Abstract
Background/Objectives: In patients with varus knee osteoarthritis, compensatory changes occur in the foot and ankle joints to compensate for the varus deformity of the knee. The aim of the study was to investigate the changes in the ankle of patients whose knee alignment was corrected with total knee arthroplasty (TKA) and to explore the clinical implications of these findings. Methods: In this retrospective observational study, we analyzed 204 knees of 179 patients who had regular follow-ups out of 431 patients who underwent TKA for varus knee osteoarthritis between January 2019 and July 2021. Patient demographics, body mass index, follow-up time, and radiographs were studied. The hip–knee–ankle (HKA) angle, joint line convergence angle (JLCA), talar tilt (TT) angle, ground talar dome (GT) angle, ground tibia plafond (GP) angle, and the American Orthopaedic Foot & Ankle Society (AOFAS) score were assessed preoperatively and at the last follow-up. Results: A total of 204 knees of 179 patients with a mean follow-up time of 32.50 ± 6.68 months were evaluated. It was found that the change in the HKA had a positive effect on the AOFAS score and a negative effect on the TT, GT, and GP angles. While the clinical score improved in 82 patients, it worsened in 8 patients. The age difference between the groups whose AOFAS score improved and worsened was statistically significant. Conclusions: The correction of the varus malalignment in the knee was shown to also improve the compensatory valgus in the foot and ankle over the mid-term, with a statistically significant improvement in the patients’ clinical ankle scores.
1. Introduction
Osteoarthritis (OA) is a chronic disease affecting a significant portion of the global population, characterized by the failed repair of joint damage due to stresses from abnormalities in joint or periarticular tissues [1]. Despite cartilage loss being a primary characteristic, OA affects the entire joint, resulting in the progressive degradation of the joint cartilage and the impairment of adjacent structures. Clinical manifestations include pain, stiffness, reduced joint mobility, and audible joint crepitus. In 2020, it was estimated that approximately 595 million people worldwide were afflicted with OA, a number expected to rise due to increasing life expectancy, obesity rates, and joint injuries [2]. This condition severely impacts the quality of life due to chronic pain and reduced mobility, leading to considerable morbidity [3]. Among the joints most affected by osteoarthritis, the knee ranks highest, followed by the hand and hip [4]. The knee, a crucial joint for daily activities, is subjected to substantial loads. As life expectancy increases and obesity rates rise, coupled with a growing number of joint injuries, the prevalence and incidence of knee osteoarthritis are expected to escalate [5,6]. The development and progression of knee OA are influenced by several risk factors, including age, gender, obesity, previous joint injuries, and occupational hazards involving repetitive joint loading [7]. Studies indicate that women are more susceptible to OA than men, and obesity is strongly associated with OA due to the increased mechanical stress on weight-bearing joints [8,9]. Additionally, participation in high-impact sports and activities can predispose individuals to osteoarthritis (OA) through cumulative joint trauma; however, there is no increased risk associated with recreational physical activities (e.g., running, swimming, or cycling) [10,11].
Biomechanical issues are major risk factors for knee osteoarthritis. Malalignment of the lower extremities disturbs knee joint biomechanics, with coronal plane malalignment accelerating the progression of knee OA [12]. Although valgus malalignment can occur, varus malalignment is more commonly associated with knee osteoarthritis [13]. The mechanical axis of the lower extremities extends from the hip to the foot. Advanced varus knee osteoarthritis is a long-term pathological process that alters the alignment of the entire lower extremity and can lead to degenerative changes in the ankle joint [14,15].
Total knee arthroplasty (TKA) is the gold standard treatment for end-stage knee OA globally. While patient satisfaction with TKA is generally high, dissatisfaction rates range from 10% to 25% [16]. Preoperative evaluations for TKA typically focus on knee alignment using plain radiographs, often overlooking adaptive and pathological changes in the hip and ankle joints. Varus or valgus malalignment of the knee can result in ankle malalignment and changes in the tibiotalar tilt angle [17]. Most TKA patients have some degree of flexibility in the ankle and hindfoot, which can result in changes after knee alignment adjustments.
Some studies suggest that varus deformity of the knee is compensated by the valgization of the ankle and subtalar joint [17,18]. However, other studies indicate that the alignment of the foot and ankle is not related to the alignment of the lower extremity [19]. There is a lack of research on the reversal of these changes following varus correction in the knee and their clinical impact on the ankle joint in the midterm. Understanding the changes in the ankle and hindfoot after correcting lower extremity varus deformities with TKA and examining their interrelationships and clinical outcomes is crucial. The aim of this study is to investigate the radiological changes in the coronal plane of the ankle after correcting varus malalignment with TKA and to explore the relationships between these changes and clinical outcomes. The findings are expected to highlight the changes in foot and ankle biomechanics in the treatment of varus knee osteoarthritis, emphasizing the factors that should be considered to achieve better clinical outcomes when planning treatment. Although there are studies in the literature on this subject, the research on mid-term results is limited, and there is still no consensus in this area.
2. Materials and Methods
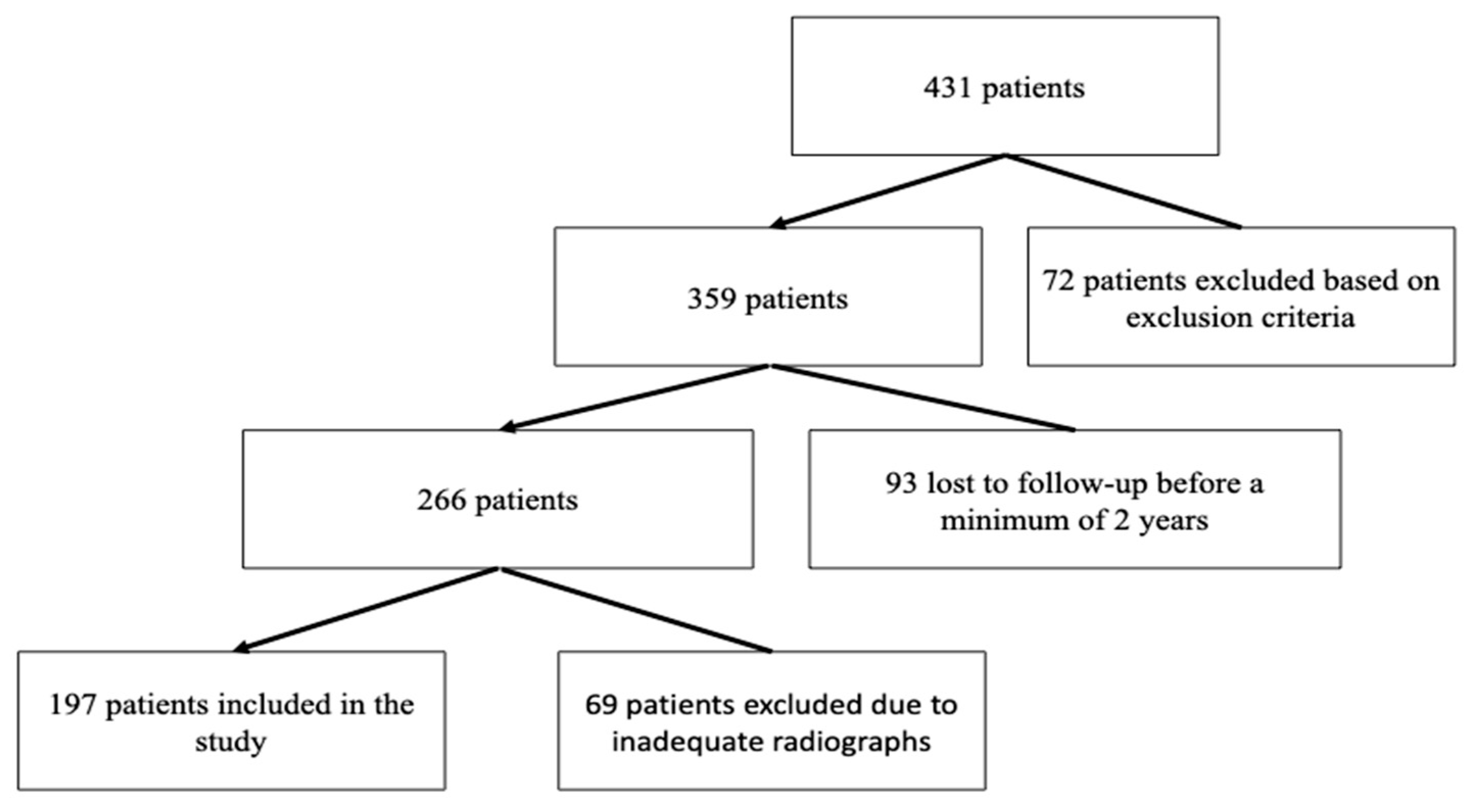
In this retrospective observational study, 204 knees of 179 patients out of 431 patients who underwent TKA for varus knee OA between January 2019 and July 2021 were included (Figure 1). Of the patients, 27 were men, and 152 were women. Of the 179 patients included in the study, 154 patients underwent TKA on one knee, and 25 patients underwent TKA on both knees. All patients underwent surgery using the same surgical technique, and the prosthetic design used for all patients was a posterior-stabilized fixed bearing. Routine preoperative and follow-up full leg standing anteroposterior and lateral knee radiographs were performed for each patient who underwent TKA.
Figure 1.
Flowchart of the patient enrollment process.
Patients were followed from 24 to 48 months, with an average follow-up of 32.50 ± 6.68 months. The study’s patient body mass index (BMI) measurements ranged from 21.8 to 46.1 kg/m2, with an average of 32.24 ± 4.23 kg/m2 (Table 1).

Table 1.
Demographic features.
This study included patients aged 18 and older who were diagnosed with primary varus knee osteoarthritis and underwent primary posterior-stabilized TKA at our clinic between January 2019 and July 2021. The exclusion criteria were as follows: a history of inflammatory disease, secondary osteoarthritis diagnosis of the knee such as septic arthritis and post-traumatic arthritis, any surgical intervention history or requiring additional intervention on the same lower extremity included in the study, insufficient follow-up duration, and low-quality or incomplete preoperative and/or postoperative imaging.
This study was approved by the institutional ethics committee of Bilkent City Hospital (number: E1-22-3026) and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its subsequent amendments.
2.1. Radiological Evaluations
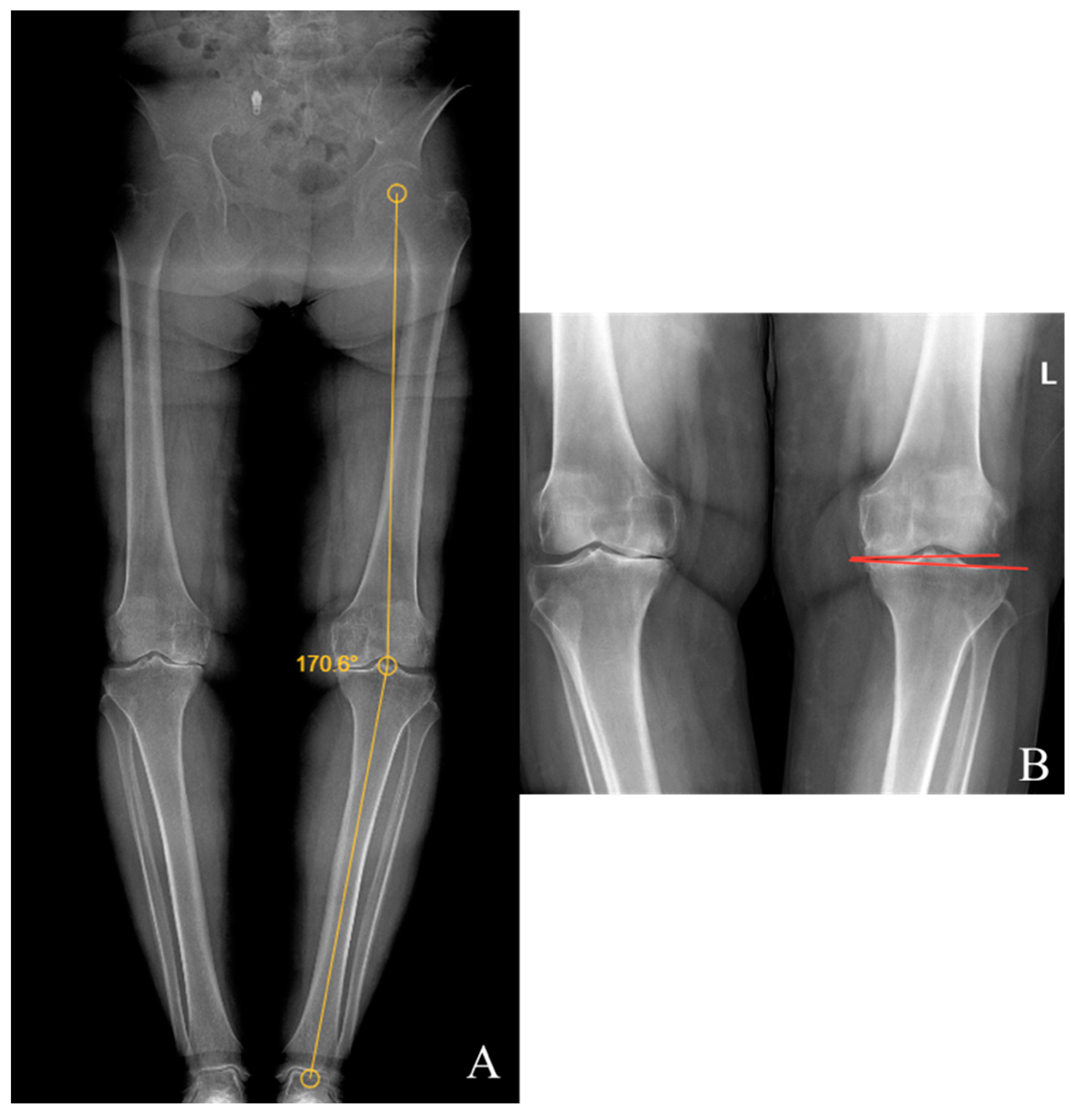
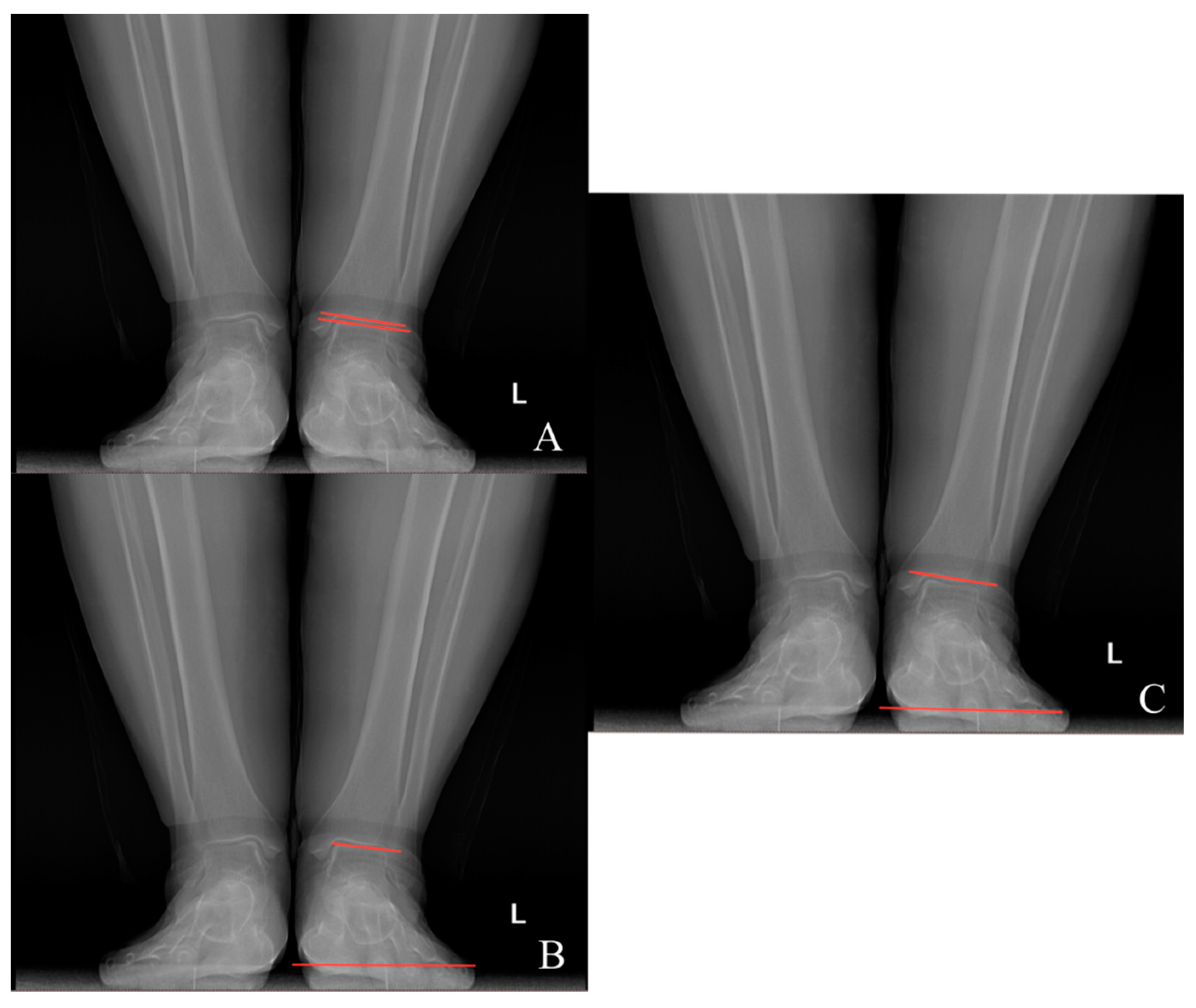
Preoperative and last visit full-leg standing radiographs were evaluated in each patient. Radiological measurements were performed using the picture archiving and communication system software. Two researchers independently measured the selected angles on all radiographs. The study utilized the average of the measured values. The hip–knee–ankle (HKA) angle was defined as the angle between a line drawn from the center of the femoral head to the femoral intercondylar notch and another line from the center of the tibial plateau to the mid-talar dome. The joint line convergence angle (JLCA) was measured as the angle between the femoral and tibial joint lines. The talar tilt (TT) angle was defined as the angle between the subchondral plate of the distal tibial articular surface and the talar dome, with the apex lateral angles positive and the apex medial angles negative. The ground talar dome (GT) angle was between the talar dome and a line parallel to the ground, and the ground plafond (GP) angle was between the subchondral plate of the distal tibial articular surface and a line parallel to the ground, both with apex lateral angles positive and apex medial angles negative.
The HKA, TT, JLCA, GT, and GP angles were measured on the patients’ radiographs (Figure 2 and Figure 3). The preoperative and last visit American Orthopaedic Foot & Ankle Society (AOFAS) scores were evaluated.
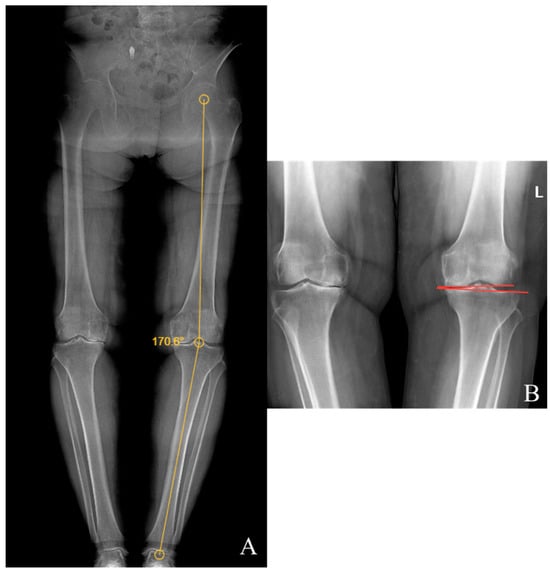
Figure 2.
(A) Hip–knee–ankle angle; (B) knee joint line convergence angle.
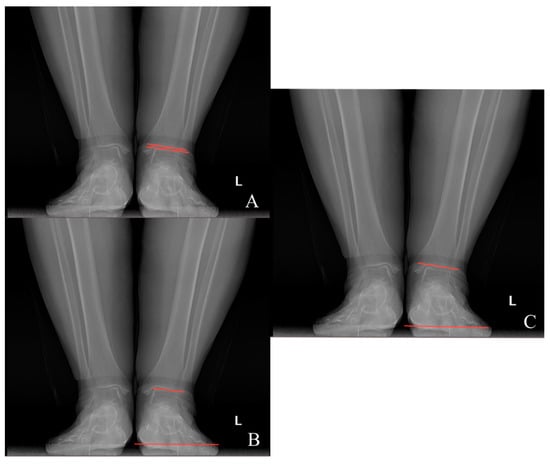
Figure 3.
(A) Talar tilt angle; (B) ground talar dome angle; (C) ground tibia plafond angle.
2.2. Statistical Analysis
The data were evaluated using IBM SPSS Statistics 26 (IBM Corporation, Armonk, NY, USA) at Bilkent City Hospital in February 2023. In the analysis of study data, frequency distribution (number, percentage) is reported for categorical variables, and descriptive statistics (mean, standard deviation) are reported for numerical variables. The independent samples t-test and chi-square test were used to determine whether there was a difference in measurements between groups in terms of improvement/deterioration, the dependent samples t-test to determine whether there was a difference between preoperative and last visit measurements, and Pearson correlation analysis to explore relationships between numerical measurements, revealing correlations between changes in the HKA angle and changes in the TT, GT, and GP angles. In addition, linear regression analysis was performed to determine the effect of changes in the HKA angle on other dependent variables, including the talar tilt (TT), ground talar dome (GT), ground tibia plafond (GP) angles, and AOFAS scores. p ≤ 0.05 was considered significant.
3. Results
Of the patients, 27 (15.1%) were male, and 152 (84.9%) were female. Of 179 patients, the right knee was operated in 70 (39.1%), the left knee in 84 (46.9%), and both knees in 25 (14%). The age of the patients was 65.57 ± 6.99 (47–83). The study’s patient body mass index (BMI) measurements ranged from 21.8 to 46.1 kg/m2, with an average of 32.24 ± 4.23 kg/m2 (Table 1).
Statistically significant differences were observed between the preoperative and last visit hip–knee–ankle angle (HKA), talar tilt angle (TT), knee joint line convergence angle (JLCA), ground talar dome angle (GT), ground tibia plafond angle (GP), and American Orthopaedic Foot & Ankle Society (AOFAS) score (Table 2, p < 0.05).

Table 2.
Differences between preoperative and last visit measurements.
We observed a statistically significant positive correlation between the increase in the HKA angle and the change in the TT, GT, and GP angles and a negative correlation with the AOFAS score. (p ≤ 0.05). The results also demonstrated a statistically significant negative correlation between the AOFAS score and the TT, GT, and GP measurements (Table 3, p ≤ 0.05).

Table 3.
Relationship between measurements.
Changes in the HKA angle showed a statistically significant effect on the TT, GT, and GP angle changes and the AOFAS score change (p < 0.05). Accordingly, a 1 unit decrease in the HKA angle displayed a 0.052 unit decrease in the TT angle, a 0.420 unit decrease in the GT angle, a 0.483 unit decrease in the GP angle, and a 0.750 unit increase in the AOFAS score (Table 4).

Table 4.
Effects of HKA changes on measurements.
While we did not observe a statistically significant difference between the AOFAS score improvement/deterioration groups in terms of gender and BMI (p > 0.05), our data showed a statistically significant difference in terms of age (p < 0.05). Accordingly, the age of patients whose AOFAS score worsened was higher than that of patients whose AOFAS score improved (Table 5).

Table 5.
AOFAS score improvement/deterioration groups’ demographic differences.
Our results also showed no statistically significant difference between the AOFAS score improvement/deterioration groups in terms of the preoperative GT and GP measurements (p > 0.05), but a statistically significant difference in terms of HKA and TT measurements (p < 0.05) was observed. Accordingly, the mean preoperative TT was found to be negative in patients whose AOFAS score deteriorated (Table 6).

Table 6.
Preoperative measurements of AOFAS Score improvement/deterioration groups.
While we did not observe statistically significant differences between the last visit AOFAS score improvement/deterioration groups in terms of the GT angle change (p > 0.05), our data displayed a statistically significant difference in terms of the TT and GP angle change (p < 0.05). Accordingly, the change in the TT and GP angle is higher in those who improve than in those who worsen (Table 7).

Table 7.
Change in measurements between the last visit AOFAS score improvement/deterioration groups.
4. Discussion
Our study provides valuable insight into the mid-term clinical and radiological changes in the ankle after TKA for varus knee OA. Correcting the varus deformities of the knee with TKA also addresses the compensatory ankle valgus. Our results demonstrate a significant correlation between the knee and ankle alignment, highlighting the interrelation of the lower extremity biomechanics.
Several studies have suggested that a varus malalignment of the knee is also associated with a compensatory valgus in the ankle. However, there is no consensus or sufficient research to determine whether correcting the knee’s varus deformity reverses this compensatory valgus in the ankle [17,18,20,21]. Norton et al. demonstrated an association between varus knee deformity and foot/ankle valgus and between valgus knee deformity and foot/ankle varus [22]. Similarly, Gao et al. showed that ankle alignment is associated with knee alignment both before and after surgery and that pre-operative malalignments in both the knee and ankle can be corrected simultaneously following TKA [20]. However, Chandler et al. found no correlation between preoperative lower extremity alignment and ankle alignment [19]. In our study, a significant relationship between varus knee osteoarthritis and ankle valgus alignment was demonstrated.
Many studies in the literature have reported an increase in AOFAS scores following a decrease in the HKA angle after TKA. Lee et al. observed a decrease in the GT, GP, and TT angles after TKA in patients with varus knee OA over a three-year follow-up period [23]. Palanisami et al. reported preoperative and final HKA angles of 18 ± 6.3 and 1.2 ± 1.9 degrees varus, respectively, with AOFAS scores improving from 59.2 ± 9.5 and 88.7 ± 5.9 [24]. Diao et al. found preoperative HKA angles of 9.15 ± 5.54 varus and final HKA angles 2.37 ± 3.05 varus, with AOFAS scores increasing from 76.50 ± 10.89 to 90.40 ± 6.05 [25]. However, the majority of studies in the literature have short-term follow-ups. The results of our study demonstrated that correcting knee varus led to an increase in the AOFAS scores at the mid-term follow-up. Furthermore, the correction of knee varus deformity also corrects compensatory valgus deformity in the ankle, resulting in both radiological and clinical improvements.
In the study by Lee et al., medial talar tilt was present in 39 of 128 patients, 18 of whom had ankle osteoarthritis [23]. However, the clinical scores of the patients were not available in this study. Wu et al. found no significant difference in the TT angle in relation to foot and ankle pain [26]. In our study, five out of eight patients with worsening AOFAS scores had medial talar tilt. In addition, a negative talar tilt angle was identified as a risk factor for worsening clinical scores (p = 0.007).
Wu et al. found no significant age difference but identified female gender and high BMI as risk factors for postoperative foot and ankle pain in TKA patients with varus knee OA [26]. In another study, Kim et al. observed that ankle pain after TKA was associated with residual varus deformity of the knee [27]. However, in our study, this association was not observed in patients with residual varus deformity of the knee. Our study found that older patients showed less improvement in clinical scores, which aligns with Diao et al.’s findings that compensatory mechanisms diminish with age. This suggests that age may be a limiting factor in the extent of improvement in ankle alignment and function after TKA [25]. This may explain why the older patients in our study showed less change in GP and TT angles and had worsened AOFAS scores.
There are studies in the literature showing changes in knee alignment and knee pain complaints after hip arthroplasty [28,29,30,31]. This demonstrates that all lower extremity alignments are interrelated. Kobayashi et al. suggest, that in patients presenting with knee and hip pain, addressing the hip first may result in a reduction in knee pain [31]. Similarly, our study shows that in patients with varus knee OA and ankle pain, the knee OA should be addressed first. However, in patients with negative talar tilt and those of advanced age, it is possible that the desired level of improvement may not be achieved or that the patient’s complaints may increase.
The main limitation of our study is the lack of a control group. Other limitations include the retrospective nature of the study, the unequal gender distribution, the narrow focus on coronal alignment, and the exclusive focus on varus deformity. The strengths of the study include the large patient cohort, long follow-up, and comprehensive clinical score evaluation. A consensus and sufficient studies on this topic are still lacking in the literature. It is therefore recommended that further research should prospectively include a larger patient population and a control group in order to provide more conclusive evidence.
5. Conclusions
The changes in the ankle after total knee arthroplasty in varus knee osteoarthritis have not been adequately clarified in the literature. In our study, the correction of the varus malalignment in the knee was shown to also improve the compensatory valgus in the foot and ankle over the mid-term, with a statistically significant improvement in patients’ clinical scores. The improvement in clinical scores in most patients after TKA in varus knee OA indicates that intervention for compensatory valgus is not necessary, and patients’ ankle pain may subside with the treatment of the varus knee OA.
While BMI and gender were not identified as risk factors for clinical score worsening in our study, age and a negative TT angle were found to be significant risk factors. However, the reasons for the deterioration in the clinical scores in some patients should be clearly identified, and appropriate plans should be made accordingly. The results we found need to be supported by prospective randomized controlled trials.
Author Contributions
Conceptualization, A.S.N. and M.D.; Formal analysis, A.S.N. and İ.D.; Methodology, A.N, J.M.-A., M.A. and M.D.; Data curation, A.S.N.; Validation, İ.D., J.M.-A., M.A. and M.D.; Writing—original draft preparation, A.S.N.; Writing—review and editing, M.D., J.M.-A. and M.A.; Supervision, M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Bilkent City Hospital (E1-22-3026; 16 November 2022).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
Joaquín Moya-Angeler is a guest Editor of the Special Issue of the Journal of Clinical Medicine. The rest of the authors declare that they have no conflicts of interest.
References
- Sharma, L. Osteoarthritis of the Knee. N. Engl. J. Med. 2021, 384, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, J.D.; Culbreth, G.T.; Haile, L.M.; Rafferty, Q.; Lo, J.; Fukutaki, K.G.; Cruz, J.A.; Smith, A.E.; Vollset, S.E.; Brooks, P.M.; et al. Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: A systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023, 5, e508–e522. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Bierma-Zeinstra, S. Osteoarthritis. Lancet 2019, 393, 1745–1759. (In English) [Google Scholar] [CrossRef] [PubMed]
- Prieto-Alhambra, D.; Judge, A.; Javaid, M.K.; Cooper, C.; Diez-Perez, A.; Arden, N.K. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: Influences of age, gender and osteoarthritis affecting other joints. Ann. Rheum. Dis. 2014, 73, 1659–1664. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; King, L.K. The Burden of Osteoarthritis in Older Adults. Clin. Geriatr. Med. 2022, 38, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Kean, W.F. Obesity and knee osteoarthritis. Inflammopharmacology 2012, 20, 53–58. (In English) [Google Scholar] [CrossRef] [PubMed]
- Hulshof, C.T.; Pega, F.; Neupane, S.; Colosio, C.; Daams, J.G.; Kc, P.; Kuijer, P.P.; Mandic-Rajcevic, S.; Masci, F.; van der Molen, H.F.; et al. The effect of occupational exposure to ergonomic risk factors on osteoarthritis of hip or knee and selected other musculoskeletal diseases: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2021, 150, 106349. (In English) [Google Scholar] [CrossRef] [PubMed]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568–578. (In English) [Google Scholar] [CrossRef]
- Silverwood, V.; Blagojevic-Bucknall, M.; Jinks, C.; Jordan, J.L.; Protheroe, J.; Jordan, K.P. Current evidence on risk factors for knee os-teoarthritis in older adults: A systematic review and meta-analysis. Osteoarthr. Cartil. 2015, 23, 507–515. [Google Scholar] [CrossRef]
- Lopes, D.G.; Costa, D.; Cruz, E.B.; Mendonça, N.; Henriques, A.R.; Branco, J.; Canhão, H.; Rodrigues, A.M. Association of physical activity with physical function and quality of life in people with hip and knee osteoarthritis: Longitudinal analysis of a population-based cohort. Arthritis Res. Ther. 2023, 25, 14. (In English) [Google Scholar] [CrossRef]
- Timmins, K.A.; Leech, R.D.; Batt, M.E.; Edwards, K.L. Running and Knee Osteoarthritis: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2017, 45, 1447–1457. (In English) [Google Scholar] [CrossRef] [PubMed]
- Goto, N.; Okazaki, K.; Akiyama, T.; Akasaki, Y.; Mizu-Uchi, H.; Hamai, S.; Nakamura, S.; Nakashima, Y. Alignment factors affecting the medial meniscus extrusion increases the risk of osteoarthritis development. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2617–2623. (In English) [Google Scholar] [CrossRef] [PubMed]
- Dell’Isola, A.; Allan, R.; Smith, S.L.; Marreiros, S.S.; Steultjens, M. Identification of clinical phenotypes in knee osteoarthritis: A systematic review of the literature. BMC Musculoskelet Disord. 2016, 17, 425. (In English) [Google Scholar] [CrossRef]
- Saxby, D.J.; Lloyd, D.G. Osteoarthritis year in review 2016: Mechanics. Osteoarthr. Cartil. 2017, 25, 190–198. (In English) [Google Scholar] [CrossRef]
- Sharma, L.; Song, J.; Felson, D.T.; Cahue, S.; Shamiyeh, E.; Dunlop, D.D. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 2001, 286, 188–195. (In English) [Google Scholar] [CrossRef]
- Bierke, S.; Häner, M.; Karpinski, K.; Hees, T.; Petersen, W. Midterm Effect of Mental Factors on Pain, Function, and Patient Satisfaction 5 Years After Uncomplicated Total Knee Arthroplasty. J. Arthroplast. 2020, 35, 105–111. (In English) [Google Scholar] [CrossRef] [PubMed]
- Shichman, I.; Ben-Ari, E.; Sissman, E.; Oakley, C.; Schwarzkopf, R. Effect of Total Knee Arthroplasty on Coronal Alignment of the Ankle Joint. J. Arthroplast. 2022, 37, 869–873. (In English) [Google Scholar] [CrossRef]
- Jeong, B.; Kim, T.Y.; Baek, J.H.; Jung, H.; Song, S.H. Following the correction of varus deformity of the knee through total knee arthroplasty, significant compensatory changes occur not only at the ankle and subtalar joint, but also at the foot. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3230–3237. (In English) [Google Scholar] [CrossRef] [PubMed]
- Chandler, J.T.; Moskal, J.T. Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: A prospective analysis. J Arthroplast. 2004, 19, 211–216. (In English) [Google Scholar] [CrossRef]
- Gao, F.; Ma, J.; Sun, W.; Guo, W.; Li, Z.; Wang, W. Radiographic assessment of knee–ankle alignment after total knee arthroplasty for varus and valgus knee osteoarthritis. Knee 2017, 24, 107–115. (In English) [Google Scholar] [CrossRef]
- Xie, K.; Han, X.; Jiang, X.; Ai, S.; Dai, K.; Yu, Z.; Wu, H.; Qu, X.; Yan, M. The effect of varus knee deformities on the ankle alignment in patients with knee osteoarthritis. J. Orthop. Surg. Res. 2019, 14, 134. (In English) [Google Scholar] [CrossRef]
- Norton, A.A.; Callaghan, J.J.; Amendola, A.; Phisitkul, P.; Wongsak, S.; Liu, S.S.; Fruehling-Wall, C. Correlation of knee and hindfoot deformities in advanced knee OA: Compensatory hindfoot alignment and where it occurs. Clin. Orthop. Relat. Res. 2015, 473, 166–174. (In English) [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; O Jeong, B. Radiologic Changes of Ankle Joint after Total Knee Arthroplasty. Foot Ankle Int. 2012, 33, 1087–1092. (In English) [Google Scholar] [CrossRef] [PubMed]
- Palanisami, D.R.; Rajasekaran, R.B.; Reddy, P.K.; Natesan, R.; Sethuraman, A.; Rajasekaran, S. Foot loading pattern and hind foot alignment are corrected in varus knees following total knee arthroplasty: A pedobarographic analysis. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 1861–1867. (In English) [Google Scholar] [CrossRef]
- Diao, N.; Yu, F.; Yang, B.; Ma, L.; Yin, H.; Guo, A. Association between changes in hip-knee-ankle angle and hindfoot alignment after total knee arthroplasty for varus knee osteoarthritis. BMC Musculoskelet. Disord. 2021, 22, 610. (In English) [Google Scholar] [CrossRef] [PubMed]
- Wu, L.-J.; Jiang, S.-G.; Cui, L.-K.; Zhang, Q.; Zhang, L.; Kang, K.; Bai, Y.-M.; Gao, S.-J. A Retrospective Study of the Risk Factors for Postoperative Foot or Ankle Pain in 90 Patients with Varus Osteoarthritis of the Knee who Underwent Total Knee Arthroplasty. Med. Sci. Monit. 2021, 27, e932796. (In English) [Google Scholar] [CrossRef]
- Kim, C.-W.; Gwak, H.-C.; Kim, J.-H.; Lee, C.-R.; Kim, J.-G.; Oh, M.; Park, J.-H. Radiologic Factors Affecting Ankle Pain before and after Total Knee Arthroplasty for the Varus Osteoarthritic Knee. J. Foot Ankle Surg. 2018, 57, 865–869. [Google Scholar] [CrossRef]
- Choi, Y.S.; Park, J.-W.; Kim, T.W.; Kang, K.S.; Lee, Y.-K.; Koo, K.-H.; Chang, C.B. Effect of Total Hip Arthroplasty on Ipsilateral Lower Limb Alignment and Knee Joint Space Width: Minimum 5-Year Follow-up. J. Korean Med. Sci. 2023, 38, e148. [Google Scholar] [CrossRef]
- Thöne, P.; Gruber, M.S.; Kindermann, H.; Gussner, W.; Sadoghi, P.; Ortmaier, R. Stem Design in Total Hip Arthroplasty Influences Ipsilateral Knee Valgus: A Retrospective Comparative Analysis of 2953 Cases. J. Clin. Med. 2023, 12, 6662. [Google Scholar] [CrossRef]
- van Drongelen, S.; Fey, B.; Stief, F.; Meurer, A. Influence of implantation of a total hip endoprosthesis on the ipsilateral leg alignment: The effect of sex and dysplasia of the hip. Arch. Orthop. Trauma Surg. 2023, 143, 3541–3549. [Google Scholar] [CrossRef]
- Kobayashi, D.; Choe, H.; Kobayashi, N.; Watanabe, S.; Inaba, Y. Effects of changes in whole-body alignment on ipsilateral knee pain after total hip arthroplasty. J. Orthop. Sci. 2023, 28, 398–402. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).