Effects of Small-Sided Soccer Games on Physical Fitness and Cardiometabolic Health Biomarkers in Untrained Children and Adolescents: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Outcome and Prioritization
2.3. Literature Search Strategy
2.4. Study Selection
2.5. Data Extraction
2.6. Assessment of Risk of Bias
2.7. Statistical Analysis
3. Results
3.1. Study Selection
3.2. Study Characteristics and Participants
3.3. Small-Sided Soccer Games and Co-Intervention Characteristics
3.4. Outcome Measures
| Author | Design | Participants | Intervention | Main Changes on Cardiometabolic Risk and Physical Fitness in SSSG (% Change) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Age (Gender) | Nutrit. Status | w | Group (n) | d/w | Session (min) | Training Characteristics | Drop Out (%) | Adh (%) | |||
| Carrasco et al., 2015 Chile [46] | CT | 55 | 15.6 ± 0.7 (M) | OW-O | 11 | SSSG (NI) | 2 | 75 | SSSG F: 3 vs. 3; App: 50 m2; P-s: 20 × 15 m; S: 2; D-s: 15; W-d: 35 min; rest 5 min. | NI | 90 | %FM: ↓ 2.54 *; BMI: ↓ 0.61 *; VO2max.: ↑ 8.58 * |
| CG (NI) | The normal level of physical activity | NI | 95 | |||||||||
| Cvetković et al., 2018 Serbia [34] | RCT | 42 | 11 to 13 (M) | OW-O | 12 | SSSG (10) | 3 | 60 | SSSG F: 5–7 a side; App: 80 m2; S: 4; D-s: 8 min; W-d: 32 min; Rest: 2 min; W-i: 75.1 ± 2.3% HRmax | 28,57 | >50 | %FM: ↓ 7.67; LM: ↑ 2.61; BMI: ↓ 3.07; BM: ↓ 1.39; SBP: ↓ 2.89; DBP: ↓ 8.57; RHR: ↓ 10.20; CMJ: ↑ 17.02; YYIET1: ↑ 79.83 * |
| HIIT (11) | 3 | 60 | HIIT; S: 3; Reps: 5–8–10; W-i: 100% MAS; rest: 3 min; W-i: 80.0 ± 3.0% HRmax | 21,43 | >50 | |||||||
| CG (14) | The normal level of physical activity | 0 | ||||||||||
| Faude et al., 2010 Germany [35] | RCT | 39 | 8 to 12 (M) | OW-O | 24 | SSSG (11) | 3 | 60 | SSSG (50%) + technique (20%) + fitness courses with the ball | 57,89 | >50 | BM: ↑ 5.78 *; BMI: ↑ 1.86 *CMJ: ↑ 15.38 *; VO2max.: ↓ 6.72 |
| STD (11) | 3 | 60 | Aerobic endurance (40%) + coordination/flexibility (20%) + strength (15%) + speed (15%) | 55 | >50 | |||||||
| Hammami et al., 2017 Tunisia [36] | RCT | 22 | 15.9 ± 0.6 (M) | N | 8 | SSSG (10) | 2 | 30–45 | SSSG F: 4–7 a side; P-s: 20 × 25 to 50 × 30 m. | 9.09 | NI | SBP: ↑ 1.3; DBP: ↓ 2.9; HRR: ↓ 6.5; HJ: ↑ 3.8; YYIRT1: ↑ 30.92 * |
| CG (10) | The normal level of physical activity | 9.09 | NI | |||||||||
| Hansen et al., 2013 Portugal [47] | CT | 31 | 8 to 12 (MF) | OW-O | 12 | SSSG (20) | 4 | 45–90 | SSSG + technical exercise; W-i: >90% HRmax; W-d: 40–60 min | 0 | NI | BM: ↑ 0.39; BMI: ↓ −0.87SBP: ↓ 1.75 *; DBP: ↑ 1.61; RHR: ↓ 4.48 |
| CG (11) | Normal level of physical activity | 0 | NI | |||||||||
| Krustrup et al., 2014 Denmark [39] | RCT | 97 | 9 to 10 (MF) | N-OW | 10 | SSSG (46) | 3 | 40 | SSSG F; 3 vs. 3; W-d: 30 min; W-i: 71 ± 28% HRmax, time >80% HRmax = 24 ± 13%. | 0 | 77 ± 18 | BM: ↑ 1.56; BMI: ↓ −0.59SBP: ↓ 0.89; DBP: ↓ 1.34; RHR: ↓ −0.71 |
| CG (51) | Normal level of physical activity | 0 | ||||||||||
| Larsen et al., 2018 Denmark [40] | cRCT | 291 | 8 to 10 (MF) | N-OW | 40 | SSSG (93) | 3 | 40 | SSSG F: 3 vs. 3; P-s: 20 × 13m | NI | NI | BM: ↑ 8.26; SBP: ↓ 1.34; DBP: ↓ 3.13; RHR: ↓ 2.36; MAP: ↓ 2.38; YYIR1C: ↑ 19.76 |
| CST (83) | 3 | 40 | Circuit training; S: 6–10; D-s: 30 s; rest: 45 s. | NI | NI | |||||||
| CG (115) | 3 | 40 | Normal level of physical activity | NI | NI | |||||||
| Ørntoft et al., 2016 Denmark [41] | cRCT | 546 | 10 to 12 (MF) | N-OW | 11 | SSSG (386) | 2 | 45 | SSSG + football skill; SSG F: 3 vs. 3. | 3.99 | NI | BM: ↑ 2.18 *; BMI: ↓ 0.11; LM: ↑ 4.17 *; %FM: ↓ 3.72 *; SBP: ↓ 2.75 * DBP: ↓ 3.43 *; MAP: ↓ 2.53; RHR: ↓ 1.39YYIR1C: ↑ 5.16 *; HJ ↓ 0.85 |
| CG (140) | Normal level of physical activity | 2.77 | NI | |||||||||
| Seabra et al., 2014 Portugal [48] | CT | 20 | 8 to 12 (M) | OW-O | 20 | SSSG (12) | 2 | 60–90 | SSSG + technical exercise: W-d: 40–60 min; W-i: >80% HRmax | 0 | >85 | BM: ↑ 5.37; BMI: ↑ 1.31; %FM: ↓ 2.39; LM: ↑ 5.0 |
| CG (8) | Normal level of physical activity | 0 | >85 | |||||||||
| Seabra et al., 2016 Portugal [49] | CT | 90 | 8 to 12 (M) | O | 24 | SSSG (29) | 3 | 60–90 | SSSG + technical exercise: W-d: 40–60 min; W-i: 78% HRmax | 3.33 | >85 | BM: ↓ 0.76; BMI: ↓ 0.84; WC: ↓ 5.02 *; %FM: ↓ 6.41 *; ↑ LM: 8.38 *; FBG: ↑ 3.47; HDL: ↑ 7.65 *; LDL: ↓ 12.85 *; TG: ↓ 22.57 *; TC: ↓ 6.99 *; SBP: ↑ 0.36; DBP: ↓ 6.77; VO2max.: ↑ 12.75 * |
| AG (29) | 3 | 60–90 | Multicomponent training: aerobic endurance, coordination, balance, flexibility, and strength; W-d: 40–60 min; W-i: 75% HRmax. | 3.33 | >85 | |||||||
| CG (30) | Normal level of physical activity | 0 | ||||||||||
| Skoradal et al., 2018 Faroe Islands [42] | cRCT | 392 | 10 to 12 (MF) | N-OW | 11 | SSSG (229) | 2 | 45 | SSSG F: 3 vs. 3–4 vs. 4. | NI | NI | BM: ↑ 4.52 *; BMI: ↑ 2.07 *; %FM: ↓ 2.60 *; LM: ↑ 5.02 *; SBP: ↓ 3.06 *; DBP: ↑ 1.59 *; RHR: ↓ 1.32; YYIR1C: ↑ 18 *; HJ: ↑ 4.59. |
| CG (100) | Normal level of physical activity | NI | NI | |||||||||
| Trajković et al., 2020 Serbia [43] | RCT | 152 | 14 to 17 (MF) | N-OW | 32 | SSSG (54) | 2 | 45 | SSSG F: 3 vs. 3, 4 vs. 4; App: 40–70 m2; S: 4; D-s: 5 min; W-d: 32 min; Rest: 3 min; W-i: 85–99% HRpeak. | 20 | >85 | BM: ↓ 1.81; BMI: ↓ 3.81; YYIRT1: ↑ 2.22 *; VJ: ↑ 3.39 *. |
| CG (51) | Normal level of physical activity | 30 | >85 | |||||||||
| Vasconcellos et al., 2016 Brazil [37] | RCT | 42 | 12 to 17 (MF) | O | 12 | SSSG (10) | 3 | 60 | SSSG F: 2–4 a side; W-d: 40 min; W-i: 84.5 ± 4.1% HRmax. | 37.5 | NI | BM: ↓ 5.35 *; BMI: ↓ 2.25 *; WC: ↓ 8.31 *; %FM: ↓ 5.35 *; LM: ↑ 4.16; FBG: ↓ 1.08; HDL: ↑ 32.74 *; LDL: ↓ 0.20; TG: ↓ 17.31 *; TC: ↓ 9.74 *; SBP: ↓ 3.91 *; DBP: ↓ 2.47; VO2 peak: ↑ 31.35 *. |
| CG (10) | Normal level of physical activity | 37.5 | NI | |||||||||
| Vasconcellos et al., 2020 Brazil [38] | RCT | 13 | 13 to 17 (MF) | O/MetS | 12 | SSSG (6) | 3 | 60 | SSSG F: 2–4 a side; W-d: 40 min | 0 | 100 | BM: ↓ 5.05; BMI: ↓ 0.33; WC: ↓ 11.79; %FM: ↓ 8.04; FBG: ↓ 18.51; HDL: ↑ 49.68 *; TG: ↓ 20.06 *; SBP: ↓ 5.19; DBP: ↓ 3.45 |
| CG (7) | Normal level of physical activity | 0 | 100 | |||||||||
| Ryom et al., 2022 Denmark [45] | cRCT | 1122 | 11 to 12 (MF) | N-OW | 11 | SSSG-PA (644) | 2 | 45 | SSSG + football skill; SSG F: 3 vs. 3. | NI | NI | YYIR1C: ↑ 16.09; BM: ↑ 1.91; BMI: ↓ −0.65; %FM: ↓ −3.07; DBP: ↓ −2.31; SBP:↑ 0.36; RHR: ↓ −0.75 |
| SSSG-NPA(300) | 2 | 45 | SSSG + football skill; SSG F: 3 vs. 3. | NI | NI | YYIR1C: ↑ 23.36; BM: ↑ 2.19; BMI: ↓ −0.15; %FM: ↓ −2.49; DBP: ↓ −3.05; SBP: ↑ 0.87; RHR: ↓ −2.03 | ||||||
| CG-PA(122) | Normal level of physical activity | NI | NI | |||||||||
| CG-NPA(56) | Normal level of physical activity | NI | NI | |||||||||
| Larsen et al., 2023 Denmark [44] | cRCT | 127 | 10 to 12 (MF) | N-OW | 11 | SSSG (61) | 2 | 45 | SSSG + football skill; SSG F: 3 vs. 3. | NI | NI | LM: ↑ 3.96; %FM: ↓ −1.72; HJ: ↑ 2.39 |
| CG (47) | Normal level of physical activity | NI | NI | |||||||||
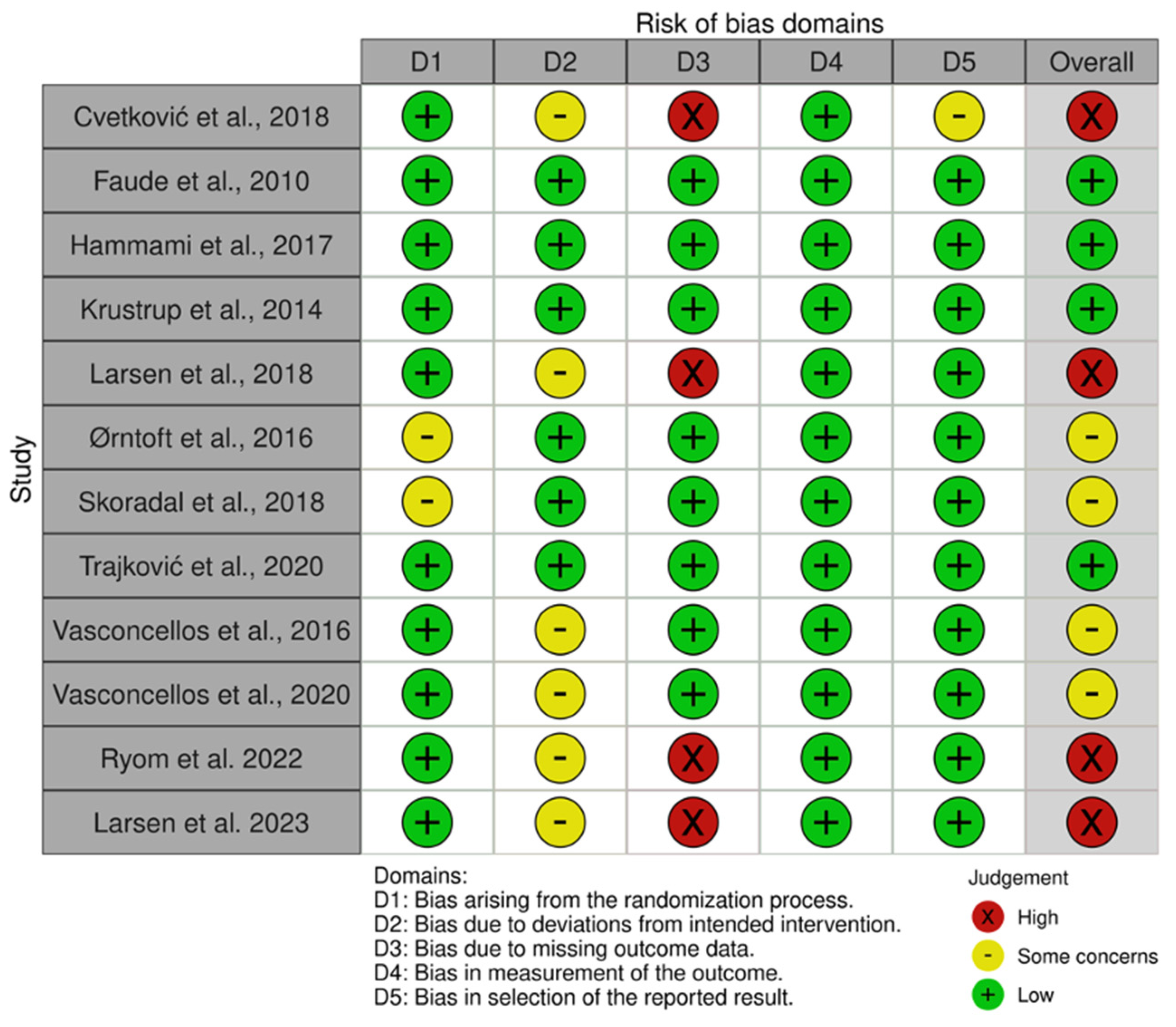
3.5. Risk of Bias within Studies
3.6. Summary of Results
| Outcome | Variables | k | Individual Significant Findings | |
|---|---|---|---|---|
| SSSG vs. CG | SSSG vs. Other Interventions | |||
| Physical fitness | Muscle strength | 1 | - | ↔ Cvetkovic et al. [34] |
| Anthropometric and body composition | Waist circumference | 1 | - | ↔ Seabra et al. [49] a |
| Body fat (%) | 2 | - | ↔ Seabra et al. [49] a ↔ Cvetkovic et al. [34] | |
| Lean mass (kg) | 2 | - | ↔ Seabra et al. [49] a ↔ Cvetkovic et al. [34] | |
| Cardiometabolic and inflammatory Variables | Total cholesterol | 2 | ↓ Seabra et al. [49] a ↓Vasconcellos et al. [37] a | ↔ Seabra et al. [49] a |
| LDL-C | 2 | ↔ Seabra et al. [49] a ↔ Vasconcellos et al. [37] | ↔ Seabra et al. [49] a | |
| HDL-C | 1 | - | ↔ Seabra et al. [49] | |
| TG | 1 | - | ↔ Seabra et al. [49] a | |
| HOMA-IR | 2 | ↓ Vasconcellos et al. [37] a ↔ Seabra et al. [49] | ↔ Seabra et al. [49] | |
| Fasting insulin | 2 | ↔ Seabra et al. [49] ↔ Vasconcellos et al. [37] | ↔ Seabra et al. [49] | |
| CRP | 2 | ↔ Seabra et al. [49] a ↔ Vasconcellos et al. [37] a | ↔ Seabra et al. [49] a | |
| Leptin | 2 | ↔ Seabra et al. [49] a ↔ Vasconcellos et al. [37] | ↔ Seabra et al. [49] a | |
| Adiponectin | 2 | ↔ Seabra et al. [49] a ↔ Vasconcellos et al. [37] | ↔ Seabra et al. [49] a | |
| IL-6 | 1 | ↔ Vasconcellos et al. [37] | ||
| Resistin | 2 | ↔ Seabra et al. [49] a ↔ Vasconcellos et al. [37] | ↔ Seabra et al. [49] a | |
| TNF-α | 1 | ↔ Vasconcellos et al. [37] a | ||
3.7. Subgroup Analyses
3.8. Publication Bias and Sensitivity Analysis
4. Discussion
Limitations and Practical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed]
- Allen, N.B.; Krefman, A.E.; Labarthe, D.; Greenland, P.; Juonala, M.; Kahonen, M.; Lehtimaki, T.; Day, R.S.; Bazzano, L.A.; Van Horn, L.V.; et al. Cardiovascular Health Trajectories from Childhood Through Middle Age and Their Association with Subclinical Atherosclerosis. JAMA Cardiol. 2020, 5, 557–566. [Google Scholar] [CrossRef]
- Umer, A.; Kelley, G.A.; Cottrell, L.E.; Giacobbi, P., Jr.; Innes, K.E.; Lilly, C.L. Childhood obesity and adult cardiovascular disease risk factors: A systematic review with meta-analysis. BMC Public Health 2017, 17, 683. [Google Scholar] [CrossRef] [PubMed]
- Di Cesare, M.; Soric, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Reinehr, T. Metabolic Syndrome in Children and Adolescents: A Critical Approach Considering the Interaction between Pubertal Stage and Insulin Resistance. Curr. Diab. Rep. 2016, 16, 8. [Google Scholar] [CrossRef]
- Boren, J.; Taskinen, M.R.; Bjornson, E.; Packard, C.J. Metabolism of triglyceride-rich lipoproteins in health and dyslipidaemia. Nat. Rev. Cardiol. 2022, 19, 577–592. [Google Scholar] [CrossRef]
- Koenen, M.; Hill, M.A.; Cohen, P.; Sowers, J.R. Obesity, Adipose Tissue and Vascular Dysfunction. Circ. Res. 2021, 128, 951–968. [Google Scholar] [CrossRef] [PubMed]
- Leopold, S.; Zachariah, J.P. Pediatric Obesity, Hypertension, Lipids. Curr. Treat. Options Pediatr. 2020, 6, 62–77. [Google Scholar] [CrossRef]
- Friend, A.; Craig, L.; Turner, S. The prevalence of metabolic syndrome in children: A systematic review of the literature. Metab. Syndr. Relat. Disord. 2013, 11, 71–80. [Google Scholar] [CrossRef]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef]
- Li, S.; Chen, W.; Srinivasan, S.R.; Bond, M.G.; Tang, R.; Urbina, E.M.; Berenson, G.S. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: The Bogalusa Heart Study. JAMA 2003, 290, 2271–2276. [Google Scholar] [CrossRef] [PubMed]
- Kelley, G.A.; Kelley, K.S.; Pate, R.R. Exercise and adiposity in overweight and obese children and adolescents: A systematic review with network meta-analysis of randomised trials. BMJ Open 2019, 9, e031220. [Google Scholar] [CrossRef]
- Kelley, G.A.; Kelley, K.S.; Pate, R.R. Exercise and Cardiovascular Disease Risk Factors in Children and Adolescents with Obesity: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. Am. J. Lifestyle Med. 2021, 16, 485–501. [Google Scholar] [CrossRef]
- Garcia-Hermoso, A.; Ramirez-Velez, R.; Saavedra, J.M. Exercise, health outcomes, and paediatric obesity: A systematic review of meta-analyses. J. Sci. Med. Sport 2019, 22, 76–84. [Google Scholar] [CrossRef]
- Clemente, F.M.; Ramirez-Campillo, R.; Sarmento, H. Effects of the Small-Sided Soccer Games on Blood Pressure in Untrained Hypertensive Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Healthcare 2021, 9, 345. [Google Scholar] [CrossRef]
- Sarmento, H.; Manuel Clemente, F.; Marques, A.; Milanovic, Z.; David Harper, L.; Figueiredo, A. Recreational football is medicine against non-communicable diseases: A systematic review. Scand. J. Med. Sci. Sports 2020, 30, 618–637. [Google Scholar] [CrossRef]
- Krustrup, P.; Krustrup, B.R. Football is medicine: It is time for patients to play! Br. J. Sports Med. 2018, 52, 1412–1414. [Google Scholar] [CrossRef]
- Hammami, A.; Chamari, K.; Slimani, M.; Shephard, R.J.; Yousfi, N.; Tabka, Z.; Bouhlel, E. Effects of recreational soccer on physical fitness and health indices in sedentary healthy and unhealthy subjects. Biol. Sport 2016, 33, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Clemente, F.M.; Moran, J.; Ramirez-Campillo, R.; Oliveira, R.; Brito, J.; Silva, A.F.; Badicu, G.; Praca, G.; Sarmento, H. Recreational Soccer Training Effects on Pediatric Populations Physical Fitness and Health: A Systematic Review. Children 2022, 9, 1776. [Google Scholar] [CrossRef]
- Clemente, F.M.; Afonso, J.; Sarmento, H. Small-sided games: An umbrella review of systematic reviews and meta-analyses. PLoS ONE 2021, 16, e0247067. [Google Scholar] [CrossRef]
- Selmi, O.; Ouergui, I.; Levitt, D.E.; Nikolaidis, P.T.; Knechtle, B.; Bouassida, A. Small-Sided Games are More Enjoyable Than High-Intensity Interval Training of Similar Exercise Intensity in Soccer. Open Access J. Sports Med. 2020, 11, 77–84. [Google Scholar] [CrossRef]
- Zouhal, H.; Hammami, A.; Tijani, J.M.; Jayavel, A.; de Sousa, M.; Krustrup, P.; Sghaeir, Z.; Granacher, U.; Ben Abderrahman, A. Effects of Small-Sided Soccer Games on Physical Fitness, Physiological Responses, and Health Indices in Untrained Individuals and Clinical Populations: A Systematic Review. Sports Med. 2020, 50, 987–1007. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2020, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, G.C.J.; Rücker, G. Meta-Analysis with R, 1st ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2015. [Google Scholar]
- Harrer, M.; Cuijpers, P.; Furukawa, T.A.; Ebert, D.D. Doing Meta-Analysis with R: A Hands-On Guide, 1st ed.; Chapman & Hall/CRC Press: Boca Raton, FL, USA; London, UK, 2021. [Google Scholar]
- Jackson, D.; White, I.R.; Thompson, S.G. Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat. Med. 2010, 29, 1282–1297. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Viechtbauer, W.; Cheung, M.W. Outlier and influence diagnostics for meta-analysis. Res. Synth. Methods 2010, 1, 112–125. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Cvetkovic, N.; Stojanovic, E.; Stojiljkovic, N.; Nikolic, D.; Scanlan, A.T.; Milanovic, Z. Exercise training in overweight and obese children: Recreational football and high-intensity interval training provide similar benefits to physical fitness. Scand. J. Med. Sci. Sports 2018, 28 (Suppl. S1), 18–32. [Google Scholar] [CrossRef] [PubMed]
- Faude, O.; Kerper, O.; Multhaupt, M.; Winter, C.; Beziel, K.; Junge, A.; Meyer, T. Football to tackle overweight in children. Scand. J. Med. Sci. Sports 2010, 20 (Suppl. S1), 103–110. [Google Scholar] [CrossRef]
- Hammami, A.; Kasmi, S.; Razgallah, M.; Tabka, Z.; Shephard, R.J.; Bouhlel, E. Recreational soccer training improves heart-rate variability indices and physical performance in untrained healthy adolescent. Sport Sci. Health 2017, 13, 507–514. [Google Scholar] [CrossRef]
- Vasconcellos, F.; Seabra, A.; Cunha, F.; Montenegro, R.; Penha, J.; Bouskela, E.; Nogueira Neto, J.F.; Collett-Solberg, P.; Farinatti, P. Health markers in obese adolescents improved by a 12-week recreational soccer program: A randomised controlled trial. J. Sports Sci. 2016, 34, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Vasconcellos, F.; Cunha, F.A.; Gonet, D.T.; Farinatti, P.T.V. Does Recreational Soccer Change Metabolic Syndrome Status in Obese Adolescents? A Pilot Study. Res. Q. Exerc. Sport 2021, 92, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Krustrup, P.; Hansen, P.R.; Nielsen, C.M.; Larsen, M.N.; Randers, M.B.; Manniche, V.; Hansen, L.; Dvorak, J.; Bangsbo, J. Structural and functional cardiac adaptations to a 10-week school-based football intervention for 9-10-year-old children. Scand. J. Med. Sci. Sports 2014, 24 (Suppl. S1), 4–9. [Google Scholar] [CrossRef]
- Larsen, M.N.; Nielsen, C.M.; Madsen, M.; Manniche, V.; Hansen, L.; Bangsbo, J.; Krustrup, P.; Hansen, P.R. Cardiovascular adaptations after 10 months of intense school-based physical training for 8- to 10-year-old children. Scand. J. Med. Sci. Sports 2018, 28 (Suppl. S1), 33–41. [Google Scholar] [CrossRef]
- Ørntoft, C.; Fuller, C.W.; Larsen, M.N.; Bangsbo, J.; Dvorak, J.; Krustrup, P. ‘FIFA 11 for Health’ for Europe. II: Effect on health markers and physical fitness in Danish schoolchildren aged 10–12 years. Br. J. Sports Med. 2016, 50, 1394–1399. [Google Scholar] [CrossRef]
- Skoradal, M.B.; Purkhus, E.; Steinholm, H.; Olsen, M.H.; Orntoft, C.; Larsen, M.N.; Dvorak, J.; Mohr, M.; Krustrup, P. “FIFA 11 for Health” for Europe in the Faroe Islands: Effects on health markers and physical fitness in 10- to 12-year-old schoolchildren. Scand. J. Med. Sci. Sports 2018, 28 (Suppl. S1), 8–17. [Google Scholar] [CrossRef]
- Trajkovic, N.; Madic, D.M.; Milanovic, Z.; Macak, D.; Padulo, J.; Krustrup, P.; Chamari, K. Eight months of school-based soccer improves physical fitness and reduces aggression in high-school children. Biol. Sport 2020, 37, 185–193. [Google Scholar] [CrossRef]
- Larsen, M.N.; Terracciano, A.; Moller, T.K.; Aggestrup, C.S.; Buono, P.; Krustrup, P.; Castagna, C. An 11-week school-based “health education through football” programme improves musculoskeletal variables in 10-12-yr-old Danish school children. Bone Rep. 2023, 18, 101681. [Google Scholar] [CrossRef] [PubMed]
- Ryom, K.; Christiansen, S.R.; Elbe, A.M.; Aggestrup, C.S.; Madsen, E.E.; Madsen, M.; Larsen, M.N.; Krustrup, P. The Danish “11 for Health” program raises health knowledge, well-being, and fitness in ethnic minority 10- to 12-year-olds. Scand. J. Med. Sci. Sports 2022, 32, 138–151. [Google Scholar] [CrossRef]
- Carrasco Beltran, H.; Reigal Garrido, R.E.; Ulloa Diaz, D.; Chirosa Rios, I.J.; Chirosa Rios, L.J. Effects of small-sided exercises on body composition and maximal oxygen uptake in adolescents. Rev. Med. Chil. 2015, 143, 744–750. [Google Scholar] [CrossRef]
- Hansen, P.R.; Andersen, L.J.; Rebelo, A.N.; Brito, J.; Hornstrup, T.; Schmidt, J.F.; Jackman, S.R.; Mota, J.; Rego, C.; Oliveira, J.; et al. Cardiovascular effects of 3 months of football training in overweight children examined by comprehensive echocardiography: A pilot study. J. Sports Sci. 2013, 31, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Seabra, A.C.; Seabra, A.F.; Brito, J.; Krustrup, P.; Hansen, P.R.; Mota, J.; Rebelo, A.; Rego, C.; Malina, R.M. Effects of a 5-month football program on perceived psychological status and body composition of overweight boys. Scand. J. Med. Sci. Sports 2014, 24 (Suppl. S1), 10–16. [Google Scholar] [CrossRef] [PubMed]
- Seabra, A.; Katzmarzyk, P.; Carvalho, M.J.; Seabra, A.; Coelho, E.S.M.; Abreu, S.; Vale, S.; Povoas, S.; Nascimento, H.; Belo, L.; et al. Effects of 6-month soccer and traditional physical activity programmes on body composition, cardiometabolic risk factors, inflammatory, oxidative stress markers and cardiorespiratory fitness in obese boys. J. Sports Sci. 2016, 34, 1822–1829. [Google Scholar] [CrossRef] [PubMed]
- Milanovic, Z.; Pantelic, S.; Covic, N.; Sporis, G.; Krustrup, P. Is Recreational Soccer Effective for Improving VO2max A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 1339–1353. [Google Scholar] [CrossRef]
- Pozuelo-Carrascosa, D.P.; Garcia-Hermoso, A.; Alvarez-Bueno, C.; Sanchez-Lopez, M.; Martinez-Vizcaino, V. Effectiveness of school-based physical activity programmes on cardiorespiratory fitness in children: A meta-analysis of randomised controlled trials. Br. J. Sports Med. 2018, 52, 1234–1240. [Google Scholar] [CrossRef]
- Solera-Martinez, M.; Herraiz-Adillo, A.; Manzanares-Dominguez, I.; De La Cruz, L.L.; Martinez-Vizcaino, V.; Pozuelo-Carrascosa, D.P. High-Intensity Interval Training and Cardiometabolic Risk Factors in Children: A Meta-analysis. Pediatrics 2021, 148, e2021050810. [Google Scholar] [CrossRef]
- Cornelissen, V.A.; Smart, N.A. Exercise training for blood pressure: A systematic review and meta-analysis. J. Am. Heart Assoc. 2013, 2, e004473. [Google Scholar] [CrossRef]
- Minatto, G.; Barbosa Filho, V.C.; Berria, J.; Petroski, E.L. School-Based Interventions to Improve Cardiorespiratory Fitness in Adolescents: Systematic Review with Meta-analysis. Sports Med. 2016, 46, 1273–1292. [Google Scholar] [CrossRef]
- Martin-Smith, R.; Cox, A.; Buchan, D.S.; Baker, J.S.; Grace, F.; Sculthorpe, N. High Intensity Interval Training (HIIT) Improves Cardiorespiratory Fitness (CRF) in Healthy, Overweight and Obese Adolescents: A Systematic Review and Meta-Analysis of Controlled Studies. Int. J. Environ. Res. Public Health 2020, 17, 2955. [Google Scholar] [CrossRef]
- Thivel, D.; Masurier, J.; Baquet, G.; Timmons, B.W.; Pereira, B.; Berthoin, S.; Duclos, M.; Aucouturier, J. High-intensity interval training in overweight and obese children and adolescents: Systematic review and meta-analysis. J. Sports Med. Phys. Fit. 2019, 59, 310–324. [Google Scholar] [CrossRef]
- Cox, A.; Fairclough, S.J.; Kosteli, M.C.; Noonan, R.J. Efficacy of School-Based Interventions for Improving Muscular Fitness Outcomes in Adolescent Boys: A Systematic Review and Meta-analysis. Sports Med. 2020, 50, 543–560. [Google Scholar] [CrossRef]
- Armstrong, N.; Welsman, J. Sex-Specific Longitudinal Modeling of Youth Peak Oxygen Uptake. Pediatr. Exerc. Sci. 2019, 31, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Malina, R.M. Top 10 research questions related to growth and maturation of relevance to physical activity, performance, and fitness. Res. Q. Exerc. Sport 2014, 85, 157–173. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, M.M.; Zeitler, P.S. Insulin Resistance of Puberty. Curr. Diab. Rep. 2016, 16, 64. [Google Scholar] [CrossRef]
- Gralla, M.H.; McDonald, S.M.; Breneman, C.; Beets, M.W.; Moore, J.B. Associations of Objectively Measured Vigorous Physical Activity with Body Composition, Cardiorespiratory Fitness, and Cardiometabolic Health in Youth: A Review. Am. J. Lifestyle Med. 2019, 13, 61–97. [Google Scholar] [CrossRef]
- Slade, S.C.; Dionne, C.E.; Underwood, M.; Buchbinder, R.; Beck, B.; Bennell, K.; Brosseau, L.; Costa, L.; Cramp, F.; Cup, E.; et al. Consensus on Exercise Reporting Template (CERT): Modified Delphi Study. Phys. Ther. 2016, 96, 1514–1524. [Google Scholar] [CrossRef]
- Ring-Dimitriou, S.; Krustrup, P.; Coelho, E.S.M.J.; Mota, J.; Seabra, A.; Rego, C.; Mazur, A.; Vlachopapadopoulou, E.; Caroli, M.; Frelut, M.L.; et al. Could sport be part of pediatric obesity prevention and treatment? Expert conclusions from the 28th European Childhood Obesity Group Congress. J. Sport Health Sci. 2019, 8, 350–352. [Google Scholar] [CrossRef]


| SSSG vs. CG | SSSG vs. Other Interventions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| K (n) | MD/SMD [95% CI] | p-Value | I2% | Egger Test p-Value | K (n) | MD/SMD [95% CI] | p-Value | I2% | Egger Test p-Value | |
| PRIMARY OUTCOMES | ||||||||||
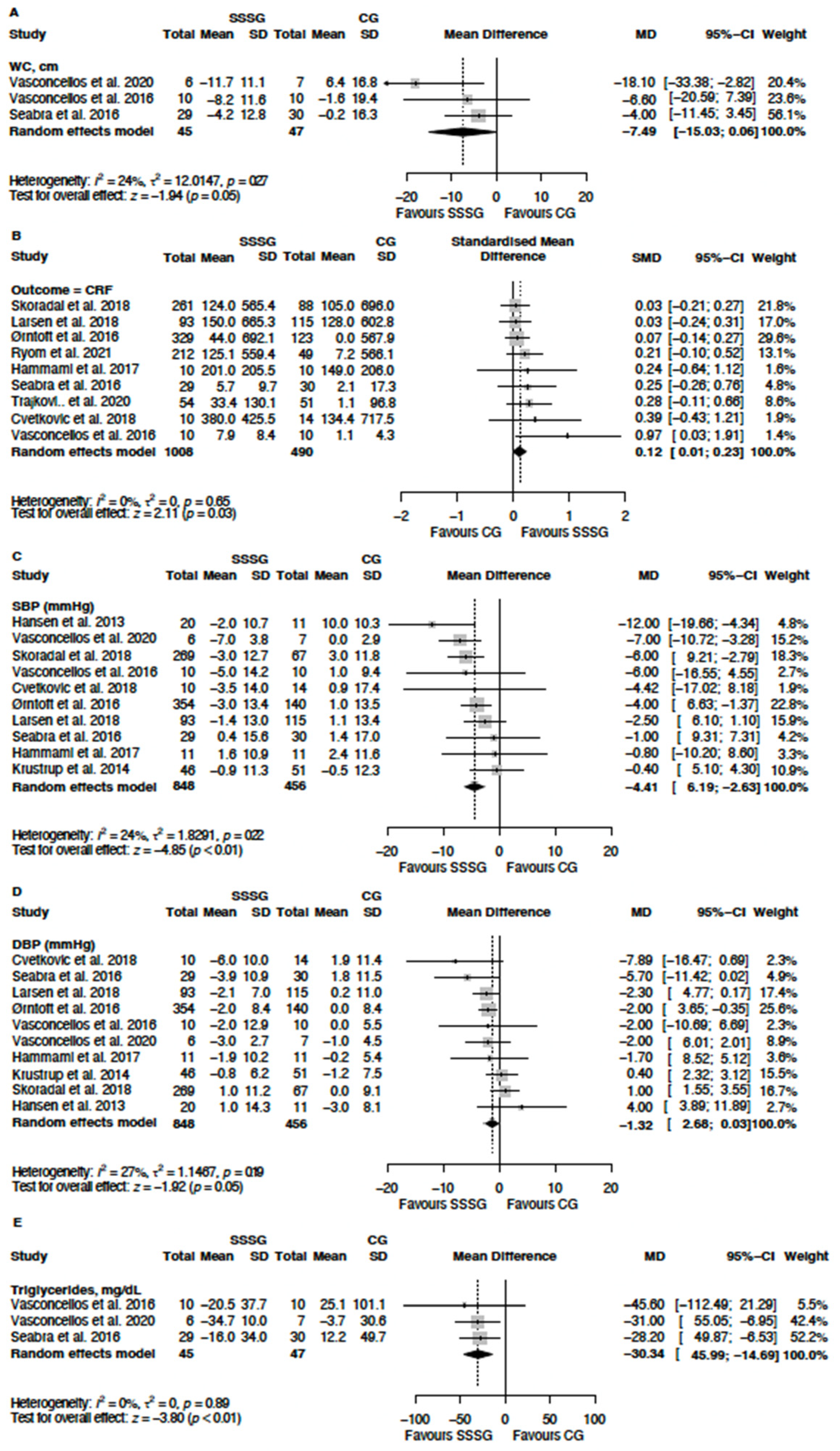
| WC, cm | 3 (45/47) | −7.49 a [−15.03; 0.06] | 0.05 | 24 | - | - | - | - | - | - |
| Cardiorespiratory fitness | 9 (108/490) | 0.12 b [0.01; 0.23] | 0.03 | 0 | - | 4 (143/134) | 0.04 [−0.20; 0.27] | 0.75 | 0 | - |
| SECONDARY OUTCOMES | ||||||||||
| Health-related Physical fitness | ||||||||||
| Muscle strength | 6 (725/333) | 0.17 b [−0.01; 0.34] | 0.06 | 28 | - | - | - | - | - | - |
| Cardiometabolic risk biomarkers | ||||||||||
| FBG, mg dL−1 | 3 (45/47) | −1.76 a [−8.73; 5.20] | 0.62 | 62 | - | - | - | - | - | - |
| TG, mg dL−1 | 3 (45/47) | −30.34 a [−45.99; −14.69] | <0.01 | 0 | - | - | - | - | - | - |
| HDL, mg dL−1 | 3 (45/47) | 4.42 a [−2.18; 11.03] | 0.19 | 0 | - | - | - | - | - | - |
| SBP, mmHg | 11 (1073/506) | −3.85 a [−5.75; −1.94] | <0.001 | 38.8 | 0.98 | 3 (132/123) | −3.35 [−6.81; 0.10] | 0.06 | 0 | - |
| DBP, mmHg | 11 (1073/506) | −1.26 a [−2.44; −0.08] | 0.04 | 19.6 | 0.72 | 3 (132/123) | 0.91 [−1.15; 2.97] | 0.39 | 0 | - |
| BMI, kg/m2 | 11 (1037/456) | −0.16 a [−0.63; 0.31] | 0.50 | 0 | 0.04 | 3 (50/51) | −0.23 [−2.51;2,01] a | 0.84 | 0 | - |
| Body mass, kg | 12 (1130/571) | −0.29 a [−1.53; 0.95] | 0.65 | 0 | 0.06 | 4 (143/134) | −0.59 [−3.31; 2.12] a | 0.67 | 0 | - |
| Fat Mass, % | 10 (728/318) | −0.10 b [−0.22; 0.01] | 0.08 | 0 | - | - | - | - | - | - |
| Lean Mass, kg | 7 (757/333) | 0.03 b [-0.10; 0.16] | 0.62 | 0 | - | - | - | - | - | - |
| RHR, bpm | 8 (1028/459) | −0.84 a [−2.81; 1.13] | 0.41 | 25.5 | - | - | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-Álvarez, N.; Boppre, G.; Hermosilla-Palma, F.; Reyes-Amigo, T.; Oliveira, J.; Fonseca, H. Effects of Small-Sided Soccer Games on Physical Fitness and Cardiometabolic Health Biomarkers in Untrained Children and Adolescents: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 5221. https://doi.org/10.3390/jcm13175221
Gómez-Álvarez N, Boppre G, Hermosilla-Palma F, Reyes-Amigo T, Oliveira J, Fonseca H. Effects of Small-Sided Soccer Games on Physical Fitness and Cardiometabolic Health Biomarkers in Untrained Children and Adolescents: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(17):5221. https://doi.org/10.3390/jcm13175221
Chicago/Turabian StyleGómez-Álvarez, Nicolás, Giorjines Boppre, Felipe Hermosilla-Palma, Tomás Reyes-Amigo, José Oliveira, and Hélder Fonseca. 2024. "Effects of Small-Sided Soccer Games on Physical Fitness and Cardiometabolic Health Biomarkers in Untrained Children and Adolescents: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 17: 5221. https://doi.org/10.3390/jcm13175221






