Abstract
Background/Objectives: This study aims to systematize the ability to use ROE to assess rhinoplasty outcomes in surgical approaches. Methods: The PubMed, Scopus, and Web of Science databases were searched for the following terms: “rhinoplasty and outcome” OR “prognosis” OR “outcomes” OR “satisfaction” OR “quality of life” OR QoL “rhinoplasty outcome evaluation”. The timeframe of the included studies is from 2011 to May 2024. Ultimately, 17 papers were included in the conducted meta-analysis of ROE scores between pre- and post-treatment data. Results The mean value of the pre-treatment ROE score was 33.50 with a CI of 29.46 to 37.53 (p < 0.001), while the post-treatment ROE was 69.60 with a CI of 63.07 to 76.14 (t ≤ 6 months). At t = 12 months it was 80.25 with a CI of 75.79 to 84.70 (p < 0.001). The mean difference between pre-treatment and post-treatment scores (t ≤ 6 months) was −36.31 with a CI of −40.93 to −31.69. The mean difference between pre-treatment and post-treatment scores for 6 m < t ≤ 12 m was −47.36 with a CI of −53.89 to −40.83. Conclusions: The result was statistically significant (p < 0.001).
1. Introduction
The nose is a distinctive facial feature of great aesthetic importance. As the central landmark of the face, its distance from other anatomical structures, dimensions, and symmetry directly affect the beauty of the face. It is crucial for the individual identity of any person. Among others, overall facial harmony and aesthetics hugely depends on the symmetry and spatial relations of the nose.
Rhinoplasty is one of the most common procedures performed in the plastic surgery/otolaryngology medical fields. The main indications are aesthetics and nasal obstruction [1]. According to the literature, rhinoplasty patients are less satisfied with the achieved results in comparison with those who underwent other facial plastic surgery procedures. Due to its aesthetic nature, having a great impact on the self-image and self-esteem of the patient, the assessment of the final rhinoplasty results should be made from the patients’ viewpoint [2]. Imposing criteria that determine aesthetics is not an easy task. For this reason, numerous questionnaires are available to evaluate quality-of-life change after the procedure (e.g., Rhinoplasty Outcome Evaluation, Sino-Nasal Outcome Test, Nasal Obstruction and Septoplasty Effectiveness Scale, and Standardized Cosmesis and Health Nasal Outcomes Survey) [3,4].
The ROE (Rhinoplasty Outcome Evaluation) is an easy-to-use questionnaire developed to assess the satisfaction and final results of rhinoplasty. It consists of six questions, two for each factor regarding the physical, emotional, and social dimensions of patient satisfaction. The author of the questionnaire took into account the main factors affecting a patient’s satisfaction with the surgery: physical, which examines the patient’s satisfaction with the shape and function of the nose; emotional, which assesses the level of self-confidence and willingness to change appearance; and the social factor, which assesses social, professional, and family acceptance. Since its creation, it has been translated into many languages and popularized as an evaluation method [5,6].
In this meta-analysis, we aim to systematize the ability of the ROE to assess rhinoplasty outcomes in surgical approaches.
2. Materials and Methods
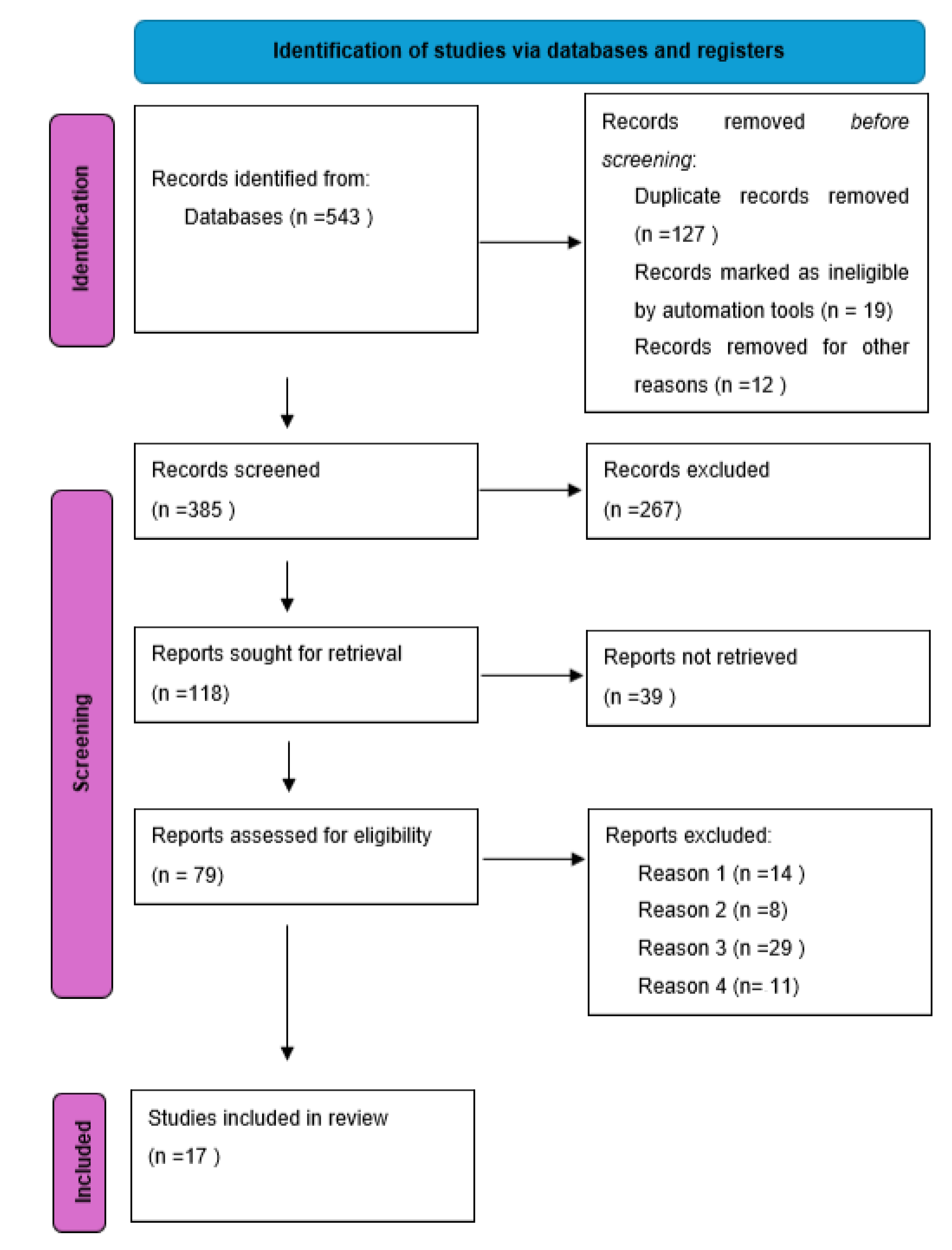
Studies included in this research were selected during a systematic search of literature in databases such as Scopus, Web of Science, and PubMed. The pool of studies was narrowed down to papers published from January 2017 to July 2023. The screening of the results was based on the phrases: “rhinoplasty and outcome” OR “prognosis” OR “outcomes” OR “satisfaction” OR “quality of life” OR QoL “rhinoplasty outcome evaluation”. The search was performed in abstracts and full texts. Two reviewers, the first and the third authors of this article, assessed each abstract and full text for potential inclusion and reached a consensus for the articles to be included in the final review. The articles were excluded if they: (1) were written in any language other than English, (2) did not evaluate the patients’ satisfaction and quality of life or (3) used a scale different than the Rhinoplasty Outcome Evaluation (ROE) for the evaluation of the quality of life (QoL) and patients’ satisfaction, or (4) did not report results as the mean and standard deviation. Seventeen articles were taken into account after repetitive papers were eliminated [7,8,9,10,11,12,13,14,15,16,17,18]. (Chart 1).
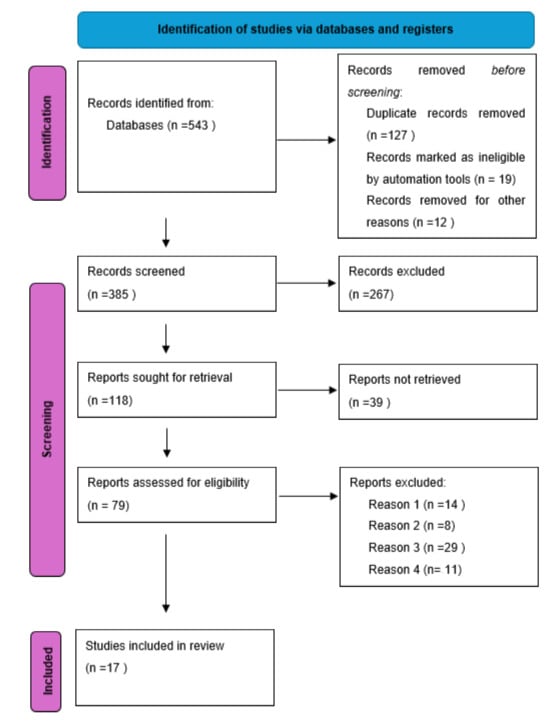
Chart 1.
Flow chart for inclusion of articles.
2.1. Study Selection
The systematic review was conducted using the PRISMA guidelines [19]. The detailed requirements are listed below:
- -
- Inclusion criteria: original, prospective, or retrospective articles concerning rhinoplasty with ROE scores, human subject studies published in English, adults, and studies published up to and inclusive of July 2023;
- -
- Exclusion criteria: article types such as case reports, editorials, letters, books, and conference papers; papers in which the results were presented as the mean without the standard deviation, or the median and range, or the median range and interquartile range; or studies with the ROE expressed as graphs, without values.
2.2. Data Extraction
The following data were extracted from each study: the authors, year of publication, number of participants, sex of participants, entry age, Rhinoplasty Outcome Evaluation scores before and after rhinoplasty, the duration of follow-up, presenting deformity, technique used, and the study site.
2.3. Statistical Analysis
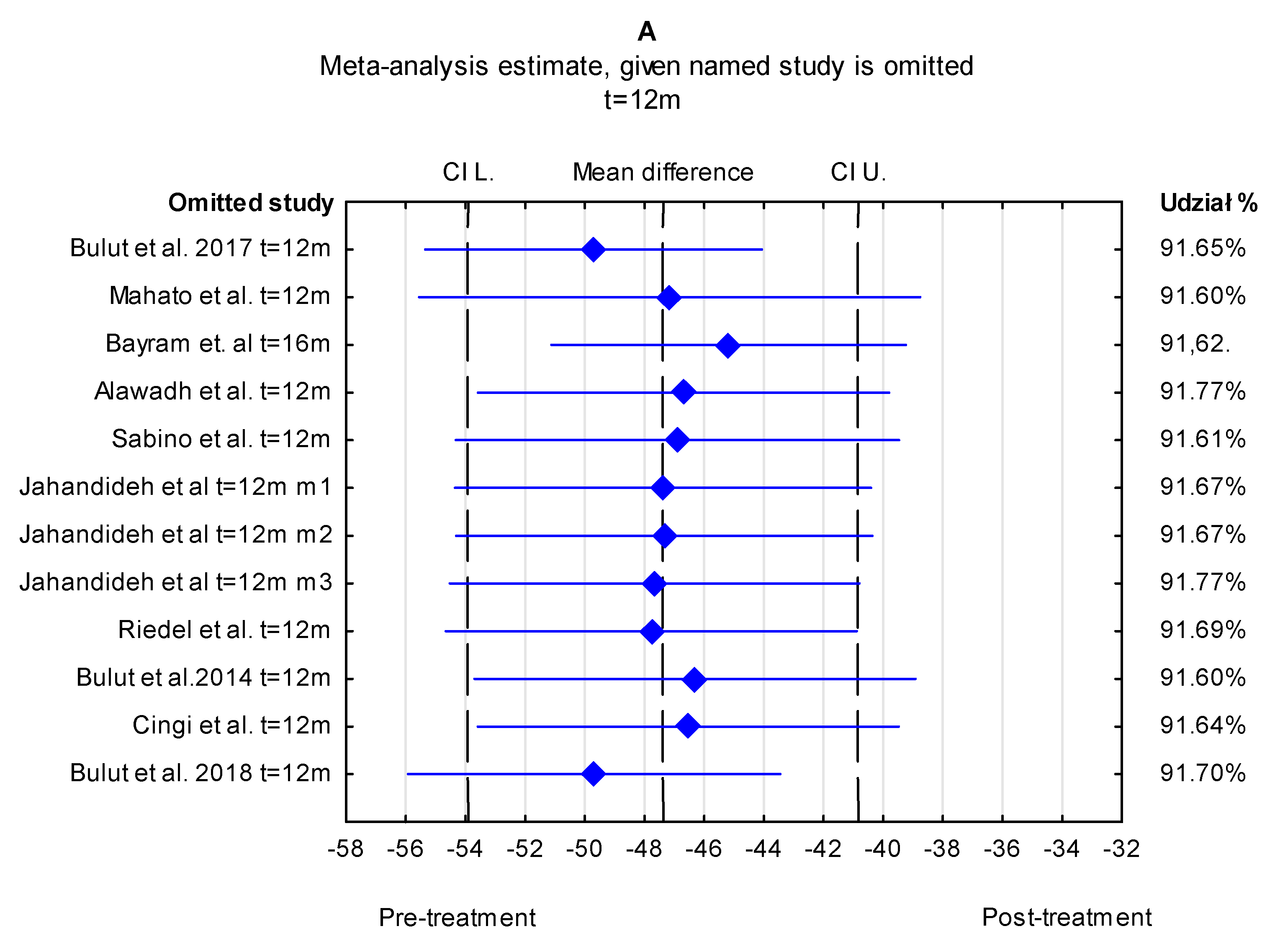
Statistical analysis was conducted using Statistics 13 (Dell Software Inc., StatSoft Warsaw, Poland). The Q test was used to test heterogeneity, and the I2 statistic was carried out to quantify and evaluate heterogeneity. The I2 values ranged from 0 to 100% with higher values indicating greater heterogeneity (25–50%—low, 50–75%—moderate, and >75%—high). Since in all the conducted analysis, heterogeneity scores exceeded 75%, the analysis was performed using a random effects model, and the standardized mean difference was provided with 95% confidence intervals (95% CI). The results were as follows: 99.14% (95% CI of 99.00% to 99.26%) in pre-treatment ROE scores, 99.51% (95% CI of 99.42% to 99.59%) in pre-treatment vs. post-treatment t ≤ 6 months, 99.58% (95% CI of 99.50% to 99.64%) in pre-treatment vs. post-treatment 6 m < t ≤ 12 m, 99.50% (95% CI of 99.40% to 99.58%) in post-treatment t ≤ 6 months, and 99.53% (95% CI of 99.44% to 99.60%) in post-treatment 6 months < t ≤ 12 months. Forest plots were generated to describe the change in Rhinoplasty Outcome Evaluation scores before and after rhinoplasty based on the duration of follow-up (≤6 months, and ≥12 months). To assess publication bias, Egger’s test and Begg’s test were performed. To assess the stability of the results, sensitivity analysis was conducted by excluding each study at a time (Figure 1). Moreover, the trim-and-fill method for publication bias was performed to estimate potentially missing studies.
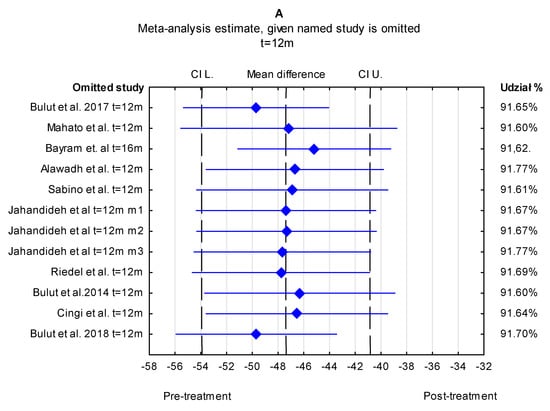
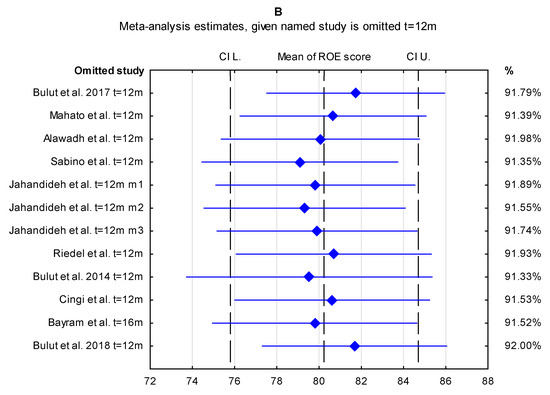
Figure 1.
Sensitivity analysis for the effect of individual studies (given named study in the Y axis is omitted) on the pooled differences of ROE score. CI (confidence interval). (A) pre-treatment vs. post-treatment t = 12 m, (B) mean value of ROE score t = 12 m.
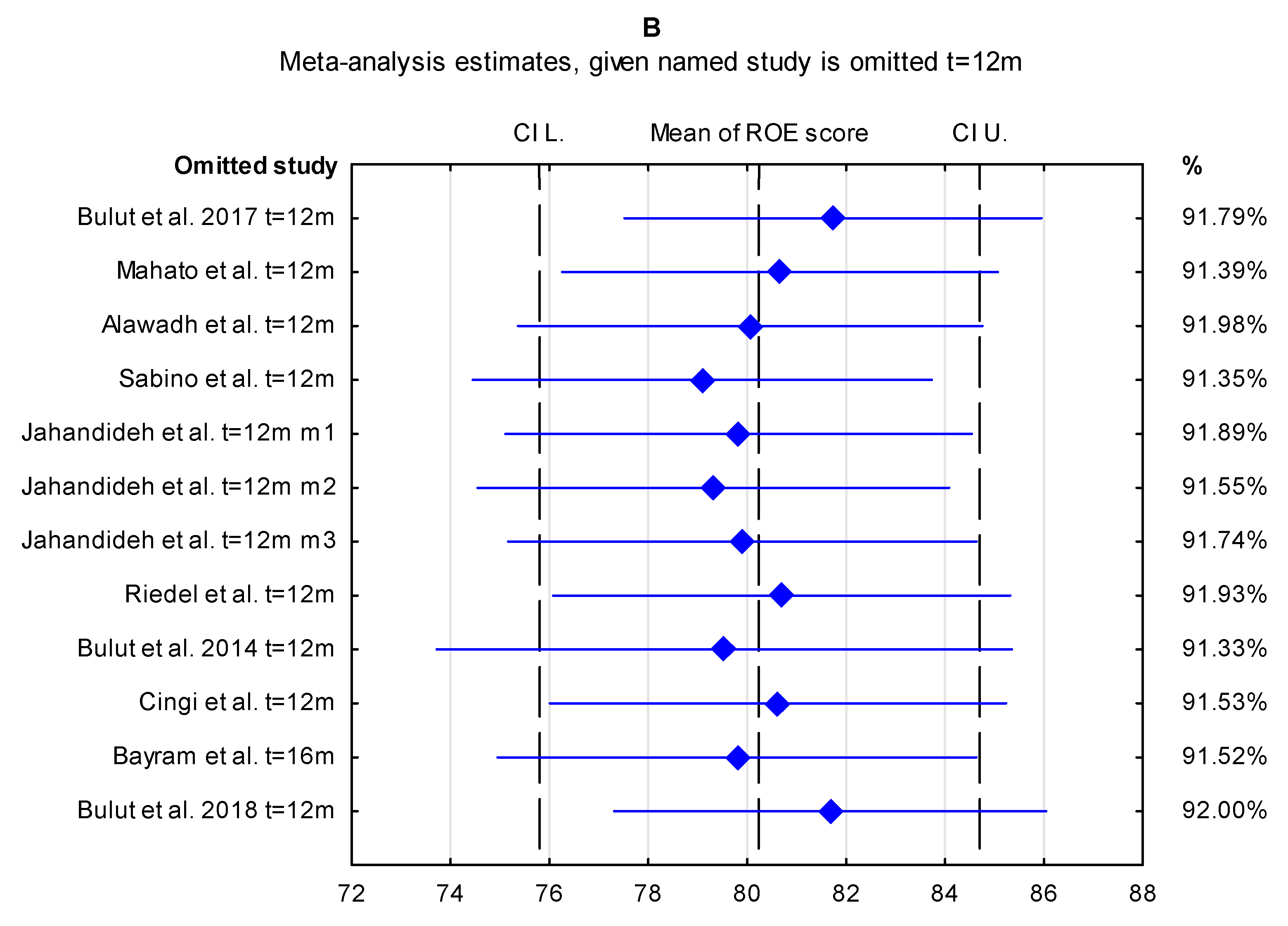
3. Results
As regards the eleven included papers, the mean pre-treatment ROE score was 33.50 with a CI of 29.46 to 37.53 (Figure 2). The result was statistically significant.
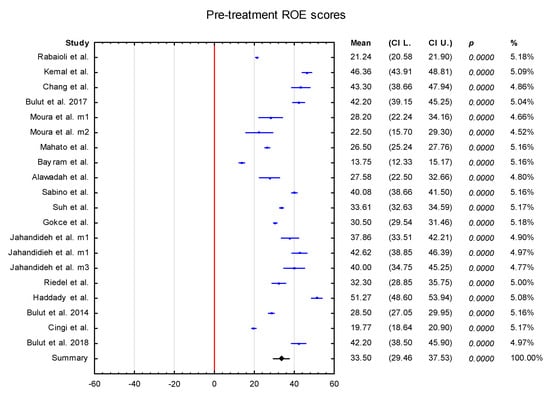
Figure 2.
The pre-treatment ROE scores.
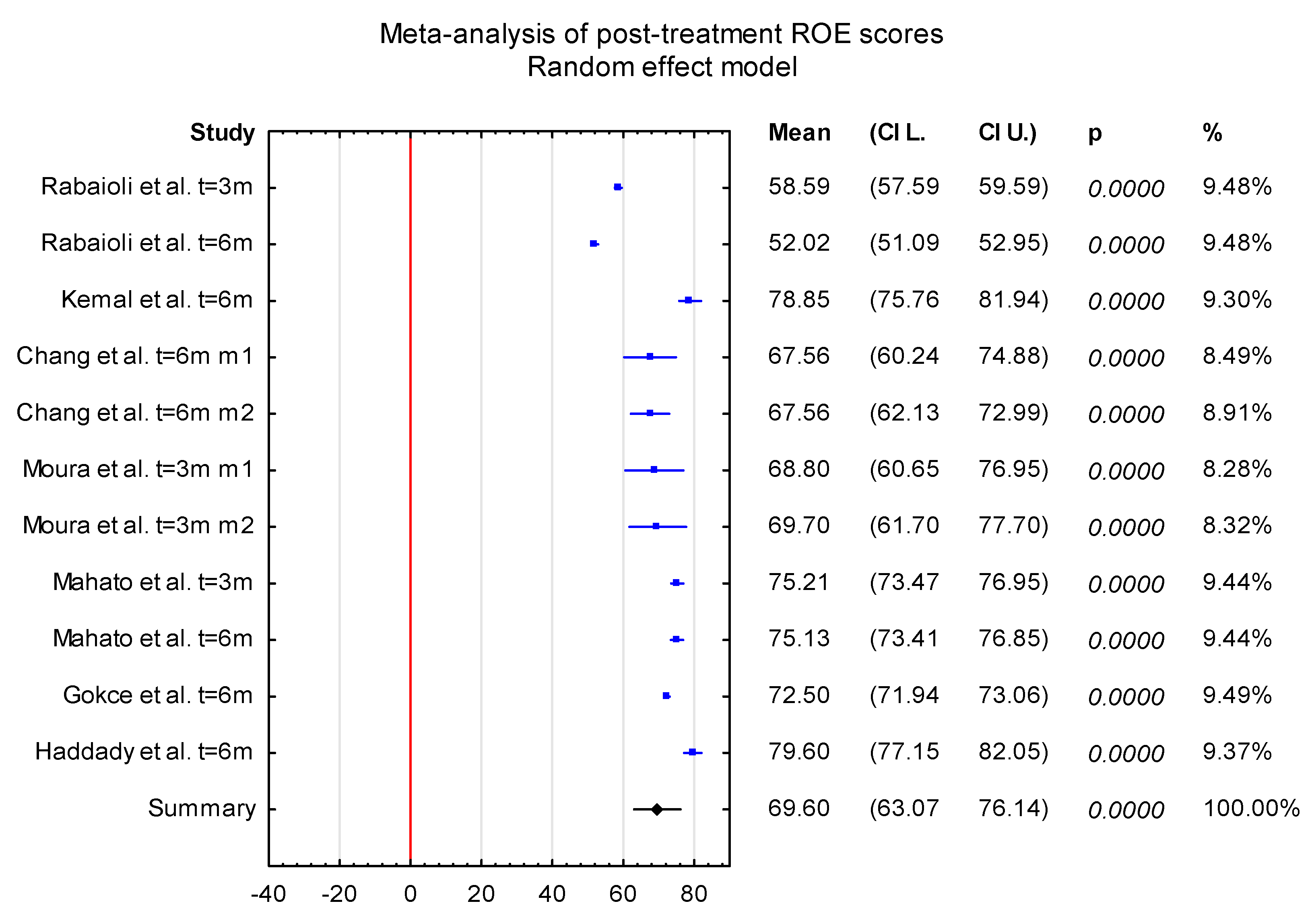
The mean post-treatment ROE score (t ≤ 6 months) was 69.60 with a CI of 63.074 to 76.14. The result was statistically significant (Figure 3).
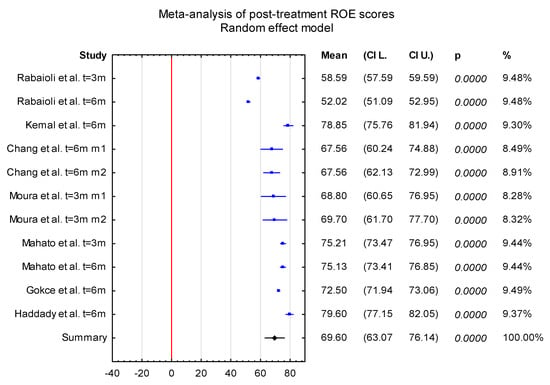
Figure 3.
The post-treatment ROE scores (t ≤ 6 months).
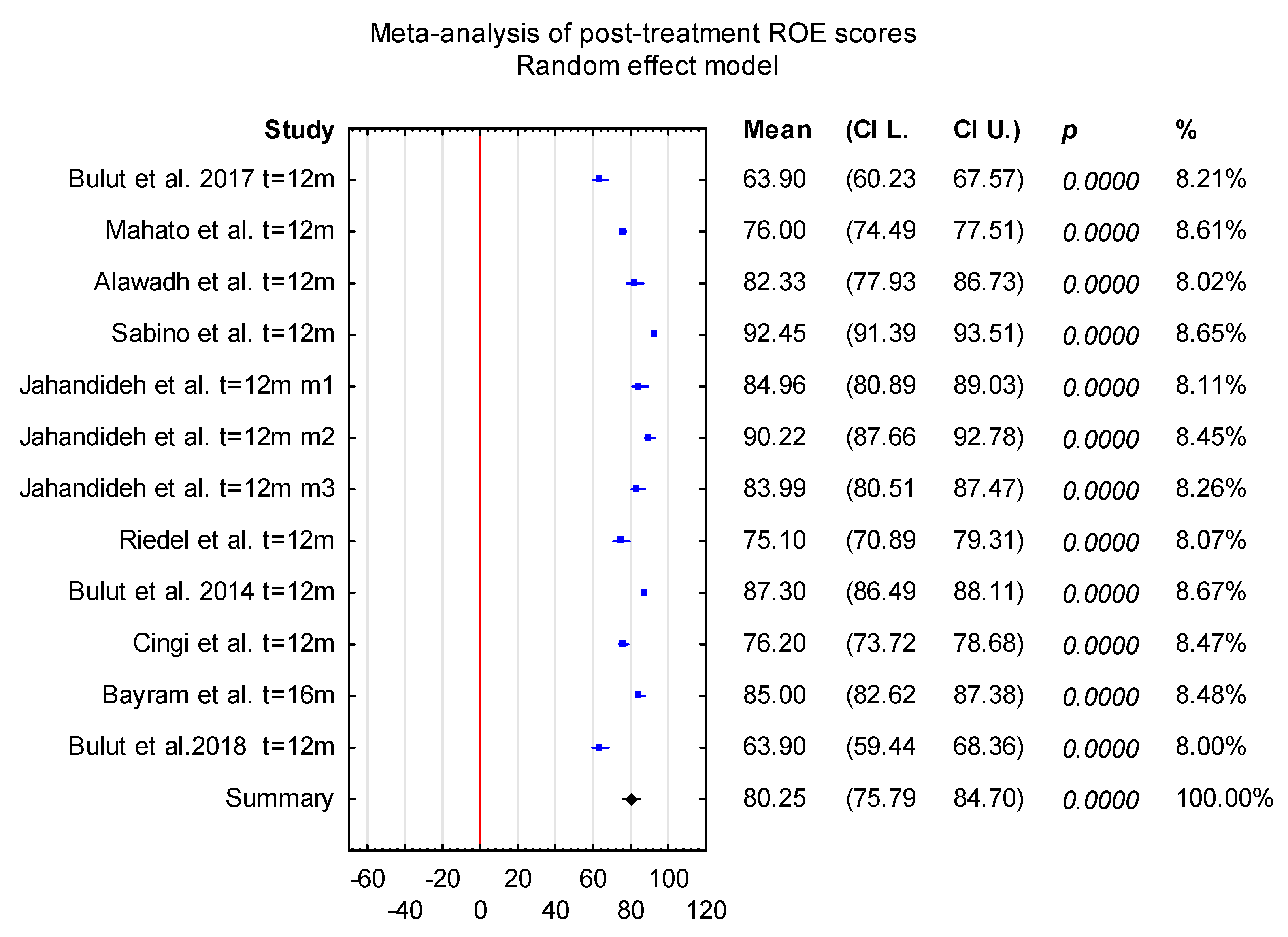
The mean post-treatment ROE score (t = 12 months) was 80.25 with a CI of 75.79 to 84.70. The result was statistically significant (Figure 4).
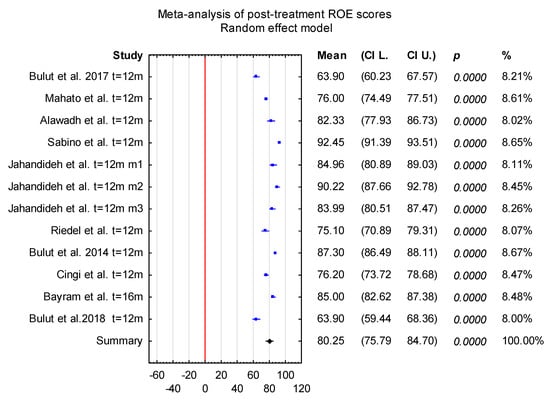
Figure 4.
The post-treatment ROE scores (t = 12 months).
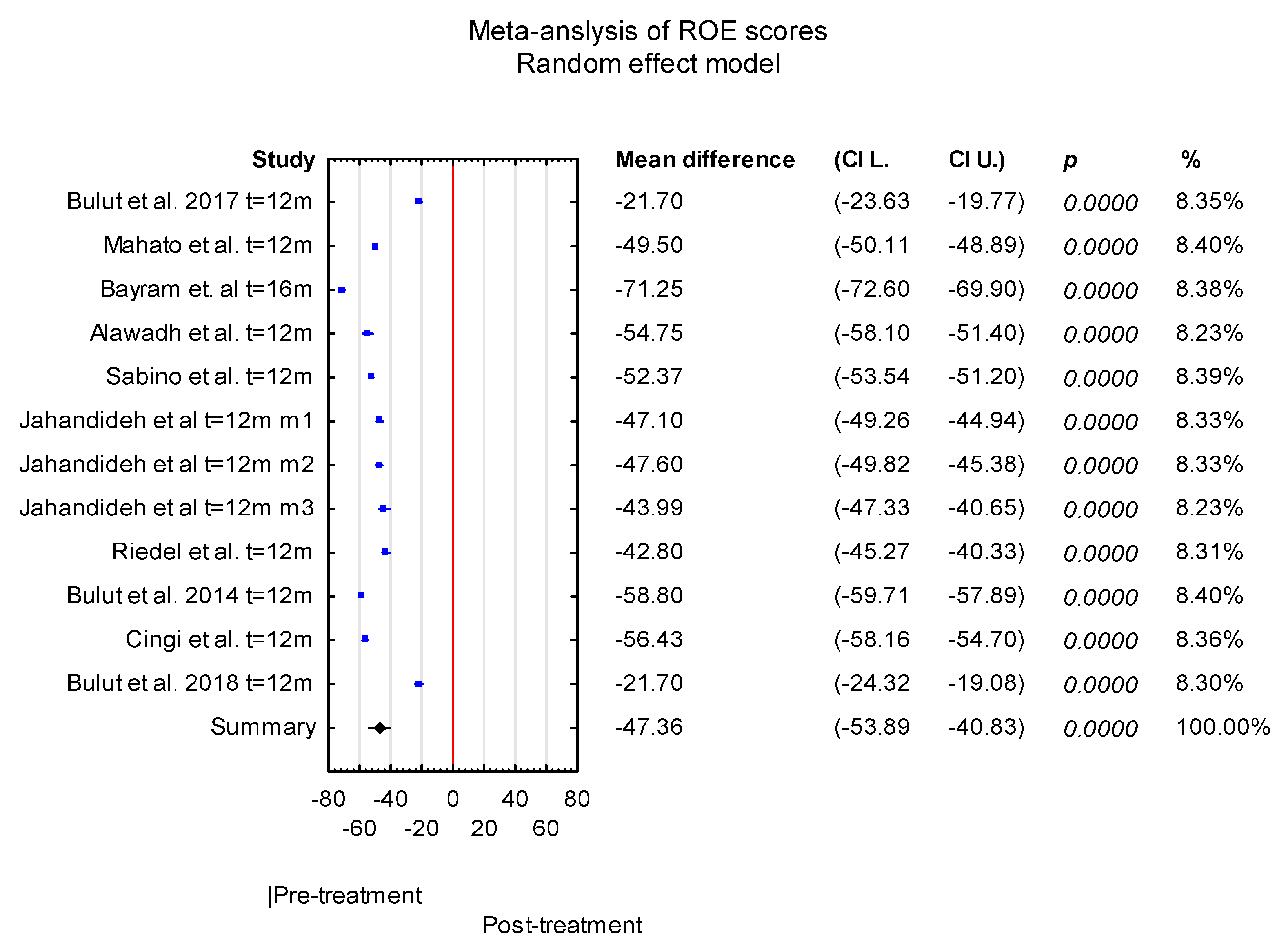
The mean difference between pre-treatment and post-treatment scores (6 months < t ≤ 12 months) was −47.36 with a CI of −53.89 to −40.83. The result was statistically significant (p < 0.001) (Figure 5).
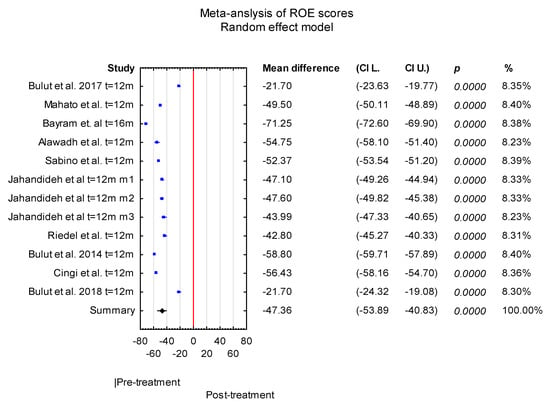
Figure 5.
The difference between pre-treatment and post-treatment scores 6 months < t ≤ 12 months.
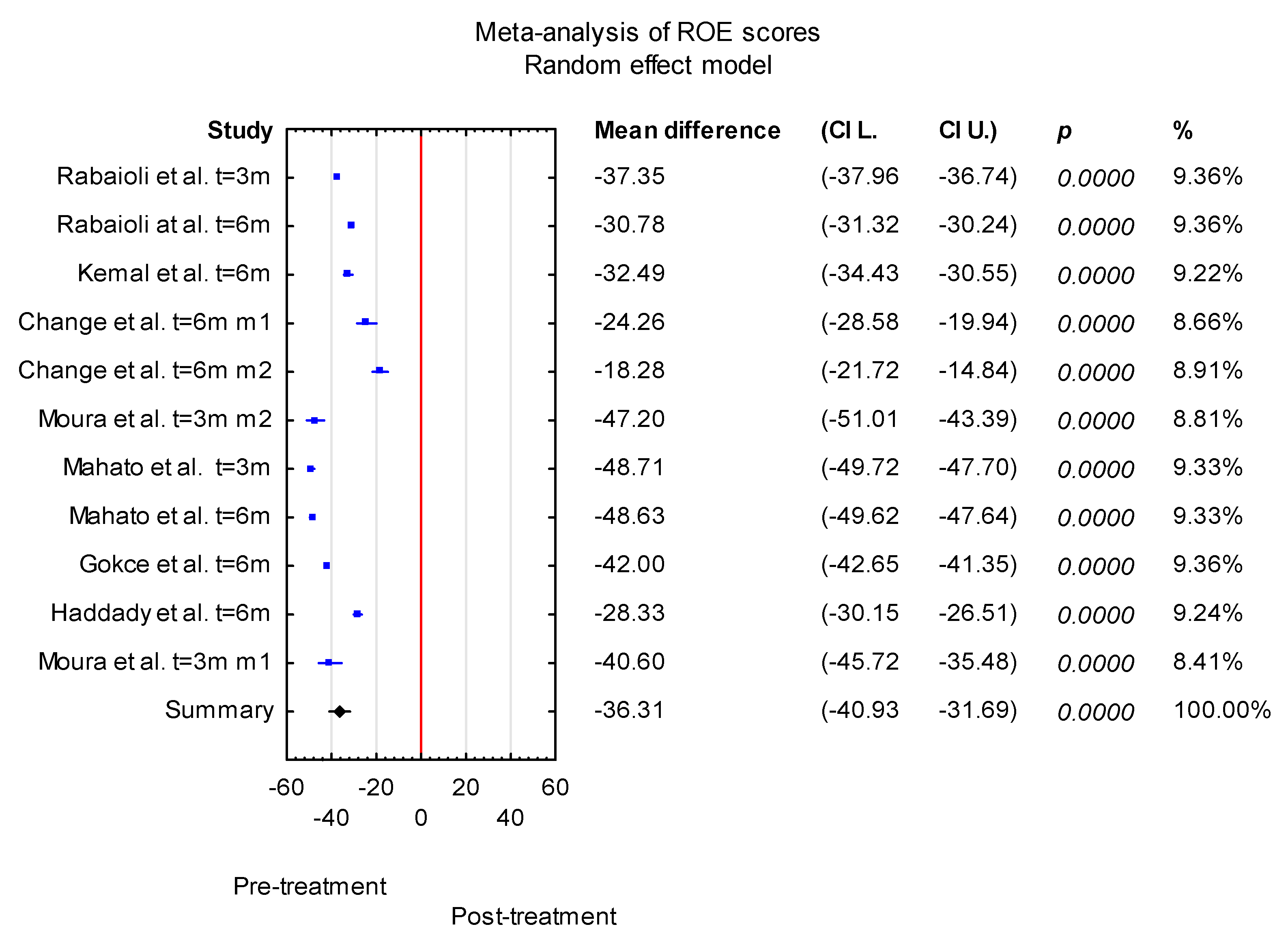
The mean difference between pre-treatment and post-treatment scores for 0 m < t ≤ 6 m was −36.31 with a CI of −40.93 to −31.69. The result was statistically significant (p < 0.001) (Figure 6).
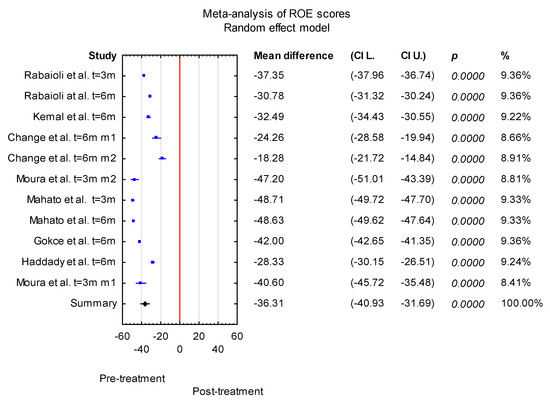
Figure 6.
The difference between pre-treatment and post-treatment scores for 0 m < t ≤ 6 m.
Overall, the forest plot for the pre-treatment vs. post-treatment results revealed that the studies denoted a higher value of ROE scores after treatment, and the increase was statistically significant in each case. However, there were differences among the included studies.
An Egger’s publication bias was generated. The results of Egger’s test (p = 0.535 pre-treatment, p = 0.123 post-treatment t = 3 m and 6 m, p = 0.068 post-treatment t = 12, and p = 0.367 pre-treatment vs. post-treatment t = 12 m) indicated a minimal potential risk of publication bias, which was also consistent with the Begg’s test results.
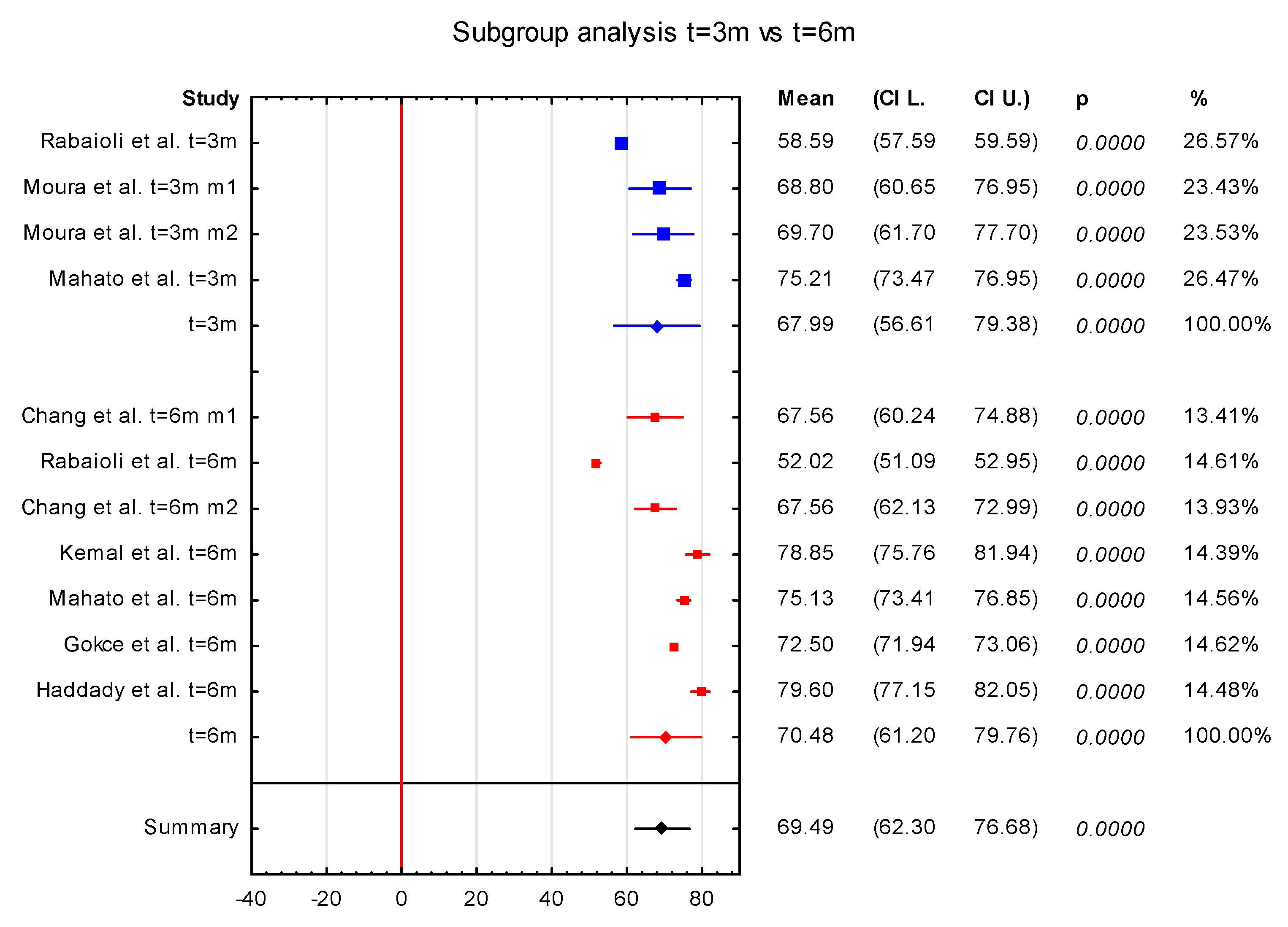
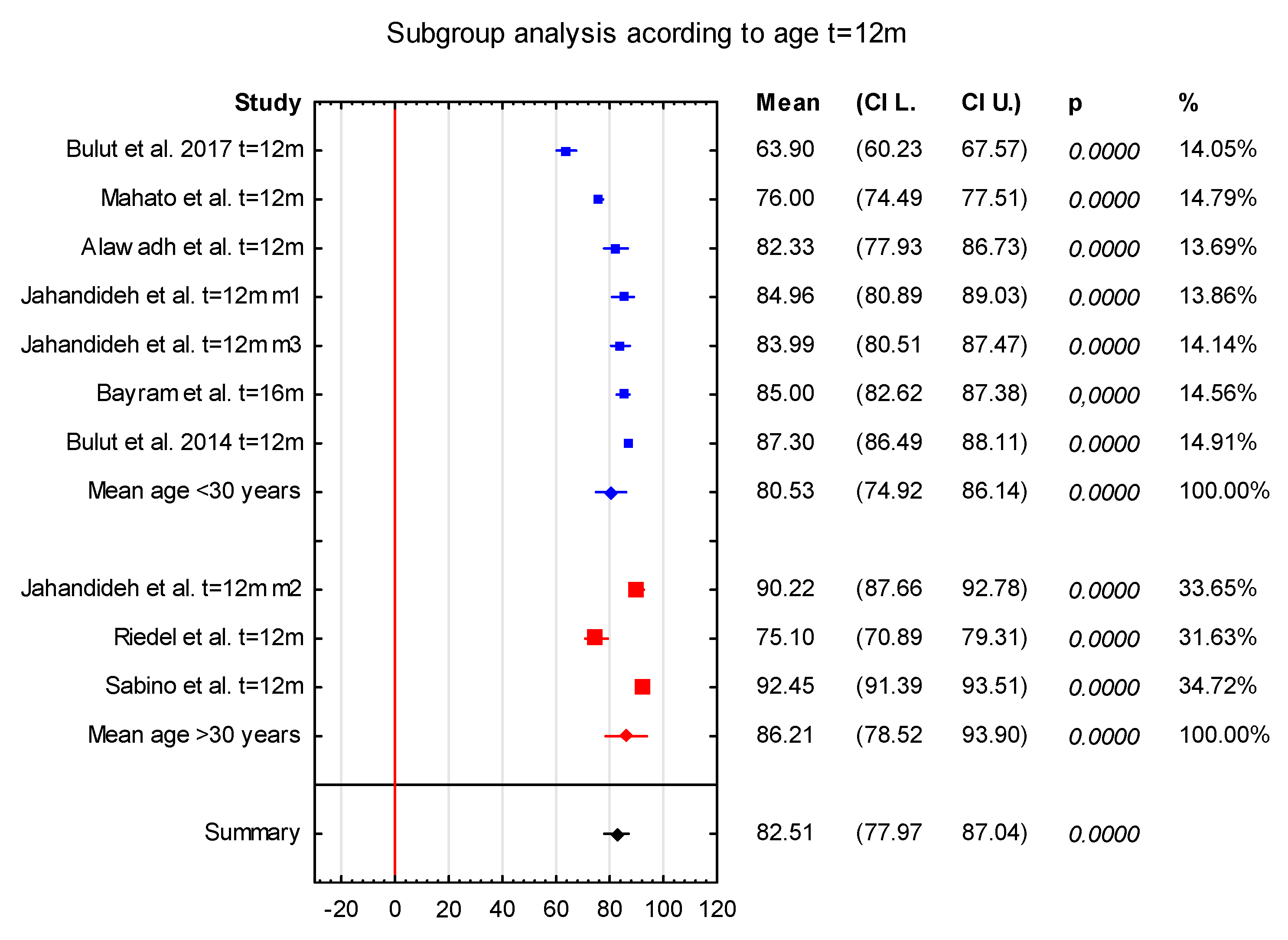
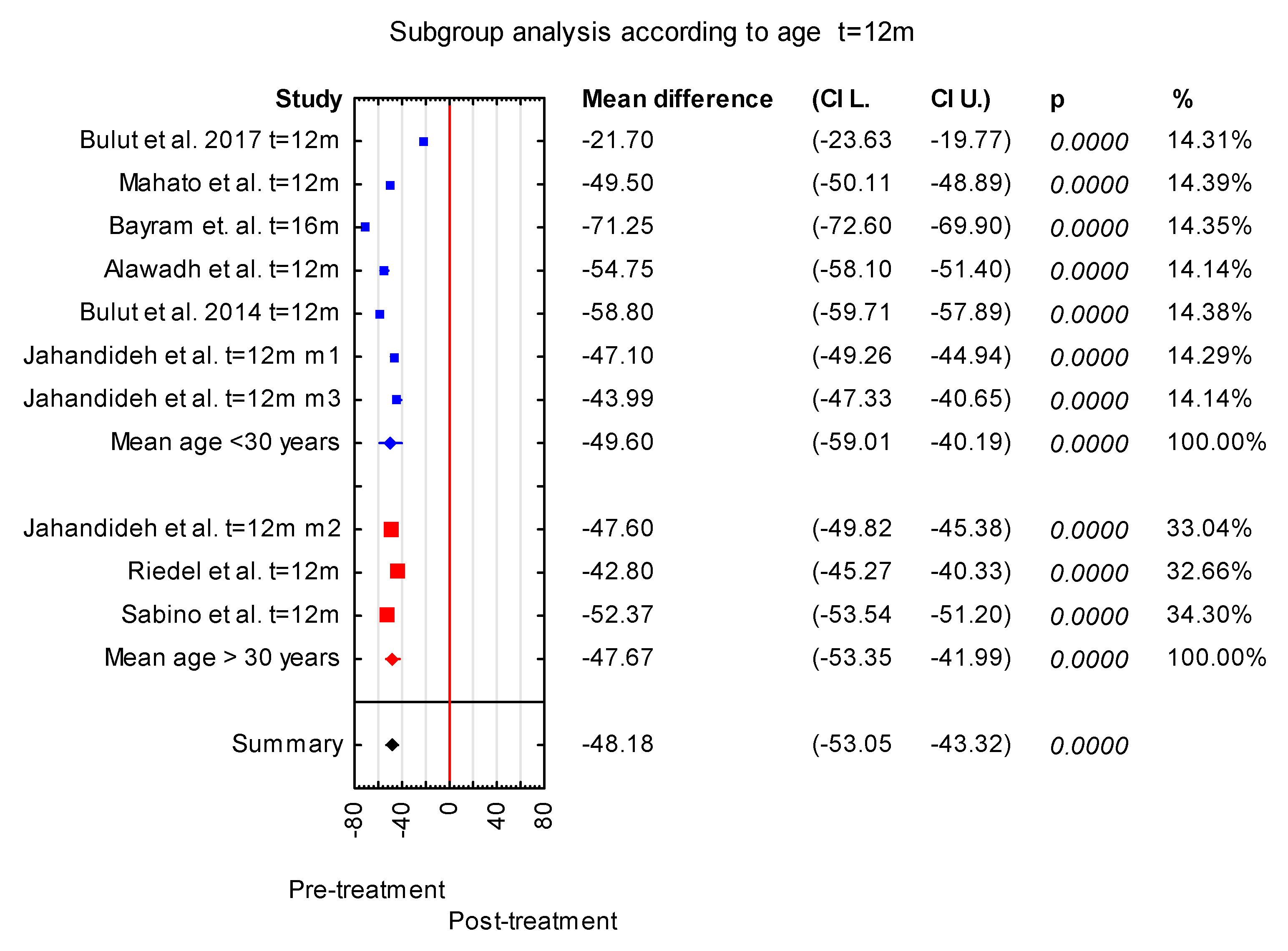
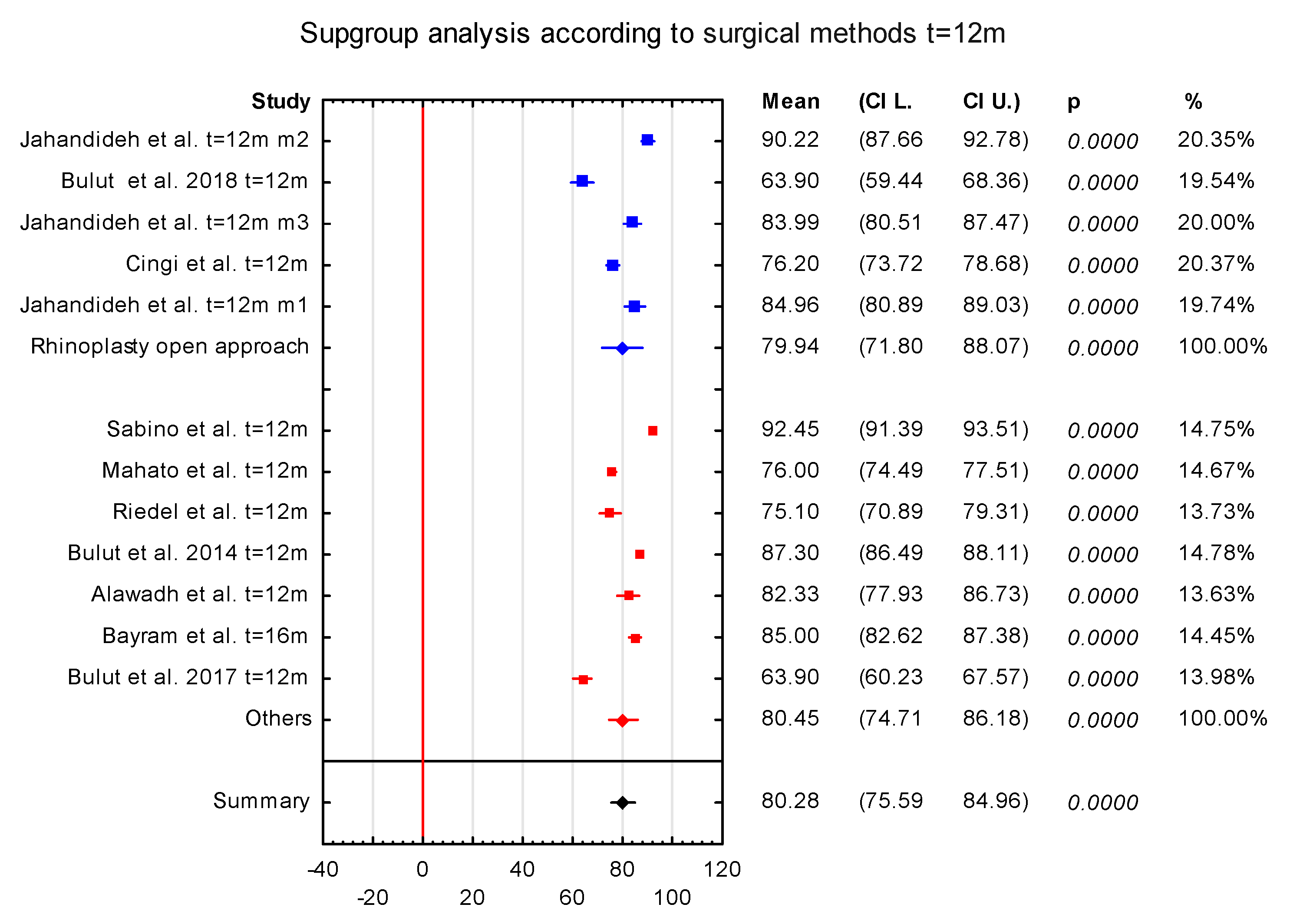
3.1. The Subgroup Analysis
Since the heterogeneity among studies was high, a subgroup analysis was performed to try to find possible reasons for the variability of the results. The different time of grading of postoperative follow-up processes (3 months or 6 months), age (age < 30 years and age > 30 years), and surgical methods (rhinoplasty open approach vs. others) for time t = 12 m were considered for the subgroup analysis. In four publications that were included in the meta-analysis, results of the ROE were given 3 months after the procedure, and in seven publications the results were given after 6 months. Statistically significant results were received for the two subgroups (Figure 7 and Figure 8). Moreover, to conduct subgroup analysis for t = 12 m according to age, the considered publications were divided into two groups, patients with mean age lower than 30 years (group 1) and mean age higher than 30 years (group 2). For this division, the papers by Cingi et al. and Bulut et al. were excluded, as the mean age of the group of patients was not given [20,21]. In seven publications, the mean age of the group of patients was lower than 30 years, and in three it was higher than 30 years. Statistically significant results were received for the two subgroups (Figure 9 and Figure 10). Then, papers were divided according to surgical methods; five publications included open-approach rhinoplasty, while in the other eight involved other techniques. Statistically significant results were received for the two subgroups (Figure 11). However, it is important to note that for each case of division one of the subgroup analyses contained only three studies; thus, the true effect is difficult to establish.
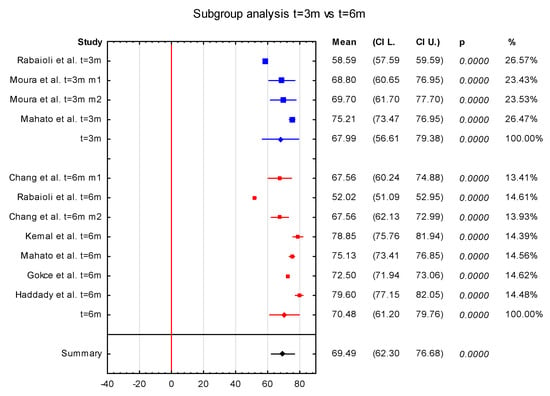
Figure 7.
The subgroup analysis for follow-up time.
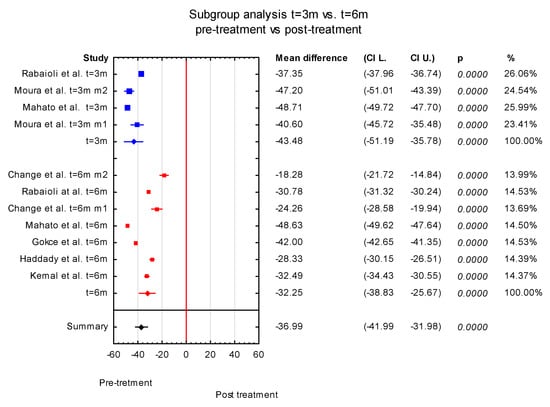
Figure 8.
The subgroup analysis of difference between pre-treatment and post-treatment (3 months and 6 months).
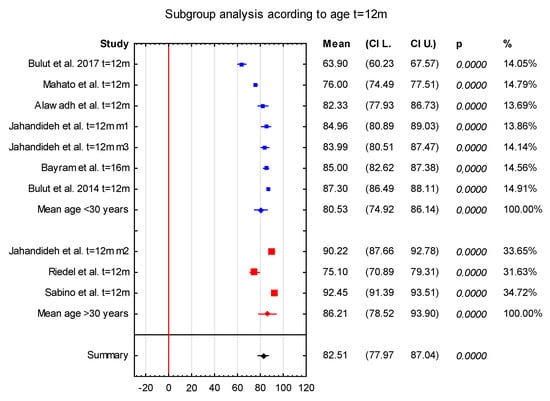
Figure 9.
The subgroup analysis t = 12 m according to age groups.
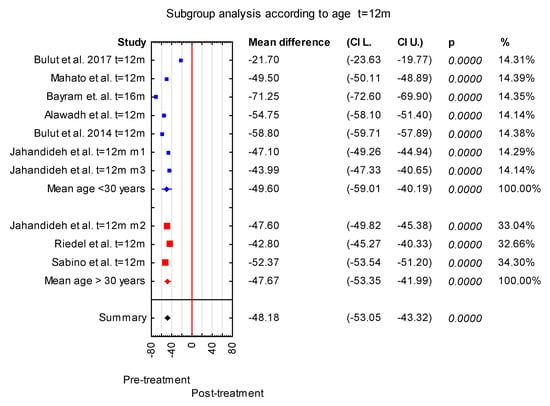
Figure 10.
The subgroup analysis of difference between pre-treatment and post-t = 12 m according to age group.
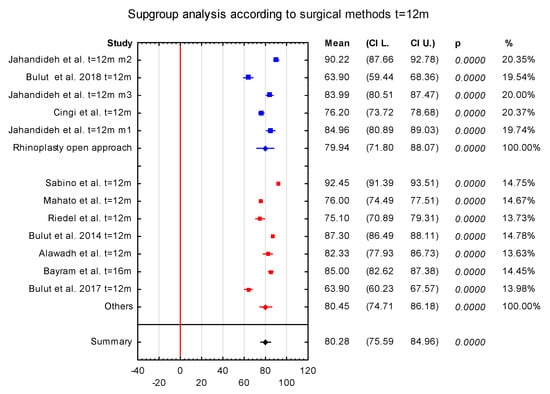
Figure 11.
The subgroup analysis t = 12 m according to surgical methods.
The subgroup analysis was also performed in case of mean difference between pre-treatment and post-treatment (3 months and 6 months). Here, we also received statistically significant results for the two subgroups (Figure 8).
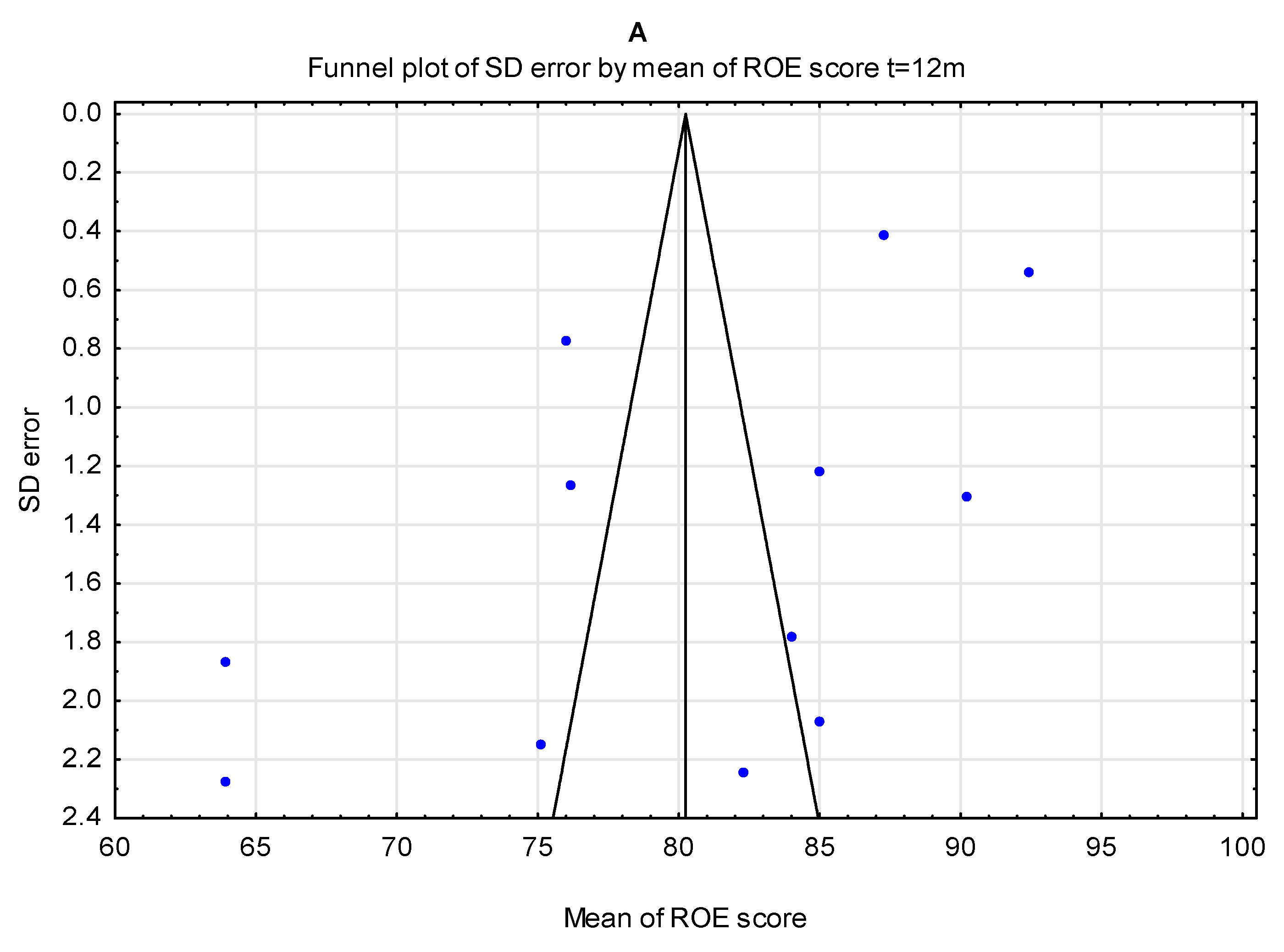
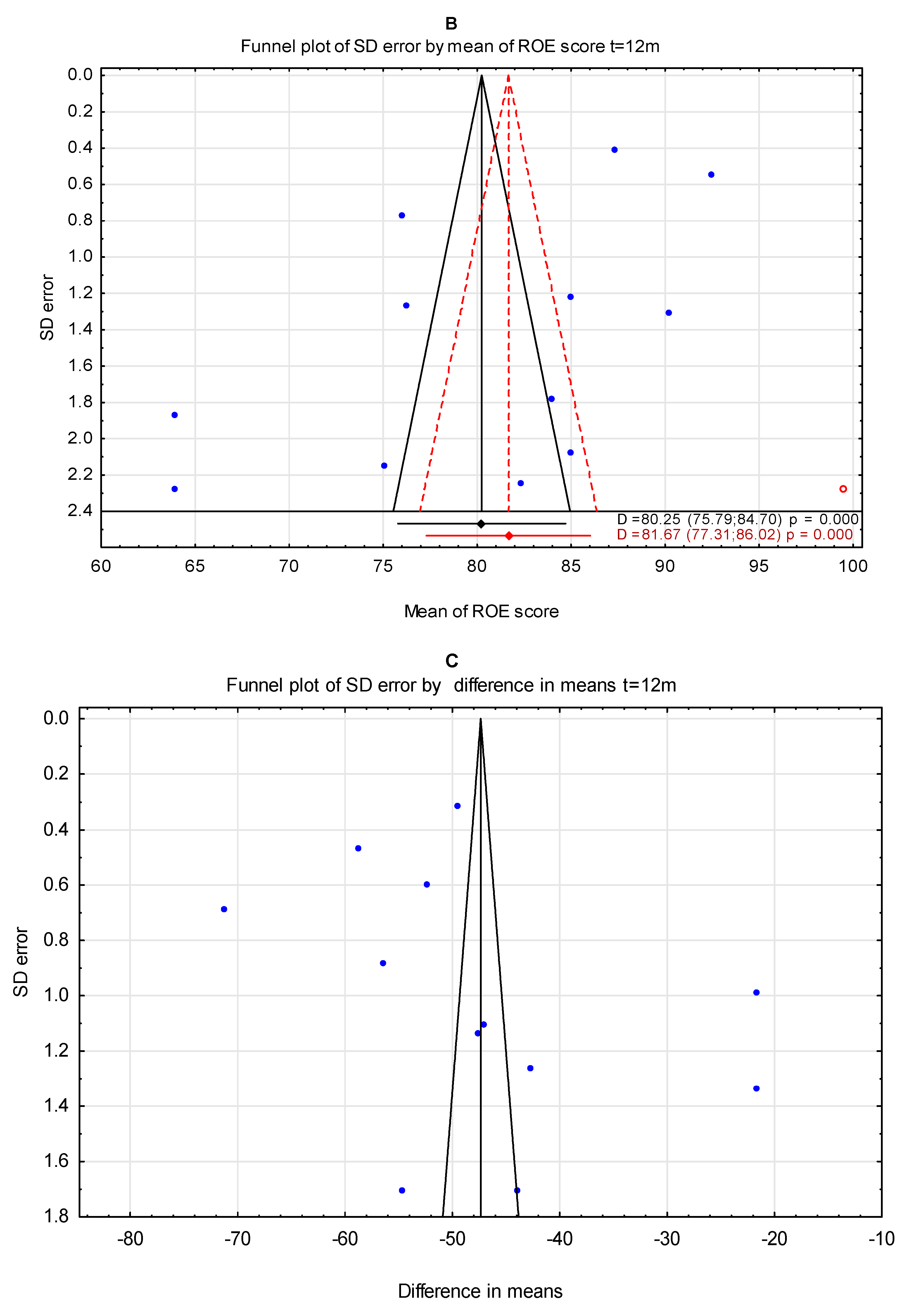
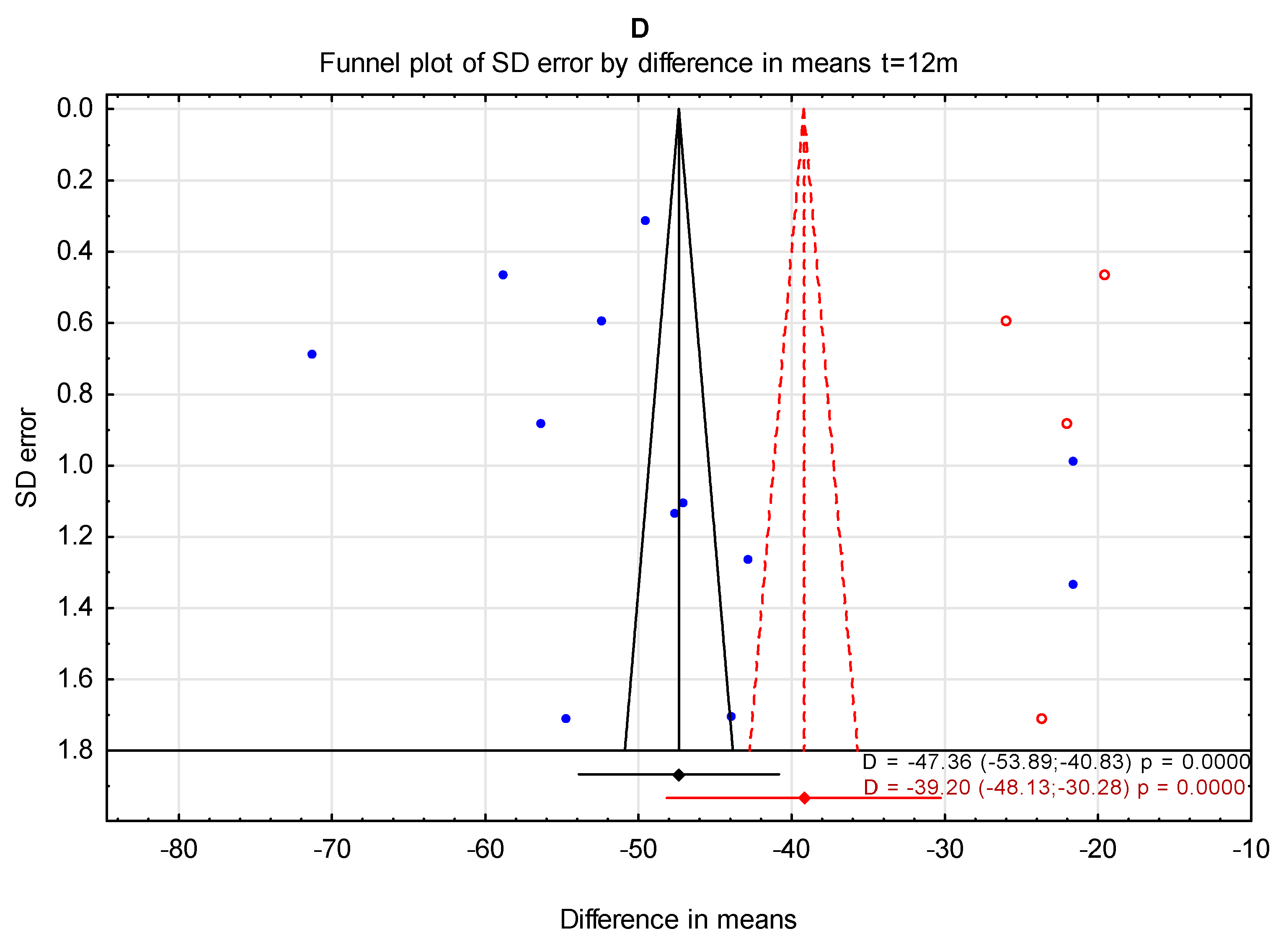
3.2. The Trim-and-Fill Method
The trim-and-fill method was used to estimate the effect of potentially missing studies due to publication bias in the funnel plot for mean post-treatment ROE score and mean difference pre-treatment vs. post-treatment ROE score after t = 12 m. In the case of mean post-treatment ROE score, the received value was 81.67 (95% confidence interval from 77.31 to 86.02), and for pre-treatment vs. post-treatment the value was −39.20 (95% confidence interval from −48.13 to −30.26) (Figure 12).
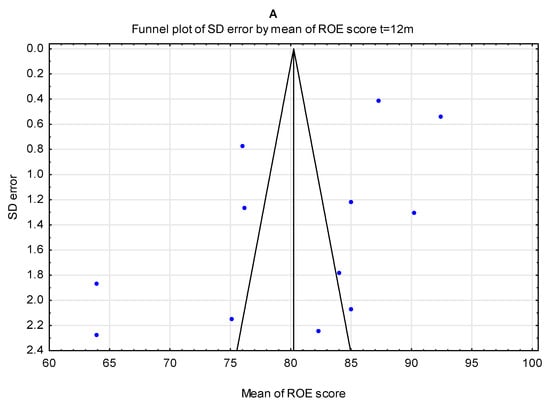
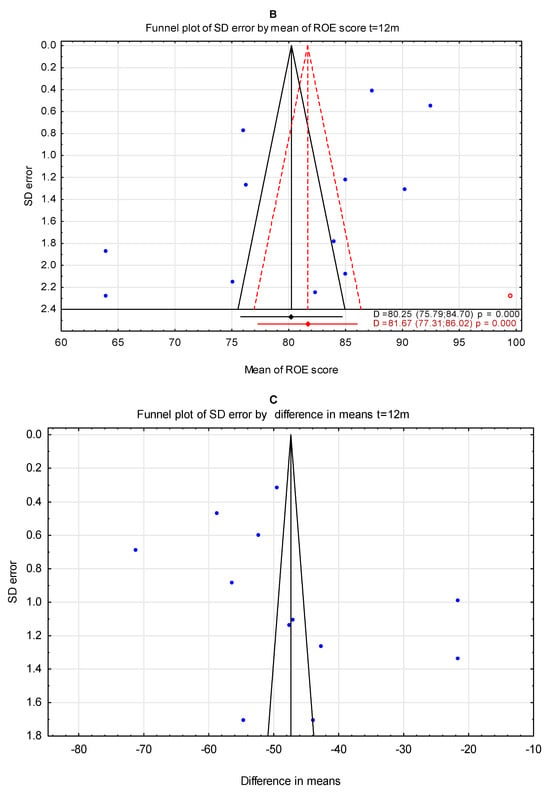
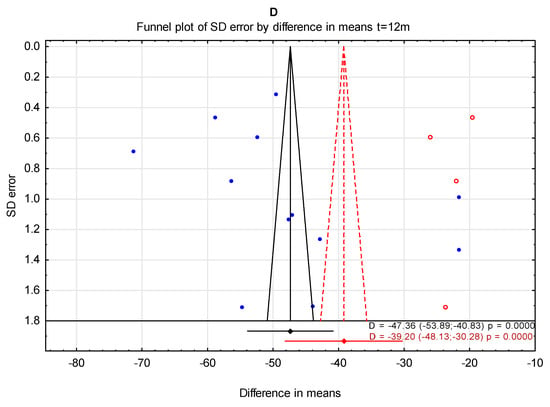
Figure 12.
Funnel plots before (A,C) and after (B,D) applying the trim-and-fill method; imputed missing studies (red dots) t = 12 m.
4. Discussion
Nasal physiology is a complex subject. The nose, as a complex structure, is a sensory organ participating in breathing as well as olfaction. Both of these functions are reliant on nasal airflow, which must be considered during mid-face surgical procedures [2,22]. Therefore, disorders of the nose affect not only its external appearance but also the inside of the nose, which may pose a real challenge for surgeons.
Rhinoplasty is a procedure whose aim is to address two aspects: achieving aesthetic goals with the simultaneous maintenance or improvement of nasal airway function. It is a complex surgery, so it has to involve a careful evaluation of overall facial symmetry, bones, and cartilage that create unique anatomy; it must consider issues such as external nasal deformity, septal deviation, turbinate hypertrophy, and nasal tip ptosis. Many patients with nasal deviation are unaware of any inherent facial asymmetries. Recognizing and discussing the interrelation between the deviated nose and asymmetry is an important factor taken into consideration before surgery [1]. The knowledge and understanding of nasal anatomy are therefore necessary for successful nasal reconstruction [22].
Rhinoplasty is one of the most complex surgeries that has been developing globally in the last decade. For example, over 200,000 nose reshaping surgeries were performed in the United States in 2018 [23,24]. Anco et al., in the study Preservation Rhinoplasty: A New Approach to Mestizo Noses, state that rhinoplasty is the fourth most requested procedure worldwide [25]. As mentioned above, the aim of a well-received nasal reconstruction is to achieve aesthetic goals while maintaining or improving nasal airway function. Rhinoseptoplasty has changed significantly since the first aesthetic nose surgery was performed. A great variety of surgical techniques and approaches are available [26]. In the pursuit of better and more consistent results, the reduction-only concept in nasal surgery has gradually been replaced by a more sparing approach. Surgeons focus on careful, minimal reduction and reimplantation of collected materials. After assessing the results of the procedures performed, the emphasis is currently placed on short-and long-term outcomes, possible complications, and secondary treatment options. Therefore, it is believed rhinoplasty could have an impact on quality of life [22].
It is worth noting that rhinoplasty, like any other surgical procedure, is associated with the possibility of occurrence of complications and the risk that there may be a discrepancy between the expectations of the patient and the doctor. For this reason, it seems crucial to conduct a properly performed initial examination, determine the patient’s expectations, and establish achievable goals for the surgery, including educating the patient about possible complications.
Complications that may occur include pain, swelling, infection, bleeding in the early and late postoperative period, postoperative deformities, discoloration of the incisors, scars, and breathing disorders, including the feeling of a blocked nose. Infections are extremely rare but can lead to a life-threatening condition if toxic shock syndrome develops. The risk is greater when sinus surgery and rhinoplasty are performed at the same time.
Skin and soft tissue complications include transient side effects such as postoperative swelling and hematomas. Late complications that are important for the patient include atrophy, fibrosis, the formation of unsightly scars, a feeling of numbness/stiffness, or even the formation of cysts from displaced mucosa or subcutaneous granulomas.
Postoperative deformities are considered the main risk of rhinoplasty and are the reason for reoperation in up to 5–15% of patients, depending on the sources. According to data, one of the most common postoperative deformities is “pollybeak”. The risk of this complication increases when, before surgery, the patient has a deep nasofrontal angle, a cartilaginous hump, and reduced apical projection. Pollybeak is the cause of up to 50% of all reoperations. Other common postoperative deformities include a drooping and wide nasal tip, recessed nasal column base, or nasal bridge irregularities [27,28].
The risk of complications can be reduced with increasing surgeon experience and previously established patient expectations. It needs to be underlined that we do not have good statistics describing frequency or percentage of possible complications, which should be a topic for further investigation.
Despite the common interpretation of assigning an aesthetic character to rhinoplasty, its functional value is crucial and has to be taken into account. Improvement of accuracy during surgery results in better visual and functional outcomes simultaneously. Thus, a measurement tool to assess these two classifications is significant regarding the holistic approach in contemporary surgeries [23].
Since there is disagreement between individual studies regarding the impact of rhinoplasty on quality of life, this systematic review and meta-analysis aimed to analyze a larger population and establish whether there was a significant difference between pre- and post-treatment data in patients who underwent such a procedure. Moreover, there is a debate concerning the selection of the questionnaire that should be used in nasal reconstruction surgery and rhinoplasty. The Rhinoplasty Outcome Evaluation (ROE) questionnaire is well known and easy to use. It allows for the assessment of rhinoplasty-related satisfaction in patients. Therefore, we decided to conduct the present meta-analysis based on the results of this questionnaire that are available in the literature.
As presented in Table 1, the time at which the ROE was used to evaluate outcomes is different in each study. As we know, rhinoplasty is a surgery for which its final effects depend on the length of time from surgery. Because of that, it seems to be quite relevant that the group of studies has no common length of time from surgery to use as a control.
The reported values from the ROE in rhinoplasty patients varied between the studies [9,10,11,12,13,14,15,16]. This might be linked to the fact that each study included patients with different lengths of postoperative follow-up or different ages of patients in the included patient groups. The mean age of patients was 44.8 years in a study by Chang et al. and 36.3 years in a study by Rabaioli et al. [7,18]. Arima et al. showed that patients from younger age groups reported lower postoperative satisfaction scores than older patients [29]. Moreover, as there are no data concerning the gender of the participants, we were not able to divide groups into sex-based subgroups to discover potential sources of heterogeneity.
Regarding the selection for the meta-analysis, studies by Sasidran et al., Plath et al., Ozturk et al., Hudise et al., Avcu et al., Kook et al., and Kim et al. were not considered [30,31,32,33,34,35,36,37]. Ozturk et al. and Hudise et al. did not provide the standard deviation, and Plath et al. also included oncological patients, which might have influenced the results of the questionnaire [30,31,34,35]. Sasidran et al. provided two different data sets of post-treatment SD reporting. Arima et al. [38] followed patients who had rhinoplasty to correct the nose over a time period from 12 months to 8.4 years. In another paper by Arima et al. [29] the mean follow-up time after rhinoplasty was 55.9 months (ranging from 6 to 10 years) with the patients being divided into two subgroups according to the follow-up period, 6 to <60 months and ≥60 months, so it was also not included in the meta-analysis. Moreover, the ROE questionnaire was filled in by telephone contact. Similarly, the study of Sezgar et al. was not included in the meta-analysis as the values of the ROE scores pre-treatment as well as post-treatment are much lower than in the considered studies, which could be due to anthropometric hallmarks and cultural habits of the group of patients [37]. Avcu et al. considered numerous subgroups of patients, Kook et al. reported the results of the modified ROE questionnaire, and Kim et al. did not report the mean value of the ROE [33,36].

Table 1.
Summary of the characteristics of the group of patients.
Table 1.
Summary of the characteristics of the group of patients.
| Publi+M18+A1:A1:M20 | Number of Subjects | Quantity of Group, F | Quantity of Group, M | Age of Group Mean | Age of Group SD | Age of Group Range | ROE Score Pre-Treatment Mean | ROE Score Pre-Treatment SD | ROE Score Post-Treatment Mean | ROE Score Post-Treatment SD | Follow-up Mean or Exact [Months] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rabaioli et al. [7] | 131 | 78 | 53 | 36.33 | 14.12 | 21.24 | 3.88 | 58.59 | 5.83 | 3 | |
| Rabaioli et al. [7] | 131 | 78 | 53 | 36.33 | 14.12 | 21.24 | 3.88 | 52.02 | 5.41 | 6 | |
| Kemal et al. [8] | 55 | 27 | 28 | 29.5 | 9.1 | 18–57 | 46.36 | 9.28 | 78.85 | 11.7 | 6 |
| Chang et al. [18] | 28 | 17 | 11 | 37.29 | 13.06 | 20–62 | 43.3 | 12.54 | 67.56 | 19.75 | 6 |
| Chang et al. [18] | 26 | 17 | 9 | 44.85 | 13.47 | 19–71 | 40.7 | 14.16 | 58.98 | 14.13 | 6 |
| Bulut 2017 et al. [11] | 102 | 51 | 51 | 28.7 | 11.4 | 42.2 | 15.7 | 63.9 | 18.9 | 12 | |
| Moura et al. [9] m1 | 25 | 11 | 14 | 36.36 | 12.87 | 28.2 | 15.2 | 68.8 | 20.8 | 3 | |
| Moura et al. [9] m2 | 24 | 14 | 10 | 35.75 | 16.1 | 22.5 | 17 | 69.7 | 20 | 3 | |
| Mahato et al. [10] | 117 | 50 | 67 | 28 | 18–50 | 26.5 | 6.95 | 75.21 | 9.58 | 3 | |
| Mahato et al. [10] | 117 | 50 | 67 | 28 | 26.5 | 6.95 | 75.13 | 9.48 | 6 | ||
| Mahato et al. [10] | 117 | 50 | 67 | 28 | 18–50 | 26.5 | 6.95 | 76 | 8.36 | 12 | |
| Bayram et al. [12] | 120 | 12 | 108 | 24 | 21–32 | 13.75 | 7.92 | 85 | 13.33 | 16 | |
| AlAwadh et al. [14] | 21 | 16 | 5 | 25.9 | 5.56 | 17–37 | 27.58 | 11.88 | 82.33 | 10.29 | 12 |
| Sabino et al. [15] | 95 | 41 | 54 | 35.52 | 9.86 | 17–59 | 40.08 | 7.07 | 92.45 | 5.28 | 12 |
| Suh et al. [16] | 30 | 28 | 2 | 23.6 | 1.08 | 17–38 | 33.61 | 2.75 | 90.42 | 1.37 | 11.1 |
| Sales et al. [39] | 20 | 11 | 9 | 28.90 | 41.13 | 19.71 | 80 | 14.38 | 8.9 | ||
| Barcagalia et al. [40] | 21 | 5 | 16 | 40 | 7.6 | 20.23 | 7.37 | 80.75 | 6.24 | 5 years | |
| Gökçe et al. [41] | 90 | 58 | 32 | 27.4 | 6.5 | 30.5 | 4.65 | 72.5 | 2.7 | 6 | |
| Jahandideh et al. [42] | 23 | 15 | 8 | 29.47 | 5.5 | 37.86 | 10.64 | 84.96 | 9.95 | 12 | |
| Jahandideh et al. [42] CT | 26 | 19 | 7 | 30.88 | 7.07 | 42.62 | 9.81 | 90.22 | 6.65 | 12 | |
| Jahandideh et al. [42] C | 25 | 17 | 8 | 29.24 | 2.01 | 40 | 13.39 | 83.99 | 8.89 | 12 | |
| Sazgar et al. [37] | 23 | 18 | 5 | 32.2 | 4.3 | 6.36 | 3.69 | 17.27 | 4.67 | 12 | |
| Riedel et al. [43] | 64 | 53 | 11 | 34.5 | 10.3 | 32.3 | 14.1 | 75.1 | 17.2 | 12 | |
| Haddady et al. [24] | 60 | 52 | 8 | 26.6 | 8.5 | 51.27 | 10.54 | 79.6 | 9..67 | 6 | |
| Bulut 2015 et al. [21] | 148 | 85 | 63 | 28.5 | 6.9 | 18–46 | 28.5 | 9 | 87.3 | 5 | 12 |
| Cingi et al. [20] | 191 | 18–57 | 19.77 | 7.99 | 76.2 | 17.46 | 12 | ||||
| Bulut 2018 et al. [13] | 69 | 37 | 32 | 42.2 | 15.7 | 63.9 | 18.9 | 12 |
This study is not devoid of limitations. In particular, the studies were conducted in different countries. Moreover, some authors suggested that the ROE scale should be adapted to consider anthropometric hallmarks and cultural habits, as it is difficult to standardize a patient satisfaction scale if this depends on different attributes and cultural beliefs [44,45]. In addition, different techniques were used (e.g., rhinoplasty using silicone implants in a study by Rabaioli et al. and rhinoseptoplasty with EPIT in a study by Moura et al.) [46]. However, some reports did not confirm the influence of surgical approach on ROE scores, as in Bulut et al. [11]. There were different postoperative follow-up processes (from 3 months up to 24 months), but based on the literature this should not have an influence on the ROE score. However, the subgroup analysis conducted by us suggested that the different times of grading of postoperative follow-up processes impacted the overall meta-analysis. The groups of patients were not homogenous as different sets of criteria were used (e.g., Rabaioli et al. included patients with symptoms of body dysmorphic disorder) [7].
The ROE seems to be an appropriate tool with which to evaluate the satisfaction and final results of rhinoplasty despite the individual differences in results from human diversity. Currently, the non-Caucasian population constitutes an important group of patients interested in the subject of rhinoplasty. This heterogenous group consists of people of varying cultures, races, and ethnicities. Evaluation of these patients requires great understanding of these differences and the ability to define what their aesthetic ideals are and what will be needed for surgery. Nevertheless, the universal goal when treating non-Caucasian patients is the same—ensuring that patients achieve their requirements in the best possible fashion [47].
Rhinoplasty in patients of African descent requires a patient-specific approach, because it must be considered based on different norms than for Caucasian noses [48].
A very specific group seeking rhinoplasty is a subgroup of people with Asian noses, the philosophy of rhinoplasty specific to this group is augmentation rather than reduction in which the dorsum is raised and the nasal tip projection and definition are enhanced. The watchword today is “ethnic preservation” rather than “effacement” for the Asian patient. An ethnically sensitive standard for aesthetic rhinoplasty for the Asian nose has been proposed [49].
The ROE also seems to be a great measuring outcome tool in other groups of non-Caucasian origin. Mahmoudi S et al. used the Rhinoplasty Outcome Evaluation (ROE) to evaluate rhinoplasties among the Iranian population. They found the questionnaire to be easy to use, and they showed that it allows comprehensive assessment of rhinoplasty-related patient satisfaction. However, the normal values for this questionnaire are not known. They found the Iranian version of the ROE to be a valid instrument to assess results in that population [50,51]. Çelik M et al. had a very similar observation. They enrolled 30 participants who were native Turkish and underwent primary rhinoplasty. The control group consisted of 58 healthy volunteers. The reliability of the Rhinoplasty Outcomes Evaluation-T was analyzed according to its internal consistency and test-retest reproducibility. The Rhinoplasty Outcomes Evaluation-T seems to be a valid questionnaire to measure rhinoplasty outcomes among Turkish patients [52].
We must measure aspects of satisfaction in cosmetic procedures, although we already know that there are some problematic subgroups that we must consider.
Body dysmorphic disorder and borderline personality disorder occur in up to 15% of patients seeking aesthetic procedures. It has been shown that performing surgery on this group of patients may worsen their previous condition [52]. Psychosocial problems may motivate the demand for aesthetic rhinoplasty. Surgery in major cases improves the quality of life and self-esteem of patients. Nevertheless, those suffering from major depressive disorder, generalized anxiety disorder, or other conditions may seek aesthetic rhinoplasty as a solution [53]. In these subgroups, the ROE needs further validation.
We must consider, as well, that articles included in our meta-analysis were examining different patient groups. Some of the cases were revision cases, and some of them were big reconstruction cases (as shown in Table 2). So, in future investigations it would be beneficial to create a more specific groups, which can determine the range of surgeries and, that way, modify the potential outcomes. Some of them were primary cases with potentially better outcomes, and some of them were secondary cases that needed bigger grafting.

Table 2.
Summary of patient groups examined in meta-analysis studies.
The results of this study demonstrated a significant difference between pre-treatment and post-treatment ROE results with a higher value of ROE score noted after treatment. This may suggest the impact of the rhinoplasty procedure on patients’ lives and should be a crucial argument, for example, for insurance companies in the insurance refund for the procedure.
When searching the literature to evaluate this topic, we noted that Arima et al. [38] found no difference in the quality of life between follow-up periods of 6 months and 10 years. However, in general, most articles revealed an improvement in quality of life. A meta-analysis showed different levels of QoL improvement in nasal obstruction [54]. Moreover, some authors observed that concomitant turbinate surgery had no influence on the nasal passage [55]. An increasing quantity of data showed a lower impact of septoplasty than had been believed before. Septoplasty (the surgical correction of a deviated nasal septum) is the most frequent laryngological procedure performed in adults. Nevertheless, published data are limited as regards to the strong level of evidence on the effectiveness of septoplasty. Therefore, trials are ongoing to try to measure the effectiveness of septoplasty with EBM gold standards [56]. Rhinoplasty is a more comprehensive procedure, so more aspects than just nasal congestion measurements have to be assessed. Hence, it seems that an improvement in the quality of life (in all its aspects) is the outcome that determines the success of cosmetic surgery. Patient-reported outcome measures (PROMs) constitute the tool to measure such areas in medicine. PROMs for clinical trials, effectiveness studies, and public health research have been defined as ‘‘any report coming directly from subjects without interpretation of the physician or others about how they function overall or feel in relation to a condition and its therapy’’ [57,58]. Therefore, we decided to conduct our systematic review using the ROE, which seems to be such a tool [50,59].
5. Conclusions
In summary, this study demonstrated a statistically significant difference between pre- and post-treatment ROE scores. The mean value of the pre-treatment ROE score was 33.50 with a CI of 29.46 to 37.53 (p < 0.001); for the post-treatment score it was 69.60 with a CI of 63.07 to 76.14 (t ≤ 6 months), and at t = 12 months it was 80.25 with a CI of 75.79 to 84.70 (p < 0.001). The mean difference between pre-treatment and post-treatment scores (t ≤ 6 months) was −36.31 with a CI of −40.93 to −31.69. The mean difference between pre-treatment and post-treatment scores for 6 m < t ≤ 12 m was −47.36 with a CI of −53.89 to −40.83. It is important to note that the received mean values of ROE scores after t = 12 m are comparable to the normative ROE scores, which are 73.1 ± 15.9. The ROE seems to be an appropriate tool to evaluate the satisfaction of patients after rhinoplasty; it is easy to carry out, and it is a valuable tool in clinical practice [60].
Author Contributions
Conceptualization, P.R., S.K. and M.S.; methodology, P.R., S.K., P.G. and M.S.; software, M.S.; validation, P.R.; formal analysis, M.S.; investigation, P.R., S.K., P.G., D.J., A.C. and M.S.; resources, P.R., S.K., P.G., D.J. and A.C.; data curation, P.R., S.K. and M.S. writing—original draft preparation, P.R., S.K., P.G. and M.S.; writing—review and editing, P.R., S.K. and M.S.; visualization, S.K. and M.S.; supervision, P.R., D.J. and A.C.; project administration, P.R., D.J. and A.C.; funding acquisition, A.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rohrich, R.J.; Villanueva, N.L.; Small, K.H.; Pezeshk, R.A. Implications of facial asymmetry in rhinoplasty. Plast. Reconstr. Surg. 2017, 140, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Ghorbani, F.; Ahmadi, H.; Davar, G. Patient dissatisfaction following rhinoplasty: A 10-year experience in Iran. Maxillofac. Plast. Reconstr. Surg. 2023, 45, 7. [Google Scholar] [CrossRef] [PubMed]
- Soler, Z.M.; Jones, R.; Le, P.; Rudmik, L.; Mattos, J.L.; Nguyen, S.A.; Schlosser, R.J. Sino-Nasal outcome test-22 outcomes after sinus surgery: A systematic review and meta-analysis. Laryngoscope 2018, 128, 581–592. [Google Scholar] [CrossRef]
- Gandomi, B.; Bayat, A.; Kazemei, T. Outcomes of septoplasty in young adults: The Nasal Obstruction Septoplasty Effectiveness study. Am. J. Otolaryngol. 2010, 31, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Izu, S.C.; Kosugi, E.M.; Brandão, K.V.; Lopes, A.S.; Garcia, L.B.S.; Suguri, V.M.; Gregório, L.C. Valores de normalidade para o questionário Rhinoplasty Outcome Evaluation (ROE). Braz. J. Otorhinolaryngol. 2012, 78, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, M.; Oddone, E.Z.; Samsa, G.P.; Landsman, P.B. Are health- -related quality-of-life measures affected by the mode of administration? J. Clin. Epidemiol. 1996, 49, 135–140. [Google Scholar] [CrossRef]
- Rabaioli, L.; Oppermann, P.D.O.; Pilati, N.P.; Klein, C.F.G.; Bernardi, B.L.; Migliavacca, R.; Lavinsky-Wolff, M. Evaluation of postoperative satisfaction with rhinoseptoplasty in patients with symptoms of body dysmorphic disorder. Braz. J. Otorhinolaryngol. 2022, 88, 539–545. [Google Scholar] [CrossRef]
- Kemal, Ö.; Tahir, E.; Kavaz, E.; Karabulut, H. Impact of Functional and Aesthetic Factors on Patient Satisfaction in Septorhinoplasty. Turk. Arch. Otorhinolaryngol. 2022, 60, 36–41. [Google Scholar] [CrossRef] [PubMed]
- de Moura, B.H.; Migliavacca, R.O.; Lima, R.K.; Dolci, J.E.; Becker, M.; Feijó, C.; Brauwers, E.; Lavinsky-Wolff, M. Partial inferior turbinectomy in rhinoseptoplasty has no effect in quality-of-life outcomes: A randomized clinical trial. Laryngoscope 2018, 128, 57–63. [Google Scholar] [CrossRef]
- Mahato, N.B.; Regmi, D.; Bista, M. Septorhinoplasty among Patients who Visited the Outpatient Department of Otolaryngology-Head and Neck Surgery of a Tertiary Care Center: A Descriptive Cross-sectional Study. J. Nepal Med. Assoc. 2021, 59, 432–436. [Google Scholar] [CrossRef]
- Bulut, O.C.; Wallner, F.; Hohenberger, R.; Plinkert, P.K.; Baumann, I. Quality of life after primary septorhinoplasty in deviated- and non-deviated nose measured with, R.O.E.; FROI-17 and SF-36. Rhinol. J. 2017, 55, 75–80. [Google Scholar] [CrossRef]
- Bayram, Y.; Yapici, A.K.; Zor, F.; Bozkurt, M.; Kilic, S.; Ozturk, S.; Afifi, A.M. Late Correction of Traumatic Nasal Deformities: A Surgical Algorithm and Experience in 120 Patients. Aesthet. Surg. J. 2018, 38, NP182–NP195. [Google Scholar] [CrossRef]
- Bulut, O.C.; Wallner, F.; Oladokun, D.; Kayser, C.; Plath, M.; Schulz, E.; Plinkert, P.K.; Baumann, I. Long-term quality of life changes after primary septorhinoplasty. Qual. Life Res. 2018, 27, 987–991. [Google Scholar] [CrossRef] [PubMed]
- AlAwadh, I.H.; Bogari, A.; Assiri, H.; Alabduljabbar, Z.; AlNassar, R.; Hudise, J.; AlArfaj, A. A Novel Technique for Spreader Flap by Folding the Dorsal Hump in Patients Undergoing Primary Rhinoplasty. J. Craniofacial Surg. 2022, 33, 2653–2658. [Google Scholar] [CrossRef]
- Sabino, L.; Cavalcanti, L.; Marcaccio, C.; Elzayat, S.; Procaccini, A.; Elfarargy, H.H.; Barbara, M. The novel traction-suturing technique in correction of caudal end deviation of the nasal septum. Eur. Arch. Oto-Rhino-Laryngol. 2023, 280, 2293–2298. [Google Scholar] [CrossRef]
- Suh, J.; Suh, M.K.; Choi, H. Triple Strut Concept for the Nasal Tip Projection in Small Lower Lateral Cartilages and Septum. J. Craniofacial Surg. 2023, 34, 1686–1689. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Zhou, L. The Effect of Functional Rhinoplasty on Quality of Life: A Systematic Review and Meta-Analysis. Aesthetic Plast. Surg. 2024, 48, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Yun, H.; Choi, J.W.; Suh, J.M.; Jeong, W.S.; Park, H.; Kang, M.K.; Shin, Y.; Kim, K.; Chung, C.H. Efficacy and safety of equine cartilage for rhinoplasty: A multicenter double-blind non-inferiority randomized confirmatory clinical trial. Arch. Craniofacial Surg. 2022, 23, 152–162. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Cingi, C.; Eskiizmir, G. Deviated nose attenuates the degree of patient satisfaction and quality of life in rhinoplasty: A prospective controlled study. Clin. Otolaryngol. 2013, 38, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Bulut, O.C.; Wallner, F.; Plinkert, P.K.; Prochnow, S.; Kuhnt, C.; Baumann, I. Quality of life after septorhinoplasty measured with the Functional Rhinoplasty Outcome Inventory 17 (FROI-17). Rhinol. J. 2015, 53, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Rot, P.; Skrzypiec, Ł.; Jadczak, M.; Jurkiewicz, D. Ocena jakości życia przed i po septorynoplastyce metodą otwartą przy użyciu ankiety WHOQOL-BREF. Otolaryngol. Pol. 2018, 72, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Fichman, M.; Piedra Buena, I.T. Rhinoplasty; StatPearls: St. Petersburg, FL, USA, 2020. [Google Scholar]
- Haddady Abianeh, S.; Moradi Bajestani, S.; Rahmati, J.; Shahrbaf, M.A.; Fatehi Meybodi, A. Evaluation of Aesthetic and Functional Outcomes After Open Rhinoplasty: A Quasi-experimental Study by the Aid of ROE and RHINO Questionnaires. Aesthetic Plast. Surg. 2021, 45, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Anco, N.; Caballero, G.; Adrianzen, G. Preservation Rhinoplasty: A New Approach to Mestizo Noses. Plast. Reconstr. Surg.–Glob. Open 2023, 11, e4972. [Google Scholar] [CrossRef] [PubMed]
- Jadczak, M.; Krzywdzińska, S.; Jurkiewicz, D. Asymmetrical Lateral Crus Steal in Geometric Tip Reshaping. In Facial Plastic Surgery; Thieme Medical Publishers, Inc.: New York, NY, USA, 2024. [Google Scholar] [CrossRef]
- Watson, D.; Crawford, K.L. Reducing Surgical Risks in the Rhinoplasty Patient. Facial Plast. Surg. Clin. N. Am. 2023, 31, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Rettinger, G. Risks and complications in rhinoplasty. GMS Curr. Top. Otorhinolaryngol. Head Neck Surg. 2007, 6, Doc08. [Google Scholar] [PubMed]
- Arima, L.M.; Velasco, L.C.; Tiago, R.S.L. Influence of Age on Rhinoplasty Outcomes Evaluation: A Preliminary Study. Aesthetic Plast. Surg. 2012, 36, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Hudise, J.Y.; Aldhabaan, S.A.; Aldosari, B.F. Complications of the nasal dorsum reconstruction using autologous or alloplastic grafts: Evidence from systematic review and meta-analysis. Braz. J. Otorhinolaryngol. 2022, 88, 406–420. [Google Scholar] [CrossRef]
- Öztürk, G. New Approaches for the Let-Down Technique. Aesthetic Plast. Surg. 2020, 44, 1725–1736. [Google Scholar] [CrossRef]
- Metin, M.; Avcu, M. The Effect on Patient Satisfaction of the Postoperative Nasal Topographic, Demographic, and Functional Results of Open and Closed Septorhinoplasty Techniques. J. Craniofacial Surg. 2021, 32, 868–873. [Google Scholar] [CrossRef]
- Kook, W.S.; Ryu, D.H.; Baek, W.; Kook, H.M.; Jang, Y.Y.; Lew, D.H. Prevention and Resolution of Silicone Implant–Related Problems in Secondary Rhinoplasty Using a Cross-Linked Human Acellular Dermal Matrix. Plast. Reconstr. Surg. 2023, 152, 45–54. [Google Scholar] [CrossRef]
- Plath, M.; Thielen, H.M.; Baumann, I.; Zaoui, K.; Federspil, P.A. Tumor Control and Quality of Life in Skin Cancer Patients With Extensive Multilayered Nasal Defects. Clin. Exp. Otorhinolaryngol. 2020, 13, 164–172. [Google Scholar] [CrossRef]
- Öztürk, G. Prevention of Nasal Deviation Related to Preservation Rhinoplasty in Non-deviated Noses using Suturing Approaches. In Aesthetic Plastic Surgery; Springer: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- Kim, J.Y.; Cha, M.J.; Kwon, S.S.; Kim, D.K. Factors that contribute to disagreement in satisfaction between surgeons and patients after corrective septorhinoplasty. Am. J. Rhinol. Allergy 2017, 31, 416–419. [Google Scholar] [CrossRef] [PubMed]
- Sazgar, A.A.; Hajialipour, S.; Razfar, A.; Rahavi-Ezabadi, S. The Effectiveness of Skeletal Reconstruction in Severe Post-Rhinoplasty Nasal Deformity. Aesthet. Surg. J. 2021, 41, 905–918. [Google Scholar] [CrossRef]
- Arima, L.M.; Velasco, L.C.; Tiago, R.S.L. Crooked nose: Outcome evaluations in rhinoplasty. Braz. J. Otorhinolaryngol. 2011, 77, 510–515. [Google Scholar] [CrossRef]
- Sales, J.O.; Gubisch, W.; Duarte, R.R.; Moreno, A.S.; Oliveira, F.M.; Coura, L.M. Caudal extension graft of the lower lateral cartilage: Technique and aesthetic and functional results. Facial Plast. Surg. 2021, 37, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Bracaglia, R.; Servillo, M.; Fortunato, R.; Pino, V.; Albanese, R.; Gentileschi, S. Rainbow graft for tip reconstruction in revision rhinoplasty. J.Plast. Reconstr. Aesthetic Surg. 2020, 73, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Gökçe Kütük, S.; Arıkan, O.K. Evaluation of the effects of open and closed rhinoplasty on the psychosocial stress level and quality of life of rhinoplasty patients. J.Plast. Reconstr. Aesthetic Surg. 2019, 72, 1347–1354. [Google Scholar] [CrossRef]
- Jahandideh, H.; Dehghani Firouzabadi, F.; Dehghani Firouzabadi, M.; Jfm Lohuis, P.; Roomiani, M. The Persian Version of Utrecht Questionnaire for Evaluation of Aesthetic Rhinoplasty Outcomes: Translation and Validation. World J. Plast. Surg. 2020, 9, 141–145. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Riedel, F.; Wähmann, M.; Veit, J.A.; Bulut, O.C. Quality of life outcome in revision rhinoplasty in regars to number of revision surgeries and cartilage donor site. Auris Nasus Larynx 2022, 49, 286–290. [Google Scholar] [CrossRef]
- Izu, S.C.; Kosugi, E.M.; Lopes, A.S.; Brandão, K.V.; Sousa, L.B.G.; Suguri, V.M.; Gregório, L.C. Validation of the Rhinoplasty Outcomes Evaluation (ROE) questionnaire adapted to Brazilian Portuguese. Qual. Life Res. 2014, 23, 953–958. [Google Scholar] [CrossRef] [PubMed]
- Bulut, O.C.; Plinkert, P.K.; Wallner, F.; Baumann, I. Quality of life in functional rhinoplasty: Rhinoplasty outcomes evaluation German version (ROE-D). Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 2569–2573. [Google Scholar] [CrossRef] [PubMed]
- de Moura, B.H. How to Prevent Nasal Obstruction After Rhino Septoplasty. Could A Routine Turbinate Reduction Improve the Outcomes in Quality of Life of Patients? Sch. J. Otolaryngol. 2020, 4, 1–3. [Google Scholar] [CrossRef]
- Cobo, R. Non-Caucasian Rhinoplasty. Clin. Plast. Surg. 2022, 49, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Boyette, J.R.; Stucker, F.J. African American Rhinoplasty. Facial Plast. Surg. Clin. N. Am. 2014, 22, 379–393. [Google Scholar] [CrossRef] [PubMed]
- Lam, S. Asian Rhinoplasty. Semin. Plast. Surg. 2009, 23, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Mahmoudi, S.; Zadeh, M.R. Development and Validation of the Rhinoplasty Outcomes Evaluation (ROE) Questionnaire: An Analytical Study. World J. Plast. Surg. 2022, 11, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Çelik, M.; Altıntaş, A. The Turkish Version of the Rhinoplasty Outcomes Evaluation Questionnaire: Validation and Clinical Application. Balk. Med. J. 2019, 36, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Wever, C.C.; Wever, A.M.E.; Constantian, M. Psychiatric Disorders in facial plastic surgery. Facial Plast. Surg. Clin. N. Am. 2020, 28, 451–460. [Google Scholar] [CrossRef]
- Shauly, O.; Calvert, J.; Stevens, G.; Rohrich, R.; Villanueva, N.; Gould, D.J. Assessment of Wellbeing and Anxiety-related Disorders in Those Seeking Rhinoplasty: A Crowdsourcing-based Study. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2737. [Google Scholar] [CrossRef]
- Zhao, R.; Chen, K.; Tang, Y. Effects of Functional Rhinoplasty on Nasal Obstruction: A Meta-Analysis. Aesthetic Plast. Surg. 2022, 46, 873–885. [Google Scholar] [CrossRef] [PubMed]
- van Egmond, M.M.H.T.; Rovers, M.M.; Hannink, G.; Hendriks, C.T.M.; van Heerbeek, N. Septoplasty with or without concurrent turbinate surgery versus non-surgical management for nasal obstruction in adults with a deviated septum: A pragmatic, randomised controlled trial. Lancet 2019, 394, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Rennie, K.J.; O’Hara, J.; Rousseau, N.; Stocken, D.; Howel, D.; Ternent, L.; Drinnan, M.; Bray, A.; Rooshenas, L.; Hamilton, D.W.; et al. Nasal Airway Obstruction Study (NAIROS): A phase III, open-label, mixed-methods, multicentre randomised controlled trial of septoplasty versus medical management of a septal deviation with nasal obstruction. Trials 2020, 21, 179. [Google Scholar] [CrossRef] [PubMed]
- Patrick, D.L.; Burke, L.B.; Powers, J.H.; Scott, J.A.; Rock, E.P.; Dawisha, S.; O’Neill, R.; Kennedy, D.L. Patient-Reported Outcomes to Support Medical Product Labeling Claims: FDA Perspective. Value Health 2007, 10, S125–S137. [Google Scholar] [CrossRef] [PubMed]
- Lasch, K.E.; Marquis, P.; Vigneux, M.; Abetz, L.; Arnould, B.; Bayliss, M.; Crawford, B.; Rosa, K. PRO development: Rigorous qualitative research as the crucial foundation. Qual. Life Res. 2010, 19, 1087–1096. [Google Scholar] [CrossRef] [PubMed]
- Nocini, R.; Chirumbolo, S.; Pirayesh, A.; Rahman, E.; Kapoor, K.M.; Caliskan, G.; Bertossi, D. A systematic review and meta-analysis of rhinoplasty using the rhinoplasty outcome evaluation scale. Ann. Maxillofac. Surg. 2022, 12, 60. [Google Scholar] [CrossRef]
- Plath, M.; Sand, M.; Cavaliere, C.; Plinkert, P.K.; Baumann, I.; Zaoui, K. How to predict the outcome of septorhinoplasty? A normative study of ROE and FROI-17 scores. Acta Otorhinolaryngol. Ital. 2021, 41, 327–335. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).