Unique Presentation of Mycoplasma pneumoniae-Induced Rash and Mucositis with Salivary Gland Inflammation in a Pediatric Patient: A Case Report
Abstract
:1. Introduction
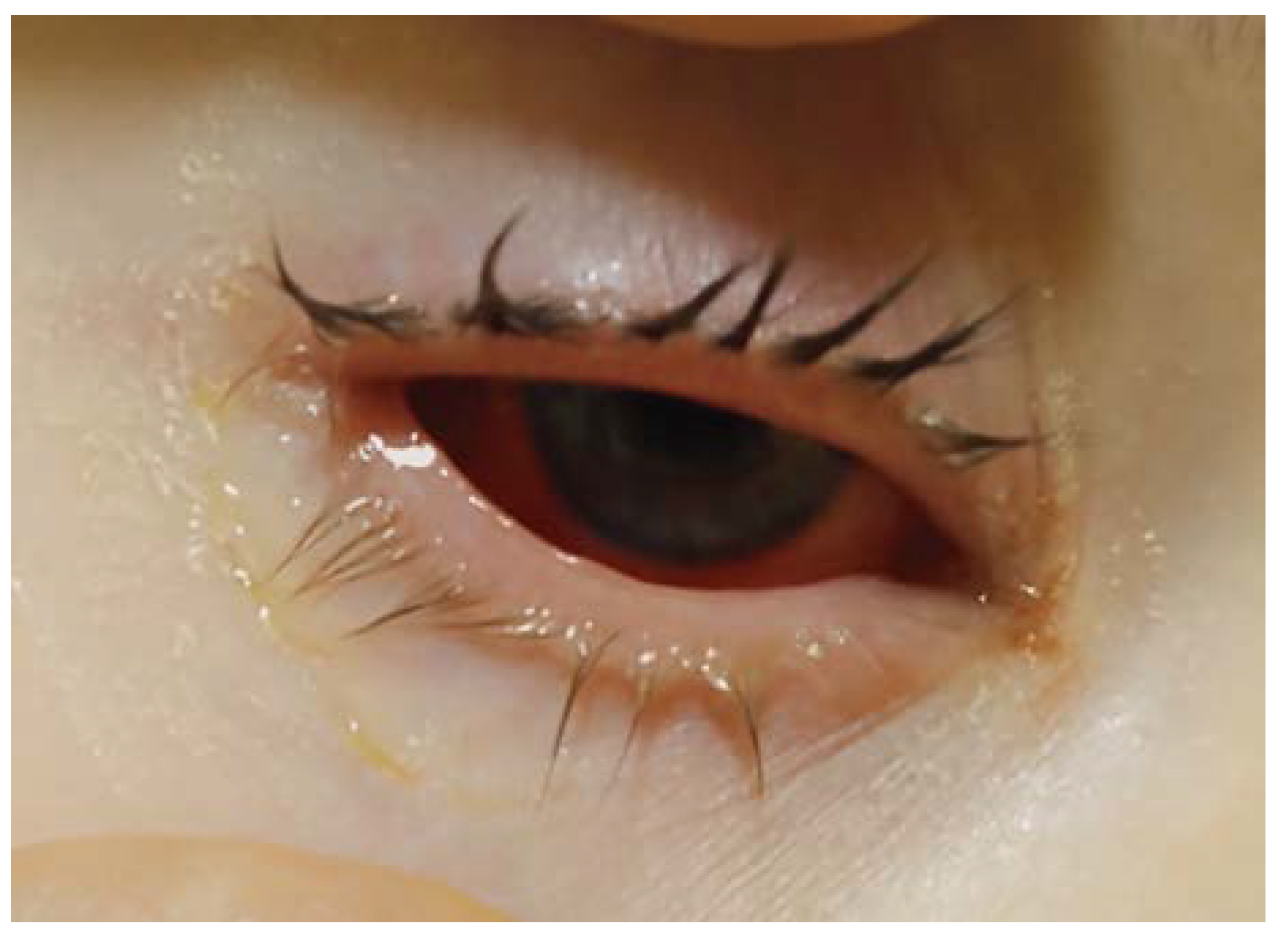
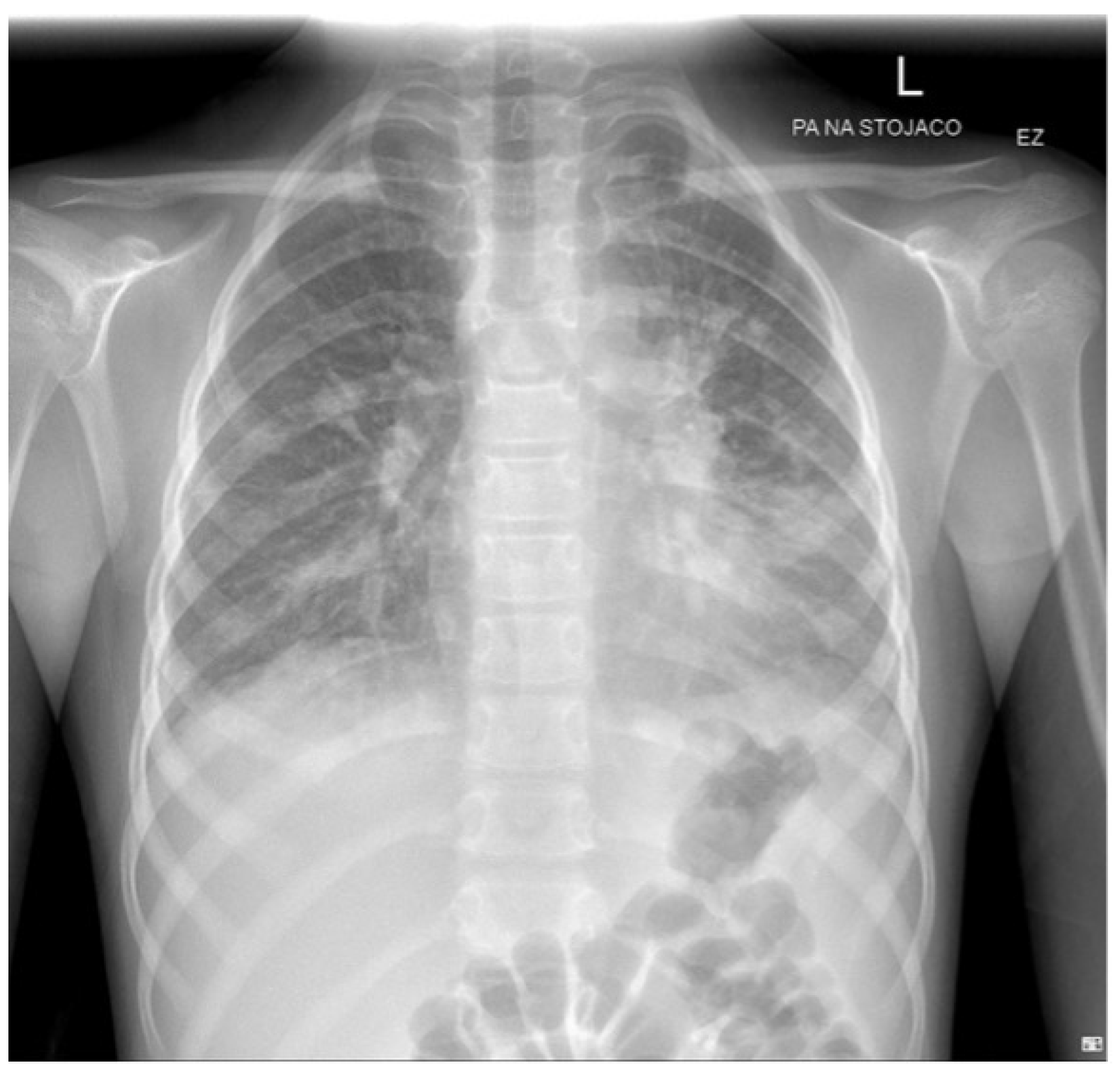
2. Case Report
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Song, H.; Huang, J.T.; Tan, J.K. Mycoplasma-induced Rash and Mucositis in a Father and Son: A Case Report. Pediatr. Infect. Dis. J. 2018, 37, E205–E206. [Google Scholar] [CrossRef] [PubMed]
- Meyer Sauteur, P.M.; Theiler, M.; Buettcher, M.; Seiler, M.; Weibel, L.; Berger, C. Frequency and Clinical Presentation of Mucocutaneous Disease Due to Mycoplasma pneumoniae Infection in Children with Community-Acquired Pneumonia. JAMA Dermatol. 2020, 156, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Canavan, T.N.; Mathes, E.F.; Frieden, I.; Shinkai, K. Mycoplasma pneumoniae-Induced Rash and Mucositis as a Syndrome Distinct from Stevens-Johnson Syndrome and Erythema Multiforme: A Systematic Review. J. Am. Acad. Dermatol. 2015, 72, 239–245.e4. [Google Scholar] [CrossRef] [PubMed]
- Ramien, M.L. Reactive Infectious Mucocutaneous Eruption: Mycoplasma pneumoniae-Induced Rash and Mucositis and Other Parainfectious Eruptions. Clin. Exp. Dermatol. 2021, 46, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Gámez-González, L.B.; Peña-Varela, C.; Ramírez-López, J.M.; Yamazaki-Nakashimada, M.A. Adenoviral-Induced Rash and Mucositis: Expanding the Spectrum of Reactive Infectious Mucocutaneous Eruption. Pediatr. Dermatol. 2021, 38, 306–308. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, Z.E.; Hussain, S.; Huang, J.T.; Delano, S. Reactive Infectious Mucocutaneous Eruption Associated With SARS-CoV-2 Infection. JAMA Dermatol. 2021, 157, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Ramien, M.L.; Bahubeshi, A.; Pope, E.; Eichenfield, L.; Lara-Corrales, I.; Nopper, A.J.; Shear, N. Redefining severe cutaneous reactions in children. In Proceedings of the Society for Pediatric Dermatology Annual Meeting, Junior Faculty Forum, Lake Tahoe, CA, USA, 13 July 2018. [Google Scholar]
- Lofgren, D.H.; Lenkeit, C.; Palanisamy, J.; Brown, J. Mycoplasma pneumoniae Induced Rash and Mucositis with Bilateral Otitis Media and Sinusitis. Cureus 2020, 12, e7449. [Google Scholar] [CrossRef]
- Lofgren, D.; Lenkeit, C. Mycoplasma pneumoniae-Induced Rash and Mucositis: A Systematic Review of the Literature. Spartan Med. Res. J. 2021, 6. [Google Scholar] [CrossRef]
- Waites, K.B.; Talkington, D.F. Mycoplasma pneumoniae and Its Role as a Human Pathogen. Clin. Microbiol. Rev. 2004, 17, 697–728. [Google Scholar] [CrossRef]
- Wrotek, A.; Robakiewicz, J.; Pawlik, K.; Rudzinski, P.; Pilarska, I.; Jaroń, A.; Imiełowska, A.; Jarzębowska, M.; Zabłocka, K.; Jackowska, T. The Etiology of Community-Acquired Pneumonia Correlates with Serum Inflammatory Markers in Children. J. Clin. Med. 2022, 11, 5506. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Wang, Y.; Sun, J.; Wang, W.; Hou, J.; Wang, X. Case Report: Clinical and Immunological Features of a Chinese Cohort With Mycoplasma-Induced Rash and Mucositis. Front. Pediatr. 2020, 8, 402. [Google Scholar] [CrossRef] [PubMed]
- Brodie, K.D.; Czechowicz, J.A.; Rosbe, K.W. Pediatric Sialendoscopy. Curr. Otorhinolaryngol. Rep. 2022, 10, 238–245. [Google Scholar] [CrossRef]
- Wray, W.; Scully, C.; Rennie, J.; Mason, D.K.; Love, W.C. Major and Minor Salivary Gland Swelling in Mycoplasma pneumoniae Infection. Br. Med. J. 1980, 1, 1421. [Google Scholar] [CrossRef] [PubMed]
- Rollins, P.D.; Prince, A.D.; Glick, M.; Biary, N. Severe Mycoplasma-Induced Rash and Mucositis Treated With IVIG. Clin. Pediatr. 2020, 59, 1097–1100. [Google Scholar] [CrossRef] [PubMed]
- Li, H.O.-Y.; Colantonio, S.; Ramien, M.L. Treatment of Mycoplasma pneumoniae-Induced Rash and Mucositis With Cyclosporine. J. Cutan. Med. Surg. 2019, 23, 608–612. [Google Scholar] [CrossRef] [PubMed]


| Diagnostic Criteria | Description |
|---|---|
| Minimal skin involvement | <10% of the total body surface area. Up to one-third of cases may have no skin lesions. |
| Vesiculobullous or diffuse atypical thyroid lesions | The rash can be scattered all over the body, often concentrated on the trunk, extremities, and face. Blisters may burst, leading to erosions and scabs. The eruptions can be painful and itchy. |
| Involvement of two or more mucosal sites | Includes inflammation of the mucous membranes of the mouth, conjunctiva, and genitals. |
| Clinical and laboratory evidence of atypical pneumonia | Clinical: fever, cough, auscultatory changes. |
| Laboratory: increase in IgM MP antibodies, MP in oropharyngeal or follicular cultures, PCR. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kucharek, I.; Bednarz, K.; Sybilski, A.J. Unique Presentation of Mycoplasma pneumoniae-Induced Rash and Mucositis with Salivary Gland Inflammation in a Pediatric Patient: A Case Report. J. Clin. Med. 2024, 13, 4587. https://doi.org/10.3390/jcm13164587
Kucharek I, Bednarz K, Sybilski AJ. Unique Presentation of Mycoplasma pneumoniae-Induced Rash and Mucositis with Salivary Gland Inflammation in a Pediatric Patient: A Case Report. Journal of Clinical Medicine. 2024; 13(16):4587. https://doi.org/10.3390/jcm13164587
Chicago/Turabian StyleKucharek, Izabela, Klaudia Bednarz, and Adam Jerzy Sybilski. 2024. "Unique Presentation of Mycoplasma pneumoniae-Induced Rash and Mucositis with Salivary Gland Inflammation in a Pediatric Patient: A Case Report" Journal of Clinical Medicine 13, no. 16: 4587. https://doi.org/10.3390/jcm13164587





