Association between Flexibility, Measured with the Back-Scratch Test, and the Odds of Oxytocin Administration during Labour and Caesarean Section
Abstract
1. Introduction
2. Materials and Methods
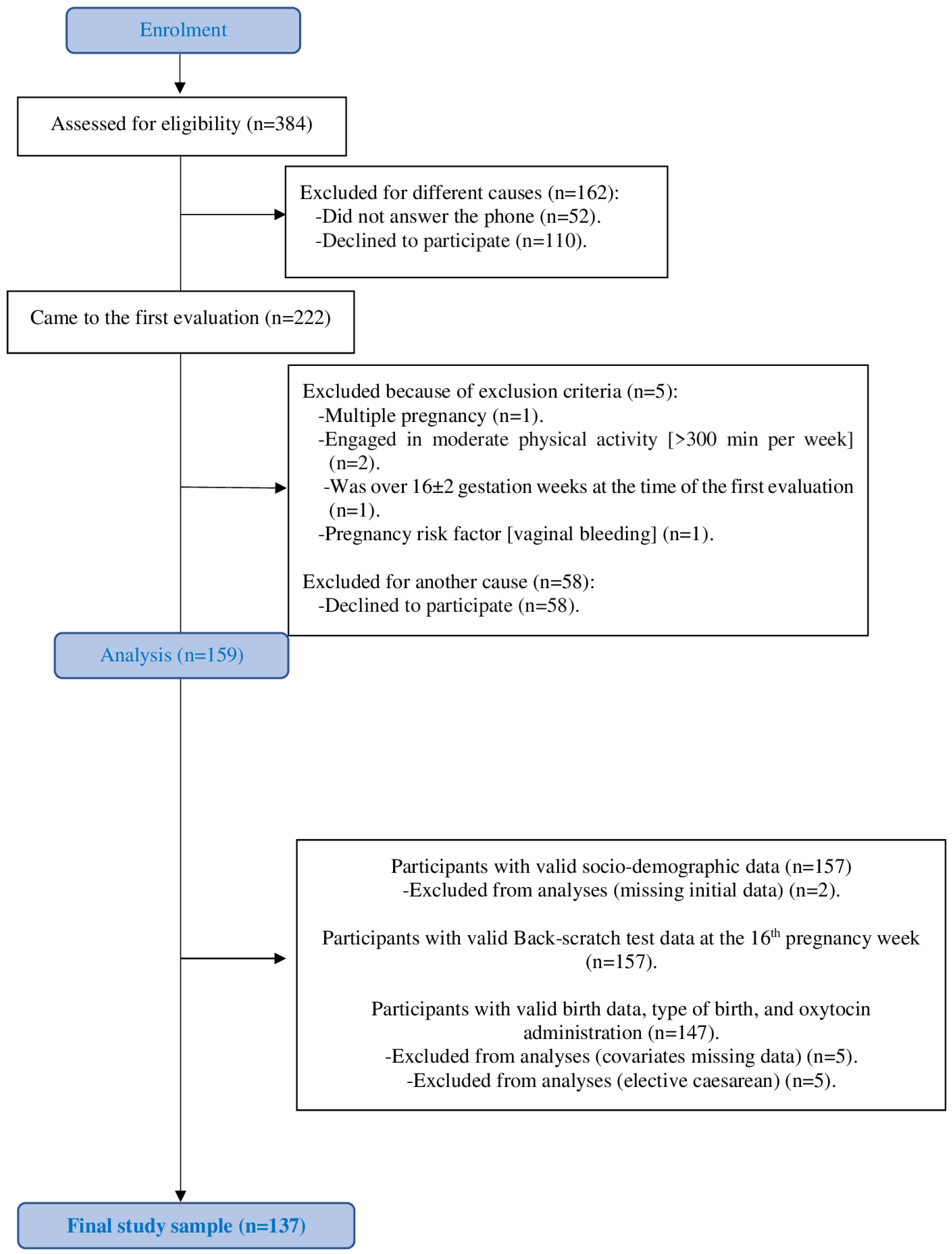
2.1. Study Sample and Design
2.2. Procedures
2.3. Maternal Sociodemographic and Clinical Data
2.4. Anthropometric Assessment
2.5. Pregnancy Health Document: Obstetric during Pregnancy and Pregnancy History
2.6. Labour Outcomes
Oxytocin Administration before or during Labour
2.7. The Back-Scratch Test
2.8. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boutsikou, T.; Malamitsi-Puchner, A. Caesarean section: Impact on mother and child. Acta Paediatr. 2011, 100, 1518–1522. [Google Scholar] [CrossRef] [PubMed]
- Oishi, A.; Tagashira, H.; Verho, A.; Holden, J.; Brimdyr, K.; Cadwell, K.; Widström, A.M.; Svensson, K.; Phillips, R. The effect of labor medications on normal newborn behavior in the first hour after birth: A prospective cohort study. BMJ Open 2019, 132, 30–36. [Google Scholar] [CrossRef]
- Hobbs, A.J.; Mannion, C.A.; McDonald, S.W.; Brockway, M.; Tough, S.C. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth 2016, 16, 90. [Google Scholar] [CrossRef]
- Olza Fernández, I.; Marín Gabriel, M.; Malalana Martínez, A.; Fernández-Cañadas Morillo, A.; López Sánchez, F.; Costarelli, V. Newborn feeding behaviour depressed by intrapartum oxytocin: A pilot study. Acta Paediatr. 2012, 101, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, A.; Burguet, A. Oxytocin administration during spontaneous labor: Guidelines for clinical practice. Chapter 5: Maternal risk and adverse effects of using oxytocin augmentation during spontaneous labor. J. Gynecol. Obstet. Hum. Reprod. 2017, 46, 509–521. [Google Scholar] [CrossRef]
- Burguet, A.; Rousseau, A. Oxytocin administration during spontaneous labor: Guidelines for clinical practice. Chapter 6: Fetal, neonatal and pediatric risks and adverse effects of using oxytocin augmentation during spontaneous labor. J. Gynecol. Obstet. Hum. Reprod. 2017, 46, 523–530. [Google Scholar] [CrossRef]
- Lothian, J.A. Healthy Birth Practice #4: Avoid Interventions Unless They Are Medically Necessary. J. Perinat. Educ. 2019, 28, 94–103. [Google Scholar] [CrossRef]
- Baena-García, L.; Marín-Jiménez, N. Association of Self-Reported Physical Fitness during Late Pregnancy with Birth Outcomes and Oxytocin Administration during Labour-The GESTAFIT Project. Int. J. Environ. Res. Public Health 2021, 18, 8201. [Google Scholar] [CrossRef]
- Baena-García, L.; Coll-Risco, I. Association of objectively measured physical fitness during pregnancy with maternal and neonatal outcomes. The GESTAFIT Project. PLoS ONE 2020, 15, e0229079. [Google Scholar] [CrossRef]
- Kongkaew, C.; Lertsinthai, P.; Jampachaisri, K.; Mongkhon, P.; Meesomperm, P.; Kornkaew, K.; Malaiwong, P. The Effects of Thai Yoga on Physical Fitness: A Meta-Analysis of Randomized Control Trials. J. Altern. Complement. Med. 2018, 24, 541–551. [Google Scholar] [CrossRef]
- Kawanishi, Y.; Hanley, S.J.; Tabata, K.; Nakagi, Y.; Ito, T.; Yoshioka, E.; Yoshida, T.; Saijo, Y. Effects of prenatal yoga: A systematic review of randomized controlled trials. Jpn. J. Public Health 2015, 62, 221–231. [Google Scholar] [CrossRef]
- Jahdi, F.; Sheikhan, F.; Haghani, H.; Sharifi, B.; Ghaseminejad, A.; Khodarahmian, M.; Rouhana, N. Yoga during pregnancy: The effects on labor pain and delivery outcomes (A randomized controlled trial). Complement. Ther. Clin. Pract. 2017, 27, 1–4. [Google Scholar] [CrossRef]
- Irving, G.; Neves, A.L.; Dambha-Miller, H. International variations in primary care physician consultation time: A systematic review of 67 countries. BMJ Open 2017, 7, e017902. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Manzano, P.; Segura-Jiménez, V.; Coll-Risco, I.; Borges-Cosic, M.; Castro-Piñero, J.; Delgado-Fernández, M.; Aparicio, V.A. Association of sedentary time and physical fitness with ideal cardiovascular health in perimenopausal women: The FLAMENCO project. Maturitas 2019, 120, 53–60. [Google Scholar] [CrossRef]
- Chang, K.V.; Hung, C.Y.; Li, C.M.; Lin, Y.H.; Wang, T.G.; Tsai, K.S.; Han, D.S. Reduced flexibility associated with metabolic syndrome in community-dwelling elders. PLoS ONE 2015, 10, e0117167. [Google Scholar] [CrossRef]
- Aparicio, V.A.; Segura-Jiménez, V.; Álvarez-Gallardo, I.C.; Soriano-Maldonado, A.; Castro-Piñero, J.; Delgado-Fernández, M.; Carbonell-Baeza, A. Fitness testing in the fibromyalgia diagnosis: The al-Ándalus project. Med. Sci. Sports Exerc. 2015, 47, 451–459. [Google Scholar] [CrossRef]
- Aparicio, V.A.; Ocon, O.; Padilla-Vinuesa, C.; Soriano-Maldonado, A.; Romero-Gallardo, L.; Borges-Cosic, M.; Coll-Risco, I.; Ruiz-Cabello, P.; Acosta-Manzano, P.; Estevez-Lopez, F.; et al. Effects of supervised aerobic and strength training in overweight and grade I obese pregnant women on maternal and foetal health markers: The GESTAFIT randomized controlled trial. BMC Pregnancy Childbirth 2016, 16, 290. [Google Scholar] [CrossRef] [PubMed]
- Rikli, R.E.; Jones, J. Development and validation of a functional fitness test for community residing older adults. J. Aging Phys. Act. 1999, 7, 129–161. [Google Scholar] [CrossRef]
- Zweig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef]
- World Health Organization. WHO Statement on Cesarean Rate. Available online: http://www.paho.org/hq/index.php?option=com_content&view=article&id=10646:2015-la-cesarea-solo-deberia-realizarse-cuando-es-medicamente-necesaria&Itemid=1926&lang=es (accessed on 16 July 2024).
- Ministry of Health and Social Policy and Equality. Strategy for Assistance at Normal Childbirth in the National Health System 2007. Available online: https://www.sanidad.gob.es/areas/calidadAsistencial/estrategias/atencionPartoNormal/docs/estrategiaPartoNormalEnglish.pdf (accessed on 30 July 2024).
- Penfield, C.A.; Wing, D.A. Labor Induction Techniques: Which Is the Best? Obstet. Gynecol. Clin. N. Am. 2017, 44, 567–582. [Google Scholar] [CrossRef]
- Dupont, C.; Carayol, M.; Le Ray, C.; Deneux-Tharaux, C.; Riethmuller, D. Oxytocin administration during spontaneous labor: Guidelines for clinical practice. Guidelines short text. J. Gynecol. Obstet. Hum. Reprod. 2017, 46, 539–543. [Google Scholar] [CrossRef] [PubMed]
- Petersen, L.K.; Vogel, I.; Agger, A.O.; Westergård, J.; Nils, M.; Uldbjerg, N. Variations in serum relaxin (hRLX-2) concentrations during human pregnancy. Acta Obstet. Gynecol. Scand. 1995, 74, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, F.; Haerian, B.S.; Muniandy, S.; Yusof, A.; Dragoo, J.L.; Salleh, N. The effect of relaxin on the musculoskeletal system. Scand. J. Med. Sci. Sports 2014, 24, e220–e229. [Google Scholar] [CrossRef] [PubMed]
- Vodstrcil, L.A.; Tare, M.; Novak, J.; Dragomir, N.; Ramirez, R.J.; Wlodek, M.E.; Conrad, K.P.; Parry, L.J. Relaxin mediates uterine artery compliance during pregnancy and increases uterine blood flow. FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 2012, 26, 4035–4044. [Google Scholar] [CrossRef]
- Pantelis, A.; Sotiriadis, A. Serum relaxin and cervical length for prediction of spontaneous preterm birth in second-trimester symptomatic women. Ultrasound Obstet. Gynecol. 2018, 52, 763–768. [Google Scholar] [CrossRef]
- Pupula, M.; MacLennan, A.H. Effect of porcine relaxin on spontaneous, oxytocin-driven and prostaglandin-driven pig myometrial activity in vitro. J. Reprod. Med. 1989, 34, 819–823. [Google Scholar]
- Lee, I.M.; Blair, S.N.; Tashiro, M.; Horikawa, C.; Matsubayashi, Y.; Yamada, T.; Fujihara, K.; Kato, K.; Sone, H.; Earnest, C.P.; et al. Maximal estimated cardiorespiratory fitness, cardiometabolic risk factors, and metabolic syndrome in the aerobics center longitudinal study. Scand. J. Med. Sci. Sports 2013, 88, 259–270. [Google Scholar] [CrossRef]
- Ebrahimzadeh, S.; Golmakani, N.; Kabirian, M.; Shakeri, M.T. Study of correlation between maternal fatigue and uterine contraction pattern in the active phase of labour. J. Clin. Nurs. 2012, 21, 1563–1569. [Google Scholar] [CrossRef]
- Baena-García, L.; Ocón-Hernández, O. Association of sedentary time and physical activity during pregnancy with maternal and neonatal birth outcomes. The GESTAFIT Project. Menopause 2019, 29, 407–414. [Google Scholar] [CrossRef]

| Maternal Outcome | Mean (SD) |
|---|---|
| Age, years | 32.9 (4.6) |
| Body mass index at 16th gestational week, kg/m2 | 24.9 (4.1) |
| Weight at 16th gestational week, kg | 66.7 (11.9) |
| n (%) | |
| Living with a partner, yes | 133 (97.1) |
| Educational status | |
| Primary or highschool | 33 (24.1) |
| Specialized training | 26 (18.9) |
| University degree | 78 (56.9) |
| Working status | |
| Homework/unemployed | 41 (29.9) |
| Partial-time employed/student | 37 (27) |
| Full-time employed | 59 (43.1) |
| Oxytocin administration to induce or stimulate labour | 44 (32.1) |
| Epidural analgesia, yes | 94 (72.9) |
| Type of birth | |
| Vaginal | 106 (77.4) |
| Non-planned caesarean section | 31 (22.6) |
| Reason of caesarean section | n (%) |
| Risk of loss of foetal well-being | 9 (29) |
| Failed induction | 2 (6.5) |
| Failure to progress | 17 (54.8) |
| Suspected Cephalopelvic Disproportion | 3 (9.7) |
| Birth place | |
| Public hospital | 131 (95.6) |
| Private hospital | 5 (3.6) |
| Home | 1 (0.7) |
| Parity | |
| Nulliparous | 84 (61.3) |
| Multiparous | 53 (38.7) |
| Back-scratch test | Mean (SD) |
| 4.1 (6.2) | |
| 16th gestational week | Median |
| 4.7 | |
| Neonatal outcome | |
| Sex (female, n (%)) | 68 (50.7) |
| Gestational age at birth, weeks | 39.6 (1.3) |
| Birth weight, grams | 3314 (482.8) |
| Apgar Test 1 min | 8.6 (1.0) |
| Apgar Test 5 min | 9.6 (0.7) |
| Oxytocin Was Not Administered (n = 93) | Oxytocin Was Administered (n = 44) | p | p * | Effect Size d-Cohen (95% CI) |
|---|---|---|---|---|
| 5.40 (0.68) | 1.76 (0.89) | 0.001 | 0.004 | 0.59 (0.23, 0.95) |
| Vaginal Birth (n = 106) | Caesarean Section (n = 31) | p | p * | Effect Size d-Cohen (95% CI) |
| 5.04 (0.63) | 1.61 (0.89) | 0.004 | 0.017 | 0.55 (0.21, 0.89) |
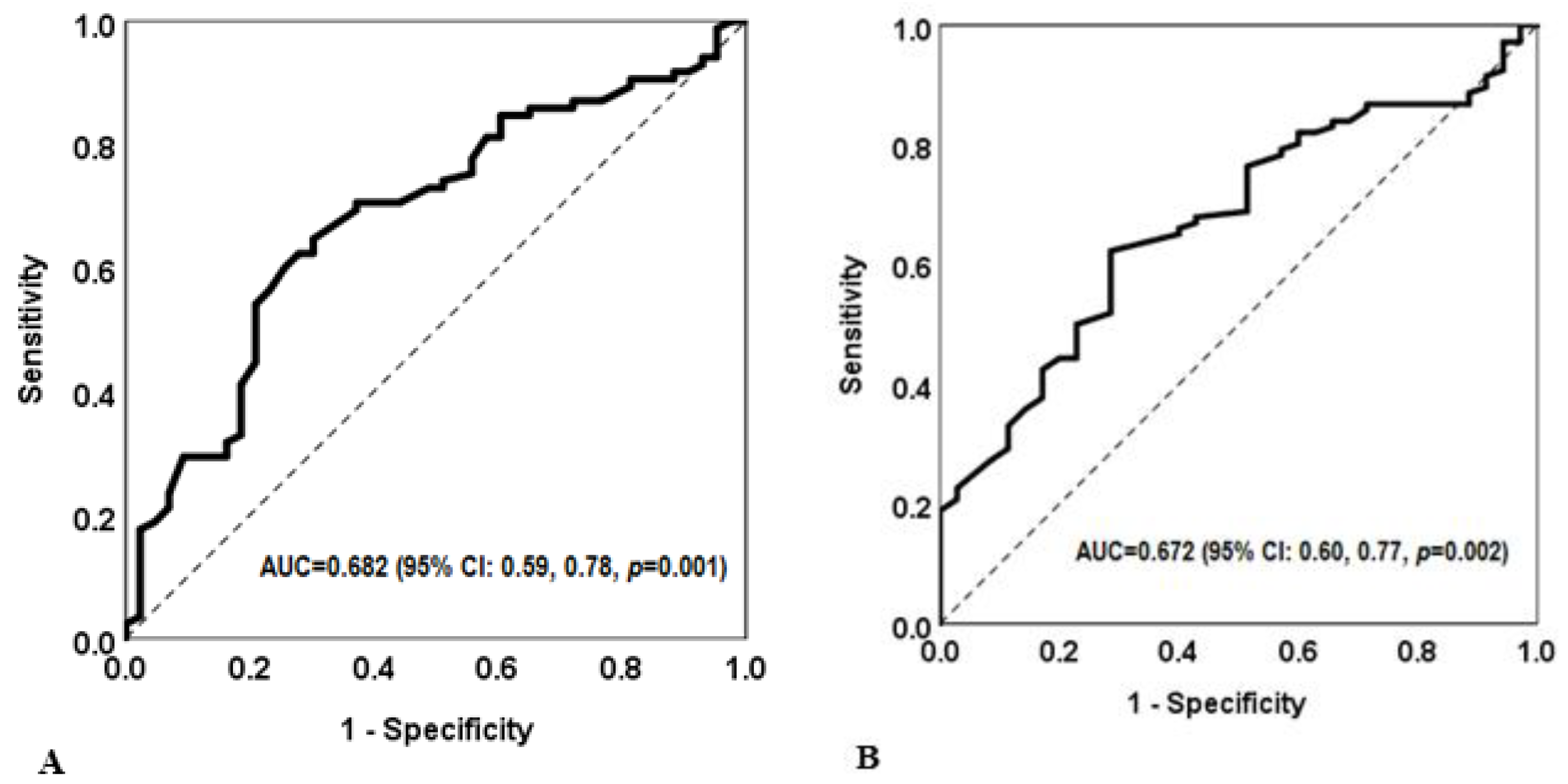
| Low Back-Scratch Test (Based on the Cut-Off) | |||||||
|---|---|---|---|---|---|---|---|
| Cut-Off Point (cm) | Unadjusted Model | Adjusted Model * | |||||
| OR | 95% CI | p | OR | 95% CI | p | ||
| Oxytocin administration | <3.6 | 4.23 | 1.92–9.31 | <0.001 | 4.79 | 1.97–11.6 | 0.001 |
| Caesarean section | <4.1 | 4.13 | 1.80–9.50 | 0.001 | 4.15 | 1.70–10.2 | 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aparicio, V.A.; Marín-Jiménez, N.; Castro-Piñero, J.; Flor-Alemany, M.; Coll-Risco, I.; Baena-García, L. Association between Flexibility, Measured with the Back-Scratch Test, and the Odds of Oxytocin Administration during Labour and Caesarean Section. J. Clin. Med. 2024, 13, 5245. https://doi.org/10.3390/jcm13175245
Aparicio VA, Marín-Jiménez N, Castro-Piñero J, Flor-Alemany M, Coll-Risco I, Baena-García L. Association between Flexibility, Measured with the Back-Scratch Test, and the Odds of Oxytocin Administration during Labour and Caesarean Section. Journal of Clinical Medicine. 2024; 13(17):5245. https://doi.org/10.3390/jcm13175245
Chicago/Turabian StyleAparicio, Virginia A., Nuria Marín-Jiménez, Jose Castro-Piñero, Marta Flor-Alemany, Irene Coll-Risco, and Laura Baena-García. 2024. "Association between Flexibility, Measured with the Back-Scratch Test, and the Odds of Oxytocin Administration during Labour and Caesarean Section" Journal of Clinical Medicine 13, no. 17: 5245. https://doi.org/10.3390/jcm13175245
APA StyleAparicio, V. A., Marín-Jiménez, N., Castro-Piñero, J., Flor-Alemany, M., Coll-Risco, I., & Baena-García, L. (2024). Association between Flexibility, Measured with the Back-Scratch Test, and the Odds of Oxytocin Administration during Labour and Caesarean Section. Journal of Clinical Medicine, 13(17), 5245. https://doi.org/10.3390/jcm13175245










