Markers of Futile Resuscitation in Traumatic Hemorrhage: A Review of the Evidence and a Proposal for Futility Time-Outs during Massive Transfusion
Abstract
:1. Introduction
1.1. Blood Product Shortages Heighten the Need for Reliable Markers of Futile Resuscitation of Severely Injured Patients
1.2. The Search for Reliable Markers of Futility Is Confounded by Varying Transfusion Practices and Measurements
1.3. Defining FR and a “Futility Index” Based on Criteria for Trauma-Induced Coagulopathy and Massive Transfusion with Laboratory and Clinical Markers
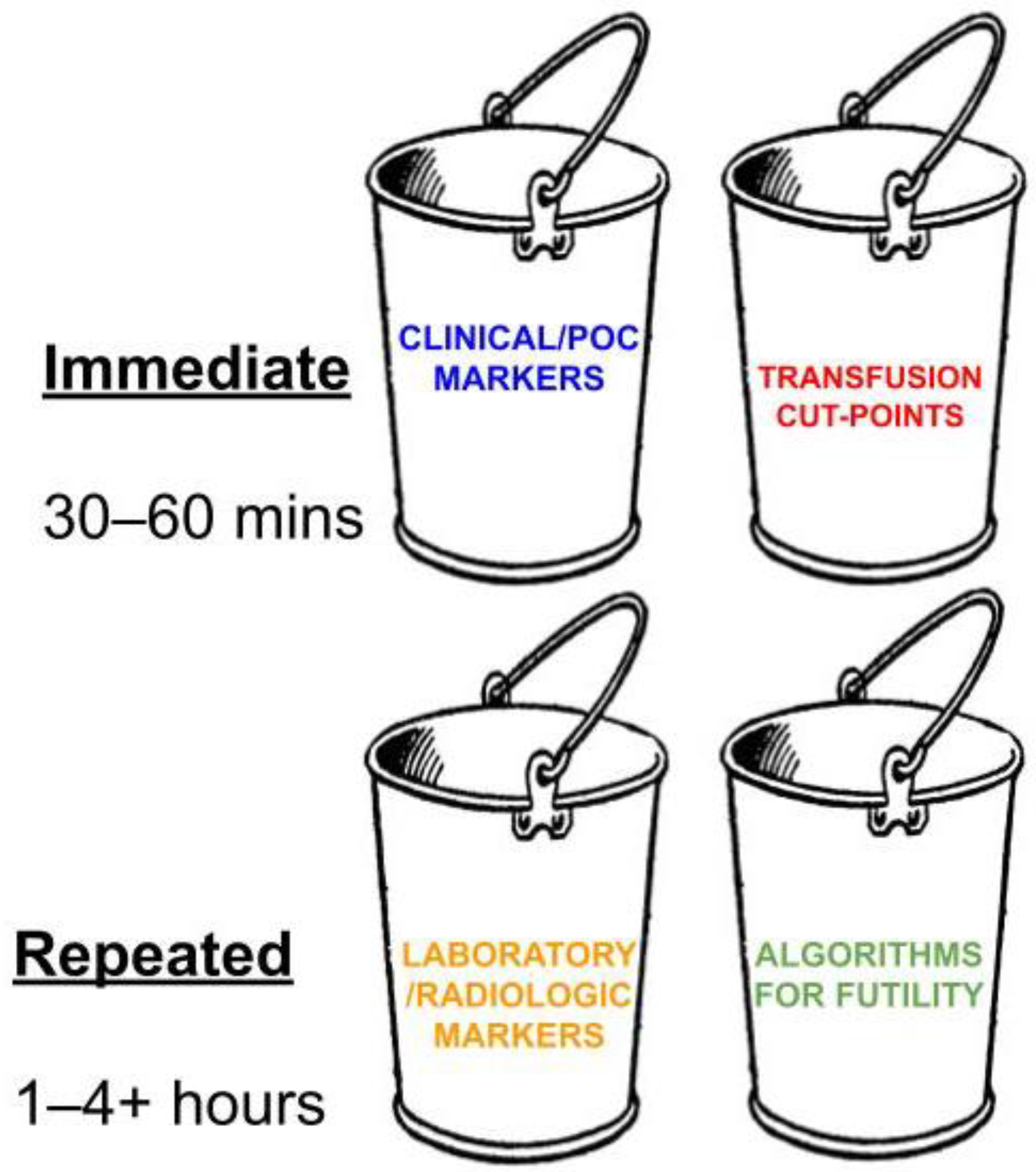
1.4. Clinical and Laboratory Measurements for Predicting FR
- (1)
- Immediate clinical/bedside POC and radiologic markers (bedside POC testing, VET POC testing, and laboratory results);
- (2)
- Transfusion cut-points;
- (3)
- Repeated laboratory and radiologic markers;
- (4)
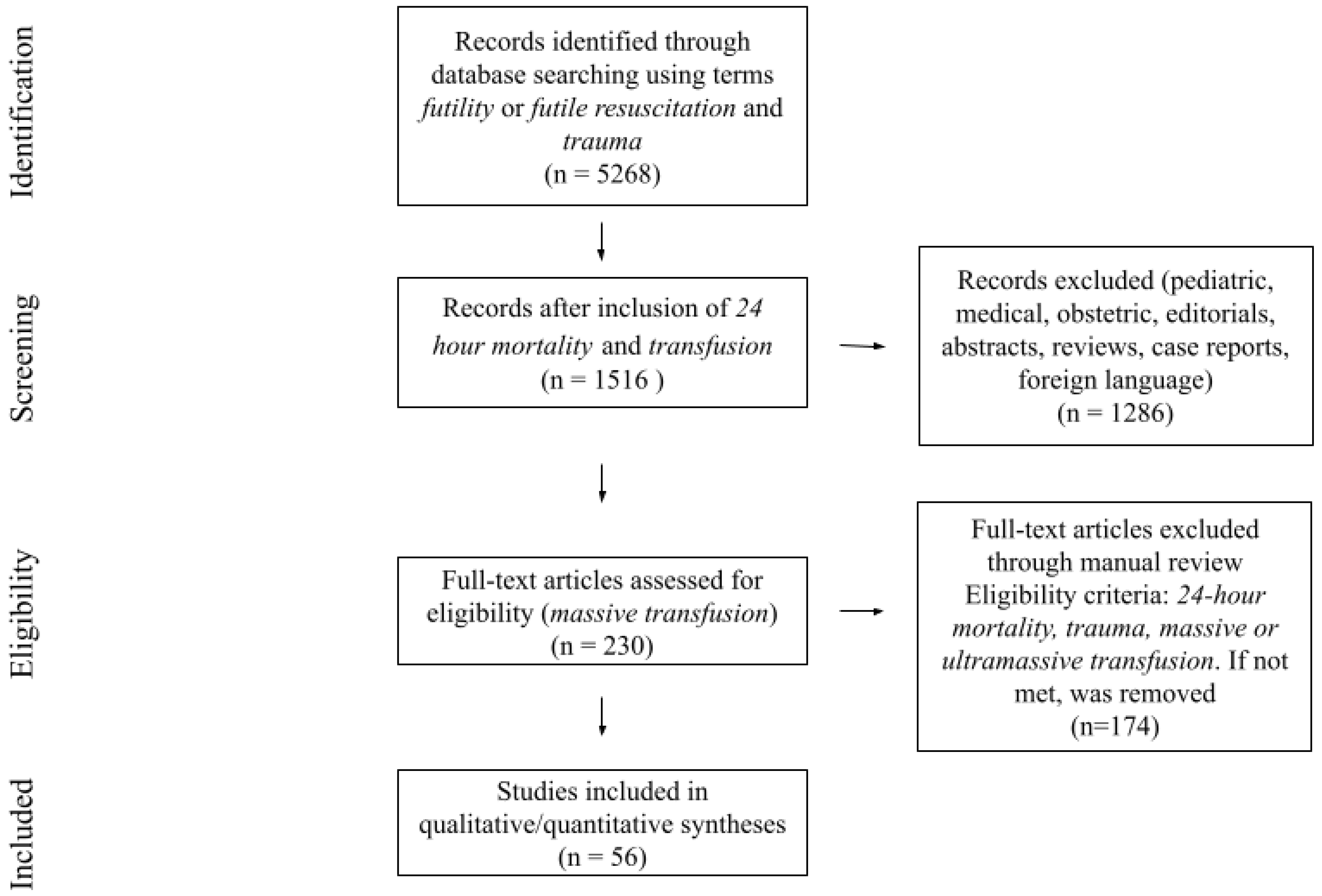
2. Methods
3. Results
| Category of Common Markers | Proposed Marker of Futility | Statistically Significant | Not Statistically Significant |
|---|---|---|---|
| Clinical markers | Age | Aichholz [103], Barbosa [104], Farrell [81], Dorken-Gallastegi [105], Hamidi [106], Huber-Wagner [107], Mitra [108], Mitra [109], Moore [110], Morris [111], Mostafa [112], Sharpe [6], Torres [113], Velmahos [114], L’Huillier [46] | Barbosa [115], Cinat [116], Criddle [117], Cripps [118], Hanna [55], Heidary [119], Katirai [120], Loudon [31], Matthay [47], Meyer [38], Mitra [121], Muldowney [85], Murray [122], Shea [123], Van Gent [41], Vaslef [59], Yang [124], Yu [53] |
| Sex | Cinat [116], Dorken-Gallastegi [105], Hamidi [106], Sharpe [6], Torres [113], Yu [53] | Barbosa [104], Barbosa [115], Criddle [117], Cripps [118], Farrell [81], Hanna [55], Heidary [119], Huber-Wagner [107], Katirai [120], Loudon [31], Matthay [47], Meyer [38], Mitra [121], Mitra [109], Moore [110], Mostafa [112], Muldowney [85], Van Gent [41], Vaslef [59], Velmahos [114], Yang [124] | |
| Race | Meyer [38], Mostafa [112], Van Gent [41], Velmahos [114] | ||
| Mechanism of injury | Dorken-Gallastegi [105], Hanna [55], Heidary [119], Mitra [108], Meyer [38], Muldowney [85], Sharpe [6], Torres [113] | Barbosa [104], Barbosa [115], Cinat [116], Cripps [118], Criddle [117], Farrell [81], Hamidi [106], Huber-Wagner [107], Loudon [31], Matthay [47], Moore [110], Mostafa [112], Vaslef [59], Van Gent [41], Velmahos [114], Yu [53] | |
| Severity of head injury | Barbosa [104], Borgman [125], Dorken-Gallastegi [105], Matthay [47], Mitra [121], Mitra [108], Muldowney [85] | Cripps [118], Hamidi [106] | |
| Traumatic arrest followed by ROSC | Aichholz [103] | Van Gent [41] | |
| GCS score | Barbosa [115], Cripps [118], Dorken-Gallastegi [105], Hamidi [106], Hanna [55], Huber-Wagner [107], Loudon [31], Matthay [47], Mitra [108], Mitra [109], Morris [111], Mostafa [112], Shea [123], Torres [113], Van Gent [41], Vaslef [59], Velmahos [114], Yu [53], Schneider [51], L’Huillier [46] | Barbosa [104] | |
| Heart rate | Dorken-Gallastegi [105], Hamidi [106], Matthay [47], Mitra [108], Torres [113] | Barbosa [104], Barbosa [115], Borgman [125], Cripps [118], Deep [126] Loudon [31], Mitra [121], Mitra [109], Moore [110], Morris [111], Velmahos [114], Yu [53] | |
| Systolic blood pressure | Borgman [125], Cosgriff [127], Cripps [118], Deep [126], Dorken-Gallastegi [105], Hamidi [106], Hanna [55], Heidary [119], Huber-Wagner [107], Loudon [31], Mitra [108], Mitra [109], Moore [110], Sharpe [6], Torres [113], Van Gent [41], Tzeng [89] | Barbosa [104], Barbosa [115], Cinat [116], Matthay [47], Mitra [121], Morris [111], Velmahos [114], Yu [53] | |
| Respiratory rate | Barbosa [115], Dorken-Gallastegi [105], Mitra [121], Mitra [109], Mitra [108] | ||
| ETCO2 | Dudaryk [128], Bryant [129], Stone [20] | ||
| Pulse oximetry and tissue oxygenation | Dorken-Gallastegi [105], Moore [110] | Velmahos [114] | |
| Temperature | Borgman [125], Cinat [116], Cosgriff [127], Mitra [121], Mitra [108], Velmahos [114] | Barbosa [104], Barbosa [115], Cripps [118], Hamidi [106], Mitra [109], Moore [110] | |
| Shock index | Arslan [15], Hosseinpour [130] | Aichholz [103], Loudon [31], Matthay [47] | |
| Aortic cross clamp | Matthay [47], Velmahos [114] | ||
| Thoracotomy | Dorken-Gallastegi [105], Loudon [31], Matthay [47], Muldowney [85], Yu [53] | Huber-Wagner [107], Van Gent [41], Velmahos [114] | |
| Endotracheal intubation | Dorken-Gallastegi [105], Hamidi [106], Huber-Wagner [107] | ||
| Presence of free fluid from FAST | Mitra 2007 [121], Velmahos [114] | ||
| Absence of cardiac activity with P-FAST | Israr [131] | ||
| Presence of REBOA balloon expansion | Anand [132] | Matthay [47] | |
| Use of inotropes | Velmahos [114] | ||
| Urgent surgery (laparotomy) | Mitra [108] | Matthay [47], Mitra [121], Yu [53] | |
| Urine output | Velmahos [114] | ||
| Laboratory markers | Base deficit/excess | Barbosa [115], Borgman [125], Cinat [116], Criddle [117], Cripps [118], Heidary [119], Huber-Wagner [107], Matthay [47], Shea [123], Van Gent [41], Vaslef [59] | Barbosa [104], Farrell [81], Moore [110] |
| pH/acidosis | Barbosa [115], Cinat [116], Cosgriff [127], Cripps [118], Katirai [120], Mitra [121], Mitra [108], Moore [110], Muldowney [85], Vaslef [59], Velmahos [114] | Barbosa [104], Farrell [81], Van Gent [41] | |
| Lactic acid level | Arslan [15], Matthay [47], Mitra [108], Sharpe [6], Shea [123], Van Gent [41] | Barbosa [104], Mitra [109], Vaslef [59] | |
| Hemoglobin/hematocrit | Barbosa [115], Borgman [125], Cripps [118], Matthay [47], Mitra [108], Moore [110] | Barbosa [104], Cinat [116], Huber-Wagner [107], Mitra [121], Mitra [109], Muldowney [85], Heidary [119], Shea [123], Vaslef [59], Velmahos [114] | |
| PT/INR/PTT | Barbosa [115], Borgman [125], Cripps [118], Heidary [119], Huber-Wagner [107], Matthay [47], Mitra [121], Mitra [108], Moore [110], Muldowney [85], Shea [123] | Barbosa [104], Mitra [109], Van Gent [41] | |
| Platelet count | Aichholz [103], Barbosa [115], Borgman [125], Cinat [116], Cripps [118], Heidary [119], Matthay [47], Mitra [121], Mitra [108], Muldowney [85], Shea [123] | Barbosa [104], Moore [110] | |
| Fibrinogen count | Cinat [116], Mitra [121], Mitra [108], Muldowney [85] | Barbosa [104], Barbosa [115] | |
| Bicarbonate | Mitra [121], Mitra [108] | Mitra [109] | |
| Serum calcium | Velmahos [114] | ||
| Serum potassium | Velmahos [114] | ||
| TEG/ROTEM | Chapman [80], Van Gent [41], Farrell [81], Shea [123] | Matthay [47] | |
| Transfusion markers | Number of blood components transfused (WB, PRBCs, FFP, platelets, with or without liquid plasma or cryoprecipitate analyzed together) | Mitra [121], Quintana [32] | Cinat [116], Clements [30], Muldowney [85], Van Gent [41], Vaslef [59], Velmahos [114] |
| Number of PRBC units transfused | Arslan [15], Barbosa [115], Cripps [118], Deep [126], Dorken-Gallastegi [105], Hamidi [106], Huber-Wagner [107], Liu [133], Loudon [31], Mitra [108], Morris [111], Mostafa [112], Quintana [32], Vaslef [59], Yang [124] | Criddle [117], Como [134], Farrell [81], Matthay [47], Mitra [109], Yu [53] | |
| Number of FFP units transfused | Cripps [118], Hamidi [106], Loudon [31], Mitra [108], Morris [111] | Cinat [116], Criddle [117], Deep [126], Farrell [81], Matthay [47], Mitra [109], Vaslef [59], Yang [124] | |
| Number of platelet units transfused | Loudon [31], Morris [111], Quintana [32] | Cinat [116], Criddle [117], Cripps [118], Farrell [81], Vaslef [59], Velmahos [114] | |
| Number of cryoprecipitate units transfused | Farrell [81], Matthay [47] | Cinat [116], Criddle [117], Vaslef [59] | |
| Whole blood transfusion | Clements [30] | Cinat [116], Muldowney [85] | |
| Number of crystalloid or colloid units transfused | Cripps [118], Deep [126], Heidary [119] | ||
| Factor VII use | Borgman [125], Matthay [47] | ||
| CAT+ | Hu [72], Meyer [38], Stone [20] | ||
| RI4+ | Hu [72], Meyer [38], Rahbar [135] | ||
| Algorithms | STOP, TIC, NBTC TTMTP | Van Gent [41], Eitel [136], Doughty [7] |
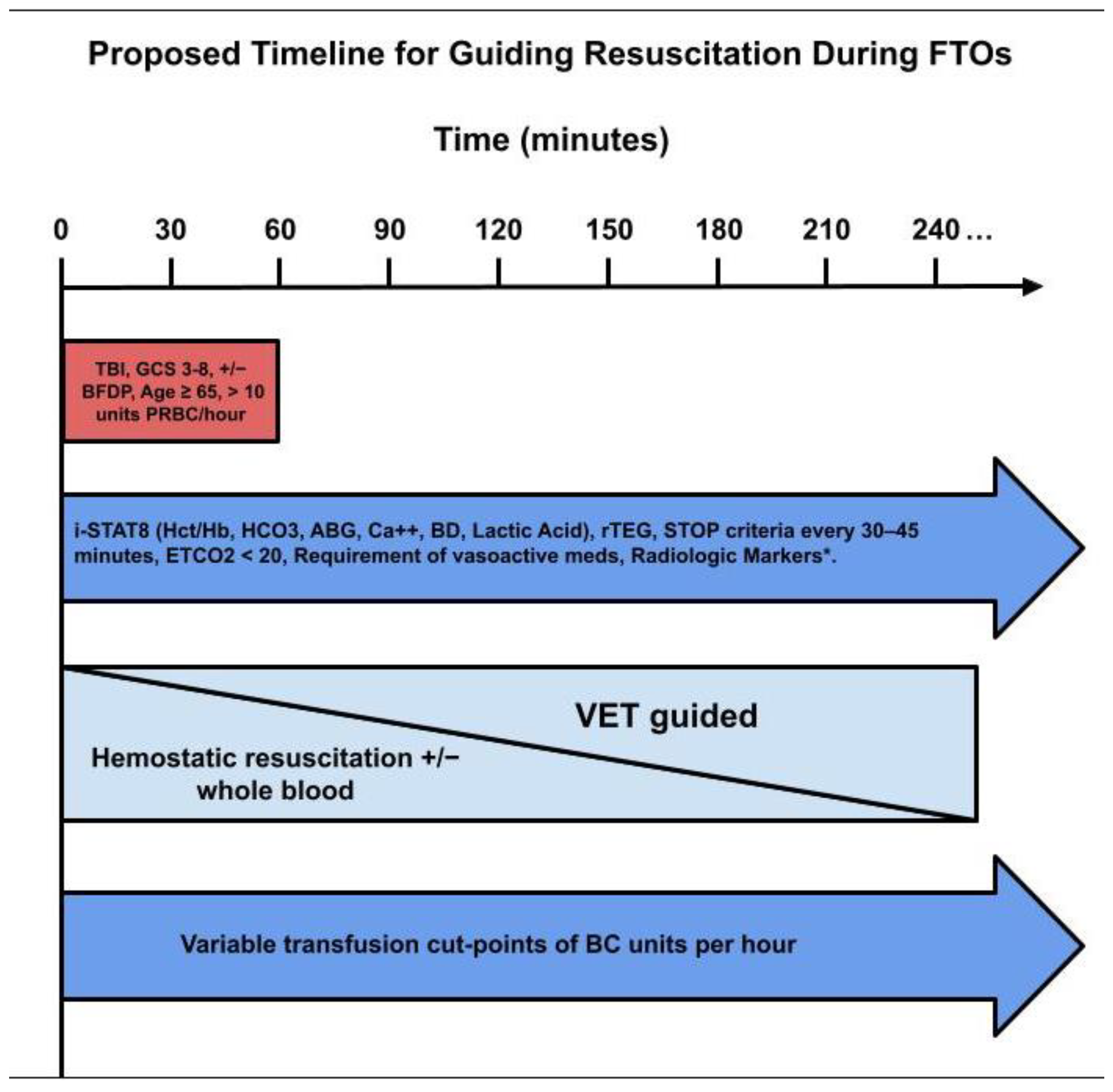
4. Discussion
4.1. Heterogeneity of the Definition of Unit of Blood Per Hour as a Predictor of FR
4.2. Bedside Algorithms Specifically for Defining FR in SBTPs
4.3. Defining Early Futility Markers during FTOs: Bedside Transfusion Cut-Points, Serial VETs, and Resolving Heterogenous Definitions of Transfusion Cut-Points
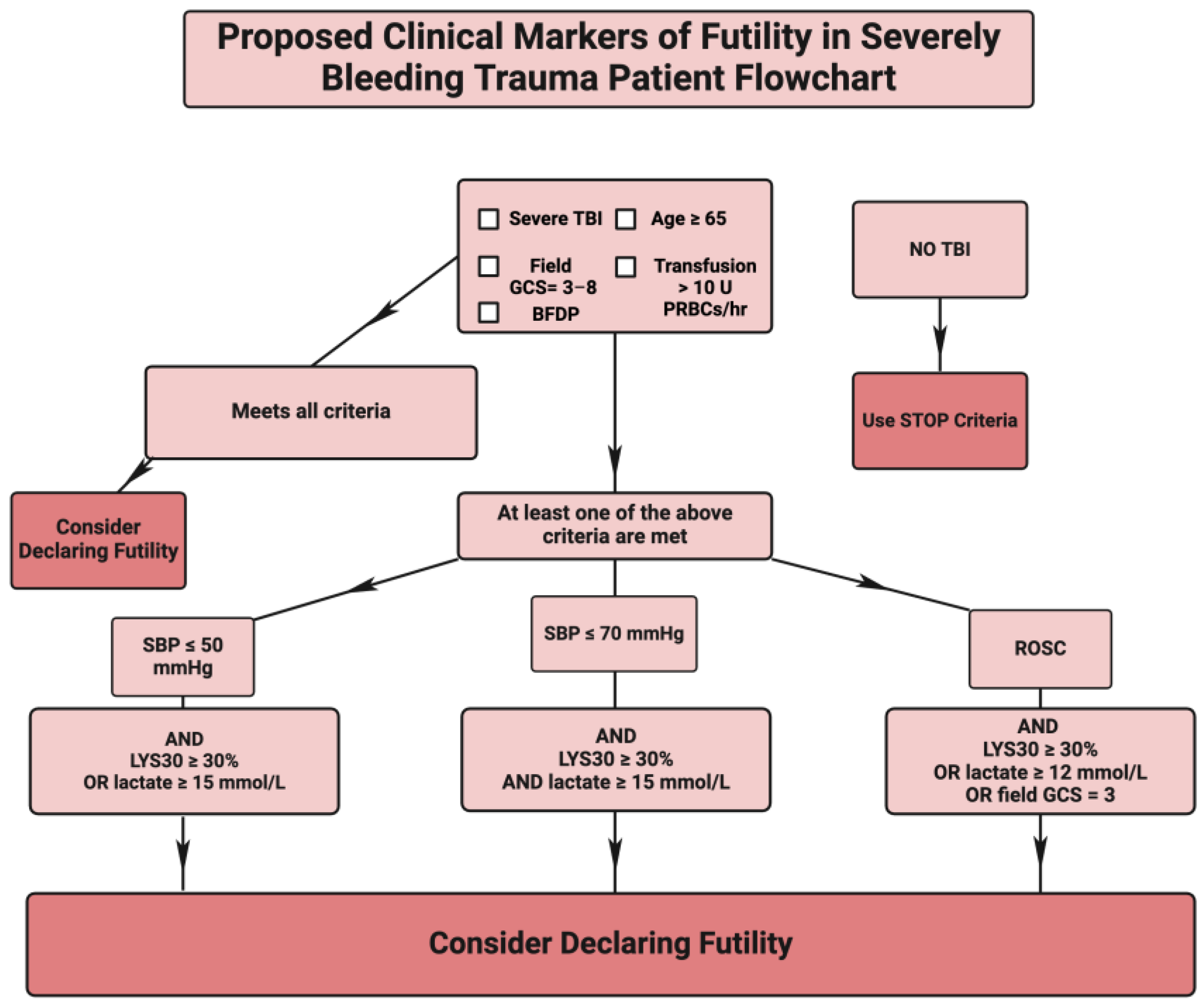
4.4. The Proposal for Defining a Futility Check List of All Bleeding Trauma Patients Who Are Candidates for FR with and without Associated TBI
5. Conclusions and Ethical Considerations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ABC | Assessment of Blood Consumption |
| ACS | American College of Surgeons |
| AIS | Abbreviated Injury Scale |
| BD | Base Deficit |
| BFDP | Bilateral Fixed and Dilated Pupils |
| CAT | Critical Administration Threshold |
| CCT | Common Coagulation Test |
| COVID-19 | Coronavirus Disease 2019 |
| CT | Computed Axial Tomography |
| cTBI | Coagulopathy of Traumatic Brain Injury |
| DD | Death Diamond |
| DDD | Double Death Diamond |
| ED | Emergency Department |
| ERAS | Edinburgh Ruptured Aneurysm Score |
| ETCO2 | End-Tidal Carbon Dioxide |
| FAST | Focused Assessment with Sonography in Trauma |
| FFP | Fresh Frozen Plasma |
| FR | Futile Resuscitation |
| FTO | Futility Time Out |
| GAS | Glasgow Aneurysm Score |
| GCS | Glasgow Coma Scale |
| GTOS | Geriatric Trauma Outcome Score |
| hMTP | Historic Massive Transfusion Protocol |
| INR | International Normalized Ratio |
| ISS | Injury Severity Score |
| LD50 | Median Lethal Dose |
| LY30 | Lysis at 30 min |
| MA | Maximum Amplitude |
| MCF | Maximum Clot Firmness |
| MELD | Model for End-Stage Liver Disease |
| MeSH | Medical Subject Headings |
| MT | Massive Transfusion |
| MTP | Massive Transfusion Protocol |
| NBTC | National Blood Transfusion Committee |
| OR | Operating Room |
| PBM | Precision-Based Medicine |
| P-FAST | Pericardial Focused Assessment with Sonography in Trauma |
| PLTs | Platelets |
| POC | Point of Care |
| POCUS | Point of Care Ultrasonography |
| PPV | Positive Predictive Value |
| PRBCs | Packed Red Blood Cells |
| PROPPR | Pragmatic Randomized Optimal Plasma and Platelet Ratio Trial |
| PT | Prothrombin Time |
| PTT | Partial Thromboplastin Time |
| rBAUX | Revised Baux Score |
| RCT | Randomized Controlled Trial |
| REBOA | Resuscitative Endovascular Balloon Occlusion of the Aorta |
| RI | Resuscitation Intensity |
| ROSC | Return of Spontaneous Circulation |
| ROTEM | Rotational Thromboelastometry |
| rTEG | Rapid Thromboelastography |
| RTO | Resuscitation Time-Outs |
| SBP | Systolic Blood Pressure |
| SHINE | SHock-INduced Endotheliopathy |
| SOFA | Sequential Organ Failure Assessment |
| SOL | Signs of Life |
| STOP | Suspension of Transfusions and Other Procedures |
| TACTIC | Trans-Agency Consortium for Trauma-Induced Coagulopathy |
| TBI | Traumatic Brain Injury |
| TEG | Thromboelastography |
| TEG LY 30 | Thromboelastography Lysis at 30 Minutes |
| TEMPT | Trauma Early Mortality Prediction Tool |
| TFT | Transfusion Futility Threshold |
| TIC | Trauma-Induced Coagulopathy |
| tPA | Tissue Plasminogen Activator |
| TRISS | Trauma Revised Injury Severity Score |
| TTMTP | Triage Tool for Massively Transfused Patients |
| TTO | Transfusion Time-Out |
| TTV | Total Transfusion Volume |
| TQIP | Trauma Quality Improvement Program |
| U | Unit |
| UMT | Ultramassive Transfusion |
| VET | Viscoelastic Testing |
| VSS | Vancouver Scoring System |
| w/o | Without |
| WB | Whole Blood |
References
- Morton, A.P.; Moore, E.E.; Wohlauer, M.V.; Lo, K.; Silliman, C.C.; Burlew, C.C.; Banerjee, A. Revisiting Early Postinjury Mortality: Are They Bleeding Because They Are Dying or Dying Because They Are Bleeding? J. Surg. Res. 2013, 179, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Hornor, M.; Khan, U.; Cripps, M.W.; Cook Chapman, A.; Knight-Davis, J.; Puzio, T.J.; Joseph, B. Futility in Acute Care Surgery: First do no Harm. Trauma Surg. Acute Care Open 2023, 8, e001167. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.H.; Nguyen, J.; ElHabr, A.; Venkatayogi, N.; Steed, T.; Gichoya, J.; Sciarretta, J.D.; Sikora, J.; Dente, C.; Lyons, J.; et al. TiME OUT: Time-Specific Machine-Learning Evaluation to Optimize Ultramassive Transfusion. J. Trauma Acute Care Surg. 2024, 96, 443–454. [Google Scholar] [CrossRef] [PubMed]
- Follette, C.; Halimeh, B.; Chaparro, A.; Shi, A.; Winfield, R. Futile Trauma Transfers: An Infrequent but Costly Component of Regionalized Trauma Care. J. Trauma Acute Care Surg. 2021, 91, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Amato, S.; Vogt, A.; Sarathy, A.; Lahey, T.; Osler, T.; Hosmer, D.; Bliss, S.; Bruzzese, C.; An, G.; Erb, A.L.; et al. Frequency and Predictors of Trauma Transfer Futility to a Rural Level I Trauma Center. J. Surg. Res. 2022, 279, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sharpe, J.P.; Weinberg, J.A.; Magnotti, L.J.; Croce, M.A.; Fabian, T.C. Toward a Better Definition of Massive Transfusion: Focus on the Interval of Hemorrhage Control. J. Trauma Acute Care Surg. 2012, 73, 1553–1557. [Google Scholar] [CrossRef] [PubMed]
- Doughty, H.; Green, L.; Callum, J.; Murphy, M.F. Triage Tool for the Rationing of Blood for Massively Bleeding Patients during a Severe National Blood Shortage: Guidance from the National Blood Transfusion Committee. Br. J. Haematol. 2020, 191, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of COVID-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Casem, C.F.; Baral, E.; Inaba, K.; Kuza, C.M. Narrative Review: Is There a Transfusion Cutoff Value After Which Nonsurvivability Is Inevitable in Trauma Patients Receiving Ultramassive Transfusion? Anesth. Analg. 2023, 137, 354–364. [Google Scholar] [CrossRef] [PubMed]
- Mladinov, D.; Frank, S.M. Massive Transfusion and Severe Blood Shortages: Establishing and Implementing Predictors of Futility. Br. J. Anaesth. 2022, 128, e71–e74. [Google Scholar] [CrossRef] [PubMed]
- Nakashima, B.; Schellenberg, M.; Gold, A.I.; Matsushima, K.; Martin, M.J.; Inaba, K. Resuscitative Thoracotomy for Traumatic Cardiac Arrest: Potential Impact of Resource Constraint on Outcomes and Blood Product Utilization. J. Surg. Res. 2024, 295, 683–689. [Google Scholar] [CrossRef] [PubMed]
- Ngo, A.; Masel, D.; Cahill, C.; Blumberg, N.; Refaai, M.A. Blood Banking and Transfusion Medicine Challenges during the COVID-19 Pandemic. Clin. Lab. Med. 2020, 40, 587–601. [Google Scholar] [CrossRef] [PubMed]
- Saillant, N.N.; Kornblith, L.Z.; Moore, H.; Barrett, C.; Schreiber, M.A.; Cotton, B.A.; Neal, M.D.; Makar, R.; Cap, A.P. The National Blood Shortage-An Impetus for Change. Ann. Surg. 2022, 275, 641–643. [Google Scholar] [CrossRef] [PubMed]
- Gammon, R.R.; Rosenbaum, L.; Cooke, R.; Friedman, M.; Rockwood, L.; Nichols, T.; Vossoughi, S. Maintaining Adequate Donations and a Sustainable Blood Supply: Lessons Learned. Transfusion 2021, 61, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Arslan, A.; Flax, L.; Fraser, R.; Kanter, M.; Simon, R.; Caputo, N.D. Twenty-Four-Hour Packed Red Blood Cell Requirement Is the Strongest Independent Prognostic Marker of Mortality in ED Trauma Patients. Am. J. Emerg. Med. 2016, 34, 1121–1124. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.W.; Adkins, B.D.; Booth, G.S. Massive Transfusion Protocols during the COVID-19 Pandemic. Vox Sang. 2022, 117, 869. [Google Scholar] [CrossRef] [PubMed]
- Pohlman, T.H.; Walsh, M.; Aversa, J.; Hutchison, E.M.; Olsen, K.P.; Lawrence Reed, R. Damage Control Resuscitation. Blood Rev. 2015, 29, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Pommerening, M.J.; Goodman, M.D.; Holcomb, J.B.; Wade, C.E.; Fox, E.E.; Del Junco, D.J.; Brasel, K.J.; Bulger, E.M.; Cohen, M.J.; Alarcon, L.H.; et al. Clinical Gestalt and the Prediction of Massive Transfusion after Trauma. Injury 2015, 46, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Stanworth, S.J.; New, H.V.; Apelseth, T.O.; Brunskill, S.; Cardigan, R.; Doree, C.; Germain, M.; Goldman, M.; Massey, E.; Prati, D.; et al. Effects of the COVID-19 Pandemic on Supply and Use of Blood for Transfusion. Lancet Haematol. 2020, 7, e756–e764. [Google Scholar] [CrossRef]
- Stone, M.E., Jr.; Kalata, S.; Liveris, A.; Adorno, Z.; Yellin, S.; Chao, E.; Reddy, S.H.; Jones, M.; Vargas, C.; Teperman, S. End-Tidal CO(2) on Admission is Associated with Hemorrhagic Shock and Predicts the Need for Massive Transfusion as Defined by the Critical Administration Threshold: A Pilot Study. Injury 2017, 48, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Braverman, M.A.; Smith, A.; Pokorny, D.; Axtman, B.; Shahan, C.P.; Barry, L.; Corral, H.; Jonas, R.B.; Shiels, M.; Schaefer, R.; et al. Prehospital Whole Blood Reduces Early Mortality in Patients with Hemorrhagic Shock. Transfusion 2021, 61 (Suppl. S1), S15–S21. [Google Scholar] [CrossRef] [PubMed]
- Gaines, B.A.; Yazer, M.H.; Triulzi, D.J.; Sperry, J.L.; Neal, M.D.; Billiar, T.R.; Leeper, C.M. Low Titer Group O Whole Blood in Injured Children Requiring Massive Transfusion. Ann. Surg. 2023, 277, e919–e924. [Google Scholar] [CrossRef] [PubMed]
- Guyette, F.X.; Zenati, M.; Triulzi, D.J.; Yazer, M.H.; Skroczky, H.; Early, B.J.; Adams, P.W.; Brown, J.B.; Alarcon, L.; Neal, M.D.; et al. Prehospital Low Titer Group O Whole Blood Is Feasible and Safe: Results of a Prospective Randomized Pilot Trial. J. Trauma Acute Care Surg. 2022, 92, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Moore, E.E.; Moore, H.B.; Thomas, S.; Kwaan, H.C.; Speybroeck, J.; Marsee, M.; Bunch, C.M.; Stillson, J.; Thomas, A.V.; et al. Whole Blood, Fixed Ratio, or Goal-Directed Blood Component Therapy for the Initial Resuscitation of Severely Hemorrhaging Trauma Patients: A Narrative Review. J. Clin. Med. 2021, 10, 320. [Google Scholar] [CrossRef] [PubMed]
- Bieler, D.; Franke, A.F.; Hentsch, S.; Paffrath, T.; Willms, A.; Lefering, R.; Kollig, E.W.; TraumaRegister, D.G.U. Gunshot and Stab Wounds in Germany--Epidemiology and Outcome: Analysis from the TraumaRegister DGU(R). Unfallchirurg 2014, 117, 995–1004. [Google Scholar] [CrossRef] [PubMed]
- Dijkink, S.; Krijnen, P.; Hage, A.; Van der Wilden, G.M.; Kasotakis, G.; Hartog, D.D.; Salim, A.; Goslings, J.C.; Bloemers, F.W.; Rhemrev, S.J.; et al. Differences in Characteristics and Outcome of Patients with Penetrating Injuries in the USA and the Netherlands: A Multi-Institutional Comparison. World J. Surg. 2018, 42, 3608–3615. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, J.B.; Minei, K.M.; Scerbo, M.L.; Radwan, Z.A.; Wade, C.E.; Kozar, R.A.; Gill, B.S.; Albarado, R.; McNutt, M.K.; Khan, S.; et al. Admission Rapid Thrombelastography Can Replace Conventional Coagulation Tests in the Emergency Department: Experience with 1974 Consecutive Trauma Patients. Ann. Surg. 2012, 256, 476–486. [Google Scholar] [CrossRef] [PubMed]
- Holcomb, J.B.; Tilley, B.C.; Baraniuk, S.; Fox, E.E.; Wade, C.E.; Podbielski, J.M.; del Junco, D.J.; Brasel, K.J.; Bulger, E.M.; Callcut, R.A.; et al. Transfusion of Plasma, Platelets, and Red Blood Cells in a 1:1:1 vs a 1:1:2 Ratio and Mortality in Patients with Severe Trauma: The PROPPR Randomized Clinical Trial. JAMA 2015, 313, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Kalkwarf, K.J.; Drake, S.A.; Yang, Y.; Thetford, C.; Myers, L.; Brock, M.; Wolf, D.A.; Persse, D.; Wade, C.E.; Holcomb, J.B. Bleeding to Death in a Big City: An Analysis of All Trauma Deaths from Hemorrhage in a Metropolitan Area during 1 Year. J. Trauma Acute Care Surg. 2020, 89, 716–722. [Google Scholar] [CrossRef]
- Clements, T.W.; Van Gent, J.M.; Lubkin, D.E.; Wandling, M.W.; Meyer, D.E.; Moore, L.J.; Cotton, B.A. The Reports of my Death are Greatly Exaggerated: An Evaluation of Futility Cut-Points in Massive Transfusion. J. Trauma Acute Care Surg. 2023, 95, 685–690. [Google Scholar] [CrossRef]
- Loudon, A.M.; Rushing, A.P.; Hue, J.J.; Ziemak, A.; Sarode, A.L.; Moorman, M.L. When Is Enough Enough? Odds of Survival by Unit Transfused. J. Trauma Acute Care Surg. 2023, 94, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Quintana, M.T.; Zebley, J.A.; Vincent, A.; Chang, P.; Estroff, J.; Sarani, B.; Forssten, M.P.; Cao, Y.; Chen, M.; Corrado, C.; et al. Cresting Mortality: Defining a Plateau in Ongoing Massive Transfusion. J. Trauma Acute Care Surg. 2022, 93, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Barnhard, S.; Klapper, E.; Kopko, P.; Tran, M.H.; Ziman, A. Too Lean: Time to Build Back True Resiliency in the National Blood Supply. Transfusion 2021, 61, 2768–2771. [Google Scholar] [CrossRef] [PubMed]
- Kornblith, L.Z.; Moore, H.B.; Cohen, M.J. Trauma-Induced Coagulopathy: The Past, Present, and Future. J. Thromb. Haemost. 2019, 17, 852–862. [Google Scholar] [CrossRef] [PubMed]
- Ngatuvai, M.; Zagales, I.; Sauder, M.; Andrade, R.; Santos, R.G.; Bilski, T.; Kornblith, L.; Elkbuli, A. Outcomes of Transfusion With Whole Blood, Component Therapy, or Both in Adult Civilian Trauma Patients: A Systematic Review and Meta-Analysis. J. Surg. Res. 2023, 287, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Ruby, K.N.; Dzik, W.H.; Collins, J.J.; Eliason, K.; Makar, R.S. Emergency Transfusion with Whole Blood Versus Packed Red Blood Cells: A Study of 1400 Patients. Transfusion 2023, 63, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Red Cross Declares First-Ever Blood Crisis Amid Omicron Surge. Available online: https://www.redcross.org/about-us/news-and-events/press-release/2022/blood-donors-needed-now-as-omicron-intensifies.html (accessed on 20 December 2023).
- Meyer, D.E.; Cotton, B.A.; Fox, E.E.; Stein, D.; Holcomb, J.B.; Cohen, M.; Inaba, K.; Rahbar, E. A Comparison of Resuscitation Intensity and Critical Administration Threshold in Predicting Early Mortality among Bleeding Patients: A Multicenter Validation in 680 Major Transfusion Patients. J. Trauma Acute Care Surg. 2018, 85, 691–696. [Google Scholar] [CrossRef] [PubMed]
- Nunns, G.R.; Moore, E.E.; Stettler, G.R.; Moore, H.B.; Ghasabyan, A.; Cohen, M.; Huebner, B.R.; Silliman, C.C.; Banerjee, A.; Sauaia, A. Empiric Transfusion Strategies during Life-Threatening Hemorrhage. Surgery 2018, 164, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.E.; Moore, H.B.; Thomas, S.G.; Farrell, M.S.; Sixta, S.; Coleman, J.R.; Miller, J.B.; Bunch, C.M.; Waxman, D.; Walsh, M.M. Serial “death diamond” TEGs are a Bedside Indicator of Futile Resuscitation during Massive Transfusion. J. Trauma Acute Care Surg. 2023, 95, e19–e21. [Google Scholar] [CrossRef] [PubMed]
- Van Gent, J.M.; Clements, T.W.; Lubkin, D.T.; Wade, C.E.; Cardenas, J.C.; Kao, L.S.; Cotton, B.A. Predicting Futility in Severely Injured Patients: Using Arrival Lab Values and Physiology to Support Evidence-Based Resource Stewardship. J. Am. Coll. Surg. 2023, 236, 874–880. [Google Scholar] [CrossRef] [PubMed]
- Cook, C. Is Clinical Gestalt Good Enough? J. Man. Manip. Ther. 2009, 17, 6–7. [Google Scholar] [CrossRef] [PubMed]
- Ranola, P.A.; Merchant, R.M.; Perman, S.M.; Khan, A.M.; Gaieski, D.; Caplan, A.L.; Kirkpatrick, J.N. How Long is Long Enough, and Have We Done Everything We Should?--Ethics of Calling Codes. J. Med. Ethics 2015, 41, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Belaunzaran, M.; Raslan, S.; Ali, A.; Newsome, K.; McKenney, M.; Elkbuli, A. Utilization and Efficacy of Resuscitation Endpoints in Trauma and Burn Patients: A Review Article. Am. Surg. 2022, 88, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Dzik, W.S.; Ziman, A.; Cohn, C.; Pai, M.; Lozano, M.; Kaufman, R.M.; Delaney, M.; Selleng, K.; Murphy, M.F.; Hervig, T.; et al. Survival after Ultramassive Transfusion: A Review of 1360 Cases. Transfusion 2016, 56, 558–563. [Google Scholar] [CrossRef] [PubMed]
- L’Huillier, J.C.; Hua, S.; Logghe, H.J.; Yu, J.; Myneni, A.A.; Noyes, K.; Guo, W.A. Transfusion Futility Thresholds and Mortality in Geriatric Trauma: Does Frailty Matter? Am. J. Surg. 2024, 228, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Matthay, Z.A.; Hellmann, Z.J.; Callcut, R.A.; Matthay, E.C.; Nunez-Garcia, B.; Duong, W.; Nahmias, J.; LaRiccia, A.K.; Spalding, M.C.; Dalavayi, S.S.; et al. Outcomes after Ultramassive Transfusion in the Modern Era: An Eastern Association for the Surgery of Trauma Multicenter Study. J. Trauma Acute Care Surg. 2021, 91, 24–33. [Google Scholar] [CrossRef] [PubMed]
- McQuilten, Z.K.; Flint, A.W.; Green, L.; Sanderson, B.; Winearls, J.; Wood, E.M. Epidemiology of Massive Transfusion—A Common Intervention in Need of a Definition. Transfus. Med. Rev. 2021, 35, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Rangarajan, K.; Subramanian, A.; Pandey, R.M. Determinants of Mortality in Trauma Patients Following Massive Blood Transfusion. J. Emerg. Trauma Shock 2011, 4, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Reppucci, M.L.; Cooper, E.; Nolan, M.M.; Lyttle, B.D.; Gallagher, L.T.; Jujare, S.; Stevens, J.; Moulton, S.L.; Bensard, D.D.; Acker, S.N. Use of Prehospital Reverse Shock Index Times Glasgow Coma Scale to Identify Children Who Require the Most Immediate Trauma Care. J. Trauma Acute Care Surg. 2023, 95, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.B.; Adams, U.; Gallaher, J.; Purcell, L.N.; Raff, L.; Eckert, M.; Charles, A. Blood Utilization and Thresholds for Mortality Following Major Trauma. J. Surg. Res. 2023, 281, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Tisherman, S.A.; Barie, P.; Bokhari, F.; Bonadies, J.; Daley, B.; Diebel, L.; Eachempati, S.R.; Kurek, S.; Luchette, F.; Carlos Puyana, J.; et al. Clinical Practice Guideline: Endpoints of Resuscitation. J. Trauma 2004, 57, 898–912. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.J.; Inaba, K.; Biswas, S.; de Leon, L.A.; Wong, M.; Benjamin, E.; Lam, L.; Demetriades, D. Supermassive Transfusion: A 15-Year Single Center Experience and Outcomes. Am. Surg. 2018, 84, 1617–1621. [Google Scholar] [CrossRef] [PubMed]
- Clements, T.; McCoy, C.; Assen, S.; Cardenas, J.; Wade, C.; Meyer, D.; Cotton, B.A. The Prehospital Use of Younger Age Whole Blood Is Associated with an Improved Arrival Coagulation Profile. J. Trauma Acute Care Surg. 2021, 90, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Hanna, K.; Bible, L.; Chehab, M.; Asmar, S.; Douglas, M.; Ditillo, M.; Castanon, L.; Tang, A.; Joseph, B. Nationwide Analysis of Whole Blood Hemostatic Resuscitation in Civilian Trauma. J. Trauma Acute Care Surg. 2020, 89, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Lo, B.D.; Merkel, K.R.; Dougherty, J.L.; Kajstura, T.J.; Cruz, N.C.; Sikorski, R.A.; Frank, S.M. Assessing Predictors of Futility in Patients Receiving Massive Transfusions. Transfusion 2021, 61, 2082–2089. [Google Scholar] [CrossRef] [PubMed]
- Wong, H.S.; Curry, N.S.; Davenport, R.A.; Yu, L.M.; Stanworth, S.J. A Delphi Study to Establish Consensus on a Definition of Major Bleeding in Adult Trauma. Transfusion 2020, 60, 3028–3038. [Google Scholar] [CrossRef] [PubMed]
- Vernon, T.E.; April, M.D.; Fisher, A.D.; Rizzo, J.A.; Long, B.J.; Schauer, S.G. An Assessment of Clinical Accuracy of Vital Sign-based Triage Tools among U.S. and Coalition Forces. Mil. Med. 2024, 189, usad500. [Google Scholar] [CrossRef] [PubMed]
- Vaslef, S.N.; Knudsen, N.W.; Neligan, P.J.; Sebastian, M.W. Massive Transfusion Exceeding 50 Units of Blood Products in Trauma Patients. J. Trauma 2002, 53, 291–295; discussion 295–296. [Google Scholar] [CrossRef] [PubMed]
- Hakala, P.; Hiippala, S.; Syrjala, M.; Randell, T. Massive Blood Transfusion Exceeding 50 Units of Plasma Poor Red Cells or Whole Blood: The Survival Rate and the Occurrence of Leukopenia and Acidosis. Injury 1999, 30, 619–622. [Google Scholar] [CrossRef] [PubMed]
- Eckstein, M. Termination of Resuscitative Efforts: Medical Futility for the Trauma Patient. Curr. Opin. Crit. Care 2001, 7, 450–454. [Google Scholar] [CrossRef] [PubMed]
- Trenga-Schein, N.; Zonies, D.; Cook, M. Goals of Care Are Rarely Discussed Prior to Potentially Futile Trauma Transfer: Is It Okay to Say “No”? J. Trauma Acute Care Surg. 2024, 96, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Ang, D.; Fakhry, S.M.; Watts, D.D.; Liu, H.; Morse, J.L.; Armstrong, J.; Ziglar, M.; Restivo, J.; Plurad, D.; Kurek, S.; et al. Data-Driven Blood Transfusion Thresholds for Severely Injured Patients During Blood Shortages. J. Surg. Res. 2023, 291, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Braverman, M.A.; Schauer, S.G.; Ciaraglia, A.; Brigmon, E.; Smith, A.A.; Barry, L.; Bynum, J.; Cap, A.D.; Corral, H.; Fisher, A.D.; et al. The Impact of Prehospital Whole Blood on Hemorrhaging Trauma Patients: A Multi-Center Retrospective Study. J. Trauma Acute Care Surg. 2023, 95, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Brill, J.B.; Tang, B.; Hatton, G.; Mueck, K.M.; McCoy, C.C.; Kao, L.S.; Cotton, B.A. Impact of Incorporating Whole Blood into Hemorrhagic Shock Resuscitation: Analysis of 1377 Consecutive Trauma Patients Receiving Emergency-Release Uncrossmatched Blood Products. J. Am. Coll. Surg. 2022, 234, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Ciaraglia, A.; Brigmon, E.; Braverman, M.; Kidd, E.; Winckler, C.J.; Epley, E.; Flores, J.; Barry, J.; DeLeon, D.; Waltman, E.; et al. Use of Whole Blood Deployment Programs for Mass Casualty Incidents: South Texas Experience in Regional Response and Preparedness. J. Trauma Acute Care Surg. 2022, 93, e182–e184. [Google Scholar] [CrossRef] [PubMed]
- Ciaraglia, A.; Myers, J.C.; Braverman, M.; Barry, J.; Eastridge, B.; Stewart, R.; Nicholson, S.; Jenkins, D. Transfusion-Related Cost Comparison of Trauma Patients Receiving Whole Blood Versus Component Therapy. J. Trauma Acute Care Surg. 2023, 95, 62–68. [Google Scholar] [CrossRef]
- Gaessler, H.; Helm, M.; Kulla, M.; Hossfeld, B.; Riedel, J.; Kerschowski, J.; Bretschneider, I. Prehospital Predictors of the Need for Transfusion in Patients with Major Trauma. Eur. J. Trauma Emerg. Surg. 2023, 49, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Hazelton, J.P.; Ssentongo, A.E.; Oh, J.S.; Ssentongo, P.; Seamon, M.J.; Byrne, J.P.; Armento, I.G.; Jenkins, D.H.; Braverman, M.A.; Mentzer, C.; et al. Use of Cold-Stored Whole Blood is Associated with Improved Mortality in Hemostatic Resuscitation of Major Bleeding: A Multicenter Study. Ann. Surg. 2022, 276, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Sperry, J.L.; Cotton, B.A.; Luther, J.F.; Cannon, J.W.; Schreiber, M.A.; Moore, E.E.; Namias, N.; Minei, J.P.; Wisniewski, S.R.; Guyette, F.X. Whole Blood Resuscitation and Association with Survival in Injured Patients with an Elevated Probability of Mortality. J. Am. Coll. Surg. 2023, 237, 206–219. [Google Scholar] [CrossRef] [PubMed]
- Yazer, M.H.; Cap, A.P.; Glassberg, E.; Green, L.; Holcomb, J.B.; Khan, M.A.; Moore, E.E.; Neal, M.D.; Perkins, G.D.; Sperry, J.L.; et al. Toward a More Complete Understanding of Who Will Benefit from Prehospital Transfusion. Transfusion 2022, 62, 1671–1679. [Google Scholar] [CrossRef] [PubMed]
- Hu, P.; Uhlich, R.; Black, J.; Jansen, J.O.; Kerby, J.; Holcomb, J.B. A New Definition for Massive Transfusion in the Modern Era of Whole Blood Resuscitation. Transfusion 2021, 61 (Suppl. S1), S252–S263. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.W.; Thomas, B.W.; Christmas, A.B.; Cunningham, K.W.; Sing, R.F. Discussion of: “Returning from the Acidotic Abyss: Mortality in Trauma Patients with a pH < 7.0”. Am. J. Surg. 2017, 214, 1073–1074. [Google Scholar] [CrossRef] [PubMed]
- Samanta, S.; Singh, R.K.; Baronia, A.K.; Mishra, P.; Poddar, B.; Azim, A.; Gurjar, M. Early pH Change Predicts Intensive Care Unit Mortality. Indian J. Crit. Care Med. 2018, 22, 697–705. [Google Scholar] [CrossRef] [PubMed]
- van Beest, P.A.; Brander, L.; Jansen, S.P.; Rommes, J.H.; Kuiper, M.A.; Spronk, P.E. Cumulative Lactate and Hospital Mortality in ICU Patients. Ann. Intensive Care 2013, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.W.; Thomas, B.W.; Christmas, A.B.; Cunningham, K.W.; Sing, R.F. Returning from the Acidotic Abyss: Mortality in Trauma Patients with a pH < 7.0. Am. J. Surg. 2017, 214, 1067–1072. [Google Scholar] [CrossRef]
- Moore, E.E.; Moore, H.B.; Kornblith, L.Z.; Neal, M.D.; Hoffman, M.; Mutch, N.J.; Schochl, H.; Hunt, B.J.; Sauaia, A. Trauma-Induced Coagulopathy. Nat. Rev. Dis. Primers 2021, 7, 30. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, J.; Walsh, M.; Grisoli, A.; Thomas, A.V.; Shariff, F.; McCauley, R.; Vande Lune, S.; Zackariya, N.; Patel, S.; Farrell, M.S.; et al. Diagnosis and Treatment of Trauma-Induced Coagulopathy by Viscoelastography. Semin. Thromb. Hemost. 2020, 46, 134–146. [Google Scholar] [CrossRef] [PubMed]
- White, N.J.; Ward, K.R.; Pati, S.; Strandenes, G.; Cap, A.P. Hemorrhagic Blood Failure: Oxygen Debt, Coagulopathy, and Endothelial Damage. J. Trauma Acute Care Surg. 2017, 82, S41–S49. [Google Scholar] [CrossRef]
- Chapman, M.P.; Moore, E.E.; Moore, H.B.; Gonzalez, E.; Morton, A.P.; Chandler, J.; Fleming, C.D.; Ghasabyan, A.; Silliman, C.C.; Banerjee, A.; et al. The “Death Diamond”: Rapid Thrombelastography Identifies Lethal Hyperfibrinolysis. J. Trauma Acute Care Surg. 2015, 79, 925–929. [Google Scholar] [CrossRef] [PubMed]
- Farrell, M.S.; Moore, E.E.; Thomas, A.V.; Coleman, J.R.; Thomas, S.; Vande Lune, S.; Marconi, T., Jr.; Cohen, M.J.; Chapman, M.P.; Moore, H.B.; et al. "Death Diamond" Tracing on Thromboelastography as a Marker of Poor Survival After Trauma. Am. Surg. 2022, 88, 1689–1693. [Google Scholar] [CrossRef]
- Farrell, M.; Marconi, T.; Getchell, J.; Green, R.; Cipolle, M.; Sixta, S. The “Death Diamond”: Death beyond Trauma. Am. Surg. 2019, 85, 757–760. [Google Scholar] [CrossRef] [PubMed]
- Neal, M.D.; Moore, H.B.; Moore, E.E.; Freeman, K.; Cohen, M.J.; Sperry, J.L.; Zuckerbraun, B.S.; Park, M.S. Clinical Assessment of Trauma-Induced Coagulopathy and Its Contribution to Postinjury Mortality: A TACTIC Proposal. J. Trauma Acute Care Surg. 2015, 79, 490–492. [Google Scholar] [CrossRef]
- Baik, D.; Yeom, S.R.; Park, S.W.; Cho, Y.; Yang, W.T.; Kwon, H.; Lee, J.I.; Ko, J.K.; Choi, H.J.; Huh, U.; et al. The Addition of Rotem Parameter Did Not Significantly Improve the Massive Transfusion Prediction in Severe Trauma Patients. Emerg. Med. Int. 2022, 2022, 7219812. [Google Scholar] [CrossRef] [PubMed]
- Muldowney, M.; Liu, Z.; Stansbury, L.G.; Vavilala, M.S.; Hess, J.R. Ultramassive Transfusion for Trauma in the Age of Hemostatic Resuscitation: A Retrospective Single-Center Cohort From a Large US Level-1 Trauma Center, 2011–2021. Anesth. Analg. 2023, 136, 927–933. [Google Scholar] [CrossRef]
- Nunez, T.C.; Dutton, W.D.; May, A.K.; Holcomb, J.B.; Young, P.P.; Cotton, B.A. Emergency Department Blood Transfusion Predicts Early Massive Transfusion and Early Blood Component Requirement. Transfusion 2010, 50, 1914–1920. [Google Scholar] [CrossRef]
- Yücel, N.; Lefering, R.; Maegele, M.; Vorweg, M.; Tjardes, T.; Ruchholtz, S.; Neugebauer, E.A.; Wappler, F.; Bouillon, B.; Rixen, D. Trauma Associated Severe Hemorrhage (Tash)-Score: Probability of Mass Transfusion as Surrogate for Life Threatening Hemorrhage after Multiple Trauma. J. Trauma 2006, 60, 1228–1236; discussion 1236–1227. [Google Scholar] [CrossRef] [PubMed]
- Van Gent, J.M.e.a. Discussion. J. Am. Coll. Surg. 2023, 236, 881–883. [Google Scholar] [CrossRef]
- Tzeng, W.J.; Tseng, H.Y.; Hou, T.Y.; Chou, S.E.; Su, W.T.; Hsu, S.Y.; Hsieh, C.H. From Death Triad to Death Tetrad-The Addition of a Hypotension Component to the Death Triad Improves Mortality Risk Stratification in Trauma Patients: A Retrospective Cohort Study. Diagnostics 2022, 12, 2885. [Google Scholar] [CrossRef] [PubMed]
- Volod, O.; Bunch, C.M.; Zackariya, N.; Moore, E.E.; Moore, H.B.; Kwaan, H.C.; Neal, M.D.; Al-Fadhl, M.D.; Patel, S.S.; Wiarda, G.; et al. Viscoelastic Hemostatic Assays: A Primer on Legacy and New Generation Devices. J. Clin. Med. 2022, 11, 860. [Google Scholar] [CrossRef] [PubMed]
- Winearls, J.; Reade, M.; Miles, H.; Bulmer, A.; Campbell, D.; Gorlinger, K.; Fraser, J.F. Targeted Coagulation Management in Severe Trauma: The Controversies and the Evidence. Anesth. Analg. 2016, 123, 910–924. [Google Scholar] [CrossRef]
- Kronstedt, S.; Roberts, N.; Ditzel, R.; Elder, J.; Steen, A.; Thompson, K.; Anderson, J.; Siegler, J. Hypocalcemia as a Predictor of Mortality and Transfusion. A Scoping Review of Hypocalcemia in Trauma and Hemostatic Resuscitation. Transfusion 2022, 62 (Suppl. S1), S158–S166. [Google Scholar] [CrossRef] [PubMed]
- Vasudeva, M.; Mathew, J.K.; Groombridge, C.; Tee, J.W.; Johnny, C.S.; Maini, A.; Fitzgerald, M.C. Hypocalcemia in Trauma Patients: A Systematic Review. J. Trauma Acute Care Surg. 2021, 90, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Wray, J.P.; Bridwell, R.E.; Schauer, S.G.; Shackelford, S.A.; Bebarta, V.S.; Wright, F.L.; Bynum, J.; Long, B. The Diamond of Death: Hypocalcemia in Trauma and Resuscitation. Am. J. Emerg. Med. 2021, 41, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Bunch, C.M.; Berquist, M.; Ansari, A.; McCoy, M.L.; Langford, J.H.; Brenner, T.J.; Aboukhaled, M.; Thomas, S.J.; Peck, E.; Patel, S.; et al. The Choice between Plasma-Based Common Coagulation Tests and Cell-Based Viscoelastic Tests in Monitoring Hemostatic Competence: Not an Either-Or Proposition. Semin. Thromb. Hemost. 2022, 48, 769–784. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Fries, D.; Moore, E.; Moore, H.; Thomas, S.; Kwaan, H.C.; Marsee, M.K.; Grisoli, A.; McCauley, R.; Lune, S.V. Whole Blood for Civilian Urban Trauma Resuscitation: Historical, Present, and Future Considerations. Semin. Thromb. Hemost. 2020, 46, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Stettler, G.R.; Moore, E.E.; Moore, H.B.; Nunns, G.R.; Silliman, C.C.; Banerjee, A.; Sauaia, A. Redefining Postinjury Fibrinolysis Phenotypes Using Two Viscoelastic Assays. J. Trauma Acute Care Surg. 2019, 86, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Stettler, G.R.; Moore, E.E.; Nunns, G.R.; Chandler, J.; Peltz, E.; Silliman, C.C.; Banerjee, A.; Sauaia, A. Rotational Thromboelastometry Thresholds for Patients at Risk for Massive Transfusion. J. Surg. Res. 2018, 228, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Stettler, G.R.; Sumislawski, J.J.; Moore, E.E.; Nunns, G.R.; Kornblith, L.Z.; Conroy, A.S.; Callcut, R.A.; Silliman, C.C.; Banerjee, A.; Cohen, M.J.; et al. Citrated Kaolin Thrombelastography (TEG) Thresholds for Goal-Directed Therapy in Injured Patients Receiving Massive Transfusion. J. Trauma Acute Care Surg. 2018, 85, 734–740. [Google Scholar] [CrossRef] [PubMed]
- Chinn, M.; Colella, M.R. Trauma Resuscitation: An Evidence-Based Review of Prehospital Traumatic Cardiac Arrest. JEMS 2017, 42, 26–32. [Google Scholar] [PubMed]
- Millin, M.G.; Galvagno, S.M.; Khandker, S.R.; Malki, A.; Bulger, E.M. Withholding and Termination of Resuscitation of Adult Cardiopulmonary Arrest Secondary to Trauma: Resource Document to the Joint NAEMSP-ACSCOT Position Statements. J. Trauma Acute Care Surg. 2013, 75, 459–467. [Google Scholar] [CrossRef]
- Rethlefsen, M.L.; Kirtley, S.; Waffenschmidt, S.; Ayala, A.P.; Moher, D.; Page, M.J.; Koffel, J.B. PRISMA-S: An Extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst. Rev. 2021, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Aichholz, P.K.; Lee, S.A.; Farr, C.K.; Tsang, H.C.; Vavilala, M.S.; Stansbury, L.G.; Hess, J.R. Platelet Transfusion and Outcomes After Massive Transfusion Protocol Activation for Major Trauma: A Retrospective Cohort Study. Anesth. Analg. 2022, 135, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, R.R.; Rowell, S.E.; Diggs, B.S.; Schreiber, M.A.; Group, T.O. Profoundly Abnormal Initial Physiologic and Biochemical Data Cannot Be Used to Determine Futility in Massively Transfused Trauma Patients. J. Trauma Acute Care Surg. 2011, 71, S364–S369. [Google Scholar] [CrossRef] [PubMed]
- Dorken Gallastegi, A.; Secor, J.D.; Maurer, L.R.; Dzik, W.S.; Saillant, N.N.; Hwabejire, J.O.; Fawley, J.; Parks, J.; Kaafarani, H.M.; Velmahos, G.C. Role of Transfusion Volume and Transfusion Rate as Markers of Futility During Ultramassive Blood Transfusion in Trauma. J. Am. Coll. Surg. 2022, 235, 468–480. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, M.; Zeeshan, M.; Kulvatunyou, N.; Adun, E.; O’Keeffe, T.; Zakaria, E.R.; Gries, L.; Joseph, B. Outcomes After Massive Transfusion in Trauma Patients: Variability among Trauma Centers. J. Surg. Res. 2019, 234, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Huber-Wagner, S.; Qvick, M.; Mussack, T.; Euler, E.; Kay, M.V.; Mutschler, W.; Kanz, K.G. Massive Blood Transfusion and Outcome in 1062 Polytrauma Patients: A Prospective Study Based on the Trauma Registry of the German Trauma Society. Vox Sang. 2007, 92, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Mitra, B.; Mori, A.; Cameron, P.A.; Fitzgerald, M.; Paul, E.; Street, A. Fresh Frozen Plasma (FFP) Use during Massive Blood Transfusion in Trauma Resuscitation. Injury 2010, 41, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Mitra, B.; Olaussen, A.; Cameron, P.A.; O’Donohoe, T.; Fitzgerald, M. Massive Blood Transfusions Post Trauma in the Elderly Compared to Younger Patients. Injury 2014, 45, 1296–1300. [Google Scholar] [CrossRef] [PubMed]
- Moore, F.A.; Nelson, T.; McKinley, B.A.; Moore, E.E.; Nathens, A.B.; Rhee, P.; Puyana, J.C.; Beilman, G.J.; Cohn, S.M. Massive Transfusion in Trauma Patients: Tissue Hemoglobin Oxygen Saturation Predicts Poor Outcome. J. Trauma 2008, 64, 1010–1023. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.C.; Niziolek, G.M.; Baker, J.E.; Huebner, B.R.; Hanseman, D.; Makley, A.T.; Pritts, T.A.; Goodman, M.D. Death by Decade: Establishing a Transfusion Ceiling for Futility in Massive Transfusion. J. Surg. Res. 2020, 252, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Mostafa, G.; Gunter, O.L.; Norton, H.J.; McElhiney, B.M.; Bailey, D.F.; Jacobs, D.G. Age, Blood Transfusion, and Survival after Trauma. Am. Surg. 2004, 70, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Torres, C.M.; Kent, A.; Scantling, D.; Joseph, B.; Haut, E.R.; Sakran, J.V. Association of Whole Blood With Survival among Patients Presenting With Severe Hemorrhage in US and Canadian Adult Civilian Trauma Centers. JAMA Surg. 2023, 158, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Velmahos, G.C.; Chan, L.; Chan, M.; Tatevossian, R.; Cornwell III, E.E.; Asensio, J.A.; Berne, T.V.; Demetriades, D. Is There a Limit to Massive Blood Transfusion after Severe Trauma? Arch. Surg. 1998, 133, 947–952. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, R.R.; Rowell, S.E.; Sambasivan, C.N.; Diggs, B.S.; Spinella, P.C.; Schreiber, M.A.; Holcomb, J.B.; Wade, C.E.; Brasel, K.J.; Vercruysse, G.; et al. A Predictive Model for Mortality in Massively Transfused Trauma Patients. J. Trauma 2011, 71, S370–S374. [Google Scholar] [CrossRef] [PubMed]
- Cinat, M.E.; Wallace, W.C.; Nastanski, F.; West, J.; Sloan, S.; Ocariz, J.; Wilson, S.E. Improved Survival Following Massive Transfusion in Patients Who Have Undergone Trauma. Arch. Surg. 1999, 134, 964–968; discussion 968–970. [Google Scholar] [CrossRef] [PubMed]
- Criddle, L.M.; Eldredge, D.H.; Walker, J. Variables Predicting Trauma Patient Survival Following Massive Transfusion. J. Emerg. Nurs. 2005, 31, 236–242; quiz 320. [Google Scholar] [CrossRef] [PubMed]
- Cripps, M.W.; Kutcher, M.E.; Daley, A.; McCreery, R.C.; Greenberg, M.D.; Cachola, L.M.; Redick, B.J.; Nelson, M.F.; Cohen, M.J. Cause and Timing of Death in Massively Transfused Trauma Patients. J. Trauma Acute Care Surg. 2013, 75, S255–S262. [Google Scholar] [CrossRef]
- Heidary, B.; Bell, N.; Ngai, J.T.; Simons, R.K.; Chipperfield, K.; Hameed, S.M. Temporal Trends in the Treatment of Severe Traumatic Hemorrhage. Am. J. Surg. 2012, 203, 568–573. [Google Scholar] [CrossRef]
- Katirai, A.; Landau, M.J.; Berger, J.M. The Utility of Abnormal Initial Arterial Blood Gas Values in Determining Clinical Futility of Trauma Cases with Severe Hemorrhage. Am. J. Emerg. Med. 2018, 36, 1253–1256. [Google Scholar] [CrossRef] [PubMed]
- Mitra, B.; Mori, A.; Cameron, P.A.; Fitzgerald, M.; Street, A.; Bailey, M. Massive Blood Transfusion and Trauma Resuscitation. Injury 2007, 38, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Barber, R.M.; Foreman, K.J.; Abbasoglu Ozgoren, A.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Abraham, J.P.; Abubakar, I.; Abu-Raddad, L.J.; et al. Global, Regional, and National Disability-Adjusted Life Years (DALYs) for 306 Diseases and Injuries and Healthy Life Expectancy (HALE) for 188 Countries, 1990–2013: Quantifying the Epidemiological Transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef] [PubMed]
- Shea, S.M.; Staudt, A.M.; Thomas, K.A.; Schuerer, D.; Mielke, J.E.; Folkerts, D.; Lowder, E.; Martin, C.; Bochicchio, G.V.; Spinella, P.C. The Use of Low-Titer Group O Whole Blood is Independently Associated with Improved Survival Compared to Component Therapy in Adults with Severe Traumatic Hemorrhage. Transfusion 2020, 60 (Suppl. S3), S2–S9. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.C.; Sun, Y.; Xu, C.X.; Dang, Q.L.; Li, L.; Xu, Y.G.; Song, Y.J.; Yan, H. Correlation between Red Blood Cell Transfusion Volume and Mortality in Patients with Massive Blood Transfusion: A Large Multicenter Retrospective Study. Exp. Ther. Med. 2015, 9, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Borgman, M.A.; Spinella, P.C.; Perkins, J.G.; Grathwohl, K.W.; Repine, T.; Beekley, A.C.; Sebesta, J.; Jenkins, D.; Wade, C.E.; Holcomb, J.B. The Ratio of Blood Products Transfused Affects Mortality in Patients Receiving Massive Transfusions at a Combat support Hospital. J. Trauma 2007, 63, 805–813. [Google Scholar] [CrossRef] [PubMed]
- Deeb, A.P.; Guyette, F.X.; Daley, B.J.; Miller, R.S.; Harbrecht, B.G.; Claridge, J.A.; Phelan, H.A.; Eastridge, B.J.; Joseph, B.; Nirula, R.; et al. Time to Early Resuscitative Intervention Association with Mortality in Trauma Patients at Risk for Hemorrhage. J. Trauma Acute Care Surg. 2023, 94, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Cosgriff, N.; Moore, E.E.; Sauaia, A.; Kenny-Moynihan, M.; Burch, J.M.; Galloway, B. Predicting Life-Threatening Coagulopathy in the Massively Transfused Trauma Patient: Hypothermia and Acidoses Revisited. J. Trauma 1997, 42, 857–861; discussion 861–852. [Google Scholar] [CrossRef] [PubMed]
- Dudaryk, R.; Bodzin, D.K.; Ray, J.J.; Jabaley, C.S.; McNeer, R.R.; Epstein, R.H. Low End-Tidal Carbon Dioxide at the Onset of Emergent Trauma Surgery Is Associated with Nonsurvival: A Case Series. Anesth. Analg. 2017, 125, 1261–1266. [Google Scholar] [CrossRef] [PubMed]
- Bryant, M.K.; Portelli Tremont, J.N.; Patel, Z.; Cook, N.; Udekwu, P.; Reid, T.; Maine, R.G.; Moore, S.M. Low Initial Pre-Hospital End-Tidal Carbon Dioxide Predicts Inferior Clinical Outcomes in Trauma Patients. Injury 2021, 52, 2502–2507. [Google Scholar] [CrossRef]
- Hosseinpour, H.; Magnotti, L.J.; Bhogadi, S.K.; Anand, T.; El-Qawaqzeh, K.; Ditillo, M.; Colosimo, C.; Spencer, A.; Nelson, A.; Joseph, B. Time to Whole Blood Transfusion in Hemorrhaging Civilian Trauma Patients: There Is Always Room for Improvement. J. Am. Coll. Surg. 2023, 237, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Israr, S.; Cook, A.D.; Chapple, K.M.; Jacobs, J.V.; McGeever, K.P.; Tiffany, B.R.; Schultz, S.P.; Petersen, S.R.; Weinberg, J.A. Pulseless Electrical Activity Following Traumatic Cardiac Arrest: Sign of Life or Death? Injury 2019, 50, 1507–1510. [Google Scholar] [CrossRef] [PubMed]
- Anand, T.; El-Qawaqzeh, K.; Nelson, A.; Hosseinpour, H.; Ditillo, M.; Gries, L.; Castanon, L.; Joseph, B. Association Between Hemorrhage Control Interventions and Mortality in US Trauma Patients With Hemodynamically Unstable Pelvic Fractures. JAMA Surg. 2023, 158, 63–71. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Fujii, Q.; Serio, F.; McCague, A. Massive Blood Transfusions and Outcomes in Trauma Patients; An Intention to Treat Analysis. Bull. Emerg. Trauma 2018, 6, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Como, J.J.; Dutton, R.P.; Scalea, T.M.; Edelman, B.B.; Hess, J.R. Blood Transfusion Rates in the Care of Acute Trauma. Transfusion 2004, 44, 809–813. [Google Scholar] [CrossRef] [PubMed]
- Rahbar, E.; Fox, E.E.; del Junco, D.J.; Harvin, J.A.; Holcomb, J.B.; Wade, C.E.; Schreiber, M.A.; Rahbar, M.H.; Bulger, E.M.; Phelan, H.A.; et al. Early Resuscitation Intensity as a Surrogate for Bleeding Severity and Early Mortality in the PROMMTT Study. J. Trauma Acute Care Surg. 2013, 75, S16–S23. [Google Scholar] [CrossRef]
- Eitel, A.P.; Moore, E.E.; Sauaia, A.; Kelher, M.R.; Vigneshwar, N.G.; Bartley, M.G.; Hadley, J.B.; Burlew, C.C.; Campion, E.M.; Fox, C.J.; et al. A Proposed Clinical Coagulation Score for Research in Trauma-Induced Coagulopathy. J. Trauma Acute Care Surg. 2023, 94, 798–802. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.J.; Scott, A.V.; Barodka, V.M.; Park, S.; Wasey, J.O.; Ness, P.M.; Gniadek, T.; Frank, S.M. Morbidity and Mortality after High-Dose Transfusion. Anesthesiology 2016, 124, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Patel, E.U.; Ness, P.M.; Marshall, C.E.; Gniadek, T.; Efron, D.T.; Miller, P.M.; Zeitouni, J.A.; King, K.E.; Bloch, E.M.; Tobian, A.A.R. Blood Product Utilization Among Trauma and Nontrauma Massive Transfusion Protocols at an Urban Academic Medical Center. Anesth. Analg. 2017, 125, 967–974. [Google Scholar] [CrossRef] [PubMed]
- Gurney, J.M.; Staudt, A.M.; Holcomb, J.B.; Martin, M.; Spinella, P.; Corley, J.B.; Rohrer, A.J.; Trevino, J.D.; Del Junco, D.J.; Cap, A.; et al. Finding the Bleeding Edge: 24-Hour Mortality by Unit of Blood Product Transfused in Combat Casualties from 2002–2020. J. Trauma Acute Care Surg. 2023, 95, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Sumislawski, J.J.; Zarzaur, B.L.; Dutton, W.P.; Croce, M.A.; Fabian, T.C. The New Metric to Define Large-Volume Hemorrhage: Results of a Prospective Study of the Critical Administration Threshold. J. Trauma Acute Care Surg. 2015, 78, 224–229; discussion 229–230. [Google Scholar] [CrossRef] [PubMed]
- Savage, S.A.; Zarzaur, B.L.; Croce, M.A.; Fabian, T.C. Redefining Massive Transfusion When Every Second Counts. J. Trauma Acute Care Surg. 2013, 74, 396–400; discussion 400–392. [Google Scholar] [CrossRef] [PubMed]
- Sihler, K.C.; Napolitano, L.M. Massive Transfusion: New Insights. Chest 2009, 136, 1654–1667. [Google Scholar] [CrossRef] [PubMed]
- Zatta, A.J.; McQuilten, Z.K.; Mitra, B.; Roxby, D.J.; Sinha, R.; Whitehead, S.; Dunkley, S.; Kelleher, S.; Hurn, C.; Cameron, P.A.; et al. Elucidating the Clinical Characteristics of Patients Captured Using Different Definitions of Massive Transfusion. Vox Sang. 2014, 107, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Beckermann, J.; Swartz, H.; Albright, J.; Street, W.; Martin, S.; Hagen, C.; Linnaus, M.; Ciresi, D. Achieving Optimal Massive Transfusion Ratios: The Trauma White Board, Whole Blood, and Liquid Plasma. Real World Low-Tech Solutions for a High Stakes Issue. Injury 2022, 53, 2974–2978. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.S.; Karam, B.S.; Murphy, P.B.; Jenkins, P.; Milia, D.J.; Hemmila, M.R.; Haines, K.L.; Puzio, T.J.; de Moya, M.A.; Tignanelli, C.J. Field-Triage, Hospital-Triage and Triage-Assessment: A Literature Review of the Current Phases of Adult Trauma Triage. J. Trauma Acute Care Surg. 2021, 90, e138–e145. [Google Scholar] [CrossRef] [PubMed]
- Kunitake, R.C.; Kornblith, L.Z.; Cohen, M.J.; Callcut, R.A. Trauma Early Mortality Prediction Tool (TEMPT) for Assessing 28-Day Mortality. Trauma Surg. Acute Care Open 2018, 3, e000131. [Google Scholar] [CrossRef] [PubMed]
- Fu, C.Y.; Bajani, F.; Bokhari, M.; Starr, F.; Messer, T.; Kaminsky, M.; Dennis, A.; Schlanser, V.; Mis, J.; Poulakidas, S.; et al. Age Itself or Age-Associated Comorbidities? A Nationwide Analysis of Outcomes of Geriatric Trauma. Eur. J. Trauma Emerg Surg. 2022, 48, 2873–2880. [Google Scholar] [CrossRef] [PubMed]
- Joseph, B.; Pandit, V.; Zangbar, B.; Kulvatunyou, N.; Tang, A.; O’Keeffe, T.; Green, D.J.; Vercruysse, G.; Fain, M.J.; Friese, R.S.; et al. Validating Trauma-Specific Frailty Index for Geriatric Trauma Patients: A Prospective Analysis. J. Am. Coll. Surg. 2014, 219, 10-17e11. [Google Scholar] [CrossRef] [PubMed]
- Edgar, M.C.; Bond, S.M.; Jiang, S.H.; Scharf, I.M.; Bejarano, G.; Vrouwe, S.Q. The Revised Baux Score as a Predictor of Burn Mortality: A Systematic Review and Meta-Analysis. J. Burn. Care Res. 2023, 44, 1278–1288. [Google Scholar] [CrossRef] [PubMed]
- Roberts, G.; Lloyd, M.; Parker, M.; Martin, R.; Philp, B.; Shelley, O.; Dziewulski, P. The Baux Score Is Dead. Long Live the Baux Score: A 27-Year Retrospective Cohort Study of Mortality at a Regional Burns Service. J. Trauma Acute Care Surg. 2012, 72, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Zhao, F.Z.; Wolf, S.E.; Nakonezny, P.A.; Minhajuddin, A.; Rhodes, R.L.; Paulk, M.E.; Phelan, H.A. Estimating Geriatric Mortality after Injury Using Age, Injury Severity, and Performance of a Transfusion: The Geriatric Trauma Outcome Score. J. Palliat. Med. 2015, 18, 677–681. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.; Kuza, C.M. Predicting Mortality in Elderly Trauma Patients: A Review of the Current Literature. Curr. Opin. Anesthesiol. 2022, 35, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.C.; Joseph, B.; Inaba, K.; Nakonezny, P.A.; Bruns, B.R.; Kerby, J.D.; Brasel, K.J.; Wolf, S.E.; Cuschieri, J.; Paulk, M.E.; et al. Multicenter External Validation of the Geriatric Trauma Outcome Score: A Study by the Prognostic Assessment of Life and Limitations after Trauma in the Elderly (Palliate) Consortium. J. Trauma Acute Care Surg. 2016, 80, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Y.; Feng, Q.; Tang, H.; Wang, Y.; Li, Z.; Bai, X. Predictive Value of the Geriatric Trauma Outcome Score in Older Patients after Trauma: A Retrospective Cohort Study. Int. J. Gen. Med. 2022, 15, 4379–4390. [Google Scholar] [CrossRef] [PubMed]
- Copes, W.S.; Champion, H.R.; Sacco, W.J.; Lawnick, M.M.; Keast, S.L.; Bain, L.W. The Injury Severity Score Revisited. J. Trauma Acute Care Surg. 1988, 28, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Mann, K.G.; Freeman, K. TACTIC: Trans-Agency Consortium for Trauma-Induced Coagulopathy. J. Thromb Haemost. 2015, 13 (Suppl. S1), S63–S71. [Google Scholar] [CrossRef]
- Meizoso, J.P.; Moore, E.E.; Pieracci, F.M.; Saberi, R.A.; Ghasabyan, A.; Chandler, J.; Namias, N.; Sauaia, A. Role of Fibrinogen in Trauma-Induced Coagulopathy. J. Am. Coll. Surg. 2022, 234, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Samuels, J.M.; Moore, E.E.; Silliman, C.C.; Banerjee, A.; Cohen, M.J.; Ghasabyan, A.; Chandler, J.; Coleman, J.R.; Sauaia, A. Severe Traumatic Brain Injury Is Associated with a Unique Coagulopathy Phenotype. J. Trauma Acute Care Surg. 2019, 86, 686. [Google Scholar] [CrossRef] [PubMed]
- Majdan, M.; Steyerberg, E.W.; Nieboer, D.; Mauritz, W.; Rusnak, M.; Lingsma, H.F. Glasgow Coma Scale Motor Score and Pupillary Reaction to Predict Six-Month Mortality in Patients with Traumatic Brain Injury: Comparison of Field and Admission Assessment. J. Neurotrauma 2015, 32, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Liang, J.J.; Wang, Z.; Winans, N.J.; Morris, M.; Doyle, S.; Fry, A.; Fiore, S.M.; Mofakham, S.; Mikell, C.B. Cardiac Arrest after Severe Traumatic Brain Injury can Be Survivable with Good Outcomes. Trauma Surg. Acute Care Open 2021, 6, e000638. [Google Scholar] [CrossRef] [PubMed]
- Yeh, C.H.; Wu, S.C.; Chou, S.E.; Su, W.T.; Tsai, C.H.; Li, C.; Hsu, S.Y.; Hsieh, C.H. Geriatric Nutritional Risk Index as a Tool to Evaluate Impact of Malnutrition Risk on Mortality in Adult Patients with Polytrauma. Int. J. Env. Res. Public Health 2020, 17, 9233. [Google Scholar] [CrossRef] [PubMed]
- Kalkwarf, K.J.; Jensen, S.D.; Allukian III, M.; Harting, M.T.; Cox, C.S.; Fox, E.E.; Wade, C.E.; Cotton, B.A. Can We Identify Futility in Kids? An Evaluation of Admission Parameters Predicting 100% Mortality in 1292 Severely Injured Children. J. Am. Coll. Surg. 2018, 226, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Al-Fadhl, M.D.; Karam, M.N.; Chen, J.; Zackariya, S.K.; Lain, M.C.; Bales, J.R.; Higgins, A.B.; Laing, J.T.; Wang, H.S.; Andrews, M.G.; et al. Traumatic Brain Injury as an Independent Predictor of Futility in the Early Resuscitation of Patients in Hemorrhagic Shock. J. Clin. Med. 2024, 13, 3915. [Google Scholar] [CrossRef] [PubMed]
- Morris, R.S.; Milia, D.; Glover, J.; Napolitano, L.M.; Chen, B.; Lindemann, E.; Hemmila, M.R.; Stein, D.; Kummerfeld, E.; Chipman, J.; et al. Predictors of Elderly Mortality after Trauma: A Novel Outcome Score. J. Trauma Acute Care Surg. 2019, 88, 416–424. [Google Scholar] [CrossRef] [PubMed]
- Robertson, R.; Eidt, J.; Bitzer, L.; Wallace, B.; Collins, T.; Parks-Miller, C.; Cone, J. Severe Acidosis Alone Does not Predict Mortality in the Trauma Patient. Am. J. Surg. 1995, 170, 691–694; discussion 694–695. [Google Scholar] [CrossRef] [PubMed]
- Mitterecker, A.; Hofmann, A.; Trentino, K.M.; Lloyd, A.; Leahy, M.F.; Schwarzbauer, K.; Tschoellitsch, T.; Böck, C.; Hochreiter, S.; Meier, J. Machine Learning-Based Prediction of Transfusion. Transfusion 2020, 60, 1977–1986. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.T.; Siddiqui, M.M.; Rhind, S.G.; Zhang, J.; da Luz, L.T.; Beckett, A. Artificial Intelligence and Machine Learning for Hemorrhagic Trauma Care. Mil. Med. Res. 2023, 10, 6. [Google Scholar] [CrossRef] [PubMed]
- Wears, R.L. Standardisation and Its Discontents. Cogn. Technol. Work 2015, 17, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.; Kryzanski, J. Prognosis and Futility in Neurosurgical Emergencies: A Review. Clin. Neurol. Neurosurg. 2020, 195, 105851. [Google Scholar] [CrossRef] [PubMed]
- Neal, C.J.; Bell, R.S.; Carmichael, J.J.; DuBose, J.J.; Grabo, D.J.; Oh, J.S.; Remick, K.N.; Bailey, J.A.; Stockinger, Z.T. Catastrophic Non-Survivable Brain Injury Care-Role 2/3. Mil. Med. 2018, 183, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Zakrison, T.L.; Essig, R.; Polcari, A.; McKinley, W.; Arnold, D.; Beyene, R.; Wilson, K.; Rogers, S., Jr.; Matthews, J.B.; Millis, J.M.; et al. Review Paper on Penetrating Brain Injury: Ethical Quandaries in the Trauma Bay and Beyond. Ann. Surg. 2023, 277, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Johansson, P.I.; Stensballe, J.; Oliveri, R.; Wade, C.E.; Ostrowski, S.R.; Holcomb, J.B. How I Treat Patients with Massive Hemorrhage. Blood 2014, 124, 3052–3058. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.; Fritz, S.; Hake, D.; Son, M.; Greve, S.; Jbara, M.; Chitta, S.; Fritz, B.; Miller, A.; Bader, M.K.; et al. Targeted Thromboelastographic (Teg) Blood Component and Pharmacologic Hemostatic Therapy in Traumatic and Acquired Coagulopathy. Curr. Drug Targets 2016, 17, 954–970. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.E.; Rickard, A.; Wise, D. Traumatic Cardiac Arrest. J. R. Soc. Med. 2015, 108, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Rubin, M. Should We Offer Blood Transfusions as a Palliative Therapy? Am. J. Bioeth. 2016, 16, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Bhogadi, S.K.; Ditillo, M.; Khurshid, M.H.; Stewart, C.; Hejazi, O.; Spencer, A.L.; Anand, T.; Nelson, A.; Magnotti, L.J.; Joseph, B. Development and Validation of Futility of Resuscitation Measure in Older Adult Trauma Patients. J. Surg. Res. 2024, 301, 591–598. [Google Scholar] [CrossRef] [PubMed]

| Study | Scoring Criteria |
|---|---|
| Suspension of Transfusion and Other Procedures (STOP) [41] | The proposed STOP criteria include any one of the combined clinical and lab markers below, each combination having a 100% PPV and specificity for death:
|
| Trans-Agency Consortium for Trauma-Induced Coagulopathy (TACTIC) TIC Score [136] |
|
| National Blood Transfusion Committee Triage Tool for Massively Transfused Patients (NBTC TTMTP) [7] |
|
| Variable | PPV, % | NPV, % | Sn, % | Sp, % |
|---|---|---|---|---|
| Arrival SBP ≤ 50 and LY30 ≥ 30% | 100 | 78 | 33 | 100 |
| Arrival SBP ≤ 50 and lactate ≥ 15 | 100 | 77 | 31 | 100 |
| Arrival SBP ≤ 70, LY30 ≥ 30%, and lactate ≥ 15 | 100 | 77 | 30 | 100 |
| ROSC and LY30 ≥ 30% | 100 | 78 | 33 | 100 |
| ROSC and lactate ≥ 12 | 100 | 76 | 29 | 100 |
| ROSC and GCS 3 | 100 | 77 | 27 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walsh, M.M.; Fox, M.D.; Moore, E.E.; Johnson, J.L.; Bunch, C.M.; Miller, J.B.; Lopez-Plaza, I.; Brancamp, R.L.; Waxman, D.A.; Thomas, S.G.; et al. Markers of Futile Resuscitation in Traumatic Hemorrhage: A Review of the Evidence and a Proposal for Futility Time-Outs during Massive Transfusion. J. Clin. Med. 2024, 13, 4684. https://doi.org/10.3390/jcm13164684
Walsh MM, Fox MD, Moore EE, Johnson JL, Bunch CM, Miller JB, Lopez-Plaza I, Brancamp RL, Waxman DA, Thomas SG, et al. Markers of Futile Resuscitation in Traumatic Hemorrhage: A Review of the Evidence and a Proposal for Futility Time-Outs during Massive Transfusion. Journal of Clinical Medicine. 2024; 13(16):4684. https://doi.org/10.3390/jcm13164684
Chicago/Turabian StyleWalsh, Mark M., Mark D. Fox, Ernest E. Moore, Jeffrey L. Johnson, Connor M. Bunch, Joseph B. Miller, Ileana Lopez-Plaza, Rachel L. Brancamp, Dan A. Waxman, Scott G. Thomas, and et al. 2024. "Markers of Futile Resuscitation in Traumatic Hemorrhage: A Review of the Evidence and a Proposal for Futility Time-Outs during Massive Transfusion" Journal of Clinical Medicine 13, no. 16: 4684. https://doi.org/10.3390/jcm13164684







