PRO-NOVELTY: Patient-Reported Outcomes in NOse VEstibule interventionaL radioTherapY (brachytherapy)
Abstract
1. Introduction
2. Materials and Methods
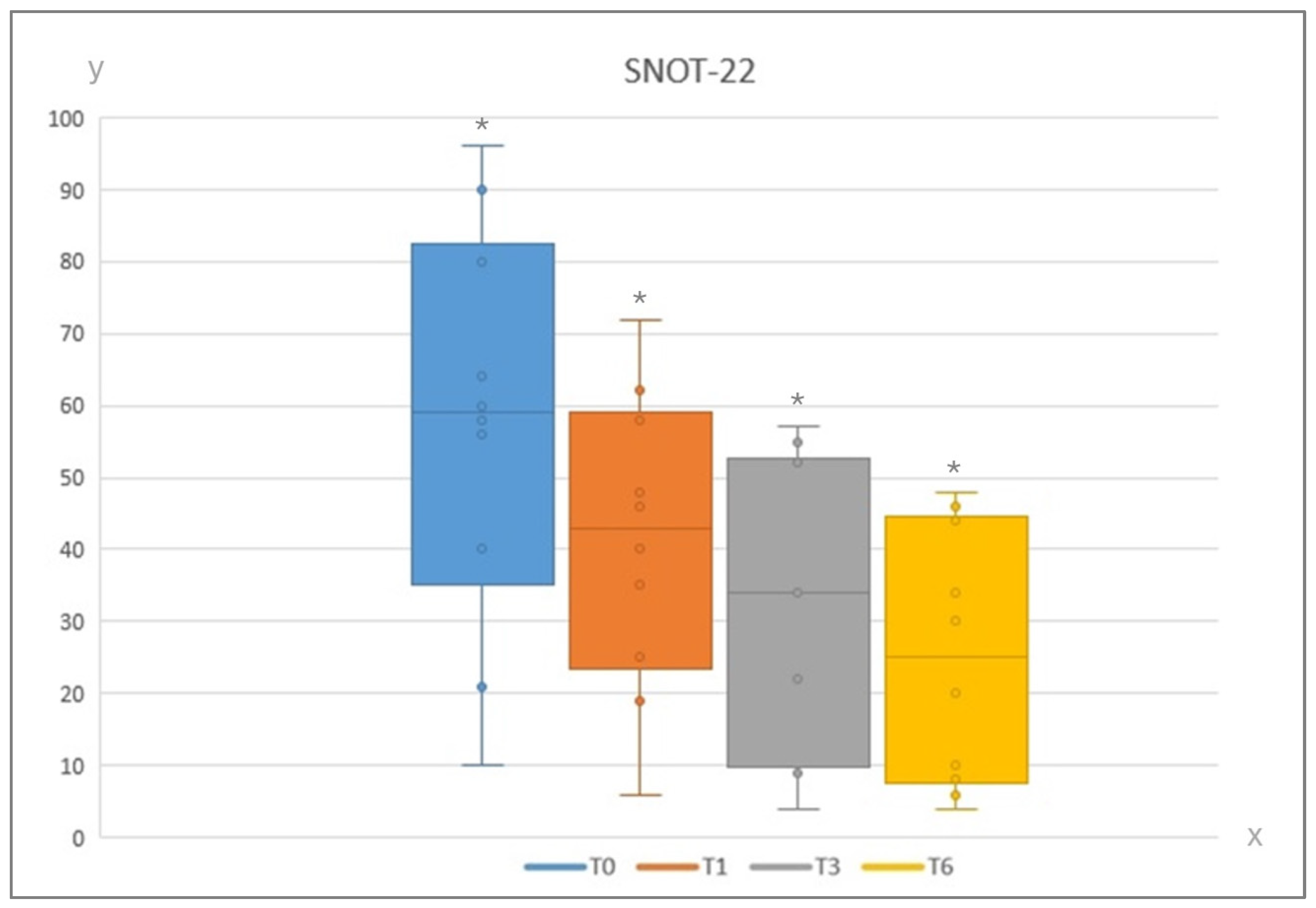
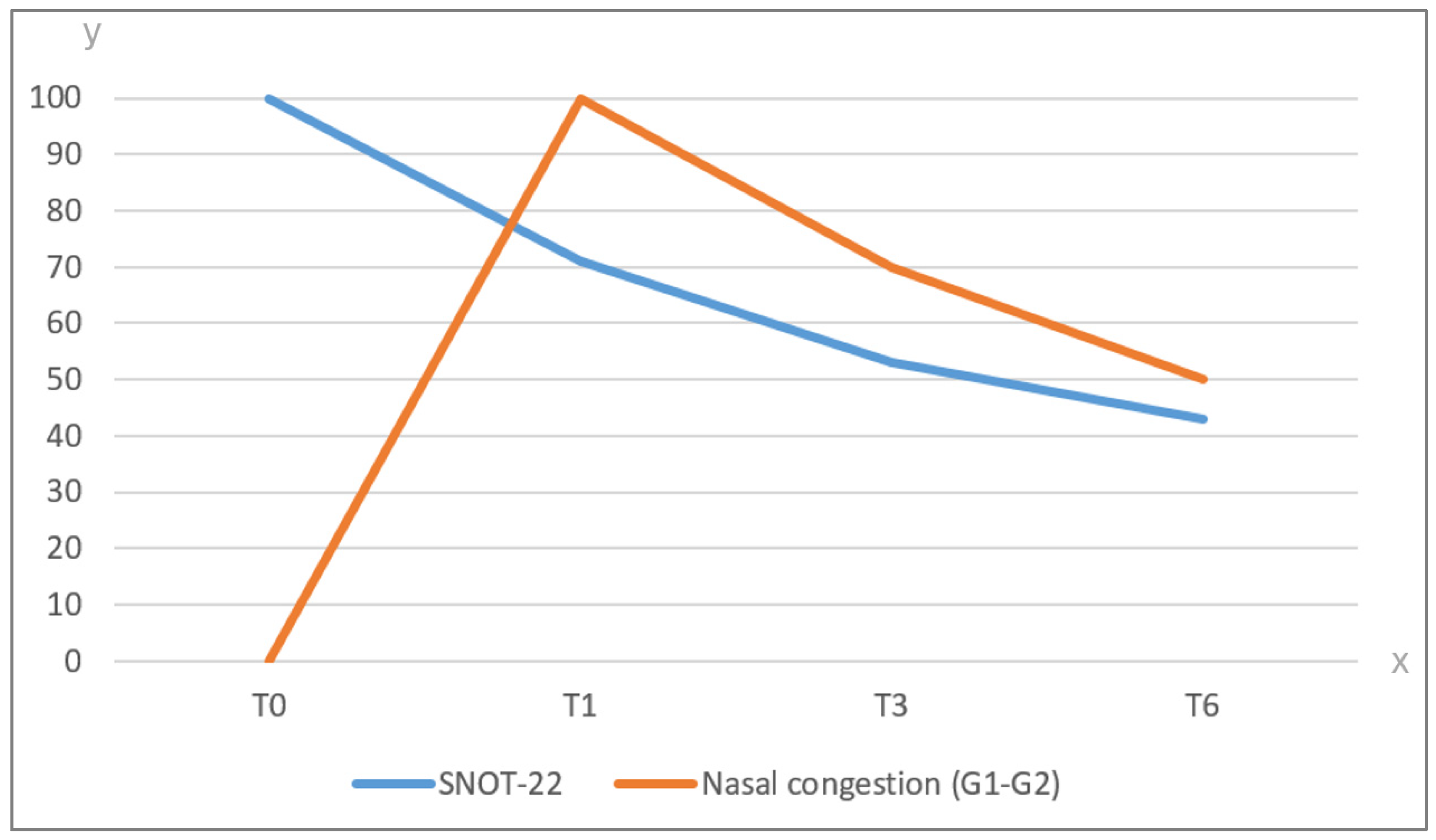
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patel, P.; Tiwari, R.; Karim, A.B.; Nauta, J.J.; Snow, G.B. Squamous cell carcinoma of the nasal vestibule. J. Laryngol. Otol. 1992, 106, 332–336. [Google Scholar] [CrossRef] [PubMed]
- van de Velde, L.J.; Scheurleer, W.F.J.; Braunius, W.W.; Devriese, L.A.; de Ridder, M.; de Bree, R.; Breimer, G.E.; van Dijk, B.A.; Rijken, J.A. Squamous cell carcinoma of the nasal vestibule in the Netherlands: A clinical and epidemiological review of 763 cases (2008–2021). Head Neck 2024, 46, 1809–1821. [Google Scholar] [CrossRef]
- Agger, A.; von Buchwald, C.; Madsen, A.R.; Yde, J.; Lesnikova, I.; Christensen, C.B.; Foghsgaard, S.; Christensen, T.B.; Hansen, H.S.; Larsen, S.; et al. Squamous cell carcinoma of the nasal vestibule 1993-2002: A nationwide retrospective study from DAHANCA. Head Neck 2009, 31, 1593–1599. [Google Scholar] [CrossRef] [PubMed]
- Filtenborg, M.V.; Lilja-Fischer, J.K.; Sharma, M.B.; Primdahl, H.; Kjems, J.; Plaschke, C.C.; Charabi, B.W.; Kristensen, C.A.; Andersen, M.; Andersen, E.; et al. Nasal vestibule squamous cell carcinoma: A population-based cohort study from DAHANCA. Acta Oncol. 2022, 61, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Haynes, W.D.; Tapley, N. Proceedings: Radiation treatment of carcinoma of the nasal vestibule. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1974, 120, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Bussu, F.; Tagliaferri, L.; Corbisiero, M.F.; Lotto, C.; Pellini, R.; Guarino, P.; Mercante, G.; Galuppi, A.; Cariti, F.; Almadori, G.; et al. Management of nasal vestibule carcinomas: Recommendations by the Oncological Committee of the Italian Society of Otorhinolaryngology—Head and Neck Surgery. Acta Otorhinolaryngol. Ital. 2024, 44, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Bussu, F.; Tagliaferri, L.; De Corso, E.; Passali, G.C.; Lancellotta, V.; Mattiucci, G.C.; Gambacorta, M.A.; Rizzo, D.; Di Cintio, G.; Salvati, A.; et al. Functional results of exclusive interventional radiotherapy (brachytherapy) in the treatment of nasal vestibule carcinomas. Brachytherapy 2021, 20, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Czerwinski, M.D.; van Leeuwen, R.G.H.; Kaanders, J.H.A.M.; Zwijnenburg, E.M.; Lipman, D.; Takes, R.P.; Verhoef, C.G. Image Guided Brachytherapy for Cancer of the Nasal Vestibule: Local Control and Cosmesis. Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 913–921. [Google Scholar] [CrossRef] [PubMed]
- Bussu, F.; Tagliaferri, L.; Mattiucci, G.; Parrilla, C.; Dinapoli, N.; Miccichè, F.; Artuso, A.; Galli, J.; Almadori, G.; Valentini, V.; et al. Comparison of interstitial brachytherapy and surgery as primary treatments for nasal vestibule carcinomas. Laryngoscope 2016, 126, 367–371. [Google Scholar] [CrossRef]
- Silveira, A.P.; Gonçalves, J.; Sequeira, T.; Ribeiro, C.; Lopes, C.; Monteiro, E.; Pimentel, F.L. Patient reported outcomes in head and neck cancer: Selecting instruments for quality of life integration in clinical protocols. Head Neck Oncol. 2010, 2, 32. [Google Scholar] [CrossRef][Green Version]
- Chow, V.J.; Tsetsos, N.; Poutoglidis, A.; Georgalas, C. Quality of life in sinonasal tumors: An up-to-date review. Curr. Opin. Otolaryngol. Head Neck Surg. 2022, 30, 46–57. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, C.; Gillett, S.; Slack, R.; Lund, V.J.; Browne, J.P. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin. Otolaryngol. 2009, 34, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Mozzanica, F.; Preti, A.; Gera, R.; Gallo, S.; Bulgheroni, C.; Bandi, F.; Ottaviani, F.; Castelnuovo, P. Correction to: Cross-cultural adaptation and validation of the SNOT-22 into Italian. Eur. Arch. Otorhinolaryngol. 2022, 279, 3753–3754. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.N.; Wang, Y.M.; Chen, W.C.; Fang, F.M.; Li, S.H.; Huang, T.L.; Hwang, C.F.; Lee, Y.; Lin, C.Y.; Luo, S.D. Evaluation of Sinonasal Outcome Test (SNOT-22) Domains in the Assessment of the Quality of Life in Patients with Nasopharyngeal Carcinoma. Cancer Manag. Res. 2023, 15, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Maoz, S.L.; Wang, E.W.; Hwang, P.H.; Choby, G.; Kuan, E.C.; Fleseriu, C.M.; Chan, E.P.; Adappa, N.D.; Geltzeiler, M.; Getz, A.E.; et al. Long-term quality of life after treatment in sinonasal malignancy: A prospective, multicenter study. Int. Forum Allergy Rhinol. 2023, 13, 2030–2042. [Google Scholar] [CrossRef]
- Grimm, D.R.; Beswick, D.M.; Maoz, S.L.; Wang, E.W.; Choby, G.W.; Kuan, E.C.; Chan, E.P.; Adappa, N.D.; Geltzeiler, M.; Getz, A.E.; et al. SNOT-22 subdomain outcomes following treatment for sinonasal malignancy: A prospective, multicenter study. Int. Forum Allergy Rhinol. 2024, 14, 1314–1326. [Google Scholar] [CrossRef]
- Fleseriu, C.M.; Beswick, D.M.; Maoz, S.L.; Hwang, P.H.; Choby, G.; Kuan, E.C.; Chan, E.P.; Adappa, N.D.; Geltzeiler, M.; Getz, A.E.; et al. Predictive factors for decreased baseline quality of life in patients with sinonasal malignancies. Int. Forum Allergy Rhinol. 2024, 14, 775–785. [Google Scholar] [CrossRef]
- Tagliaferri, L.; Carra, N.; Lancellotta, V.; Rizzo, D.; Casà, C.; Mattiucci, G.; Parrilla, C.; Fionda, B.; Deodato, F.; Cornacchione, P.; et al. Interventional radiotherapy as exclusive treatment for primary nasal vestibule cancer: Single-institution experience. J. Contemp. Brachyther. 2020, 12, 413–419. [Google Scholar] [CrossRef]
- Available online: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_5x7.pdf (accessed on 25 January 2023).
- Wagenblast, J.; Baghi, M.; Helbig, M.; Arnoldner, C.; Bisdas, S.; Gstöttner, W.; Hambek, M.; May, A. Craniofacial reconstructions with bone-anchored epithesis in head and neck cancer patients—A valid way back to self-perception and social reintegration. Anticancer Res. 2008, 28, 2349–2352. [Google Scholar]
- Pantelakos, S.T.; McGuirt, W.F.; Nussear, D.W. Squamous cell carcinoma of the nasal vestibule and anterior nasal passages. Am. J. Otolaryngol. 1994, 15, 33–36. [Google Scholar] [CrossRef]
- Tagliaferri, L.; Fionda, B.; Bussu, F.; Parrilla, C.; Lancellotta, V.; Deodato, F.; Cammelli, S.; Boldrini, L.; Gambacorta, M.A.; Morganti, A.G.; et al. Interventional radiotherapy (brachytherapy) for squamous cell carcinoma of the nasal vestibule: A multidisciplinary systematic review. Eur. J. Dermatol. 2019, 29, 417–421. [Google Scholar] [CrossRef]
- Wang, C.C. Treatment of carcinoma of the nasal vestibule by irradiation. Cancer 1976, 38, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Bussu, F.; Tagliaferri, L.; Piras, A.; Rizzo, D.; Tsatsaris, N.; De Corso, E.; Parrilla, C.; Paludetti, G. Multidisciplinary approach to nose vestibule malignancies: Setting new standards. Acta Otorhinolaryngol. Ital. 2021, 1, S158–S165. [Google Scholar] [CrossRef] [PubMed]
- Czerwinski, M.D.; Jansen, P.P.; Zwijnenburg, E.M.; Al-Mamgani, A.; Vergeer, M.R.; Langendijk, J.A.; Wesseling, F.W.R.; Kaanders, J.H.A.M.; Verhoef, C.G. Radiotherapy as nose preservation treatment strategy for cancer of the nasal vestibule: The Dutch experience. Radiother. Oncol. 2021, 164, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Levendag, P.C.; Nijdam, W.M.; van Moolenburgh, S.E.; Tan, L.; Noever, I.; van Rooy, P.; Mureau, M.A.; Jansen, P.P.; Munte, K.; Hofer, S.O. Interstitial radiation therapy for early-stage nasal vestibule cancer: A continuing quest for optimal tumor control and cosmesis. Int. J. Radiat. Oncol. Biol. Phys. 2006, 66, 160–169. [Google Scholar] [CrossRef]
- Bussu, F.; Tagliaferri, L.; Crescio, C.; Rizzo, D.; Gallus, R.; Parrilla, C.; Fionda, B.; Lancellotta, V.; Mattiucci, G.C.; Galli, J. New standards for the management of nose vestibule malignancies. Acta Otolaryngol. 2023, 143, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.M.; Dasgeb, B.; Liem, S.; Ali, A.; Harrison, A.; Finkelstein, M.; Cha, J.; Anne, R.; Greenbaum, S.; Sherwin, W.; et al. High-Dose-Rate Brachytherapy for the Treatment of Basal and Squamous Cell Carcinomas on Sensitive Areas of the Face: A Report of Clinical Outcomes and Acute and Subacute Toxicities. Adv. Radiat. Oncol. 2020, 6, 100616. [Google Scholar] [CrossRef] [PubMed]
- Vital, D.; Morand, G.; Huber, G.F.; Studer, G.; Holzmann, D. Outcome in squamous cell carcinoma of the nasal vestibule: A single center experience. Head Neck 2015, 37, 46–51. [Google Scholar] [CrossRef]
- Langendijk, J.A.; Poorter, R.; Leemans, C.R.; de Bree, R.; Doornaert, P.; Slotman, B.J. Radiotherapy of squamous cell carcinoma of the nasal vestibule. Int. J. Radiat. Oncol. Biol. Phys. 2004, 59, 1319–1325. [Google Scholar] [CrossRef]
- Kılıç, C.; Tunçel, Ü.; Cömert, E.; Kaya, B.V. The effect of radiotherapy on mucociliary clearance in patients with laryngeal and nasopharyngeal cancer. Eur. Arch. Otorhinolaryngol. 2015, 272, 1517–1520. [Google Scholar] [CrossRef]
- Kamel, R.; Al-Badawy, S.; Khairy, A.; Kandil, T.; Sabry, A. Nasal and paranasal sinus changes after radiotherapy for nasopharyngeal carcinoma. Acta Otolaryngol. 2004, 124, 532–535. [Google Scholar] [CrossRef]
- Surico, G.; Muggeo, P.; Mappa, L.; Muggeo, V.; Conti, V.; Lucarelli, A.; Novielli, C.; Rigillo, N. Impairment of nasal mucociliary clearance after radiotherapy for childhood head cancer. Head Neck 2001, 23, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Camacho, M.; Gonella, S.; Campbell, S.; Scrimger, R.A.; Wismer, W.V. A systematic review of smell alterations after radiotherapy for head and neck cancer. Cancer Treat. Rev. 2017, 54, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Stringer, S.P.; Stiles, W.; Slattery, W.H.; Krumerman, J.; Parsons, J.T.; Mendenhall, W.M.; Cassisi, N.J. Nasal mucociliary clearance after radiation therapy. Laryngoscope 1995, 105, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Boita, M.; Ravera, M.; Moretto, F.; Badellino, S.; Rampino, M.; Ricardi, U.; Pecorari, G.; Garzaro, M. Nasal cytological changes as late effects of radiotherapy for nasopharyngeal cancer. Am. J. Rhinol. Allergy 2015, 29, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Scheurleer, W.F.J.; Dehnad, H.; Braunius, W.W.; Janssen, L.M.; Tijink, B.M.; Breimer, G.E.; Smid, E.J.; Devriese, L.A.; Bree, R.; Ridder, M.; et al. Long-term oncological follow-up after mold-based pulsed dose rate brachytherapy for early stage squamous cell carcinoma of the nasal vestibule: A single center experience of 68 patients over a 17-year period. Brachytherapy 2023, 22, 221–230. [Google Scholar] [CrossRef]
- Chargari, C.; Van Limbergen, E.; Mahantshetty, U.; Deutsch, É.; Haie-Méder, C. Radiobiology of brachytherapy: The historical view based on linear quadratic model and perspectives for optimization. Cancer Radiother. 2018, 22, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Murakami, N.; Omura, G.; Yatsuoka, W.; Okamoto, H.; Yoshimoto, S.; Ueno, T.; Itami, J. Hybrid Intracavitary-Interstitial brachytherapy in a case of nasal vestibule cancer penetrating the hard palate. BJR Case Rep. 2021, 7, 20200178. [Google Scholar] [CrossRef] [PubMed]
- Fionda, B.; Bussu, F.; Placidi, E.; Rosa, E.; Lancellotta, V.; Parrilla, C.; Zinicola, T.; De Angeli, M.; Greco, F.; Rigante, M.; et al. Interventional Radiotherapy (Brachytherapy) for Nasal Vestibule: Novel Strategies to Prevent Side Effects. J. Clin. Med. 2023, 12, 6154. [Google Scholar] [CrossRef]
- Plath, M.; Thielen, H.M.; Baumann, I.; Zaoui, K.; Federspil, P.A. Tumor Control and Quality of Life in Skin Cancer Patients with Extensive Multilayered Nasal Defects. Clin. Exp. Otorhinolaryngol. 2020, 13, 164–172. [Google Scholar] [CrossRef]
- Moolenburgh, S.E.; Mureau, M.A.; Duivenvoorden, H.J.; Hofer, S.O. Validation of a questionnaire assessing patient’s aesthetic and functional outcome after nasal reconstruction: The patient NAFEQ-score. J. Plast. Reconstr. Aesthetic Surg. 2009, 62, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.; Becker, A.M.; Pfeiffer, J. Health-related quality of life in patients with nasal prosthesis. J. Cranio-Maxillofac. Surg. 2016, 44, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Liao, L.J.; Hsu, W.L.; Lo, W.C.; Cheng, P.W.; Shueng, P.W.; Hsieh, C.H. Health-related quality of life and utility in head and neck cancer survivors. BMC Cancer 2019, 19, 425. [Google Scholar] [CrossRef] [PubMed]
- Whoqol Group. The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.S.; Lin, P.Y.; Chien, C.Y.; Fang, F.M.; Chiu, N.M.; Hung, C.F.; Lee, Y.; Chong, M.Y. Anxiety and depression in patients with head and neck cancer: 6-month follow-up study. Neuropsychiatr. Dis. Treat. 2016, 12, 1029–1036. [Google Scholar] [CrossRef]
- Terrell, J.E.; Ronis, D.L.; Fowler, K.E.; Bradford, C.R.; Chepeha, D.B.; Prince, M.E.; Teknos, T.N.; Wolf, G.T.; Duffy, S.A. Clinical predictors of quality of life in patients with head and neck cancer. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.; Haywood, K.; Fitzpatrick, R. Impact of patient-reported outcome measures on routine practice: A structured review. J. Eval. Clin. Pract. 2006, 12, 559–568. [Google Scholar] [CrossRef]
- Black, N. Patient reported outcome measures could help transform healthcare. BMJ 2013, 346, 167. [Google Scholar] [CrossRef] [PubMed]
- Dawson, J.; Doll, H.; Fitzpatrick, R.; Jenkinson, C.; Carr, A.J. The routine use of patient reported outcome measures in healthcare settings. BMJ 2010, 340, 186. [Google Scholar] [CrossRef]
- Churruca, K.; Pomare, C.; Ellis, L.A.; Long, J.C.; Henderson, S.B.; Murphy, L.E.D.; Leahy, C.J.; Braithwaite, J. Patient-reported outcome measures (PROMs): A review of generic and condition-specific measures and a discussion of trends and issues. Health Expect. 2021, 24, 1015–1024. [Google Scholar] [CrossRef]
- Piccirillo, J.F.; Merritt, M.G.J.; Richards, M.L. Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol. Head Neck Surg. 2002, 126, 41–47. [Google Scholar] [CrossRef] [PubMed]
- DeConde, A.S.; Mace, J.C.; Bodner, T.; Hwang, P.H.; Rudmik, L.; Soler, Z.M.; Smith, T.L. SNOT-22 quality of life domains differentially predict treatment modality selection in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2014, 4, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, C.; Browne, J.P.; Slack, R.; Lund, V.; Topham, J.; Reeves, B.; Copley, L.; Brown, P.; van der Meulen, J. The national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Clin. Otolaryngol. 2006, 31, 390–398. [Google Scholar] [CrossRef] [PubMed]
- Bellocchi, G.; Loperfido, A.; Passali, F.M.; Millarelli, S.; Velletrani, G.; Perla, M.; Di Michele, L.; Di Girolamo, S. Biologics in severe uncontrolled chronic rhinosinusitis with nasal polyps: A bicentric experience. Acta Biomed. 2023, 94, 2023227. [Google Scholar] [CrossRef]
- Soler, Z.M.; Jones, R.; Le, P.; Rudmik, L.; Mattos, J.L.; Nguyen, S.A.; Schlosser, R.J. Sino-Nasal outcome test-22 outcomes after sinus surgery: A systematic review and meta-analysis. Laryngoscope 2018, 128, 581–592. [Google Scholar] [CrossRef] [PubMed]
- Poirrier, A.L.; Ahluwalia, S.; Goodson, A.; Ellis, M.; Bentley, M.; Andrews, P. Is the Sino-Nasal Outcome Test-22 a suitable evaluation for septorhinoplasty? Laryngoscope 2013, 123, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Dizdar, D.; Bozan, A.; Dizdar, S.K.; Göde, S.; Alpay, H.C. Evaluation of nasal symptoms in septoplasty patients using SNOT-22. Acta Otorhinolaryngol. Ital. 2019, 39, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Vlaykov, A.N. Application of SNOT-22 test and visual analogue scale in quality of life evaluation in patients with allergic rhinitis. Folia Medica 2021, 63, 337–347. [Google Scholar] [CrossRef]
- Kuan, E.C.; Peng, K.A.; Thompson, C.F.; Suh, J.D.; Wang, M.B. Sinonasal quality of life outcomes following laser treatment of epistaxis related to hereditary hemorrhagic telangiectasia. Lasers Med. Sci. 2017, 32, 527–531. [Google Scholar] [CrossRef]
- Cazzador, D.; Padoan, R.; Colangeli, R.; Pendolino, A.L.; Felicetti, M.; Zanoletti, E.; Emanuelli, E.; Martini, A.; Doria, A.; Nicolai, P.; et al. Health-Related Quality of Life in Patients With ANCA-Associated Vasculitis and Sinonasal Involvement: A Single-Center Cross-Sectional Study. J. Clin. Rheumatol. 2022, 28, 89–94. [Google Scholar] [CrossRef]
- Fiorita, A.; Scarano, E.; Mastrapasqua, R.; Picciotti, P.M.; Loperfido, A.; Rizzotto, G.; Paludetti, G. Moderate OSAS and turbinate decongestion: Surgical efficacy in improving the quality of life and compliance of CPAP using Epworth score and SNOT-20 score. Acta Otorhinolaryngol. Ital. 2018, 38, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Aydin, O.; Akbay, N.O.; Buyukatalay, Z.C.; Arslan, F.; Dumlupinar, E.; Sozener, Z.C.; Gokcan, M.K.; Yildiz, O.; Demirel, Y.S.; Mungan, D. Evaluation of sinonasal involvement in patients with asthma and chronic obstructive pulmonary disease. Allergy Asthma Proc. 2024, 45, 166–172. [Google Scholar] [CrossRef] [PubMed]
| Main Features | Outcomes |
|---|---|
| n. of patients | 10 |
| M/F | 50%/50% |
| Median age | 70 years (range 45–81) |
| Histology | SCC 100% |
| Wall of origin | Lateral 60% Inferior 40% |
| Wang staging system | T1 30% T2 70% |
| Rome staging system | T1 20% T2a 30% T2b 40% T3 10% |
| N status | Negative (100%) |
| M status | Negative (100%) |
| Side Effects | At 1 Month | At 3 Months | At 6 Months |
|---|---|---|---|
| Rhinorrhea * | 100% | 70% | 50% |
| Nasal congestion | G2 (100%) | G2 (50%)–G1 (20%) | G1 50% |
| Postnasal drip | G1 (20%) | - | - |
| Sinus disorder | - | - | - |
| Sinus Pain | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tagliaferri, L.; Sciurti, E.; Fionda, B.; Loperfido, A.; Lancellotta, V.; Placidi, E.; Parrilla, C.; La Milia, M.C.; Rosa, E.; Rigante, M.; et al. PRO-NOVELTY: Patient-Reported Outcomes in NOse VEstibule interventionaL radioTherapY (brachytherapy). J. Clin. Med. 2024, 13, 4683. https://doi.org/10.3390/jcm13164683
Tagliaferri L, Sciurti E, Fionda B, Loperfido A, Lancellotta V, Placidi E, Parrilla C, La Milia MC, Rosa E, Rigante M, et al. PRO-NOVELTY: Patient-Reported Outcomes in NOse VEstibule interventionaL radioTherapY (brachytherapy). Journal of Clinical Medicine. 2024; 13(16):4683. https://doi.org/10.3390/jcm13164683
Chicago/Turabian StyleTagliaferri, Luca, Elisabetta Sciurti, Bruno Fionda, Antonella Loperfido, Valentina Lancellotta, Elisa Placidi, Claudio Parrilla, Maria Concetta La Milia, Enrico Rosa, Mario Rigante, and et al. 2024. "PRO-NOVELTY: Patient-Reported Outcomes in NOse VEstibule interventionaL radioTherapY (brachytherapy)" Journal of Clinical Medicine 13, no. 16: 4683. https://doi.org/10.3390/jcm13164683
APA StyleTagliaferri, L., Sciurti, E., Fionda, B., Loperfido, A., Lancellotta, V., Placidi, E., Parrilla, C., La Milia, M. C., Rosa, E., Rigante, M., De Angeli, M., Cornacchione, P., Galli, J., Bussu, F., & Gambacorta, M. A. (2024). PRO-NOVELTY: Patient-Reported Outcomes in NOse VEstibule interventionaL radioTherapY (brachytherapy). Journal of Clinical Medicine, 13(16), 4683. https://doi.org/10.3390/jcm13164683







