An Association between HTRA1 and TGF-β2 in the Vitreous Humor of Patients with Chorioretinal Vascular Diseases
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Ophthalmic Examinations
2.4. Collection of Vitreous Humor
2.5. Measurement of TGF-, TGF-, TGF- and VEGF in the Vitreous Humor
2.6. Measurement of HTRA1 in the Vitreous Humor
2.7. Statistical Analysis
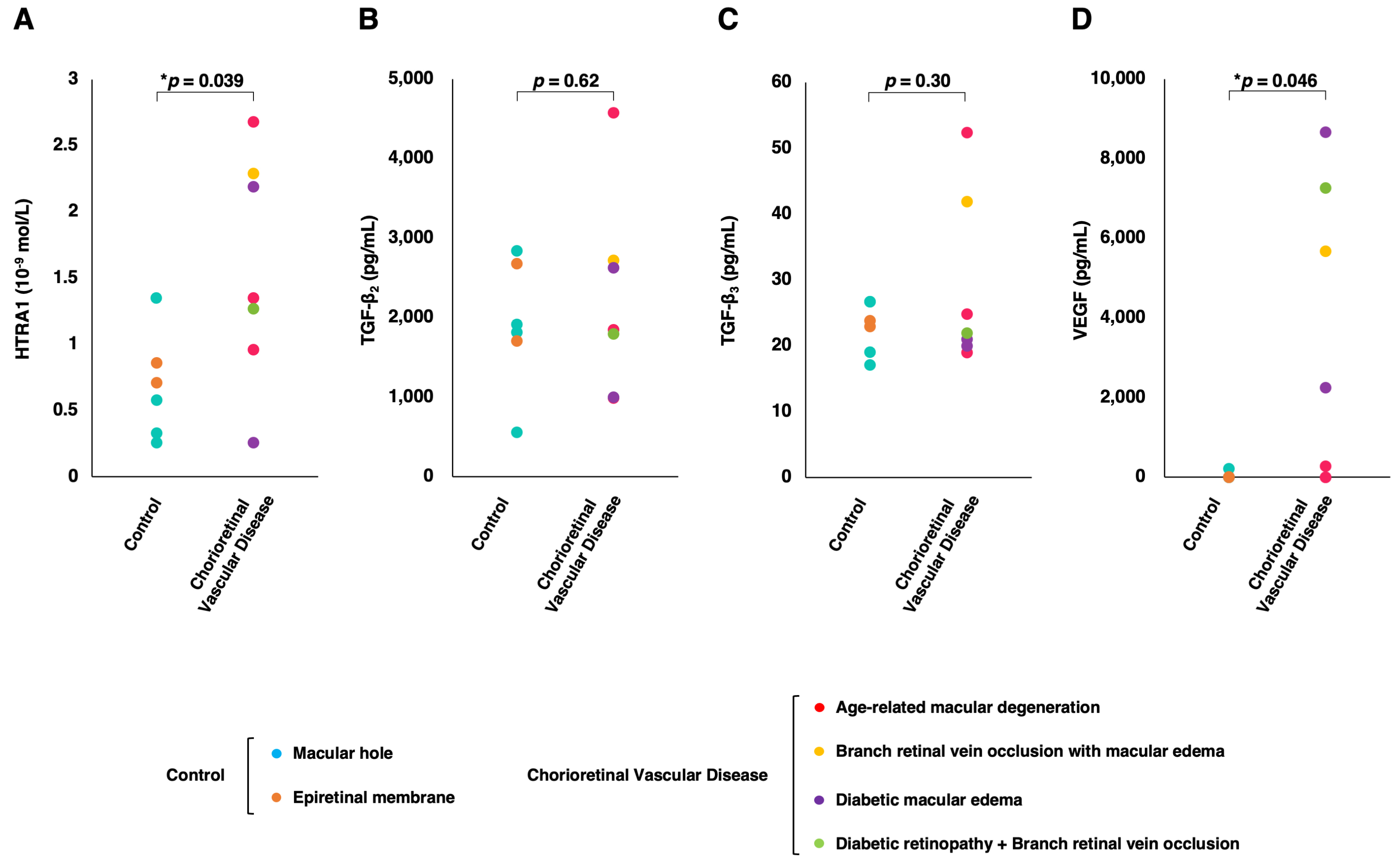
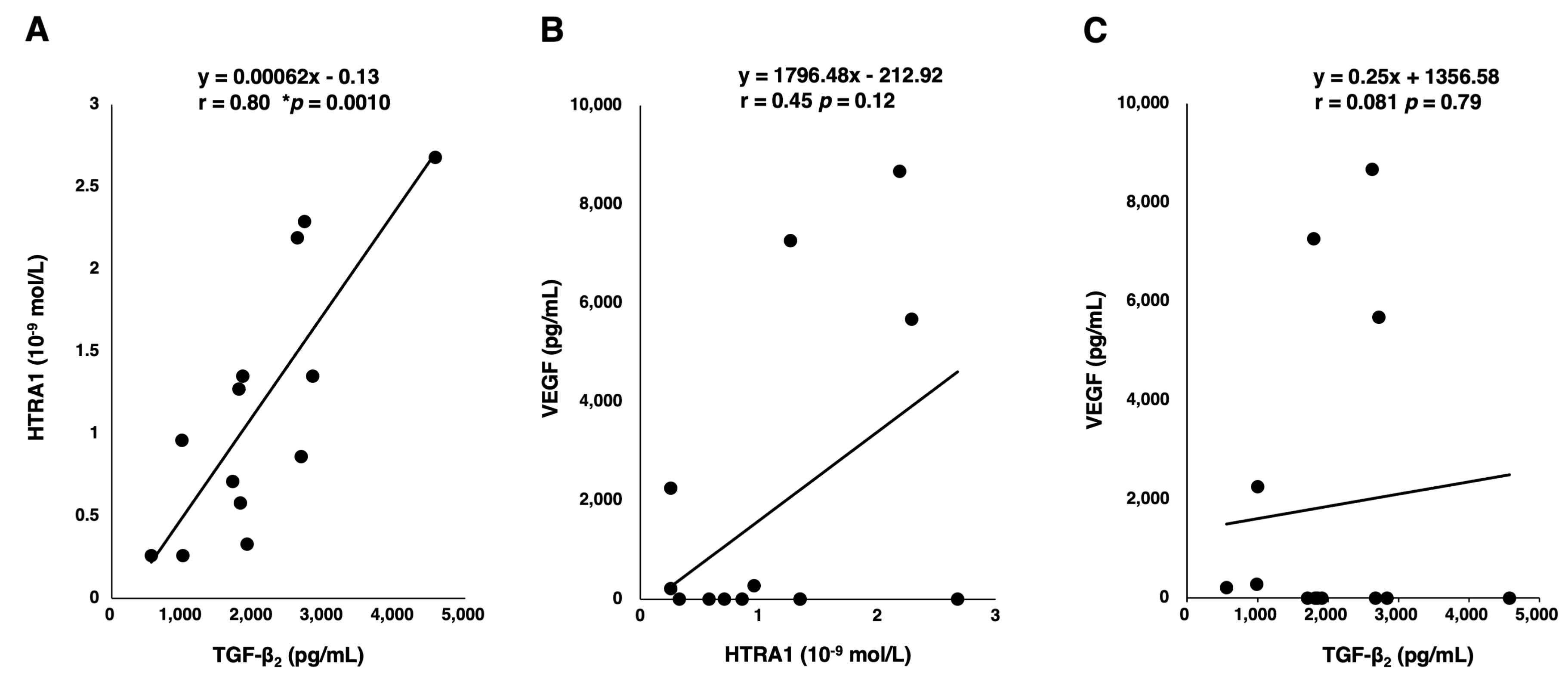
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HTRA1 | Human high-temperature requirement A 1 |
| AMD | Age-related macular degeneration |
| TGF- | Transforming growth factor beta |
| VEGF | Vascular endothelial growth factor |
| DR | Diabetic retinopathy |
| RVO | Optical coherence tomography |
| FA | Fluorescein angiography |
| non-PDR | Non-proliferative diabetic retinopathy |
| DME | Diabetic macular edema |
| BRVO | Branch retinal vein occlusion |
| CI | Confidence interval |
References
- Zurawa-Janicka, D.; Skorko-Glonek, J.; Lipinska, B.T. HtrA proteins as targets in therapy of cancer and other diseases. Expert. Opin. Ther. Targets 2010, 14, 665–679. [Google Scholar] [CrossRef] [PubMed]
- Oka, C.; Saleh, R.; Bessho, Y.; Reza, H.M. Interplay between HTRA1 and classical signalling pathways in organogenesis and diseases. Saudi J. Biol. Sci. 2022, 29, 1919–1927. [Google Scholar] [CrossRef] [PubMed]
- Hara, K.; Shiga, A.; Fukutake, T.; Nozaki, H.; Miyashita, A.; Yokoseki, A.; Kawata, H.; Koyama, A.; Arima, K.; Takahashi, T.; et al. Association of HTRA1 mutations and familial ischemic cerebral small-vessel disease. N. Engl. J. Med. 2009, 360, 1729–1739. [Google Scholar] [CrossRef] [PubMed]
- Iejima, D.; Nakayama, M.; Iwata, T. HTRA1 overexpression induces the exudative form of age-related macular degeneration. J. Stem Cells 2015, 10, 193–203. [Google Scholar]
- Iejima, D.; Itabashi, T.; Kawamura, Y.; Noda, T.; Yuasa, S.; Fukuda, K.; Oka, C.; Iwata, T. HTRA1 (high temperature require-ment A serine peptidase 1) gene is transcriptionally regulated by insertion/deletion nucleotides located at the 3′ end of the ARMS2 (age-related maculopathy susceptibility 2) gene in patients with age-related macular degeneration. J. Biol. Chem. 2015, 290, 2784–2797. [Google Scholar]
- Oura, Y.; Nakamura, M.; Takigawa, T.; Fukushima, Y.; Wakabayashi, T.; Tsujikawa, M.; Nishida, K. High-temperature requirement A 1 causes photoreceptor cell death in zebrafish disease models. Am. J. Pathol. 2018, 188, 2729–2744. [Google Scholar] [CrossRef] [PubMed]
- Beguier, F.; Housset, M.; Roubeix, C.; Augustin, S.; Zagar, Y.; Nous, C.; Mathis, T.; Eandi, C.; Benchaboune, M.; Drame-Maigné, A.; et al. The 10q26 risk haplotype of age-related macular degeneration aggravates subretinal inflammation by impairing monocyte elimination. Immunity 2020, 53, 429–441. [Google Scholar] [CrossRef]
- Coleman, H.R.; Chan, C.C.; Ferris, F.L., III; Chew, E.Y. Age-related macular degeneration. Lancet 2008, 372, 1835–1845. [Google Scholar] [CrossRef]
- Oka, C.; Tsujimoto, R.; Kajikawa, M.; Koshiba-Takeuchi, K.; Ina, J.; Yano, M.; Tsuchiya, A.; Ueta, Y.; Soma, A.; Kanda, H.; et al. HtrA1 serine protease inhibits signaling mediated by Tgfβ family proteins. Development 2004, 131, 1041–1053. [Google Scholar] [CrossRef]
- Shiga, A.; Nozaki, H.; Yokoseki, A.; Nihonmatsu, M.; Kawata, H.; Kato, T.; Koyama, A.; Arima, K.; Ikeda, M.; Katada, S.; et al. Cerebral small-vessel disease protein HTRA1 controls the amount of TGF-β1 via cleavage of proTGF-β1. Hum. Mol. Genet. 2011, 20, 1800–1810. [Google Scholar] [CrossRef]
- Zhang, L.; Lim, S.L.; Du, H.; Zhang, M.; Kozak, I.; Hannum, G.; Wang, X.; Ouyang, H.; Hughes, G.; Zhao, L.; et al. High temperature requirement factor A1 (HTRA1) gene regulates angiogenesis through transforming growth factor-β family member growth differentiation factor 6. J. Biol. Chem. 2012, 287, 1520–1526. [Google Scholar] [CrossRef] [PubMed]
- Graham, J.R.; Chamberl, A.; Lin, Q.; Li, X.J.; Dai, D.; Zeng, W.; Ryan, M.S.; Rivera-Bermúdez, M.A.; Flannery, C.R.; Yang, Z. Serine protease HTRA1 antagonizes transforming growth factor-β signaling by cleaving its receptors and loss of HTRA1 in vivo enhances bone formation. PLoS ONE 2013, 8, e74094. [Google Scholar] [CrossRef] [PubMed]
- Hirota, S.; Clements, T.P.; Tang, L.K.; Morales, J.E.; Lee, H.S.; Oh, S.P.; Rivera, G.M.; Wagner, D.S.; McCarty, J.H. Neuropilin 1 balances β8 integrin-activated TGFβ signaling to control sprouting angiogenesis in the brain. Development 2015, 142, 4363–4373. [Google Scholar] [CrossRef] [PubMed]
- Santibañez, J.F.; Quintanilla, M.; Bernabeu, C. TGF-β/TGF-β receptor system and its role in physiological and pathological conditions. Clin. Sci. 2011, 121, 233–251. [Google Scholar] [CrossRef]
- Schmierer, B.; Hill, C.S. TGFβ-SMAD signal transduction: Molecular specificity and functional flexibility. Nat. Rev. Mol. Cell Biol. 2007, 8, 970–982. [Google Scholar] [CrossRef]
- Allinson, K.R.; Lee, H.S.; Fruttiger, M.; McCarty, J.; Arthur, H.M. Endothelial expression of TGFβ type II receptor is required to maintain vascular integrity during postnatal development of the central nervous system. PLoS ONE 2012, 7, e39336. [Google Scholar] [CrossRef]
- Connor, T.B.; Roberts, A.B.; Sporn, M.B.; Danielpour, D.; Dart, L.L.; Michels, R.G.; de Bustros, S.; Enger, C.; Kato, H.; Lansing, M. Correlation of fibrosis and trans-forming growth factor-β type 2 levels in the eye. J. Clin. Investig. 1989, 83, 1661–1666. [Google Scholar] [CrossRef]
- Tosi, G.M.; Neri, G.; Caldi, E.; Fusco, F.; Bacci, T.; Tarantello, A.; Nuti, E.; Marigliani, D.; Baiocchi, S.; Traversi, C.; et al. TGF-β concentrations and activity are down-regulated in the aqueous humor of patients with neovascular age-related macular degeneration. Sci. Rep. 2018, 8, 8053. [Google Scholar]
- McAuley, A.K.; Sanfilippo, P.G.; Hewitt, A.W.; Liang, H.; Lamoureux, E.; Wang, J.J.; Connell, P.P. Vitreous biomarkers in diabetic retinopathy: A systematic review and metaanalysis. J. Diabetes Complicat. 2014, 28, 419–425. [Google Scholar] [CrossRef]
- Tosi, G.M.; Caldi, E.; Neri, G.; Nuti, E.; Marigliani, D.; Baiocchi, S.; Traversi, C.; Cevenini, G.; Tarantello, A.; Fusco, F.; et al. HTRA1 and TGF-β1 concentrations in the aqueous humor of patients with neovascular age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2017, 58, 162–167. [Google Scholar] [CrossRef]
- Gerhardinger, C.; Dagher, Z.; Sebastiani, P.; Yong, S.P.; Lorenzi, M. The transforming growth factor-β pathway is a common target of drugs that prevent experimental diabetic retinopathy. Diabetes 2009, 58, 1659–1667. [Google Scholar] [CrossRef]
- Avramovic, D.; Archaimbault, S.A.; Kemble, A.M.; Gruener, S.; Lazendic, M.; Westenskow, P.D. TGFβ1 induces senescence and attenuated VEGF production in retinal pericytes. Biomedicines 2022, 10, 1404. [Google Scholar] [CrossRef]
- Kajdaniuk, D.; Marek, B.; Borgiel-Marek, H.; Kos-Kudła, B. Transforming growth factor β1 (TGFβ1) in physiology and pathology. Endokrynol. Pol. 2013, 64, 384–396. [Google Scholar] [CrossRef]
- Bai, Y.; Liang, S.; Yu, W.; Zhao, M.; Huang, L.; Zhao, M.; Li, X. Semaphorin 3A blocks the formation of pathologic choroidal neovascularization induced by transforming growth factor beta. Mol. Vis. 2014, 20, 1258–1270. [Google Scholar] [PubMed]
- The R Project for Statistical Computing. R Software Version 4.1.2. Available online: https://www.r-project.org/ (accessed on 1 July 2024).
- Hachana, S.; Larrivée, B. TGF-β superfamily signaling in the eye: Implications for ocular pathologies. Cells 2022, 11, 2336. [Google Scholar] [CrossRef] [PubMed]
- Hirase, K.; Ikeda, T.; Sotozono, C.; Nishida, K.; Sawa, H.; Kinoshita, S. Transforming growth factor β2 in the vitreous in proliferative diabetic retinopathy. Arch. Ophthalmol. 1998, 116, 738–741. [Google Scholar] [CrossRef]
- Dai, Y.; Wu, Z.; Wang, F.; Zhang, Z.; Yu, M. Identification of chemokines and growth factors in proliferative diabetic retinopathy vitreous. BioMed Res. Int. 2014, 486386. [Google Scholar] [CrossRef]
- Hirsch, L.; Nazari, H.; Sreekumar, P.G.; Kannan, R.; Dustin, L.; Zhu, D.; Barron, E.; Hinton, D.R. TGF-β2 secretion from RPE decreases with polarization and becomes apically oriented. Cytokine 2015, 71, 394–396. [Google Scholar] [CrossRef]
- Braunger, B.M.; Leimbeck, S.V.; Schlecht, A.; Volz, C.; Jägle, H.; Tamm, E.R. Deletion of ocular transforming growth factor β signaling mimics essential character-istics of diabetic retinopathy. Am. J. Pathol. 2015, 185, 1749–1768. [Google Scholar] [CrossRef]
- Walshe, T.E.; Saint-Geniez, M.; Maharaj, A.S.R.; Sekiyama, E.; Maldonado, A.E.; D’Amore, P.A. TGF-β is required for vascular barrier function, endothelial survival and homeostasis of the adult microvasculature. PLoS ONE 2009, 4, e5149. [Google Scholar] [CrossRef] [PubMed]
- Kita, T.; Hata, Y.; Kano, K.; Miura, M.; Nakao, S.; Noda, Y.; Shimokawa, H.; Ishibashi, T. Transforming growth factor-β2 and connective tissue growth factor in proliferative vitreoretinal diseases: Possible involvement of hyalocytes and therapeutic potential of rho kinase inhibitor. Diabetes 2007, 56, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Kimoto, K.; Nakatsuka, K.; Matsuo, N.; Yoshioka, H. p38 MAPK mediates the expression of type I collagen induced by TGF-β2 in human retinal pigment epithelial cells ARPE-19. Investig. Ophthalmol. Vis. Sci. 2004, 45, 2431–2437. [Google Scholar] [CrossRef] [PubMed]
- Kita, T.; Hata, Y.; Arita, R.; Kawahara, S.; Miura, M.; Nakao, S.; Mochizuki, Y.; Enaida, H.; Goto, Y.; Shimokawa, H.; et al. Role of TGF-beta in proliferative vitreoretinal diseases and ROCK as a therapeutic target. Proc. Natl. Acad. Sci. USA 2008, 105, 17504–17509. [Google Scholar] [CrossRef] [PubMed]
- Hoerster, R.; Muether, P.S.; Vierkotten, S.; Hermann, M.M.; Kirchhof, B.; Fauser, S. Upregulation of TGF-β1 in experimental proliferative vitreoretinopathy is accompanied by epithelial to mesenchymal transition. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 252, 11–16. [Google Scholar] [CrossRef]


| Characteristics | Control (n = 6) | Chorioretinal Vascular Disease (n = 7) | p Value |
|---|---|---|---|
| Male Gender no. (%) | 4 (66.67%) | 4 (57.14%) | 0.93 |
| Age (years); mean ± SD 1 | 67.17 ± 2.79 | 71.57 ± 10.91 | 0.40 |
| Disease Duration (mo); mean ± SD 1 | 11.50 ± 14.56 | 8.43 ± 10.91 | 0.70 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukushima, Y.; Takahashi, S.; Nakamura, M.; Inoue, T.; Fujieda, Y.; Sato, T.; Noguchi, S.; Tsujikawa, M.; Sakaguchi, H.; Nishida, K. An Association between HTRA1 and TGF-β2 in the Vitreous Humor of Patients with Chorioretinal Vascular Diseases. J. Clin. Med. 2024, 13, 5073. https://doi.org/10.3390/jcm13175073
Fukushima Y, Takahashi S, Nakamura M, Inoue T, Fujieda Y, Sato T, Noguchi S, Tsujikawa M, Sakaguchi H, Nishida K. An Association between HTRA1 and TGF-β2 in the Vitreous Humor of Patients with Chorioretinal Vascular Diseases. Journal of Clinical Medicine. 2024; 13(17):5073. https://doi.org/10.3390/jcm13175073
Chicago/Turabian StyleFukushima, Yoko, Shizuka Takahashi, Machiko Nakamura, Tatsuya Inoue, Yusuke Fujieda, Toshiyuki Sato, Shingo Noguchi, Motokazu Tsujikawa, Hirokazu Sakaguchi, and Kohji Nishida. 2024. "An Association between HTRA1 and TGF-β2 in the Vitreous Humor of Patients with Chorioretinal Vascular Diseases" Journal of Clinical Medicine 13, no. 17: 5073. https://doi.org/10.3390/jcm13175073
APA StyleFukushima, Y., Takahashi, S., Nakamura, M., Inoue, T., Fujieda, Y., Sato, T., Noguchi, S., Tsujikawa, M., Sakaguchi, H., & Nishida, K. (2024). An Association between HTRA1 and TGF-β2 in the Vitreous Humor of Patients with Chorioretinal Vascular Diseases. Journal of Clinical Medicine, 13(17), 5073. https://doi.org/10.3390/jcm13175073






