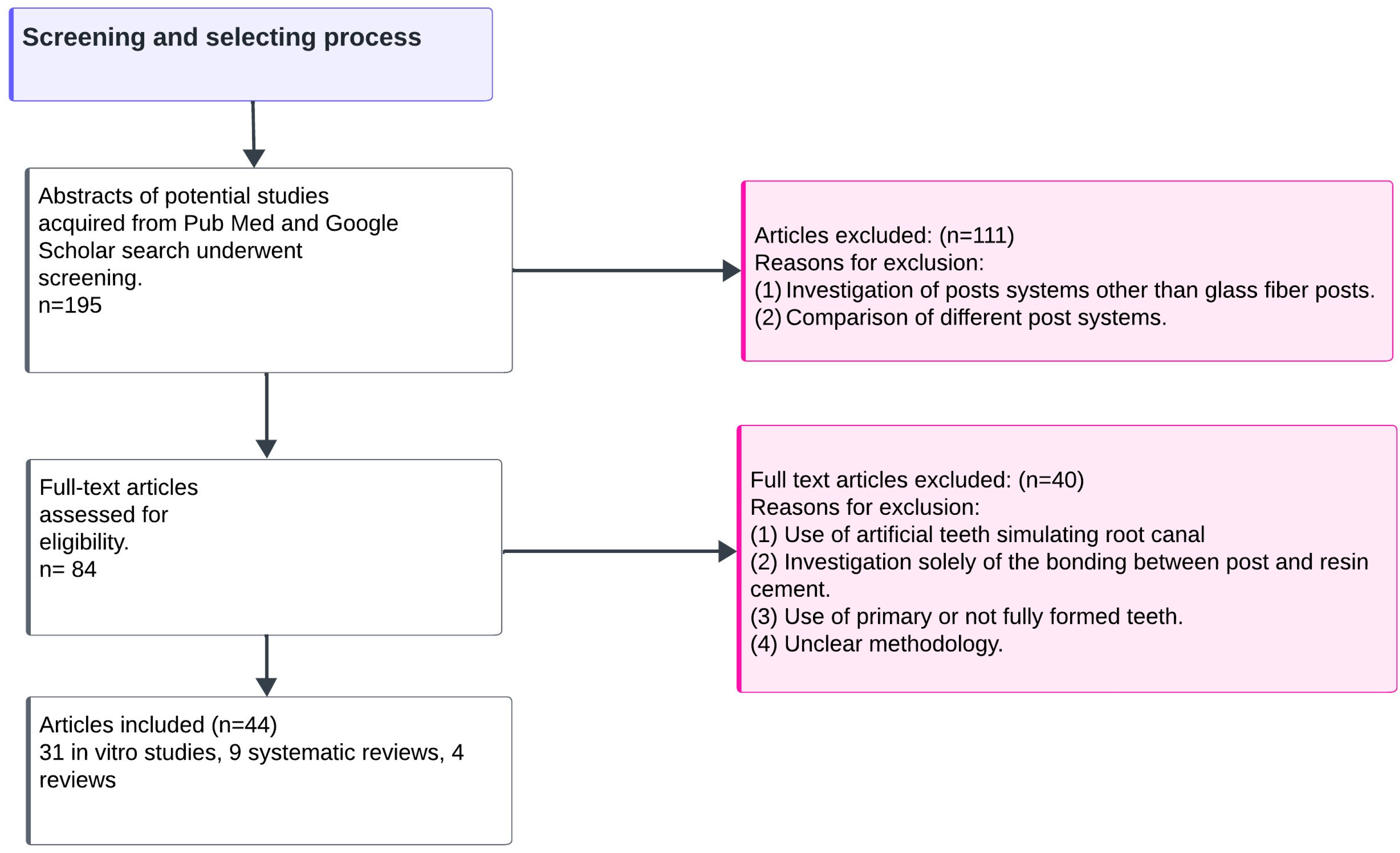
2. Materials and Methods
2.1. Data Sources
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Included Data
3. Results
3.1. Endodontic Sealers
3.2. Post Dimensions
3.3. Root Canal Irrigants
3.4. Surface Pretreatment of Glass Fiber Posts
3.5. Resin Cements, Adhesive Systems, and Hybrid Layer Formation
3.6. Cementation Technique
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Naumann, M.; Schmitter, M.; Frankenberger, R.; Krastl, G. “Ferrule comes first. Post is second!” fake news and alternativefacts? A systematic review. J. Endod. 2018, 44, 212–219. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Pontoriero, D.I.K.; Ferrari, C.E.; Carboncini, F. Restorative difficulty evaluation system of endodontically treated teeth. J. Esthet. Restor. Dent. 2022, 34, 65–80. [Google Scholar] [CrossRef] [PubMed]
- De Morais, D.C.; Butler, S.; Santos, M.J.M.C. Current Insights on Fiber Posts: A Narrative Review of Laboratory and Clinical Studies. Dent. J. 2023, 11, 236. [Google Scholar] [CrossRef] [PubMed]
- Coelho, C.S.; Biffi, J.C.; Silva, G.R.; Abrahão, A.; Campos, R.E.; Soares, C.J. Finite element analysis of weakened rootsrestored with composite resin and posts. Dent. Mater. J. 2009, 28, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Cagidiaco, M.C.; Goracci, C.; Vichi, A.; Mason, P.N.; Radovic, I.; Tay, F. Long-term retrospective study of the clinical performance of fiber posts. Am. J. Dent. 2007, 20, 287–291. [Google Scholar] [PubMed]
- De Moraes, A.P.; Cenci, M.S.; de Moraes, R.R.; Pereira-Cenci, T. Current concepts on the use and adhesive bonding of glass-fiber posts in dentistry: A review. Appl. Adhes. Sci. 2013, 1, 4. [Google Scholar] [CrossRef]
- Skupien, J.A.; Sarkis-Onofre, R.; Cenci, M.S.; Moraes, R.R.; Pereira-Cenci, T. A systematic review of factors associated with the retention of glass fiber posts. Braz. Oral Res. 2015, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sarkis-Onofre, R.; Skupien, J.A.; Cenci, M.S.; Moraes, R.R.; Pereira-Cenci, T. The role of resin cement on bond strength of glass-fiber posts luted into root canals: A systematic review and meta-analysis of in vitro studies. Oper. Dent. 2014, 39, E31–E44. [Google Scholar] [CrossRef] [PubMed]
- Daleprane, B.; Pereira, C.N.d.B.; Oréfice, R.L.; Bueno, A.C.; Vaz, R.R.; Moreira, A.N.; Magalhães, C. The effect of light-curing access and different resin cements on apical bond strength of fiber posts. Oper. Dent. 2014, 39, 93–100. [Google Scholar] [CrossRef]
- Pulido, C.A.; Franco, A.P.G.d.O.; Gomes, G.M.; Bittencourt, B.F.; Kalinowski, H.J.; Gomes, J.C.; Gomes, O.M.M. An in situ evaluation of the polymerization shrinkage, degree of conversion, and bond strength of resin cements used for luting fiber posts. J. Prosthet. Dent. 2016, 116, 570–576. [Google Scholar] [CrossRef]
- Tay, F.R.; Loushine, R.J.; Lambrechts, P.; Weller, R.N.; Pashley, D.H. Geometric factors affecting dentin bonding in root canals: A theoretical modeling approach. J. Endod. 2005, 31, 584–589. [Google Scholar] [CrossRef] [PubMed]
- Farina, A.P.; de Oliveira, E.; Disarz, A.; de Moura, A.L.; Durigon, M.; Souza, M.A.; Cecchin, D. Assessment of the Ability of Different Cleaning Protocols to Remove Eugenol-based Endodontic Sealer from the Root Dentin. J. Contemp. Dent. Pract. 2019, 20, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Vilas-Boas, D.A.; Grazziotin-Soares, R.; Ardenghi, D.M.; Bauer, J.; de Souza, P.O.; Candeiro, G.T.d.M.; Maia-Filho, E.M.; Carvalho, C.N. Effect of different endodontic sealers and time of cementation on push-out bond strength of fiber posts. Clin. Oral Investig. 2018, 22, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- Soares, I.M.V.; Crozeta, B.M.; Pereira, R.D.; Silva, R.G.; da Cruz-Filho, A.M. Influence of endodontic sealers with different chemical compositions on bond strength of the resin cement/glass fiber post junction to root dentin. Clin. Oral Investig. 2020, 24, 3417–3423. [Google Scholar] [CrossRef] [PubMed]
- Zaniboni, J.F.; Silva, A.M.; Fernández, E.; Alencar, C.D.M.; Morais, J.M.P.; de Campos, E.A.; Kuga, M.C. Temporary cement residues affect the bond strength and dentin penetration of self-adhesive resin cement in fiberglass post cementation. Microsc. Res. Tech. 2021, 84, 2351–2360. [Google Scholar] [CrossRef] [PubMed]
- Webber, M.B.; Michida, S.M.; Marson, F.C.; de Oliveira, G.C.; Silva, C.D.O. Analysis of bond strength by pull out test on fiber glass posts cemented in different lengths. J. Int. Oral Health 2015, 7, 7–12. [Google Scholar] [PubMed]
- Abdulrazzak, S.S.; Sulaiman, E.; Atiya, B.K.; Jamaludin, M. Effect of ferrule height and glass fibre post length on fracture resistance and failure mode of endodontically treated teeth. Aust. Endod. J. 2014, 40, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Franco, E.B.; Lins do Valle, A.; Pompéia Fraga de Almeida, A.L.; Rubo, J.H.; Pereira, J.R. Fracture resistance of endodontically treated teeth restored with glass fiber posts of different lengths. J. Prosthet. Dent. 2014, 111, 30–34. [Google Scholar] [CrossRef]
- Freitas, T.L.; Vitti, R.P.; Miranda, M.E.; Brandt, W.C. Effect of Glass Fiber Post Adaptation on Push-Out Bond Strength to Root Dentin. Braz. Dent. J. 2019, 30, 350–355. [Google Scholar] [CrossRef]
- Durski, M.; Metz, M.; Crim, G.; Hass, S.; Mazur, R.; Vieira, S. Effect of Chlorhexidine Treatment Prior to Fiber Post Cementation on Long-Term Resin Cement Bond Strength. Oper. Dent. 2018, 43, E72–E80. [Google Scholar] [CrossRef]
- Cândido, B.D.; Manzoli, T.M.; Zaniboni, J.F.; Besegato, J.F.; Godoy, E.F.; Kuga, M.C.; Dantas, A.A.R. Effect of antioxidants after post-space irrigation on the adhesive interface of glass fiber post cementation. J. Esthet. Restor. Dent. 2023, 35, 1293–1300. [Google Scholar] [CrossRef] [PubMed]
- Alkahtany, M.F. Extrusion bond strength of glass fiber post to radicular dentin after final irrigation using MTAD, EDTA, Pineapple peel extract, and Riboflavin. Photodiagn. Photodyn. Ther. 2022, 39, 102982. [Google Scholar] [CrossRef] [PubMed]
- Jalali, H.; Farid, F.; Kulivand, S.; Nokar, S.; Dadgar, K. Effect of Different Irrigants Applied After Post Space Preparation on Push-Out Bond Strength of a Self-Etch Resin Cement. J. Dent. 2018, 15, 222–229. [Google Scholar]
- Wan, S.; Tan, Y.; Xie, J.; Huang, X.; Guo, L. The effect of a root-dentin pretreatment technique combining PIPS with MTAD aiming to improve the bond strength of glass fiber post. Microsc. Res. Tech. 2020, 83, 824–833. [Google Scholar] [CrossRef] [PubMed]
- Elnaghy, A.M.; Elsaka, S.E. Effect of surface treatments on the flexural properties and adhesion of glass fiber-reinforced composite post to self-adhesive luting agent and radicular dentin. Odontology 2016, 104, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Samimi, P.; Mortazavi, V.; Salamat, F. Effects of heat treating silane and different etching techniques on glass fiber post push-out bond strength. Oper. Dent. 2014, 39, E217–E224. [Google Scholar] [CrossRef] [PubMed]
- Majeti, C.; Veeramachaneni, C.; Morisetty, P.K.; Rao, S.A.; Tummala, M. A simplified etching technique to improve the adhesion of fiber post. J. Adv. Prosthodont. 2014, 6, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Do Nascimento Rechia, B.C.; Bravo, R.P.; de Oliveira, N.D.; Baratto Filho, F.; Gonzaga, C.C.; Storrer, C.L.M. Influence of Different Surface Treatments of Fiberglass Posts on the Bond Strength to Dentin. Braz. J. Oral Sci. 2016, 15, 158–162. [Google Scholar] [CrossRef]
- Dos Santos, L.R.; Lima, D.M.; Carvalho, E.M.; Rodrigues, V.P.; Alves, C.M.C. Effect of Glass Fiber Post Surface Treatment on Bond Strength of a Self-Adhesive Resin Cement: An “In Vitro” Study. Int. J. Dent. 2021, 2021, 8856657. [Google Scholar] [CrossRef]
- Jana, S.; Desai, P.D.; Das, D.; Mazumdar, P.; Majumdar, T.K. Comparative evaluation of adhesion of glass fiber post to the root dentin after surface treatment of post and using universal bonding agent: An in vitro study. J. Conserv. Dent. 2022, 25, 636–641. [Google Scholar] [CrossRef]
- Gomes, K.G.F.; Faria, N.S.; Neto, W.R.; Colucci, V.; Gomes, E.A. Influence of laser irradiation on the push-out bond strength between a glass fiber post and root dentin. J. Prosthet. Dent. 2018, 119, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Hm, K.K.; Barakat, A.A.; Qamar, Z.; Reddy, R.N.; Vempalli, S.; Ramadan, A.H.; Niazi, F.; Noushad, M. Glass fiber post resistance to dislodgement from radicular dentin after using contemporary and conventional methods of disinfection. Photodiagn. Photodyn. Ther. 2022, 40, 103026. [Google Scholar] [CrossRef] [PubMed]
- Migliau, G.; Piccoli, L.; Di Carlo, S.; Pompa, G.; Besharat, L.K.; Dolci, M. Comparison between three glass fiber post cementation techniques. Ann. Stomatol. 2017, 8, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Nadler, A.; da Silva, E.; Lins-Filho, P.; Dias, M.; Guimarães, R.; da Silva, C.; Silva, S.; Gomes, A. Influence of different adhesion strategies on glass fiber post retention. J. Clin. Exp. Dent. 2023, 15, e649–e657. [Google Scholar] [CrossRef] [PubMed]
- Yaman, B.C.; Ozer, F.; Takeichi, T.; Karabucak, B.; Koray, F.; Blatz, M.B. Effect of thermomechanical aging on bond strength and interface morphology of glass fiber and zirconia posts bonded with a self-etch adhesive and a self-adhesive resin cement to natural teeth. J. Prosthet. Dent. 2014, 112, 455–464. [Google Scholar] [CrossRef]
- Barcellos, D.C.; Huhtala, M.F.R.L.; Silva, M.A.; Gomes, A.P.M.; Franco, L.T.F. Influence of adhesive system in bond strength of fiber glass posts to radicular dentin using dual cure resin cement. Braz. Dent. Sci. 2014, 17, 4–10. [Google Scholar] [CrossRef]
- Rezende, E.C.; Gomes, G.M.; Szesz, A.L.; da Silveira Bueno, C.E.; Reis, A.; Loguercio, A.D. Effects of Dentin Moisture on Cementation of Fiber Posts to Root Canals. J. Adhes. Dent. 2016, 18, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Durski, M.T.; Metz, M.J.; Thompson, J.Y.; Mascarenhas, A.; Crim, G.; Vieira, S.; Mazur, R. Push-Out Bond Strength Evaluation of Glass Fiber Posts with Different Resin Cements and Application Techniques. Oper. Dent. 2016, 41, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Pereira, R.D.; Valdívia, A.D.; Bicalho, A.A.; Franco, S.; Tantbirojn, D.; Versluis, A.; Soares, C. Effect of Photoactivation Timing on the Mechanical Properties of Resin Cements and Bond Strength of Fiberglass Post to Root Dentin. Oper. Dent. 2015, 40, E206–E221. [Google Scholar] [CrossRef]
- Borges, M.G.; Faria-e-Silva, A.L.; Santos-Filho, P.C.; Silva, F.P.; Martins, L.R.; Menezes Mde, S. Does the moment of fiber post cutting influence on the retention to root dentin? Braz. Dent. J. 2015, 26, 141–145. [Google Scholar] [CrossRef]
- Silva, N.R.D.; Rodrigues, M.P.; Bicalho, A.A.; Deus, R.A.; Soares, P.B.F.; Soares, C.J. Effect of Magnification during Post Space Preparation on Root Cleanness and Fiber Post Bond Strength. Braz. Dent. J. 2019, 30, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Altmann, A.S.; Leitune, V.C.; Collares, F.M. Influence of Eugenol-based Sealers on Push-out Bond Strength of Fiber Post Luted with Resin Cement: Systematic Review and Meta-analysis. J. Endod. 2015, 41, 1418–1423. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, L.V.; Maia, T.S.; Zancopé, K.; Menezes, M.S.; Soares, C.J.; Moura, C.C.G. Can intra-radicular cleaning protocols increase the retention of fiberglass posts? A systematicreview. Braz. Oral Res. 2018, 32, e16. [Google Scholar] [CrossRef] [PubMed]
- Mishra, L.; Khan, A.S.; Velo, M.M.d.A.C.; Panda, S.; Zavattini, A.; Rizzante, F.A.P.; Arbildo Vega, H.I.; Sauro, S.; Lukomska-Szymanska, M. Effects of Surface Treatments of Glass Fiber-Reinforced Post on Bond Strength to Root Dentine: A Systematic Review. Materials 2020, 13, 1967. [Google Scholar] [CrossRef] [PubMed]
- Moraes, A.P.; Sarkis-Onofre, R.; Moraes, R.R.; Cenci, M.S.; Soares, C.J.; Pereira-Cenci, T. Can Silanization Increase the Retention of Glass-fiber posts? A Systematic Review and Meta-analysis of In Vitro Studies. Oper. Dent. 2015, 40, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.C.M.; Fernandes, V.; Correia, A.; Miller, P.; Carvalho, O.; Silva, F.; Özcan, M.; Henriques, B. Surface modification of glass fiber-reinforced composite posts to enhance their bond strength to resin-matrix cements: An integrative review. Clin. Oral Investig. 2022, 26, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Miotti, L.L.; Follak, A.C.; Montagner, A.F.; Pozzobon, R.T.; da Silveira, B.L.; Susin, A.H. Is Conventional Resin Cement Adhesive Performance to Dentin Better Than Self-adhesive? A Systematic Review and Meta-Analysis of Laboratory Studies. Oper. Dent. 2020, 45, 484–495. [Google Scholar] [CrossRef]
- Angnanon, W.; Thammajaruk, P.; Guazzato, M. Effective luting agents for glass-fiber posts: A network meta-analysis. Dent. Mater. 2023, 39, 1180–1189. [Google Scholar] [CrossRef]
| Authors | Year | Method | Results |
|---|---|---|---|
| Ana P Farina, Emanuele de Oliveira, Alana Disarz, Ana LC de Moura, Migueli Durigon, Matheus A Souza, Doglas Cecchin [12]. | 2019 | 60 bovine teeth obturated with eugenol-based sealer and gutta-percha points: 1. negative control (unfilled), 2. positive control (saline solution), 3. 95% alcohol, 4. amylacetate, 5. largo bur. | Cleaning protocols 3 and 5 led to the same bond strength values as the negative control group. |
| Danielle Araújo Vilas-Boas, Renata Grazziotin-Soares, Diego Machado Ardenghi, José Bauer, Patrícia Oliveira de Souza, George Táccio de Miranda Candeiro, Etevaldo Matos Maia-Filho, Ceci Nunes Carvalho [13]. | 2018 | 72 premolars obturated with 1. epoxy-amine resin-based sealer, 2. eugenol-based sealer, 3. bioceramic sealer and gutta-percha points. Posts were cemented either immediately after obturation or seven days after. Bond strength was compared with a control group where no obturation was performed. | Bond strength values of posts cemented at root canals obturated with epoxy-amine resin-based sealer was equal to that of the control group. Eugenol-based and bioceramic sealers showed reduced bond strength values. |
| Isadora Mello Vilarinho Soares, Bruno Monguilhott Crozeta, Rodrigo Dantas Pereira, Ricardo Gariba Silva, Antonio Miranda da Cruz-Filho [14]. | 2020 | 72 canines were divided into 6 groups according to the endodontic sealer used. 1: control; 2: eugenol-based sealer; 3 salicylate-based sealer with calcium hydroxide; 4: epoxy resin-based sealer; 5: epoxy resin-based sealer with calcium hydroxide; and 6: calcium silicate-based sealer. | Group 4 showed the highest bond strength values, similar to the control group. |
| Joissi Ferrari Zaniboni, Aryvelto Miranda Silva, Cristiane de Melo Alencar, Eduardo Fernandez, Jéssika Mayhara Pereira Morais, Edson Alves de Campos, Milton Carlos Kuga [15]. | 2021 | Temporary metal posts were cemented to 60 root canals using 3 different temporary cements, one eugenol-based and 2 eugenol-free, before glass fiber post cementation with resin cement. Twenty glass fiber posts were cemented to root canals in which no metal post was cemented (control group). | Temporary resin cement negatively affects bond strength values of glass fiber posts regardless of its composition and root canal third. |
| Mariana Benedetti Ferreira Webber, Silvia Masae de Araújo Michida, Fabiano Carlos Marso, Giovani Corrêa de Oliveira, Cleverson de Oliveira e Silva [16]. | 2014 | Specimens were divided into three groups according to length of the glass fiber posts. Group 1: 2/3 of root canal’s length (14 mm); Group 2: 1/2 (10.5 mm); Group 3: 1/4 (5.25 mm). | Bond strength values did not differ between Group 1 and Group 2. |
| Shurooq S. Abdulrazzak, Eshamsul Sulaiman, Basim K. Atiya, Marhazlinda Jamaludin [17]. | 2014 | 90 maxillary central incisors received glass fiber posts, resin composite core build-up, and cast metal crowns. Specimens were divided into three groups. Group 1: 4 mm ferrule height; Group 2: 2 mm ferrule height; Group 3: 0 mm ferrule height. Each group was further subdivided into 3 groups. Subgroup 1: posts with length equal to 2/3 of root length; Subgroup 2: posts with length equal to 1/2 of root length; Subgroup 3: posts with length equal to 1/3 of root length. | There were significant differences in the failure load in the ferrule height groups, but no significant differences in post length groups and no significant interaction between ferrule heights and post lengths. |
| Érico Braga Franco, Accacio Linsdo Valle, Ana Lúcia Pompéia Fragade Almeida, José Henrique Rubo, Jefferson Ricardo Pereira [18]. | 2014 | 40 canines were divided into 4 groups according to the core build up restoration. Group 1: custom metal post and core-control group; Group 2: glass fiber post with length equal to 1/3 of root’s length (5 mm); Group 3: 1/2 (7.5 mm); Group 4: 2/3 (10 mm). | Control group presented three times higher resistance to static load than the other groups. There were no differences between Groups 2, 3, and 4. |
| Thiago Lopes de Freitas, Rafael Pino Vitti, Milton Edson Miranda, William Cunha Brandt [19]. | 2019 | 40 human teeth with same post space size (1.8 mm cervical, 1.05 mm apical) received glass fiber posts with 4 different sizes. Group 1: 1.6 mm coronal, 0.65 mm apical; Group 2: 1.8 mm coronal, 1.05 mm apical; Group 3: 1.4 mm coronal, 0.65 mm apical; Group 4: customized posts with composite resin. | Group 2 and Group 4 had the highest bond strength values that were significant different from the two other groups. |
| M. Durski, M. Metz, G. Crim, S. Hass, R. Mazur, S. Vieira [20] | 2018 | 120 premolars were divided into 12 groups according to 1. treatment with chlorhexidine, 2. type of resincement (conventional/self-adhesive), and 3. Number of thermal cycles (0/20,000/40,000). | Additional treatment with chlorhexidine before the cement application produced significantly higher bond strength values regardless of cement, root thirds, or thermocycling. |
| Beatriz Dansini Cândido, Tatiane Miranda Manzoli, Joissi Ferrari Zaniboni, Joao Felipe Besegato, Eduardo Fernández Godoy, Milton Carlos Kuga, Andréa Abi Rached Dantas [21]. | 2023 | 60 bovine roots were divided into 6 groups according to the root canal irrigants used before the cementation of the post. Group 1: 2.5% NaOCl + 17% EDTA; Group 2: 2.5% NaOCl + 17% EDTA + 10% sodium ascorbate; Group 3: 2.5% NaOCl + 17% EDTA + 20% alpha-tocopherol; Group 4: peracetic acid; Group 5: peracetic acid + 10% sodium ascorbate; Group 6: peracetic acid + 20% alpha-tocopherol. | Groups 2, 3, 4, 5, and 6 had similar bond strength values. |
| Mazen F. Alkahtany [22] | 2022 | 140 premolars were divided into 4 groups according to the root canal irrigant used. Group 1: NaOCl + EDTA; Group 2: NaOCl + MTAD; Group 3: NaOCl + riboflavin; Group 4: NaOCl + pineapple peel extract. | Group 2 and Group 4 showed the highest bond strength values with no significant difference between them. |
| Hamid Jalali, Farzaneh Farid, Sudabeh Kulivand, Saeed Nokar, Kosar Dadgar [23]. | 2018 | 72 premolars were divided into 6 groups according to the root canal irrigant used before the cementation of the post. Group 1: Saline solution control group; Group 2: NaOCl; Group 3: EDTA; Group 4: chlorhexidine; Group 5: MTAD; Group 6: phosphoric acid. | Groups 3, 5, and 6 showed the highest bond strength values, which were similar to each other and significantly different from the control group. The difference between the control group and Group 4 was marginally significant. |
| Shu Wan, Yujie Tan, Jing Xie, Xiaoyu Huang, Ling Guo [24]. | 2020 | 55 human mandibular premolars were divided into 5 groups according to the root canal irrigant or technique used before the cementation of the glass fiber posts. Group 1: control group (distilled water); Group 2: 2.5% NaOCl + 17%EDTA; Group 3: MTAD; Group 4: PIPS technique; Group 5: MTAD + PIPS technique. | Group 5 displayed the best result concerning smear layer removal and bond strength values. |
| Amr M. Elnaghy, Shaymaa E. Elsaka [25]. | 2014 | 75 human teeth received glass fiber posts cemented with dual-cure self-adhesive resin cement. Specimens were divided according to the surface treatment of the posts: Control group 1: no treatment; Group 1: silanization for 60 s; Group 2: airborne-particle abrasion; Group 3: etching with 9% hydrofluoric acid for 1 min; and Group 4: etching with CH2 Cl2 for 10 min. | Group 4 showed a significantly higher bond strength than the other groups. The bond strength of Group 1 was equal to the bond strength of the control group. The bond strength of Group 2 and Group 3 was significantly lower than the bond strength of the control group. |
| P. Samimi, V. Mortazavi, F. Salamat [26]. | 2014 | 40 human teeth received glass fiber posts. Specimens were divided into 5 groups according to post surface treatment. Group 1: hydrofluoric acid etching and silane application; Group 2: hydrofluoric acid etching and silane application that received heat treatment; Group 3: hydrogen peroxide etching and silane application; Group 4: hydrogen peroxide etching application that received heat treatment; Control group: no pretreatment. Conventional resin cement combined with self-etch adhesive system was used. | Bond strength was significantly affected by the heat treatment of the applied silane. |
| Chandrakanth Majeti, Chandrasekhar Veeramachaneni, Pradeep Kumar Morisetty, Saggurti Anitha Rao, Muralidhar Tummala [27]. | 2014 | 90 human maxillary central incisors received glass fiber posts luted with self-adhesive resin cement. Posts were divided into 3 groups based on the surface treatment they received (phosphoric acid 37%, hydrogen peroxide 24%, and distilled water). Each surface treatment method was applied for 3 different time periods (15 s, 30 s, 60 s). | The highest bond strength values were acquired when phosphoric acid was used for 15 s and when hydrogen peroxide was used for 60 s. There was no significant difference between those two groups. |
| Bruna Cristinado Nascimento Rechia, Ruth Peggy Bravo, Naylin Danyelede Oliveira Carla Castiglia Gonzaga, Flares Baratto Filho, Carmen L. Mueller Storrer [28]. | 2016 | 30 glass fiber posts were cemented to 30 bovine root canals with self-adhesive resin cement. Specimens were divided into 3 groups according to the surface treatment of the posts. Group 1: silane application; Group 2: silane and adhesive system application; Group 3: silane application dried with hot air. | Group 2 and Group 3 had the highest bond strength values with no significant difference between them. |
| Lairds Rodrigues dos Santos, Darlon Martins Lima, Edilausson Moreno Carvalho, Vandilson Pinheiro Rodrigues, Claudia Maria Coelho Alves [29]. | 2021 | 84 bovine teeth received glass fiber posts. The specimens were divided into 6 groups according to the post’s surface pretreatment. Group 1: no surface pretreatment; Group 2: silane application; Group 3: 24% hydrogen peroxide application; Group 4: 24% hydrogen peroxide and silane application; Group 5: air abrasion (50 μm aluminum oxide particles); Group 6: air abrasion and silane application. | Groups 2, 4, and 6 had the highest bond strength values with no significant difference between them. |
| Sriparna Jana, Priti D. Desai, Debojyoti Das, Paromita Mazumdar, Tushar Kanti Majumdar [30]. | 2022 | 40 maxillary central incisors received glass fiber posts. The specimens were divided into 4 groups according to the post’s surface pretreatment. Group 1: silane application; Group 2: air abrasion (30 μm silicone dioxide particles) and silane application; Group 3: 9% hydrofluoric acid and silane application; Group 4: silane and universal bond application. | Group 2 had the highest mean bond strength values. |
| Karla G. F. Gomes, Natália S. Faria, Walter R. Neto, Vivian Colucci, Erica A. Gomes [31]. | 2017 | 32 bovine teeth received glass fiber posts. The specimens were divided into 4 groups according to the surface pretreatment of the posts. Group 1: silane application control group; Group 2: irradiation with Er:YAG laser; Group 3: irradiation with Er;Cr:YSSG laser; Group 4: irradiation with 980 nm diode laser. | Group 3 had the highest mean bond strength values. |
| Khuthija Khanum HM, Ali Abdulmajeed Barakat, Zeeshan Qamar, R. Naveen Reddy, Swetha Vempalli, Anas Hussam Ramadan, Fayez Niazi, Mohammed Noushad [32] | 2022 | 50 premolars received glass fiber posts. The specimens were divided into 5 groups according to the post surface disinfection protocol. Group 1: autoclave sterilization; Group 2: chlorhexidine digluconate; Group 3: CPS solution; Group 4: 35% phosphoric acid gel; Group 5: no disinfection. | Group 2 and Group 4 had the highest bond strength values that were significantly different from the other groups. |
| Camilo Andrés Pulido, Ana Paula Gebertde Oliveira Franco, Giovana Mongruel Gomes, Bruna Fortes Bittencourt, Hypolito José Kalinowski, João Carlos Gomes, Osnara Maria Mongruel Gomes [10]. | 2016 | 30 maxillary canines received glass fiber posts. Specimens were divided into 2 groups according to the cementation system. Group 1: conventional resin cement combined with etch-and-rinse adhesive system; Group 2: self-adhesive resin cement. | Group 1 and Group 2 had similar polymerization shrinkage values. Group 1 had higher degree of conversion values. Bond strength was significantly higher in the cervical region only when conventional resin cement was used. |
| Guido Migliau, Luca Piccoli, Stefano Di Carlo, Giorgio Pompa, Laith Konstantinos Besharat, Marco Dolci [33]. | 2017 | 30 teeth divided into 3 groups according to the resin cement/adhesive system used for the adhesive luting of the posts. Group 1: Conventional resin cement combined with total etch adhesive system; Group 2: self-adhesive resin cement; Group 3: conventional resin cement combined with self-etch adhesive system. | Group 1 had double mean bond strength values than Groups 2 and 3. |
| Ana Michelle Oliveira Nadler, Evair Josino da Silva, Paulo Cardoso Lins Filho, Marlon Ferreira Dias, Renata Pedrosa Guimarães, Claudio Heliomar Vicente da Silva, Sérgiodos Santos Silva, Anderson Stevens Leonidas Gomes [34]. | 2023 | 55 premolars divided into 5 groups according to the resin cement/adhesive system used for the adhesive luting of the posts. Groups 1, 2, and 3: conventional resin cement combined with etch-and-rinse adhesive system; Group 4: conventional resin cement combined with self-etch adhesive system; Group 5: self-adhesive resin cement. | Groups 2 and 3 had the highest mean bond strength values. Group 3 had similar bond strength values as Group 4 and Group 5 in the middle and in the apical third of the root canal. Group 1 had similar bond strength values with Group 4 and Group 5 in the cervical and the middle third of the root canal. |
| Batu Can Yaman, Fusun Ozer, Takuro Takeichi, Bekir Karabucak, Fatma Koray, Markus B. Blatz [35]. | 2014 | Glass fiber posts or zirconia posts were luted to root canals of 80 premolars. Specimens were divided into 2 main groups according to the resin cement/adhesive system used. Group 1: conventional resin cement combined with self-etch adhesive system; Group 2: self-adhesive cement. In each group, half of the specimens were subjected to a thermomechanical aging procedure. | For glass fiber posts without TMA, Group 1 had higher bond strength values than Group 2. After the TMA bond strength values of Group 1 were reduced, Group 2 had higher bond strength values than Group 1. |
| Daphne Câmara Barcellos, Maria Filomena Rochalima Huhtala, Melissa Aline Silva, Ana Paula Martins Gomes, Lucas Teixeira Franco [36]. | 2014 | Glass fiber posts were luted to root canals of 25 human teeth using the same conventional resin cement in combination with a. a self-etch adhesive system; b. etch-and-rinse adhesive system (etching with phosphoric acid 37% for 15 s.) | Bond strength values, when self-etch adhesive system was used, were double that of those acquired when the etch-and-rinse adhesive system was used. |
| Eluise C. Rezende, Giovana Mongruel Gomes, Anna Luiza Szesz, Carlos Eduardo da Silveira Bueno, Alessandra Reise, Alessandro D. Loguercio [37]. | 2016 | 72 glass fiber posts were luted to premolars. Specimens were divided into 6 groups according to the combination of 2 factors: resin cement/adhesive system (2 different etch-and-rinse adhesive systems and 2 different conventional resin cements) and dentine moisture (dry, wet, and overwet). | For both adhesive systems/resin cements, higher bond strength values and lower nanoleakages were observed when the dentin was wet, and lower bond strength values and higher nanoleakage were observed when the dentin was dry. The results when the dentin was overwet were intermediate. |
| MT. Durski, MJ. Metz, JY. Thompson, AK. Mascarenhas, GA. Crim, S. Vieira, R. Mazur [38]. | 2016 | 60 glass fiber posts were luted to premolars. Specimens where divided into 3 groups according to the resin cement. Group 1: conventional resin cement in combination with etch-and-rinse adhesive system; Group 2: self-adhesive resin cement; Group 3: the same self-adhesive resin cement in combination with an extra step of phosphoric acid etching. Each group further divided into 3 subgroups according to cement application technique. Subgroup 1: application with an elongation tip; Subgroup 2: application with a microbrush. | Higher mean bond strength values at the apical third of all groups were observed when the resin cement was applied with the elongation tip compared to the micro brush. Resin cement application with the elongation tip led to higher bond strength values at the cervical and the middle thirds for Group 2. The extra etching step before the self-etch adhesive cementation appeared to be effective in enhancing bond strength. |
| RD. Pereira, Valdivia, AA. Bicalho, SD. Franco, D. Tantbirojn, A. Versluis, CJ. Soares [39]. | 2015 | 135 glass fiber posts were luted to bovine teeth with 3 different resin cements. Group 1: self-adhesive resin cement; Group 2: conventional resin cement in combination with self-etch adhesive system; Group 3: conventional resin cement in combination with etch-and-rinse adhesive system. Three different photoactivation timings were used: 1. light curing immediately; 2. after 3 min; 3. after 5 min. | Higher bond strength values were achieved when photoactivation timing 2 and 3 were used in all groups, with significant differences between photoactivation timing 2 and photoactivation timing 3 for Group 1 and Group 3. Photoactivation timing affected the resin cement’s mechanical properties in Group 1. Shrinkage stress values decreased gradually with delayed photoactivation in all groups. |
| Marcela G. Borges, André L. Faria-e-Silva, Paulo C. F. Santos-Filho, Fernanda P. Silva, Luís R. M. Martins, Murilo de Sousa Menezes [40]. | 2015 | 60 glass fiber posts were cemented to bovine incisors using 1. conventional resin cement in combination with etch-and-rinse adhesive system and 2. self-adhesive resin cement. Posts were cut 1. prior to post cementation; 2. immediately after post cementation; 3. after core build up. | Bond strength was reduced when conventional resin cement was used and the post was cut immediately. |
| Natércia Rezende da Silva, Monise de Paula Rodrigues, Aline Aredes Bicalho, Raissa Albuquerque de Deus1 Soares, Carlos José Soares, Priscilla Barbosa Ferreira [41]. | 2019 | 30 central upper incisors were divided into 3 groups according to magnification method used during the cementation process. Group 1: naked eye; Group 2: 3× magnification using dental loupe; Group 3: 6× magnification using microscope. | No difference in the amount of residues and in bond strength values were observed between the 3 groups. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsolomitis, P.; Diamantopoulou, S.; Papazoglou, E. Contemporary Concepts of Adhesive Cementation of Glass-Fiber Posts: A Narrative Review. J. Clin. Med. 2024, 13, 3479. https://doi.org/10.3390/jcm13123479
Tsolomitis P, Diamantopoulou S, Papazoglou E. Contemporary Concepts of Adhesive Cementation of Glass-Fiber Posts: A Narrative Review. Journal of Clinical Medicine. 2024; 13(12):3479. https://doi.org/10.3390/jcm13123479
Chicago/Turabian StyleTsolomitis, Panayiotis, Sofia Diamantopoulou, and Efstratios Papazoglou. 2024. "Contemporary Concepts of Adhesive Cementation of Glass-Fiber Posts: A Narrative Review" Journal of Clinical Medicine 13, no. 12: 3479. https://doi.org/10.3390/jcm13123479
APA StyleTsolomitis, P., Diamantopoulou, S., & Papazoglou, E. (2024). Contemporary Concepts of Adhesive Cementation of Glass-Fiber Posts: A Narrative Review. Journal of Clinical Medicine, 13(12), 3479. https://doi.org/10.3390/jcm13123479






