ACL Injury Etiology in Its Context: A Systems Thinking, Group Model Building Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
3. Results
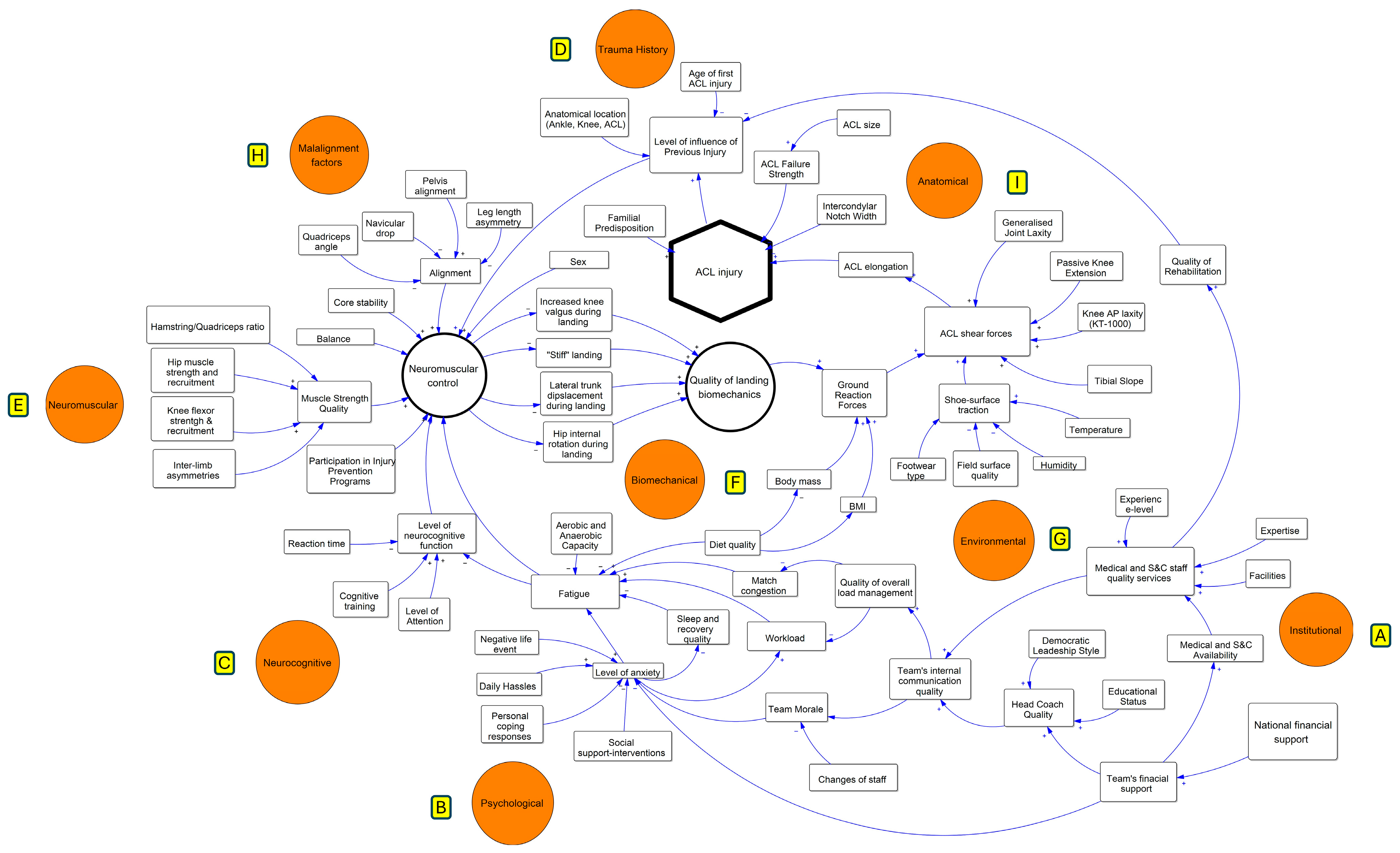
3.1. General Characteristics of the ACLI-CLD Model
3.2. Factors’ Interactions of Landing Mechanism
3.2.1. Effect of Neuromuscular Control on Quality of Landing Biomechanics
3.2.2. Effect of Neurocognitive, Institutional and Psychological Factors on Neuromuscular Control
3.2.3. Effect of Malalignment on Neuromuscular Control
3.2.4. Effect of Trauma History Characteristics, Sex, and Participation in Injury Prevention Programs on Neuromuscular Control
3.3. Effects of Anatomic and Environmental Factors on the Forces Transmitted to the ACL
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eliakim, E.; Morgulev, E.; Lidor, R.; Meckel, Y. Estimation of Injury Costs: Financial Damage of English Premier League Teams’ Underachievement Due to Injuries. BMJ Open Sport Exerc. Med. 2020, 6, e000675. [Google Scholar] [CrossRef] [PubMed]
- Suter, L.G.; Smith, S.R.; Katz, J.N.; Englund, M.; Hunter, D.J.; Frobell, R.; Losina, E. Projecting Lifetime Risk of Symptomatic Knee Osteoarthritis and Total Knee Replacement in Individuals Sustaining a Complete Anterior Cruciate Ligament Tear in Early Adulthood. Arthritis Care Res. 2017, 69, 201–208. [Google Scholar] [CrossRef]
- Chia, L.; De Oliveira Silva, D.; Whalan, M.; McKay, M.J.; Sullivan, J.; Fuller, C.W.; Pappas, E. Non-Contact Anterior Cruciate Ligament Injury Epidemiology in Team-Ball Sports: A Systematic Review with Meta-Analysis by Sex, Age, Sport, Participation Level, and Exposure Type. Sports Med. 2022, 52, 2447–2467. [Google Scholar] [CrossRef]
- Silvers-Granelli, H.; Mandelbaum, B.; Adeniji, O.; Insler, S.; Bizzini, M.; Pohlig, R.; Junge, A.; Snyder-Mackler, L.; Dvorak, J. Efficacy of the FIFA 11+ Injury Prevention Program in the Collegiate Male Soccer Player. Am. J. Sports Med. 2015, 43, 2628–2637. [Google Scholar] [CrossRef]
- Waldén, M.; Hägglund, M.; Magnusson, H.; Ekstrand, J. ACL Injuries in Men’s Professional Football: A 15-Year Prospective Study on Time Trends and Return-to-Play Rates Reveals Only 65% of Players Still Play at the Top Level 3 Years after ACL Rupture. Br. J. Sports Med. 2016, 50, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Maniar, N.; Verhagen, E.; Bryant, A.L.; Opar, D.A. Trends in Australian Knee Injury Rates: An Epidemiological Analysis of 228,344 Knee Injuries over 20 Years. Lancet Reg. Health West. Pac. 2022, 21, 100409. [Google Scholar] [CrossRef]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex Systems Approach for Sports Injuries: Moving from Risk Factor Identification to Injury Pattern Recognition—Narrative Review and New Concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [PubMed]
- Mehl, J.; Diermeier, T.; Herbst, E.; Imhoff, A.B.; Stoffels, T.; Zantop, T.; Petersen, W.; Achtnich, A. Evidence-Based Concepts for Prevention of Knee and ACL Injuries. 2017 Guidelines of the Ligament Committee of the German Knee Society (DKG). Arch. Orthop. Trauma Surg. 2017, 138, 51–61. [Google Scholar] [CrossRef]
- Hewett, T.E.; Ford, K.R.; Hoogenboom, B.J.; Myer, G.D. Understanding and Preventing Acl Injuries: Current Biomechanical and Epidemiologic Considerations—Update 2010. N. Am. J. Sports Phys. Ther. 2010, 5, 234–251. [Google Scholar]
- Alentorn-Geli, E.; Myer, G.D.; Silvers, H.J.; Samitier, G.; Romero, D.; Lázaro-Haro, C.; Cugat, R. Prevention of Non-Contact Anterior Cruciate Ligament Injuries in Soccer Players. Part 2: A Review of Prevention Programs Aimed to Modify Risk Factors and to Reduce Injury Rates. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 859–879. [Google Scholar] [CrossRef]
- Huang, Y.L.; Jung, J.; Mulligan, C.M.S.; Oh, J.; Norcross, M.F. A Majority of Anterior Cruciate Ligament Injuries Can Be Prevented by Injury Prevention Programs: A Systematic Review of Randomized Controlled Trials and Cluster-Randomized Controlled Trials With Meta-Analysis. Am. J. Sports Med. 2020, 48, 1505–1515. [Google Scholar] [CrossRef] [PubMed]
- Collings, T.J.; Bourne, M.N.; Barrett, R.S.; du Moulin, W.; Hickey, J.T.; Diamond, L.E. Risk Factors for Lower Limb Injury in Female Team Field and Court Sports: A Systematic Review, Meta-Analysis, and Best Evidence Synthesis. Sports Med. 2021, 51, 759–776. [Google Scholar] [CrossRef]
- Dingenen, B.; Malfait, B.; Nijs, S.; Peers, K.H.E.; Vereecken, S.; Verschueren, S.M.P.; Staes, F.F. Can Two-Dimensional Video Analysis during Single-Leg Drop Vertical Jumps Help Identify Non-Contact Knee Injury Risk? A One-Year Prospective Study. Clin. Biomech. 2015, 30, 781–787. [Google Scholar] [CrossRef]
- Smith, H.C.; Vacek, P.; Johnson, R.J.; Slauterbeck, J.R.; Hashemi, J.; Shultz, S.; Beynnon, B.D. Risk Factors for Anterior Cruciate Ligament Injury: A Review of the Literature—Part 1: Neuromuscular and Anatomic Risk. Sports Health 2012, 4, 69–78. [Google Scholar] [CrossRef]
- Vacek, P.M.; Slauterbeck, J.R.; Tourville, T.W.; Sturnick, D.R.; Holterman, L.A.; Smith, H.C.; Shultz, S.J.; Johnson, R.J.; Tourville, K.J.; Beynnon, B.D. Multivariate Analysis of the Risk Factors for First-Time Noncontact ACL Injury in High School and College Athletes: A Prospective Cohort Study with a Nested, Matched Case-Control Analysis. Am. J. Sports Med. 2016, 44, 1492–1501. [Google Scholar] [CrossRef]
- Beynnon, B.D.; Tourville, T.W.; Hollenbach, H.C.; Shultz, S.; Vacek, P. Intrinsic Risk Factors for First-Time Noncontact ACL Injury: A Prospective Study of College and High School Athletes. Sports Health 2023, 15, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, S.T.; Souza, T.R.; Verhagen, E.; van Emmerik, R.; Bittencourt, N.F.N.; Mendonça, L.D.M.; Andrade, A.G.P.; Resende, R.A.; Ocarino, J.M. Sports Injury Forecasting and Complexity: A Synergetic Approach. Sports Med. 2020, 50, 1757–1770. [Google Scholar] [CrossRef] [PubMed]
- Finch, C. A New Framework for Research Leading to Sports Injury Prevention. J. Sci. Med. Sport 2006, 9, 3–9. [Google Scholar] [CrossRef]
- Fältström, A.; Kvist, J.; Bittencourt, N.F.N.; Mendonça, L.D.; Hägglund, M. Clinical Risk Profile for a Second Anterior Cruciate Ligament Injury in Female Soccer Players after Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2021, 49, 1421–1430. [Google Scholar] [CrossRef]
- Fältström, A.; Hägglund, M.; Kvist, J.; Mendonça, L.D. Risk Factors for Sustaining a Second ACL Injury after Primary ACL Reconstruction in Female Football Players: A Study Investigating the Effects of Follow-Up Time and the Statistical Approach. Sports Med. Open 2023, 9, 29. [Google Scholar] [CrossRef]
- Bolling, C.; Van Mechelen, W.; Pasman, H.R.; Verhagen, E. Context Matters: Revisiting the First Step of the “Sequence of Prevention” of Sports Injuries. Sports Med. 2018, 48, 2227–2234. [Google Scholar] [CrossRef]
- Hovmand, P.S.; Andersen, D.F.; Rouwette, E.; Richardson, G.P.; Rux, K.; Calhoun, A. Group Model-Building ‘Scripts’ as a Collaborative Planning Tool. Syst. Res. Behav. Sci. 2012, 29, 179–193. [Google Scholar] [CrossRef]
- Bérard, C. Group Model Building Using System Dynamics: An Analysis of Methodological Frameworks. Electron. J. Bus. Res. Methods 2010, 8, 13–24. [Google Scholar]
- Hulme, A.; Thompson, J.; Nielsen, R.O.; Read, G.J.M.; Salmon, P.M. Towards a Complex Systems Approach in Sports Injury Research: Simulating Running-Related Injury Development with Agent-Based Modelling. Br. J. Sports Med. 2019, 53, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Sterman, J.D. Business Dynamics: Systems Thinking and Modeling for a Complex World, 1st ed.; McGraw-Hill Higher Education; Irwin/McGraw-Hill: Boston, MA, USA, 2000; Volume 19, ISBN 9780072311358. [Google Scholar]
- Liveris, N.I.; Papageorgiou, G.; Tsepis, E.; Fousekis, K.; Tsarbou, C.; Xergia, S.A. Towards the Development of a System Dynamics Model for the Prediction of Lower Extremity Injuries. Int. J. Exerc. Sci. 2023, 16, 1052–1065. [Google Scholar]
- Liveris, N.I.; Tsarbou, C.; Papageorgiou, G.; Tsepis, E.; Fousekis, K.; Kvist, J.; Xergia, S.A. The Complex Interrelationships of the Risk Factors Leading to Hamstring Injury and Implications for Injury Prevention: A Group Model Building Approach. Appl. Sci. 2024, 14, 6316. [Google Scholar] [CrossRef]
- Hovmand, P.; Rouwette, E.; Andersen, D.; Richardson, G.P.; Calhoun, A.; Rux, K.; Hower, T. Scriptapedia: A Handbook of Scripts for Developing Structured Group Model Building Sessions. In Proceedings of the 2011 System Dynamics Conference, Washington, DC, USA, 24–28 July 2011; pp. 1476–1491. Available online: https://hdl.handle.net/2066/95406 (accessed on 16 March 2024).
- Hovmand, P.S.; Rouwette, E.; Andersen, D.F.; Richardson, G.P. Scriptapedia. Available online: https://en.wikibooks.org/wiki/Scriptapedia (accessed on 16 March 2024).
- Hewett, T.E.; Stroupe, A.L.; Nance, T.A.; Noyes, F.R. Plyometric Training in Female Athletes: Decreased Impact Forces and Increased Hamstring Torques. Am. J. Sports Med. 1996, 24, 765–773. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Myer, G.D. The Mechanistic Connection between the Trunk, Hip, Knee, and Anterior Cruciate Ligament Injury. Exerc. Sport Sci. Rev. 2011, 39, 161–166. [Google Scholar] [CrossRef]
- Boden, B.P.; Dean, C.S.; Feagin, J.A.; Garrett, W.E. Mechanisms of Anterior Cruciate Ligament Injury. Orthopedics 2000, 23, 573–578. [Google Scholar] [CrossRef]
- Della Villa, F.; Buckthorpe, M.; Grassi, A.; Nabiuzzi, A.; Tosarelli, F.; Zaffagnini, S.; Della Villa, S. Systematic Video Analysis of ACL Injuries in Professional Male Football (Soccer): Injury Mechanisms, Situational Patterns and Biomechanics Study on 134 Consecutive Cases. Br. J. Sports Med. 2020, 54, 1423–1432. [Google Scholar] [CrossRef]
- Weinhandl, J.T.; Earl-Boehm, J.E.; Ebersole, K.T.; Huddleston, W.E.; Armstrong, B.S.R.; O’Connor, K.M. Reduced Hamstring Strength Increases Anterior Cruciate Ligament Loading during Anticipated Sidestep Cutting. Clin. Biomech. 2014, 29, 752–759. [Google Scholar] [CrossRef]
- Arumugam, A.; Häger, C.K. Thigh Muscle Co-Contraction Patterns in Individuals with Anterior Cruciate Ligament Reconstruction, Athletes and Controls during a Novel Double-Hop Test. Sci. Rep. 2022, 12, 8431. [Google Scholar] [CrossRef]
- Barcellona, M.G.; Morrissey, M.C.; Milligan, P.; Amis, A.A. The Effect of Thigh Muscle Activity on Anterior Knee Laxity in the Uninjured and Anterior Cruciate Ligament-Injured Knee. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2821–2829. [Google Scholar] [CrossRef] [PubMed]
- Pfile, K.; Boling, M.; Baellow, A.; Zuk, E.; Nguyen, A.-D. Greater Core Endurance Identifies Improved Mechanics during Jump Landing in Female Youth Soccer Athletes. Women Sport Phys. Act. J. 2023, 32, 1–7. [Google Scholar] [CrossRef]
- Straub, R.K.; Powers, C.M. Is Muscular Strength a Predictor for Primary or Secondary ACL Injury? A Scoping Review of Prospective Studies. Phys. Ther. Sport 2023, 61, 91–101. [Google Scholar] [CrossRef]
- Jeong, J.; Choi, D.-H.; Shin, C.S. Core Strength Training Can Alter Neuromuscular and Biomechanical Risk Factors for Anterior Cruciate Ligament Injury. Am. J. Sports Med. 2021, 49, 183–192. [Google Scholar] [CrossRef]
- Maniar, N.; Schache, A.G.; Sritharan, P.; Opar, D.A. Non-Knee-Spanning Muscles Contribute to Tibiofemoral Shear as Well as Valgus and Rotational Joint Reaction Moments during Unanticipated Sidestep Cutting. Sci. Rep. 2018, 8, 2501. [Google Scholar] [CrossRef]
- Dix, J.; Marsh, S.; Dingenen, B.; Malliaras, P. The Relationship between Hip Muscle Strength and Dynamic Knee Valgus in Asymptomatic Females: A Systematic Review. Phys. Ther. Sport 2019, 37, 197–209. [Google Scholar] [CrossRef]
- Khayambashi, K.; Ghoddosi, N.; Straub, R.K.; Powers, C.M. Hip Muscle Strength Predicts Noncontact Anterior Cruciate Ligament Injury in Male and Female Athletes: A Prospective Study. Am. J. Sports Med. 2016, 44, 355–361. [Google Scholar] [CrossRef]
- De Blaiser, C.; Roosen, P.; Willems, T.; De Bleecker, C.; Vermeulen, S.; Danneels, L.; De Ridder, R. The Role of Core Stability in the Development of Non-Contact Acute Lower Extremity Injuries in an Athletic Population: A Prospective Study. Phys. Ther. Sport 2021, 47, 165–172. [Google Scholar] [CrossRef]
- Withrow, T.J.; Huston, L.J.; Wojtys, E.M.; Ashton-Miller, J.A. Effect of Varying Hamstring Tension on Anterior Cruciate Ligament Strain During in Vitro Impulsive Knee Flexion and Compression Loading. J. Bone Jt. Surg. Am. 2008, 90, 815–823. [Google Scholar] [CrossRef]
- MacWilliams, B.A.; Wilson, D.R.; Desjardins, J.D.; Romero, J.; Chao, E.Y.S. Hamstrings Cocontraction Reduces Internal Rotation, Anterior Translation, and Anterior Cruciate Ligament Load in Weight-Bearing Flexion. J. Orthop. Res. 1999, 17, 817–822. [Google Scholar] [CrossRef] [PubMed]
- Myer, G.D.; Ford, K.R.; Barber Foss, K.D.; Liu, C.; Nick, T.G.; Hewett, T.E. The Relationship of Hamstrings and Quadriceps Strength to Anterior Cruciate Ligament Injury in Female Athletes. Clin. J. Sport Med. 2009, 19, 3–8. [Google Scholar] [CrossRef]
- Ford, K.R.; Van Den Bogert, J.; Myer, G.D.; Shapiro, R.; Hewett, T.E. The Effects of Age and Skill Level on Knee Musculature Co-Contraction during Functional Activities: A Systematic Review. Br. J. Sports Med. 2008, 42, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Paterno, M.V.; Schmitt, L.C.; Ford, K.R.; Rauh, M.J.; Myer, G.D.; Huang, B.; Hewett, T.E. Biomechanical Measures during Landing and Postural Stability Predict Second Anterior Cruciate Ligament Injury after Anterior Cruciate Ligament Reconstruction and Return to Sport. Am. J. Sports Med. 2010, 38, 1968–1978. [Google Scholar] [CrossRef] [PubMed]
- Taketomi, S.; Kawaguchi, K.; Mizutani, Y.; Takei, S.; Yamagami, R.; Kono, K.; Murakami, R.; Kage, T.; Arakawa, T.; Fujiwara, S.; et al. Lower Hamstring to Quadriceps Muscle Strength Ratio and Lower Body Weight as Factors Associated with Noncontact Anterior Cruciate Ligament Injury in Male American Football Players: A Prospective Cohort Study. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2023, 35, 43–47. [Google Scholar] [CrossRef]
- Benjaminse, A.; Webster, K.E.; Kimp, A.; Meijer, M.; Gokeler, A. Revised Approach to the Role of Fatigue in Anterior Cruciate Ligament Injury Prevention: A Systematic Review with Meta-Analyses. Sports Med. 2019, 49, 565–586. [Google Scholar] [CrossRef] [PubMed]
- Wesley, C.A.; Aronson, P.A.; Docherty, C.L. Lower Extremity Landing Biomechanics in Both Sexes after a Functional Exercise Protocol. J. Athl. Train. 2015, 50, 914–920. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Xia, R.; Dai, B.; Sun, X.; Fu, W. Effects of Exercise-Induced Fatigue on Lower Extremity Joint Mechanics, Stiffness, and Energy Absorption during Landings. J. Sports Sci. Med. 2018, 17, 640–649. [Google Scholar]
- Liederbach, M.; Kremenic, I.J.; Orishimo, K.F.; Pappas, E.; Hagins, M. Comparison of Landing Biomechanics between Male and Female Dancers and Athletes, Part 2: Influence of Fatigue and Implications for Anterior Cruciate Ligament Injury. Am. J. Sports Med. 2014, 42, 1089–1095. [Google Scholar] [CrossRef]
- O’Connor, K.M.; Johnson, C.; Benson, L.C. The Effect of Isolated Hamstrings Fatigue on Landing and Cutting Mechanics. J. Appl. Biomech. 2015, 31, 211–220. [Google Scholar] [CrossRef]
- Borotikar, B.S.; Newcomer, R.; Koppes, R.; McLean, S.G. Combined Effects of Fatigue and Decision Making on Female Lower Limb Landing Postures: Central and Peripheral Contributions to ACL Injury Risk. Clin. Biomech. 2008, 23, 81–92. [Google Scholar] [CrossRef]
- von Rosen, P.; Frohm, A.; Kottorp, A.; Fridén, C.; Heijne, A. Too Little Sleep and an Unhealthy Diet Could Increase the Risk of Sustaining a New Injury in Adolescent Elite Athletes. Scand. J. Med. Sci. Sports 2017, 27, 1364–1371. [Google Scholar] [CrossRef]
- Andersen, M.B.; Williams, J.M. A Model of Stress and Athletic Injury: Prediction and Prevention. J. Sport Exerc. Psychol. 1988, 10, 294–306. [Google Scholar] [CrossRef]
- Gokeler, A.; Benjaminse, A.; Della Villa, F.; Tosarelli, F.; Verhagen, E.; Baumeister, J. Anterior Cruciate Ligament Injury Mechanisms through a Neurocognition Lens: Implications for Injury Screening. BMJ Open Sport Exerc. Med. 2021, 7, e001091. [Google Scholar] [CrossRef] [PubMed]
- Windt, J.; Gabbett, T.J. How Do Training and Competition Workloads Relate to Injury? The Workload—Injury Aetiology Model. Br. J. Sports Med. 2017, 51, 428–435. [Google Scholar] [CrossRef]
- Ommundsen, Y.; Roberts, G.C.; Lemyre, P.-N.; Miller, B.W. Parental and Coach Support or Pressure on Psychosocial Outcomes of Pediatric Athletes in Soccer. Clin. J. Sport Med. 2006, 16, 522–526. [Google Scholar] [CrossRef]
- Wadey, R.; Day, M.; Cavallerio, F.; Martinelli, L. Multilevel Model of Sport Injury (MMSI): Can Coaches Impact and Be Impacted by Injury? 1st ed.; Routledge: London, UK, 2018; ISBN 9781351210980. [Google Scholar]
- Ekstrand, J.; Lundqvist, D.; Davison, M.; D’Hooghe, M.; Pensgaard, A.M. Communication Quality between the Medical Team and the Head Coach/Manager Is Associated with Injury Burden and Player Availability in Elite Football Clubs. Br. J. Sports Med. 2019, 53, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.J.; Carcia, C.R.; Gansneder, B.M.; Perrin, D.H. The Independent and Interactive Effects of Navicular Drop and Quadriceps Angle on Neuromuscular Responses to a Weight-Bearing Perturbation. J. Athl. Train. 2006, 41, 251–259. [Google Scholar]
- Eliks, M.; Ostiak-Tomaszewska, W.; Lisiński, P.; Koczewski, P. Does Structural Leg-Length Discrepancy Affect Postural Control? Preliminary Study. BMC Musculoskelet. Disord. 2017, 18, 346. [Google Scholar] [CrossRef]
- Toohey, L.A.; Drew, M.K.; Cook, J.L.; Finch, C.F.; Gaida, J.E. Is Subsequent Lower Limb Injury Associated with Previous Injury? A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2017, 51, 1670–1678. [Google Scholar] [CrossRef] [PubMed]
- Kramer, L.C.; Denegar, C.R.; Buckley, W.E.; Hertel, J. Factors Associated with Anterior Cruciate Ligament Injury: History in Female Athletes. J. Sports Med. Phys. Fitness 2007, 47, 446–454. [Google Scholar]
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef] [PubMed]
- Hasani, S.; Feller, J.A.; Webster, K.E. Familial Predisposition to Anterior Cruciate Ligament Injury: A Systematic Review with Meta-Analysis. Sports Med. 2022, 52, 2657–2668. [Google Scholar] [CrossRef] [PubMed]
- Webster, K.E.; Hewett, T.E. Meta-analysis of Meta-analyses of Anterior Cruciate Ligament Injury Reduction Training Programs. J. Orthop. Res. 2018, 36, 2696–2708. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.L.; Coen, S.E.; Bekker, S. Anterior Cruciate Ligament Injury: Towards a Gendered Environmental Approach. Br. J. Sports Med. 2021, 55, 984–990. [Google Scholar] [CrossRef]
- Somerson, J.S.; Isby, I.J.; Hagen, M.S.; Kweon, C.Y.; Gee, A.O. The Menstrual Cycle May Affect Anterior Knee Laxity and the Rate of Anterior Cruciate Ligament Rupture: A Systematic Review and Meta-Analysis. JBJS Rev. 2019, 7, e2. [Google Scholar] [CrossRef]
- Zeitlin, J.; Fontana, M.A.; Parides, M.K.; Nawabi, D.H.; Wickiewicz, T.L.; Pearle, A.D.; Beynnon, B.D.; Imhauser, C.W. Key Thresholds and Relative Contributions of Knee Geometry, Anteroposterior Laxity, and Body Weight as Risk Factors for Noncontact ACL Injury. Orthop. J. Sports Med. 2023, 11, 23259671231163628. [Google Scholar] [CrossRef]
- Kiapour, A.M.; Wordeman, S.C.; Paterno, M.V.; Quatman, C.E.; Levine, J.W.; Goel, V.K.; Demetropoulos, C.K.; Hewett, T.E. Diagnostic Value of Knee Arthrometry in the Prediction of Anterior Cruciate Ligament Strain during Landing. Am. J. Sports Med. 2014, 42, 312–319. [Google Scholar] [CrossRef]
- Andrade, R.; Vasta, S.; Sevivas, N.; Pereira, R.; Leal, A.; Papalia, R.; Pereira, H.; Espregueira-Mendes, J. Notch Morphology Is a Risk Factor for ACL Injury: A Systematic Review and Meta-Analysis. J. ISAKOS 2016, 1, 70–81. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, T.; Zeng, C.; Wei, J.; Xie, D.; Yang, Y.; Long, H.; Xu, B.; Qian, Y.; Jiang, S.; et al. Association Between Tibial Plateau Slopes and Anterior Cruciate Ligament Injury: A Meta-Analysis. Arthroscopy 2017, 33, 1248–1259.e4. [Google Scholar] [CrossRef]
- Shao, Q.; MacLeod, T.D.; Manal, K.; Buchanan, T.S. Estimation of Ligament Loading and Anterior Tibial Translation in Healthy and ACL-Deficient Knees during Gait and the Influence of Increasing Tibial Slope Using EMG-Driven Approach. Ann. Biomed. Eng. 2011, 39, 110–121. [Google Scholar] [CrossRef]
- Guenther, D.; Herbst, E.; Musahl, V. Anatomy and Biomechanics of the Anterior Cruciate Ligament. In Orthopaedic Biomechanics in Sports Medicine; Springer International Publishing: Cham, Switzerland, 2021; pp. 287–295. [Google Scholar]
- McLean, S.G.; Oh, Y.K.; Palmer, M.L.; Lucey, S.M.; Lucarelli, D.G.; Ashton-Miller, J.A.; Wojtys, E.M. The Relationship Between Anterior Tibial Acceleration, Tibial Slope, and ACL Strain During a Simulated Jump Landing Task. J. Bone Jt. Surg. Am. 2011, 93, 1310. [Google Scholar] [CrossRef]
- Shultz, S.J.; Schmitz, R.J. Tibial Plateau Geometry Influences Lower Extremity Biomechanics during Landing. Am. J. Sports Med. 2012, 40, 2029–2036. [Google Scholar] [CrossRef]
- McLean, S.G.; Lucey, S.M.; Rohrer, S.; Brandon, C. Knee Joint Anatomy Predicts High-Risk in Vivo Dynamic Landing Knee Biomechanics. Clin. Biomech. 2010, 25, 781–788. [Google Scholar] [CrossRef]
- Shelburne, K.B.; Kim, H.J.; Sterett, W.I.; Pandy, M.G. Effect of Posterior Tibial Slope on Knee Biomechanics during Functional Activity. J. Orthop. Res. 2011, 29, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Li, C.; Li, L.; Wang, P. Correlation between Notch Width Index Assessed via Magnetic Resonance Imaging and Risk of Anterior Cruciate Ligament Injury: An Updated Meta-Analysis. Surg. Radiol. Anat. 2020, 42, 1209–1217. [Google Scholar] [CrossRef] [PubMed]
- Jha, V.; Azam, M.Q.; Jain, P.; Bali, S.A. Does Femoral Intercondylar Notch Volume Differ in Anterior Cruciate Ligament-Injured Adult Patients Compared to the Uninjured?: A Meta-Analysis. Clin. Orthop. Surg. 2022, 14, 76. [Google Scholar] [CrossRef]
- Zhang, C.; Zhang, X.; Fang, Z.; Wang, F.; Yuan, F.; Xie, G.; Zhao, J. The Correlation between Common 2D Femoral Notch Parameters and 3D Notch Volume: A Retrospective MRI Study. BMC Musculoskelet. Disord. 2019, 20, 146. [Google Scholar] [CrossRef]
- Chandrashekar, N.; Slauterbeck, J.; Hashemi, J. Sex-Based Differences in the Anthropometric Characteristics of the Anterior Cruciate Ligament and Its Relation to Intercondylar Notch Geometry: A Cadaveric Study. Am. J. Sports Med. 2005, 33, 1492–1498. [Google Scholar] [CrossRef]
- Thomson, A.; Whiteley, R.; Bleakley, C. Higher Shoe-Surface Interaction Is Associated with Doubling of Lower Extremity Injury Risk in Football Codes: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2015, 49, 1245–1252. [Google Scholar] [CrossRef] [PubMed]
- Lambson, R.B.; Barnhill, B.S.; Higgins, R.W. Football Cleat Design and Its Effect on Anterior Cruciate Ligament Injuries. A Three-Year Prospective Study. Am. J. Sports Med. 1996, 24, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Orchard, J.; Walden, M.; Hagglund, M.; Orchard, J.; Chivers, I.; Seward, H.; Ekstrand, J. Comparison of Injury Incidences between Football Teams Playing in Different Climatic Regions. Open Access J. Sports Med. 2013, 4, 251. [Google Scholar] [CrossRef]
- Torg, J.S.; Stilwell, G.; Rogers, K. The Effect of Ambient Temperature on the Shoe-Surface Interface Release Coefficient. Am. J. Sports Med. 1996, 24, 79–82. [Google Scholar] [CrossRef]
- O’Brien, J.; Finch, C.F.; Pruna, R.; McCall, A. A New Model for Injury Prevention in Team Sports: The Team-Sport Injury Prevention (TIP) Cycle. Sci. Med. Footb. 2019, 3, 77–80. [Google Scholar] [CrossRef]
- Romero-Franco, N.; Ortego-Mate, M.D.C.; Molina-Mula, J. Knee Kinematics During Landing: Is It Really a Predictor of Acute Noncontact Knee Injuries in Athletes? A Systematic Review and Meta-Analysis. Orthop. J. Sports Med. 2020, 8, 2325967120966952. [Google Scholar] [CrossRef]
- Chia, L.; de Oliveira Silva, D.; McKay, M.J.; Sullivan, J.; Micolis de Azevedo, F.; Pappas, E. Limited Support for Trunk and Hip Deficits as Risk Factors for Athletic Knee Injuries: A Systematic Review With Meta-Analysis and Best-Evidence Synthesis. J. Orthop. Sports Phys. Ther. 2020, 50, 476–489. [Google Scholar] [CrossRef]
- Cronström, A.; Creaby, M.W.; Ageberg, E. Do Knee Abduction Kinematics and Kinetics Predict Future Anterior Cruciate Ligament Injury Risk? A Systematic Review and Meta-Analysis of Prospective Studies. BMC Musculoskelet. Disord. 2020, 21, 563. [Google Scholar] [CrossRef]
- Mendonça, L. To Do or Not to Do?—The Value of the Preseason Assessment in Sport Injury Prevention. Int. J. Sports Phys. Ther. 2022, 17, 111–113. [Google Scholar] [CrossRef]
- Tsarbou, C.; Liveris, N.I.; Xergia, S.A.; Tsekoura, M.; Fousekis, K.; Tsepis, E. Pre-Season ACL Risk Classification of Professional and Semi-Professional Football Players, via a Proof-of-Concept Test Battery. Appl. Sci. 2023, 13, 7780. [Google Scholar] [CrossRef]
- Fan, Y.; Chen, J.; Shirkey, G.; John, R.; Wu, S.R.; Park, H.; Shao, C. Applications of Structural Equation Modeling (SEM) in Ecological Studies: An Updated Review. Ecol. Process 2016, 5, 19. [Google Scholar] [CrossRef]
- Vitharana, V.H.P.; Chinda, T. Structural Equation Modelling of Lower Back Pain Due to Whole-Body Vibration Exposure in the Construction Industry. Int. J. Occup. Saf. Ergon. 2019, 25, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Hulme, A.; Mclean, S.; Salmon, P.M.; Thompson, J.; Lane, B.R.; Nielsen, R.O. Computational Methods to Model Complex Systems in Sports Injury Research: Agent-Based Modelling (ABM) and Systems Dynamics (SD) Modelling. Br. J. Sports Med. 2019, 53, 1507–1510. [Google Scholar] [CrossRef] [PubMed]
| Steps | Task’s Purpose | Time | Script from Scriptapedia | Actions | Participants |
|---|---|---|---|---|---|
| A | To review the primary risk factors for anterior cruciate ligament injury (ACLI) through systematic reviews and pertinent literature | - | - | Create a list of ACLI risk factors for further discussion in the group modeling building workshops | Two members of the modeling Team |
| B | Group Modeling Building Workshops | ||||
| B1 | To discuss list of risk factors for ACLI | 120′ | Variable elicitation | Participants discuss the variables and remove or add variables. | Modeling Team and two members of the stakeholders’ team |
| B1.1 | To develop a CLD for ACLI (ACLI-CLD) using literature as a reference and incorporating the insights gained from the previous GMB session’s discussion | - | - | Developing an initial understanding of the ACLI risk factors’ interplay | One member of the modeling team |
| B2 | To engage in conversation and evaluate the ACLI-CLD with the modeling team | 120′ | 1. Causal Mapping with Seed Structure, 2. Model Review 3. Next steps and closing | Review the ACLI-CLD and propose corrections | Modeling Team |
| B3 | To review ACLI-CLD with the modeling team | 60′ | 1. Model Review, 2. Next Steps and Closing | Review the ACLI-CLD after the corrections and prepare the following steps | Modeling team |
| B4 | To present ACLI-CLD to stakeholders and integrate their perspectives | 120′ | 1. Modeling project community presentation, 2. Model Review | Presentation of the ACLI-CLD to stakeholders, accompanied by a discussion of the ACLI-CLD and its constituent variables | Modeling team and all members of the Stakeholders’ team |
| B5 | To review the ACLI-CLD and incorporate stakeholders’ points of view | 90′ | Initiating and elaborating a “Causal Loop Diagram” or “Stock and Flow” Model, 2. Model Review | Summarizing the inputs from stakeholders | Modeling Team |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsarbou, C.; Liveris, N.I.; Xergia, S.A.; Papageorgiou, G.; Kvist, J.; Tsepis, E. ACL Injury Etiology in Its Context: A Systems Thinking, Group Model Building Approach. J. Clin. Med. 2024, 13, 4928. https://doi.org/10.3390/jcm13164928
Tsarbou C, Liveris NI, Xergia SA, Papageorgiou G, Kvist J, Tsepis E. ACL Injury Etiology in Its Context: A Systems Thinking, Group Model Building Approach. Journal of Clinical Medicine. 2024; 13(16):4928. https://doi.org/10.3390/jcm13164928
Chicago/Turabian StyleTsarbou, Charis, Nikolaos I. Liveris, Sofia A. Xergia, George Papageorgiou, Joanna Kvist, and Elias Tsepis. 2024. "ACL Injury Etiology in Its Context: A Systems Thinking, Group Model Building Approach" Journal of Clinical Medicine 13, no. 16: 4928. https://doi.org/10.3390/jcm13164928






