A Comparison of the Effectiveness of the Serratus Anterior Plane Block and Erector Spinae Plane Block to that of the Paravertebral Block in the Surgical Treatment of Breast Cancer—A Randomized, Prospective, Single-Blinded Study
Abstract
1. Introduction
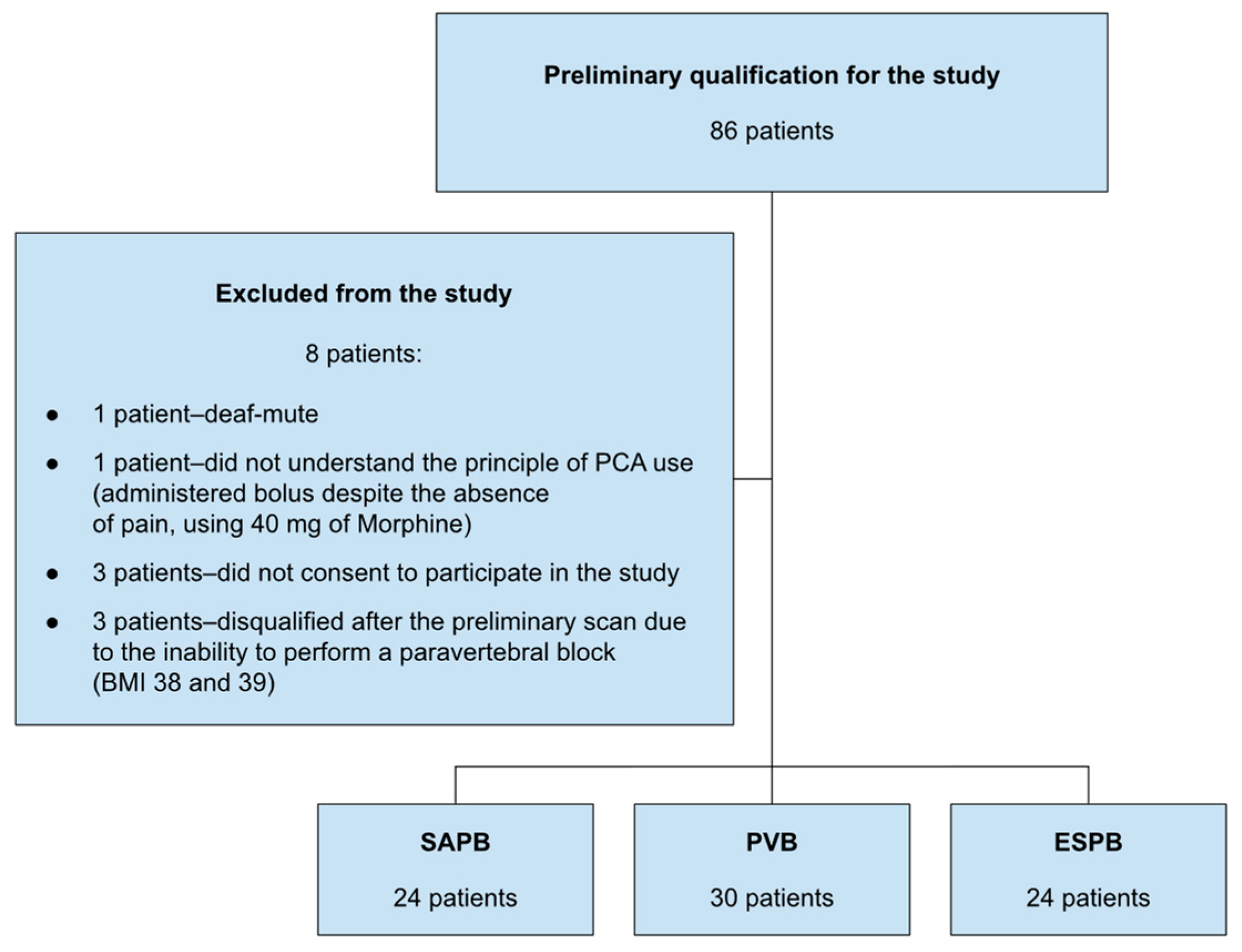
2. Materials and Methods
- To assess the impact of SAPB, ESPB, and PVBs on fentanyl consumption during surgery.
- To assess the impact of SAPB, ESPB, and PVBs on the amount of morphine administered to patients postoperatively.
- To assess the impact of SAPB, ESPB, and PVBs on pain intensity during coughing and at rest on the first day post-surgery six times daily from the first hour post-operation until the end of the second postoperative day.
- To evaluate the safety of the paravertebral block and the applied fascial blocks SAPB and ESPB.
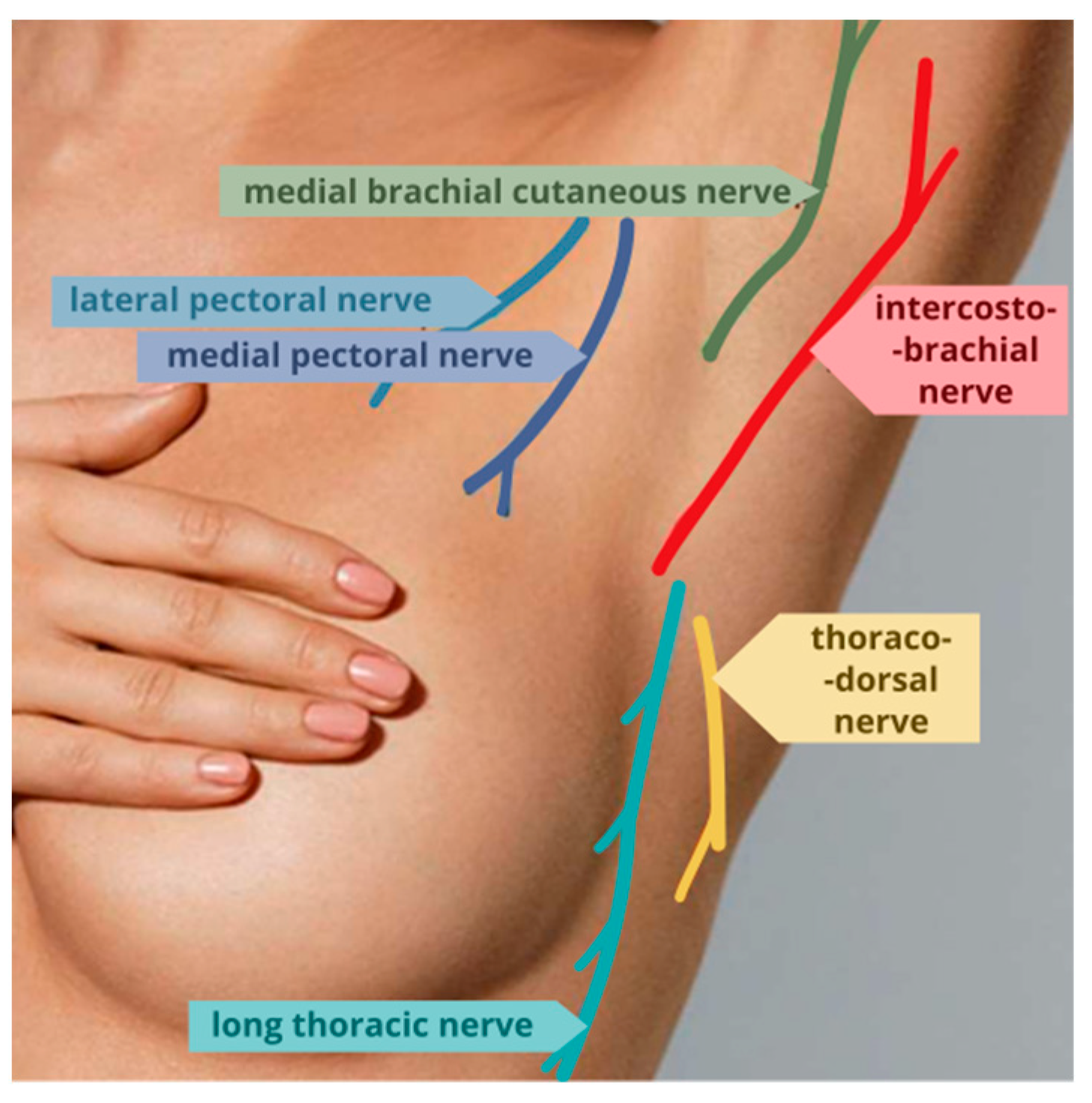
2.1. Serratus Anterior Plane Block (SAPB)
2.2. Paravertebral Block (PVB)
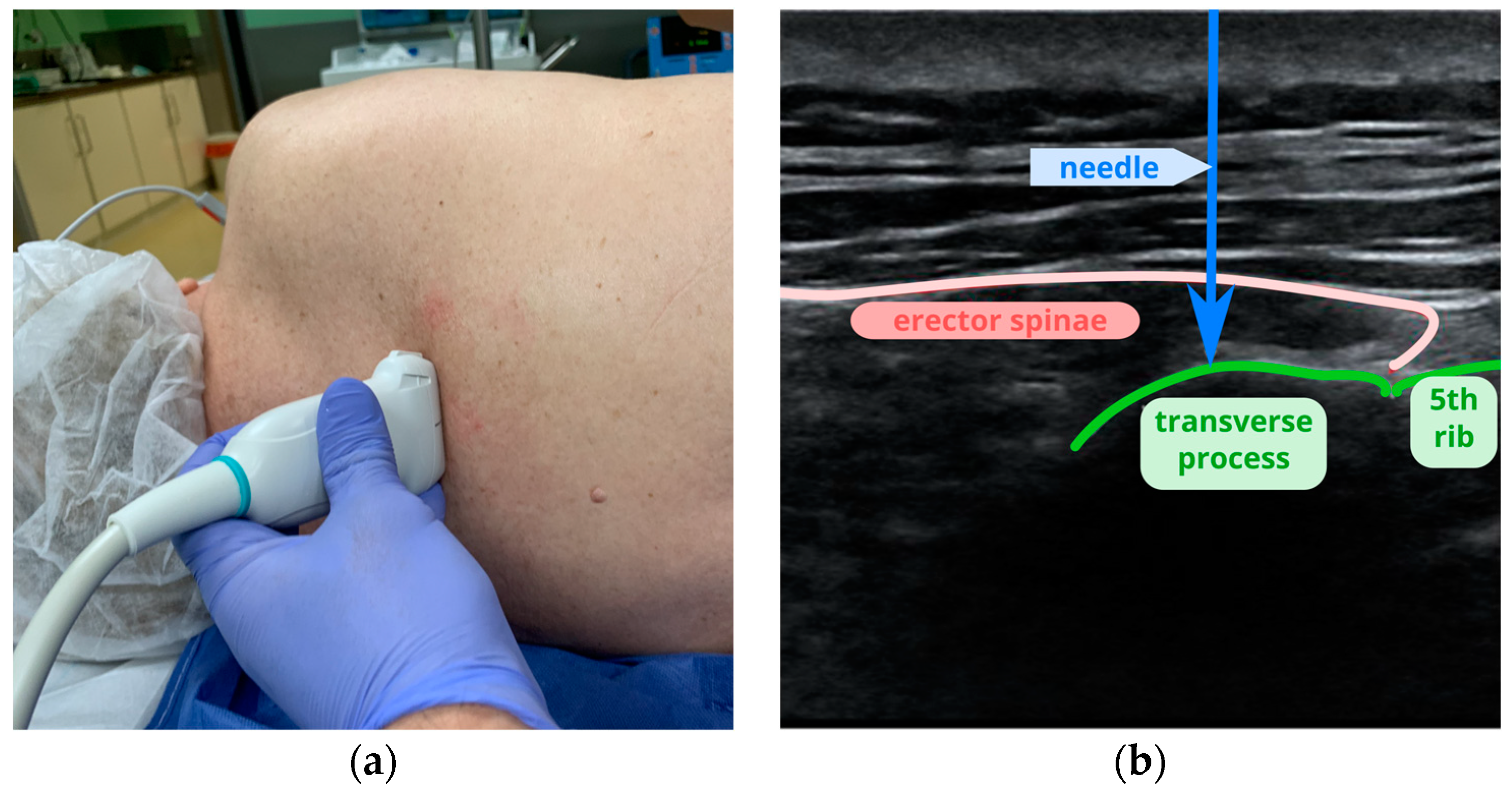
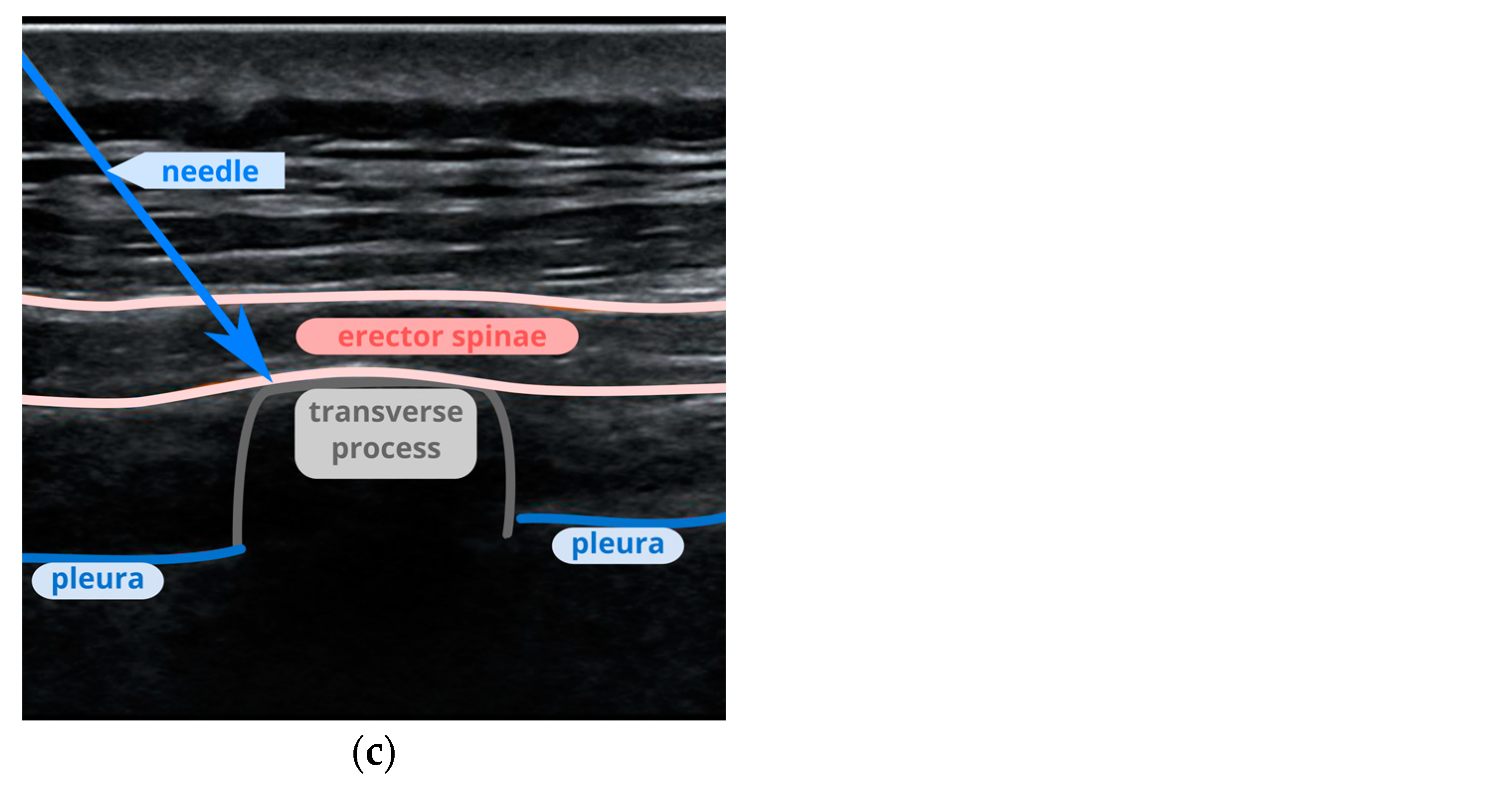
2.3. Erector Spinae Plane Block (ESPB)
2.4. Perioperative Management
2.5. Postoperative Pain Intensity Measurement
2.6. Complication Evaluation
2.7. Statistical Analysis
2.8. Sample Size and Power of the Study
3. Results
3.1. Intraoperative Fentanyl Consumption and Postoperative Morphine Consumption
3.2. Pain Intensity at Rest
3.3. Pain Intensity during Coughing
4. Discussion
4.1. Intraoperative Analgesia
4.2. SAPB vs. PVB in Postoperative Analgesia
4.3. ESPB vs. PVB in Postoperative Analgesia
4.4. ESPB vs. SAPB in Postoperative Analgesia
4.5. Limitations
5. Conclusions
- Both the serratus anterior plane block and the erector spinae plane block were as effective as the paravertebral block in achieving intraoperative analgesia.
- The serratus anterior plane block was equally as effective as the paravertebral block in achieving postoperative analgesia.
- The erector spinae plane block was significantly less effective in achieving postoperative analgesia than both the paravertebral block and serratus anterior plane block.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Didkowska, J.; Barańska, K.; Miklewska, M.J.; Wojciechowska, U. Cancer incidence and mortality in Poland in 2023. Nowotw. J. Oncol. 2024, 74, 75–93. [Google Scholar] [CrossRef]
- Calapai, M.; Esposito, E.; Puzzo, L.; Vecchio, D.A.; Blandino, R.; Bova, G.; Quattrone, D.; Mannucci, C.; Ammendolia, I.; Mondello, C.; et al. Post-Mastectomy Pain: An updated overview on risk factors, predictors, and markers. Life 2021, 11, 1026. [Google Scholar] [CrossRef] [PubMed]
- Rao, F.; Wang, Z.; Chen, X.; Liu, L.; Qian, B.; Guo, Y. Ultrasound-guided thoracic paravertebral block enhances the quality of recovery after modified radical mastectomy: A randomized controlled trial. J. Pain. Res. 2021, 14, 2563–2570. [Google Scholar] [CrossRef] [PubMed]
- Niesen, A.D.; Jacob, A.K.; Law, L.A.; Sviggum, H.P.; Johnson, R.L. Complication rate of ultrasound-guided paravertebral block for breast surgery. Reg. Anesth. Pain. Med. 2020, 10, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Schnabel, A.; Reichl, S.U.; Kranke, P.; Pogatzki-Zahn, E.M.; Zahn, P.K. Efficacy and safety of paravertebral blocks in breast surgery: A meta-analysis of randomized controlled trials. Br. J. Anaesth. 2010, 6, 842–852. [Google Scholar] [CrossRef] [PubMed]
- Blanco, R. The ‘pecs block’: A novel technique for providing analgesia after breast surgery. Anaesthesia 2011, 9, 847–848. [Google Scholar] [CrossRef] [PubMed]
- Blanco, R.; Fajardo, M.; Parras Maldonado, T. Ultrasound description of Pecs II (modified Pecs I): A novel approach to breast surgery. Rev. Esp. Anestesiol. Reanim. 2012, 9, 470–475. [Google Scholar] [CrossRef]
- Blanco, R.; Parras, T.; McDonnell, J.G.; Prats-Galino, A. Serratus plane block: A novel ultrasound-guided thoracic wall nerve block. Anaesthesia 2013, 11, 1107–1113. [Google Scholar] [CrossRef]
- Singh, S.; Chowdhary, N.K. Erector spinae plane block an effective block for post-operative analgesia in modified radical mastectomy. Indian. J. Anaesth. 2018, 2, 148–150. [Google Scholar] [CrossRef]
- Gabriel, R.A.; Swisher, M.W.; Sztain, J.F.; Curran, B.P.; Said, E.T.; Abramson, W.B.; Khatibi, B.; Alexander, B.S.; Finneran, J.J.; Wallace, A.M.; et al. Serratus anterior plane versus paravertebral nerve blocks for postoperative analgesia after non-mastectomy breast surgery: A randomized controlled non-inferiority trial. Reg. Anesth. Pain. Med. 2021, 9, 773–778. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.; Srikanth, K.; Girdhar, K.K.; Chan, V. Analgesic efficacy of ultrasound-guided paravertebral block versus serratus plane block for modified radical mastectomy: A randomised, controlled trial. Indian. J. Anaesth. 2017, 5, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.T.; Langridge, X.T.; Cheng, G.S.; McBroom, M.M.; Minhajuddin, A.; Machi, A.T. Superficial vs. deep serratus anterior plane block for analgesia in patients undergoing mastectomy: A randomized prospective trial. J. Clin. Anesth. 2021, 75, 110470. [Google Scholar] [CrossRef]
- Tan, K.W.; Sayed Masri, S.N.N.; Musthafa, Q.A.; Mohd Azidin, A.; Nik Mohamed Kamil, A.; Izaham, A.; Md Nor, N. Analgesic efficacy of the superficial versus deep serratus plane blocks for mastectomy with axillary clearance: A randomized controlled trial. Medicine 2022, 35, e30515. [Google Scholar] [CrossRef]
- Abdallah, F.W.; Cil, T.; MacLean, D.; Madjdpour, C.; Escallon, J.; Semple, J.; Brull, R. Too deep or not too deep?: A propensity-matched comparison of the analgesic effects of a superficial versus deep serratus fascial plane block for ambulatory breast cancer surgery. Reg. Anesth. Pain. Med. 2018, 5, 480–487. [Google Scholar] [CrossRef]
- Aoyama, Y.; Sakura, S.; Tsuchiya, R.; Wittayapairoj, A.; Saito, Y. Erector spinae plane block and paravertebral block for breast surgery: A retrospective propensity-matched noninferiority. Trial. J. Pain. Res. 2020, 13, 2367–2376. [Google Scholar] [CrossRef]
- Jayakrishnan, S.; Dua, A.; Kumar, A. Comparison of fascial plane blocks (ESPB vs. TPVB) for pain relief following modified radical mastectomy. J. Anaesthesiol. Clin. Pharmacol. 2023. [Google Scholar] [CrossRef]
- Elsabeeny, W.Y.; Shehab, N.N.; Wadod, M.A.; Elkady, M.A. Perioperative analgesic modalities for breast cancer surgeries: A prospective randomized controlled trial. J. Pain. Res. 2020, 13, 2885–2894. [Google Scholar] [CrossRef]
- Cowie, B.; McGlade, D.; Ivanusic, J.; Barrington, M.J. Ultrasound-guided thoracic paravertebral blockade: A cadaveric study. Anesth. Analg. 2010, 6, 1735–1739. [Google Scholar] [CrossRef] [PubMed]
- Mekhaeil, M.F.W.; Abdelkader, S.F.; Marof, H.M.; Yousef, A.A.E. Prospective study: The analgesic efficacy of ultrasound-guided erector spinae plane block versus serratus plane block in patients undergoing modified radical mastectomy. J. Adv. Med. Med. Res. 2021, 33, 9–18. [Google Scholar] [CrossRef]
- Ahuja, D.; Kumar, V.; Gupta, N.; Bharati, S.J.; Garg, R.; Mishra, S.; Khan, M.A.; Bhatnagar, S. Comparison of the efficacy of ultrasound-guided serratus anterior plane block versus erector spinae plane block for postoperative analgesia after modified radical mastectomy: A randomised controlled trial. Turk. J. Anaesthesiol. Reanim. 2022, 6, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Swisher, M.W.; Wallace, A.M.; Sztain, J.F.; Said, E.T.; Khatibi, B.; Abanobi, M.; Finneran Iv, J.J.; Gabriel, R.A.; Abramson, W.; Blair, S.L.; et al. Erector spinae plane versus paravertebral nerve blocks for postoperative analgesia after breast surgery: A randomized clinical trial. Reg. Anesth. Pain. Med. 2020, 4, 260–266. [Google Scholar] [CrossRef] [PubMed]


| SAPB (n = 24) | PVB (n = 30) | ESPB (n = 24) | Total (n = 78) | p-Value | |
|---|---|---|---|---|---|
| Procedure | 0.8031 1 | ||||
| Mastectomy + SNLD | 4 (16.7%) | 5 (17.9%) | 3 (12.5%) | 12 (15.8%) | |
| BCT + SNLD | 16 (66.7%) | 16 (57.1%) | 15 (62.5%) | 47 (61.8%) | |
| Madens’ mastectomy | 2 (8.3%) | 4 (14.3%) | 4 (16.7%) | 10 (13.2%) | |
| Quadrantectomy + SNLD | 0 (0.0%) | 1 (3.6%) | 0 (0.0%) | 1 (1.3%) | |
| Tumorectomy | 2 (8.3%) | 0 (0.0%) | 1 (4.2%) | 3 (3.9%) | |
| Quadrantectomy | 0 (0.0%) | 1 (3.6%) | 0 (0.0%) | 1 (1.3%) | |
| BCT | 0 (0.0%) | 1 (3.6%) | 1 (4.2%) | 2 (2.6%) |
| SAPB (n = 24) | PVB (n = 30) | ESPB (n = 24) | Total (n = 78) | p-Value | |
|---|---|---|---|---|---|
| Fentanyl (mg) | 0.4246 1 | ||||
| Mean (SD) | 0.12 (0.04) | 0.12 (0.05) | 0.11 (0.03) | 0.12 (0.04) | |
| Range | 0.10–0.20 | 0.10–0.30 | 0.10–0.20 | 0.10–0.30 | |
| Median | 0.10 | 0.10 | 0.10 | 0.10 | |
| 95% CI | [0.10;0.14] | [0.10;0.14] | [0.10;0.12] | [0.11;0.13] | |
| Morphine (mg) | 0.0004 1 | ||||
| Mean (SD) | 5.4 (3.7) | 4.4 (2.1) | 9.4 (5.5) | 6.3 (4.4) | a 0.0074 2 |
| Range | 1.0–15.0 | 1.0–18.0 | 3.0–23.0 | 1.0–23.0 | b 0.0005 2 |
| Median | 4.0 | 4.0 | 8.0 | 5.0 | |
| 95% CI | [3.8;6.9] | [3.6;5.2] | [7.1;11.7] | [5.3;7.3] |
| SAPB (n = 24) | PVB (n = 30) | ESPB (n = 24) | Total (n = 78) | p-Value | |
|---|---|---|---|---|---|
| 1 h after the procedure | n = 20 | n = 28 | n = 23 | n = 71 | 0.8651 1 |
| mean (SD) | 4.1 (1.8) | 4.0 (1.7) | 3.9 (1.6) | 4.0 (1.6) | |
| median (range) | 4.0 (2.0–9.0) | 4.0 (1.0–7.0) | 3.0 (2.0–8.0) | 4.0 (1.0–9.0) | |
| 95%CI | [3.3;4.9] | [3.3;4.7] | [3.2;4.6] | [3.6;4.4] | |
| 4:00 PM | n = 24 | n = 27 | n = 24 | n = 75 | 0.0017 1 |
| mean (SD) | 2.6 (0.8) | 2.6 (0.9) | 3.6 (1.2) | 2.9 (1.1) | a 0.0129 2 |
| median (range) | 2.0 (2.0–5.0) | 2.0 (1.0–5.0) | 4.0 (1.0–5.0) | 3.0 (1.0–5.0) | b 0.0071 2 |
| 95%CI | [2.3;3.0] | [2.2;2.9] | [3.1;4.1] | [2.7;3.2] | |
| 8:00 PM | n = 24 | n = 27 | n = 24 | n = 75 | 0.0017 1 |
| mean (SD) | 2.6 (0.8) | 2.6 (0.9) | 3.6 (1.2) | 2.9 (1.1) | a 0.0129 2 |
| median (range) | 2.0 (2.0–5.0) | 2.0 (1.0–5.0) | 4.0 (1.0–5.0) | 3.0 (1.0–5.0) | b 0.0071 2 |
| 95%CI | [2.3;3.0] | [2.2;2.9] | [3.1;4.1] | [2.7;3.2] | |
| 12:00 AM | n = 2 | n = 7 | n = 6 | n = 15 | -- |
| mean (SD) | 2.5 (0.7) | 2.4 (0.5) | 2.8 (1.2) | 2.6 (0.8) | |
| median (range) | 2.5 (2.0–3.0) | 2.0 (2.0–3.0) | 2.5 (2.0–5.0) | 2.0 (2.0–5.0) | |
| 95%CI | [-3.9;8.9] | [1.9;2.9] | [1.6;4.1] | [2.1;3.1] | |
| 4:00 AM | n = 0 | n = 1 | n = 1 | n = 2 | -- |
| mean (SD) | 2.0 (0.0) | 1.0 (0.0) | 1.5 (0.7) | ||
| median (range) | 2.0 (2.0–2.0) | 1.0 (1.0–1.0) | 1.5 (1.0–2.0) | ||
| 95%CI | [0.0;0.0] | [0.0;0.0] | [0.0;0.0] | ||
| 8:00 AM | n =24 | n = 28 | n = 24 | n = 76 | 0.0176 1 |
| mean (SD) | 2.1 (0.7) | 2.0 (0.7) | 2.7 (1.0) | 2.3 (0.9) | a 0.0388 2 |
| median (range) | 2.0 (1.0–4.0) | 2.0 (1.0–4.0) | 3.0 (1.0–4.0) | 2.0 (1.0–4.0) | |
| 95%CI | [1.8;2.4] | [1.7;2.3] | [2.3;3.1] | [2.1;2.5] | |
| 12:00 PM | n = 24 | n = 29 | n = 24 | n = 77 | >0.05 1 |
| mean (SD) | 1.8 (0.5) | 1.9 (0.8) | 2.4 (1.0) | 2.0 (0.8) | |
| median (range) | 2.0 (1.0–3.0) | 2.0 (1.0–4.0) | 2.5 (1.0–4.0) | 2.0 (1.0–4.0) | |
| 95%CI | [1.6;2.0] | [1.6;2.2] | [2.0;2.8] | [1.8;2.2] | |
| 4:00 PM | n = 24 | n = 29 | n = 24 | n = 77 | 0.2182 1 |
| mean (SD) | 1.8 (0.6) | 1.8 (0.8) | 2.2 (0.9) | 1.9 (0.8) | |
| median (range) | 2.0 (1.0–3.0) | 2.0 (1.0–4.0) | 2.0 (1.0–4.0) | 2.0 (1.0–4.0) | |
| 95%CI | [1.5;2.0] | [1.5;2.1] | [1.8;2.5] | [1.8;2.1] |
| SAPB (n = 24) | PVB (n = 30) | ESPB (n = 24) | Total (n = 78) | p-Value | |
|---|---|---|---|---|---|
| 1 h after the procedure | n = 20 | n = 28 | n = 23 | n = 71 | 0.8809 1 |
| mean (SD) | 4.8 (1.6) | 4.8 (1.7) | 4.8 (1.4) | 4.8 (1.6) | |
| median (range) | 5.0 (2.0–8.0) | 5.0 (1.0–8.0) | 4.0 (3.0–8.0) | 5.0 (1.0–8.0) | |
| 95%CI | [4.1;5.5] | [4.2;5.5] | [4.2;5.4] | [4.4;5.2] | |
| 4:00 PM | n = 24 | n = 28 | n = 24 | n = 76 | 0.0010 1 |
| mean (SD) | 3.5 (0.9) | 3.5 (0.9) | 4.5 (1.1) | 3.8 (1.0) | a 0.0080 2 |
| median (range) | 3.0 (1.0–5.0) | 3.0 (2.0–5.0) | 4.5 (2.0–6.0) | 4.0 (1.0–6.0) | b 0.0045 2 |
| 95%CI | [3.1;3.9] | [3.2;3.8] | [4.0;4.9] | [3.5;4.0] | |
| 8:00 PM | n = 24 | n = 28 | n = 24 | n = 76 | 0.0010 1 |
| mean (SD) | 3.5 (0.9) | 3.5 (0.9) | 4.5 (1.1) | 3.8 (1.0) | a 0.0080 2 |
| median (range) | 3.0 (1.0–5.0) | 3.0 (2.0–5.0) | 4.5 (2.0–6.0) | 4.0 (1.0–6.0) | b 0.0045 2 |
| 95%CI | [3.1;3.9] | [3.2;3.8] | [4.0;4.9] | [3.5;4.0] | |
| 12:00 AM | n = 2 | n = 7 | n = 6 | n = 15 | -- |
| mean (SD) | 3.5 (0.7) | 3.6 (0.8) | 3.7 (0.8) | 3.6 (0.7) | |
| median (range) | 3.5 (3.0–4.0) | 3.0 (3.0–5.0) | 3.5 (3.0–5.0) | 3.0 (3.0–5.0) | |
| 95%CI | [−2.9;9.9] | [2.8;4.3] | [2.8;4.5] | [3.2;4.0] | |
| 4:00 AM | n = 0 | n = 1 | n = 1 | n = 2 | -- |
| mean (SD) | 3.0 (0.0) | 1.0 (0.0) | 2.0 (1.4) | ||
| median (range) | 3.0 (3.0–3.0) | 1.0 (1.0–1.0) | 2.0 (1.0–3.0) | ||
| 95%CI | [0.0;0.0] | [0.0;0.0] | [0.0;0.0] | ||
| 8:00 AM | n =24 | n = 28 | n = 24 | n = 76 | 0.0128 1 |
| mean (SD) | 3.1 (0.7) | 3.1 (0.8) | 3.7 (0.9) | 3.3 (0.8) | a 0.0478 2 |
| median (range) | 3.0 (2.0–5.0) | 3.0 (2.0–5.0) | 4.0 (2.0–5.0) | 3.0 (2.0–5.0) | |
| 95%CI | [2.8;3.4] | [2.8;3.4] | [3.3;4.1] | [3.1;3.5] | |
| 12:00 PM | n = 24 | n = 29 | n = 24 | n = 77 | 0.0097 1 |
| mean (SD) | 2.8 (0.5) | 2.8 (0.8) | 3.4 (0.9) | 3.0 (0.8) | a 0.0253 2 |
| median (range) | 3.0 (2.0–4.0) | 3.0 (2.0–5.0) | 3.0 (2.0–5.0) | 3.0 (2.0–5.0) | |
| 95%CI | [2.6;3.0] | [2.5;3.1] | [3.0;3.7] | [2.8;3.1] | |
| 4:00 PM | n = 24 | n = 29 | n = 24 | n = 77 | >0.05 1 |
| mean (SD) | 2.8 (0.6) | 2.6 (0.7) | 3.2 (0.9) | 2.8 (0.8) | |
| median (range) | 3.0 (2.0–4.0) | 3.0 (2.0–5.0) | 3.0 (2.0–5.0) | 3.0 (2.0–5.0) | |
| 95%CI | [2.5;3.0] | [2.3;2.9] | [2.8;3.5] | [2.7;3.0] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
But, M.; Wernicki, K.; Zieliński, J.; Szczecińska, W. A Comparison of the Effectiveness of the Serratus Anterior Plane Block and Erector Spinae Plane Block to that of the Paravertebral Block in the Surgical Treatment of Breast Cancer—A Randomized, Prospective, Single-Blinded Study. J. Clin. Med. 2024, 13, 4836. https://doi.org/10.3390/jcm13164836
But M, Wernicki K, Zieliński J, Szczecińska W. A Comparison of the Effectiveness of the Serratus Anterior Plane Block and Erector Spinae Plane Block to that of the Paravertebral Block in the Surgical Treatment of Breast Cancer—A Randomized, Prospective, Single-Blinded Study. Journal of Clinical Medicine. 2024; 13(16):4836. https://doi.org/10.3390/jcm13164836
Chicago/Turabian StyleBut, Michał, Krzysztof Wernicki, Jacek Zieliński, and Weronika Szczecińska. 2024. "A Comparison of the Effectiveness of the Serratus Anterior Plane Block and Erector Spinae Plane Block to that of the Paravertebral Block in the Surgical Treatment of Breast Cancer—A Randomized, Prospective, Single-Blinded Study" Journal of Clinical Medicine 13, no. 16: 4836. https://doi.org/10.3390/jcm13164836
APA StyleBut, M., Wernicki, K., Zieliński, J., & Szczecińska, W. (2024). A Comparison of the Effectiveness of the Serratus Anterior Plane Block and Erector Spinae Plane Block to that of the Paravertebral Block in the Surgical Treatment of Breast Cancer—A Randomized, Prospective, Single-Blinded Study. Journal of Clinical Medicine, 13(16), 4836. https://doi.org/10.3390/jcm13164836





