Management of Mandibular Condyle Fractures in Pediatric Patients: A Multicentric Retrospective Study with 180 Children and Adolescents
Abstract
1. Introduction
2. Patients and Methods
3. Results
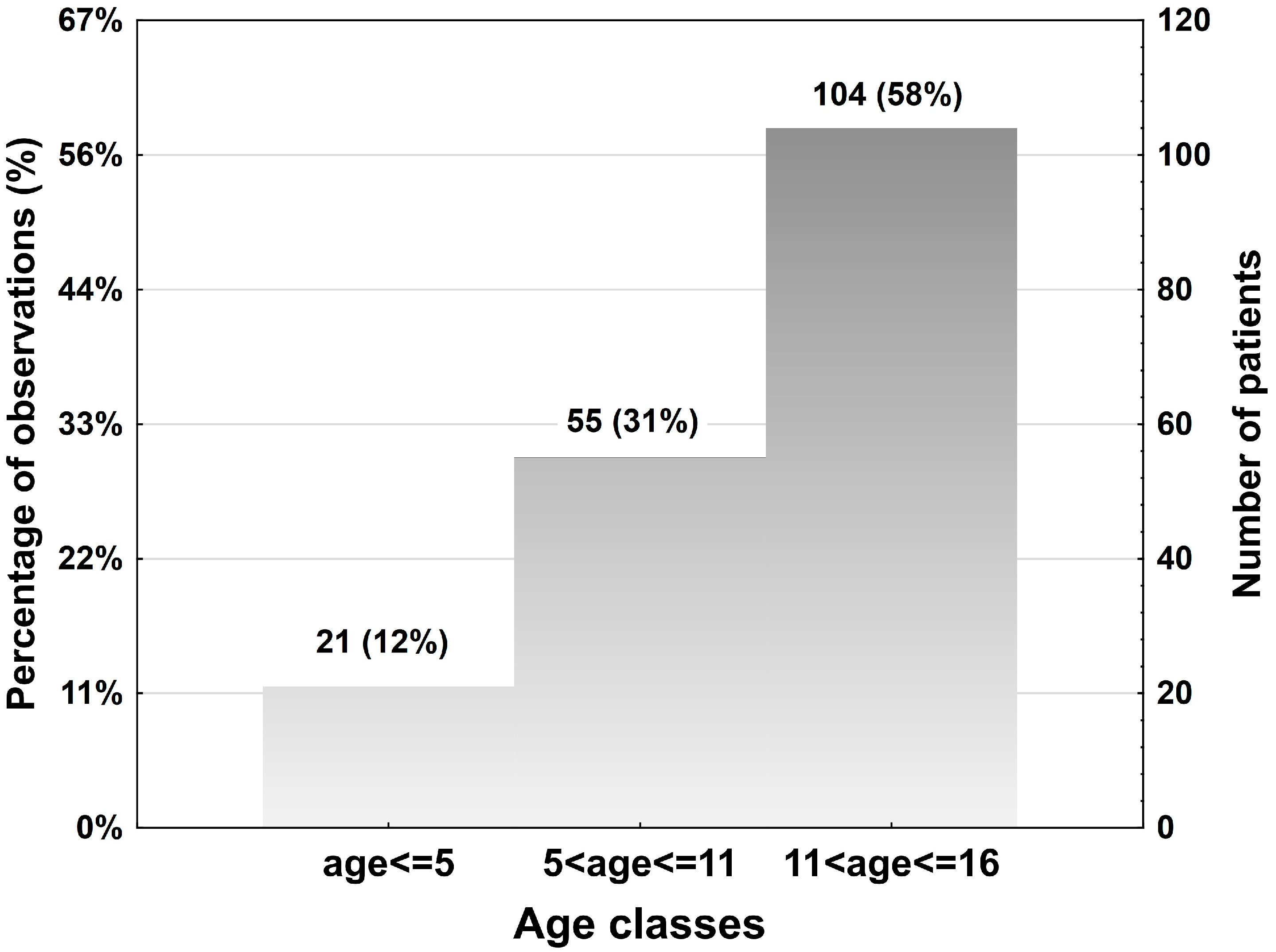
3.1. Epidemiology
3.2. Etiology
3.3. Fractures Localizations and Patterns
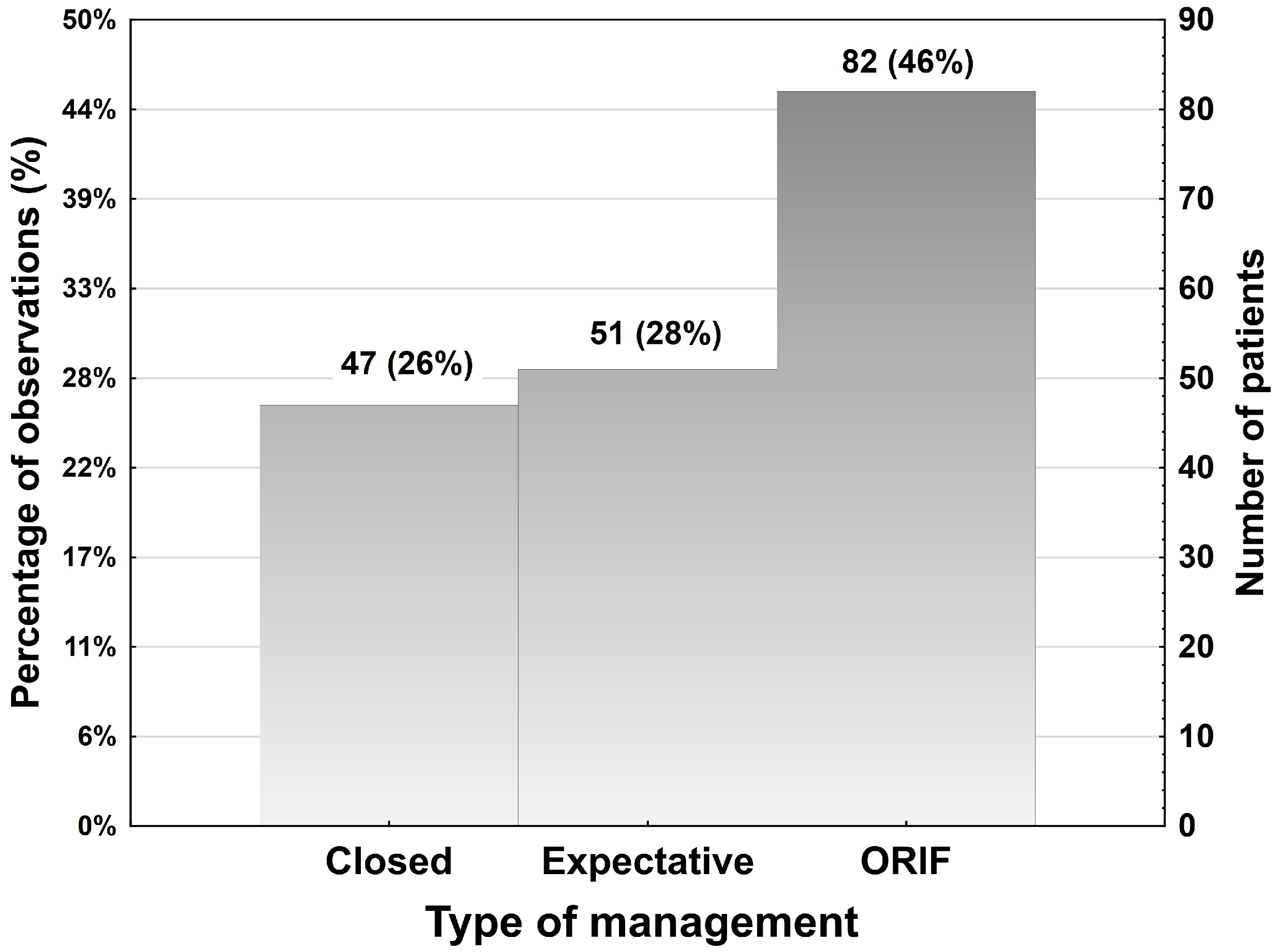
3.4. Management Options: Expectative, Closed and ORIF
3.5. Hardware Removal
3.6. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roccia, F.; Sobrero, F.; Strada, C.; Bottini, G.B.; Goetzinger, M.; Samieirad, S.; Vesnaver, A.; Birk, A.; Gorla, L.F.d.O.; Pereira-Filho, V.A.; et al. Open reduction and internal fixation of paediatric maxillozygomatic complex fractures: An 11-year multicentric retrospective study. Dent. Traumatol. 2024. epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Smartt, J.M., Jr.; Low, D.W.; Bartlett, S.P. The pediatric mandible: II. Management of traumatic injury or fracture. Plast. Reconstr. Surg. 2005, 116, 28e–41e. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F.; Zavattero, E.; Dediol, E.; Uglešić, V.; Kovačič, Ž.; Vesnaver, A.; Konstantinović, V.S.; Petrović, M.; Stephens, J.; et al. European Maxillofacial Trauma (EURMAT) in children: A multicenter and prospective study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Segura-Palleres, I.; Sobrero, F.; Roccia, F.; Gorla, L.F.d.O.; Pereira-Filho, V.A.; Gallafassi, D.; Faverani, L.P.; Romeo, I.; Bojino, A.; Copelli, C.; et al. Characteristics and age-related injury patterns of maxillofacial fractures in children and adolescents: A multicentric and prospective study. Dent. Traumatol. 2022, 38, 213–222. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meier, J.D.; Tollefson, T.T. Pediatric facial trauma. Curr. Opin. Otolaryngol. Head Neck Surg. 2008, 16, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Liao, L.; Huo, S.; Wu, J.; Li, W. Characteristics of pediatric mandibular condylar fractures in Southwest China: A single-center and 12-year retrospective study. Dent. Traumatol. 2024, 40, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Esposito, N.R.; Cisternas, I.N.; Gonzalez, A.C. Surgical treatment of paediatric fractures of the mandibular condyle: A systematic review of the literature. Br. J. Oral Maxillofac. Surg. 2024, 62, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F.; Schellino, E.M.; Baietto, F.; Gallesio, C.M.; Berrone, S.M. Conservative treatment of unilateral displaced condylar fractures in children with mixed dentition. J. Craniofacial Surg. 2012, 23, e376–e378. [Google Scholar] [CrossRef] [PubMed]
- Ghasemzadeh, A.B.; Mundinger, G.S.; Swanson, E.W.; Utria, A.F.B.; Dorafshar, A.H.M. Treatment of Pediatric Condylar Fractures: A 20-Year Experience. Plast. Reconstr. Surg. 2015, 136, 1279–1288. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eckelt, U.; Schneider, M.; Erasmus, F.; Gerlach, K.L.; Kuhlisch, E.; Loukota, R.; Rasse, M.; Schubert, J.; Terheyden, H. Open versus closed treatment of fractures of the mandibular condylar process–a prospective randomized multi-centre study. J. Cranio-Maxillofacial Surg. 2006, 34, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.; Erasmus, F.; Gerlach, K.L.; Kuhlisch, E.; Loukota, R.A.; Rasse, M.; Schubert, J.; Terheyden, H.; Eckelt, U. Open reduction and internal fixation versus closed treatment and mandibulomaxillary fixation of fractures of the mandibular condylar process: A randomized, prospective, multicenter study with special evaluation of fracture level. J. Oral Maxillofac. Surg. 2008, 66, 2537–2544. [Google Scholar] [CrossRef] [PubMed]
- Loukota, R.; Eckelt, U.; De Bont, L.; Rasse, M. Subclassification of fractures of the condylar process of the mandible. Br. J. Oral Maxillofac. Surg. 2005, 43, 72–73. [Google Scholar] [CrossRef] [PubMed]
- Neff, A.; Cornelius, C.-P.; Rasse, M.; Torre, D.; Audigé, L. The Comprehensive AOCMF Classification System: Condylar Process Fractures—Level 3 Tutorial. Craniomaxillofacial Trauma Reconstr. 2014, 7 (Suppl. S1), 44–58. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- WMA Declaration of Helsinki–Ethical Principles for Medical Research Involving Human Subjects. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 1 July 2024).
- Neff, A.; Chossegros, C.; Blanc, J.-L.; Champsaur, P.; Cheynet, F.; Devauchelle, B.; Eckelt, U.; Ferri, J.; Gabrielli, M.F.R.; Guyot, L.; et al. Position paper from the IBRA Symposium on Surgery of the Head—The 2nd International Symposium for Condylar Fracture Osteosynthesis, Marseille, France 2012. J. Cranio-Maxillofacial Surg. 2014, 42, 1234–1249. [Google Scholar] [CrossRef] [PubMed]
- Altikulaç, S.; Lee, N.C.; van der Veen, C.; Benneker, I.; Krabbendam, L.; van Atteveldt, N. The Teenage Brain: Public Perceptions of Neurocognitive Development during Adolescence. J. Cogn. Neurosci. 2019, 31, 339–359. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Youth most at risk for Motor Vehicle Crashes. Available online: https://youth.gov/youth-topics/youth-most-risk-motor-vehicle-crashes (accessed on 1 July 2024).
- Appelbaum, R.D.; Farrell, M.S.; Gelbard, R.B.; Hoth, J.J.; Jawa, R.S.; Kirsch, J.M.; Mandell, S.; A Nohra, E.; Rinderknecht, T.; Rowell, S.; et al. Antibiotic prophylaxis in injury: An American Association for the Surgery of Trauma Critical Care Committee clinical consensus document. Trauma Surg. Acute Care Open 2024, 9, e001304. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Goormans, F.; Coropciuc, R.; Vercruysse, M.; Spriet, I.; Willaert, R.; Politis, C. Systemic Antibiotic Prophylaxis in Maxillofacial Trauma: A Scoping Review and Critical Appraisal. Antibiotics 2022, 11, 483. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Singh, A.K.; Dhungel, S.; Bhattarai, K.; Roychoudhury, A. Do the Benefits of Systemic Corticosteroids Outweigh Adverse Effects During Maxillofacial Trauma Surgery? A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2021, 79, 1530.e1–1530.e21. [Google Scholar] [CrossRef] [PubMed]
- Li, M.-X.; Xing, X.; Li, Z.-B. Classification and treatment strategies for condylar fractures in children. Br. J. Oral Maxillofac. Surg. 2021, 59, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.C.; Reynolds, R.; Recker, M.J.; Markiewicz, M.R. Rigid Fixation of the Pediatric Facial Skeleton. Oral Maxillofac. Surg. Clin. N. Am. 2023, 35, 529–541. [Google Scholar] [CrossRef] [PubMed]
- Magge, S.N.; Chen, H.I.; Heuer, G.G.; Carrasco, L.R.; Storm, P.B. Dislocation of the mandible into the middle cranial fossa. J. Neurosurgery Pediatr. 2007, 107, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Haug, R.H.; Brandt, M.T. Closed reduction, open reduction, and endoscopic assistance: Current thoughts on the management of mandibular condyle fractures. Plast. Reconstr. Surg. 2007, 120 (Suppl. 2), 90S–102S. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E.; Throckmorton, G.S. Treatment of mandibular condylar process fractures: Biological considerations. J. Oral Maxillofac. Surg. 2005, 63, 115–134. [Google Scholar] [CrossRef] [PubMed]
- Dimitroulis, G. Condylar injuries in growing patients. Aust. Dent. J. 1997, 42, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Kao, R.; Rabbani, C.C.; Patel, J.M.; Parkhurst, S.M.; Mantravadi, A.V.; Ting, J.Y.; Sim, M.W.; Koehler, K.; Shipchandler, T.Z. Management of Mandible Fracture in 150 Children Across 7 Years in a US Tertiary Care Hospital. JAMA Facial Plast. Surg. 2019, 21, 414–418. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zide, M.F.; Kent, J.N. Indications for open reduction of mandibular condyle fractures. J. Oral Maxillofac. Surg. 1983, 41, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Kommers, S.C.; Boffano, P.; Forouzanfar, T. Consensus or controversy? The classification and treatment decision-making by 491 maxillofacial surgeons from around the world in three cases of a unilateral mandibular condyle fracture. J. Cranio-Maxillofacial Surg. 2015, 43, 1952–1960. [Google Scholar] [CrossRef] [PubMed]
- Cornelius, C.P.; Ehrenfeld, M.; Laubengeiger, M.; Simonis, A.; Kaltsounis, E. Ergebnisse eines konservativ-funktionellen Therapiekonzepts bei kindlichen Kondylusfrakturen. Dtsch. Zahnärztl. Z. 1991, 46, 46–49. [Google Scholar] [PubMed]
- Schiel, S.; Probst, F.; Mayer, P.; Kaeppler, G.; Cornelius, C.P. Kiefergelenkfortsatzbasis- und Kiefergelenkhalsfrakturen bei Kindern und Jugendlichen—Plädoyer für eine transoral endoskopisch assistierte operative Versorgung bei starker Dislokation und Luxation. Condylar Base and Neck Fractures in Children and Adolescents—A Plea for Transoral Endoscopically Assisted Management of Severe Dislocations and Luxations. OP-J. 2013, 29, 156–163. Available online: https://www.thieme-connect.de/products/ejournals/html/10.1055/s-0033-1350818 (accessed on 1 June 2024).
- Vesnaver, A.; Kansky, A.A. Dislocated pediatric condyle fractures—should conservative treatment always be the rule? J. Cranio-Maxillofacial Surg. 2020, 48, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Bera, R.N.; Kumar, J.A.; Kanojia, S.; Boojar, F.M.A.; Chauhan, N.; Hirani, M.S. How far we have come with the Management of Condylar Fractures? A Meta-Analysis of Closed Versus Open Versus Endoscopic Management. J. Maxillofac. Oral Surg. 2021, 21, 888–903. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schön, R.; Gutwald, R.; Schramm, A.; Gellrich, N.-C.; Schmelzeisen, R. Endoscopy-assisted open treatment of condylar fractures of the mandible: Extraoral vs intraoral approach. Int. J. Oral Maxillofac. Surg. 2002, 31, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Schön, R.; Schramm, A.; Gellrich, N.-C.; Schmelzeisen, R. Follow-up of condylar fractures of the mandible in 8 patients at 18 months after transoral endoscopic-assisted open treatment. J. Oral Maxillofac. Surg. 2003, 61, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Schön, R.; Fakler, O.; Gellrich, N.-C.; Schmelzeisen, R. Five-Year Experience with the transoral endoscopically assisted treatment of displaced condylar mandible fractures. Plast. Reconstr. Surg. 2005, 116, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Schoen, R.; Gellrich, N.-C.; Schmelzeisen, R. Minimally invasive open reduction of a displaced condylar fracture in a child. Br. J. Oral Maxillofac. Surg. 2005, 43, 258–260. [Google Scholar] [CrossRef] [PubMed]
- Schoen, R.; Fakler, O.; Metzger, M.; Weyer, N.; Schmelzeisen, R. Preliminary functional results of endoscope-assisted transoral treatment of displaced bilateral condylar mandible fractures. Int. J. Oral Maxillofac. Surg. 2008, 37, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Schiel, S.; Mayer, P.; Probst, F.; Otto, S.; Cornelius, C.-P. Transoral open reduction and fixation of mandibular condylar base and neck fractures in children and young teenagers—A beneficial treatment option? J. Oral Maxillofac. Surg. 2013, 71, 1220–1230. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.-M.; Yang, J.; Bai, R.-C.; Ge, L.-H.; Zhang, Y. A retrospective study of using removable occlusal splint in the treatment of condylar fracture in children. J. Cranio-Maxillofacial Surg. 2014, 42, 1078–1082. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Y.; Zou, Y.; Wang, S.; Du, C.; Xu, B.; Zhu, M. Three-dimensional evaluation of condylar morphology after closed treatment of unilateral intracapsular condylar fracture in children and adolescents. J. Cranio-Maxillofacial Surg. 2020, 48, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Malinge, M.; Grimaud, F.; Perrin, J.-P.; Loin, J.; Anquetil, M.; Mercier, J.; Corre, P.; Bertin, H. Outcomes of functional treatment of condylar mandibular fractures with an articular impact: A retrospective study of 108 children. J. Stomatol. Oral Maxillofac. Surg. 2021, 123, 177–183. [Google Scholar] [CrossRef] [PubMed]
- de Amaratunga, N. Mouth opening after release of maxillomandibular fixation in fracture patients. J. Oral Maxillofac. Surg. 1987, 45, 383–385. [Google Scholar] [CrossRef] [PubMed]
- Sobrero, F.; Roccia, F.; Galetta, G.; Strada, C.; Gerbino, G. Pediatric mandibular fractures: Surgical management and outcomes in the deciduous, mixed and permanent dentitions. Dent. Traumatol. 2023, 39, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Sudduth, J.D.; Byrd, R.D.; Marquez, J.L.B.; Bautista, C.H.B.; Chen, J.B.; Battistini, A.; Yamashiro, D.K.D.; Gociman, B. Pediatric Mandibular Fracture Management: Intraoperative Thermoplastic Splint Fabrication and Circummandibular Wires, without Maxillomandibular Fixation. Plast. Reconstr. Surg. Glob. Open 2024, 12, e5883. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bottini, G.B.M.; Gaggl, A.M.; Brandtner, C.M. Advances in Open Reduction and Internal Fixation of Multiple Mandibular Fractures with Condylar Involvement. Plast. Reconstr. Surg. 2023, 154, 348e–350e. [Google Scholar] [CrossRef] [PubMed]
- Pontell, M.E.; Niklinska, E.B.; Braun, S.A.; Jaeger, N.; Kelly, K.J.; Golinko, M.S. Resorbable Versus Titanium Rigid Fixation for Pediatric Mandibular Fractures: A Systematic Review, Institutional Experience and Comparative Analysis. Craniomaxillofacial Trauma Reconstr. 2022, 15, 189–200. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bos, R.R. Treatment of pediatric facial fractures: The case for metallic fixation. J. Oral Maxillofac. Surg. 2005, 63, 382–384. [Google Scholar] [CrossRef] [PubMed]
- Skroch, L.; Fischer, I.; Meisgeier, A.; Kozolka, F.; Apitzsch, J.; Neff, A. Condylar remodeling after osteosynthesis of fractures of the condylar head or close to the temporomandibular joint. J. Cranio-Maxillofacial Surg. 2020, 48, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Thorén, H.; Hallikainen, D.; Iizuka, T.; Lindqvist, C. Condylar process fractures in children: A follow-up study of fractures with total dislocation of the condyle from the glenoid fossa. J. Oral Maxillofac. Surg. 2001, 59, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Talwar, R.M.; Ellis, E.; Throckmorton, G.S. Adaptations of the masticatory system after bilateral fractures of the mandibular condylar process. J. Oral Maxillofac. Surg. 1998, 56, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.; Yang, Y.; Liu, Y.; Wang, J.; Zhang, W.; Ma, Q. How Does the Remodeling Capacity of Children Affect the Morphologic Changes of Fractured Mandibular Condylar Processes After Conservative Treatment? J. Oral Maxillofac. Surg. 2018, 76, 1279.e1–1279.e7. [Google Scholar] [CrossRef] [PubMed]
- Helkimo, M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state. Sven. Tandlak. Tidskr. Swed. Dent. J. 1974, 67, 101–121. [Google Scholar] [PubMed]
- Alyahya, A.; Bin Ahmed, A.; Nusair, Y.; Ababtain, R.; Alhussain, A.; Alshafei, A. Mandibular condylar fracture: A systematic review of systematic reviews and a proposed algorithm for management. Br. J. Oral Maxillofac. Surg. 2020, 58, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Jenkyn, I.; Bosley, R.; Jenkyn, C.; Basyuni, S.; Fowell, C. Management of Mandibular Condyle Fractures in Paediatric Patients: A Systematic Review. J. Oral Maxillofac. Res. 2023, 14, e1. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Khattak, Y.R.; Sardar, T.; Iqbal, A.; Khan, M.H.; Khan, A.; Ullah, U.; Ahmad, I. Treatment of pediatric bilateral condylar fractures: A comprehensive analysis. J. Stomatol. Oral Maxillofac. Surg. 2023, 124, 101339. [Google Scholar] [CrossRef] [PubMed]

| Country | City | Institution |
|---|---|---|
| Austria | Salzburg | Dpt. Oral and Maxillofacial Surgery, Paracelsus Medical University |
| Belgium | Leuven | Dpt. Oral and Maxillofacial Surgery, University Hospitals Leuven |
| Bosnia and Herzegovina | Mostar | Clinic for ENT and OMS University Clinical Hospital |
| Brazil | São Paulo | Dpt. Diagnosis and Surgery, Araraquara Dental School—UNESP—State University |
| Bulgaria | Plovdiv | Dpt. Maxillofacial Surgery, Medical University |
| Croatia | Zagreb | Dpt. Maxillofacial Surgery, University Hospital Dubrava |
| India | Aligarh | Dpt. Oral and Maxillofacial Surgery, Aligarh Muslim University |
| Iran | Mashhad | Dpt. Oral and Maxillofacial Surgery, Mashhad Dental School, University of Medical Sciences |
| Italy | Turin | Division of Maxillofacial Surgery, Città della Salute e della Scienza, University of Turin |
| Nigeria | Ibadan | Dpt. Oral and Maxillofacial Surgery, College of Medicine, University of Ibadan |
| Serbia | Belgrade | Clinic of Maxillofacial Surgery, School of Dental Medicine, University of Belgrade |
| Slovenia | Ljubljana | Dpt. Maxillofacial and Oral Surgery, University Medical Centre |
| Tanzania | Muhimbili | Dpt. Oral and Maxillofacial Surgery, University of Health and Allied Sciences |
| United Kingdom | Dundee | Dpt. Oral and Maxillofacial Surgery, University of Dundee |
| Management | ||||
|---|---|---|---|---|
| Country | Closed | Expectative | ORIF | Number of Patients |
| ITALY | 1 | 7 | 2 | 10 |
| Percentage (%) | 10% | 70% | 20% | |
| BULGARIA | 12 | 0 | 0 | 12 |
| Percentage (%) | 100% | 0% | 0% | |
| SLOVENIA | 0 | 11 | 40 | 51 |
| Percentage (%) | 0% | 22% | 78% | |
| BELGIUM | 6 | 0 | 0 | 6 |
| Percentage (%) | 100% | 0% | 0% | |
| AUSTRIA | 0 | 11 | 17 | 28 |
| Percentage (%) | 0% | 39% | 61% | |
| CROATIA | 7 | 4 | 5 | 16 |
| Percentage (%) | 44% | 25% | 31% | |
| SERBIA | 9 | 2 | 0 | 11 |
| Percentage (%) | 82% | 18% | 0% | |
| INDIA | 8 | 2 | 0 | 10 |
| Percentage (%) | 80% | 20% | 0% | |
| BOSNIA | 0 | 2 | 1 | 3 |
| Percentage (%) | 0% | 67% | 33% | |
| BRAZIL | 0 | 2 | 7 | 9 |
| Percentage (%) | 0% | 22% | 78% | |
| IRAN | 2 | 0 | 10 | 12 |
| Percentage (%) | 17% | 0% | 83% | |
| TANZANIA | 1 | 3 | 0 | 4 |
| Percentage (%) | 25% | 75% | 0% | |
| UK | 1 | 6 | 0 | 7 |
| Percentage (%) | 14% | 86% | 0% | |
| NIGERIA | 0 | 1 | 0 | 1 |
| Percentage (%) | 0% | 100% | 0% | |
| Number of patients | 47 | 51 | 82 | 180 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bottini, G.B.; Hitzl, W.; Götzinger, M.; Politis, C.; Dubron, K.; Kordić, M.; Sivrić, A.; Pechalova, P.; Sapundzhiev, A.; Pereira-Filho, V.A.; et al. Management of Mandibular Condyle Fractures in Pediatric Patients: A Multicentric Retrospective Study with 180 Children and Adolescents. J. Clin. Med. 2024, 13, 5455. https://doi.org/10.3390/jcm13185455
Bottini GB, Hitzl W, Götzinger M, Politis C, Dubron K, Kordić M, Sivrić A, Pechalova P, Sapundzhiev A, Pereira-Filho VA, et al. Management of Mandibular Condyle Fractures in Pediatric Patients: A Multicentric Retrospective Study with 180 Children and Adolescents. Journal of Clinical Medicine. 2024; 13(18):5455. https://doi.org/10.3390/jcm13185455
Chicago/Turabian StyleBottini, Gian Battista, Wolfgang Hitzl, Maximilian Götzinger, Constantinus Politis, Kathia Dubron, Mario Kordić, Anamaria Sivrić, Petia Pechalova, Angel Sapundzhiev, Valfrido Antonio Pereira-Filho, and et al. 2024. "Management of Mandibular Condyle Fractures in Pediatric Patients: A Multicentric Retrospective Study with 180 Children and Adolescents" Journal of Clinical Medicine 13, no. 18: 5455. https://doi.org/10.3390/jcm13185455
APA StyleBottini, G. B., Hitzl, W., Götzinger, M., Politis, C., Dubron, K., Kordić, M., Sivrić, A., Pechalova, P., Sapundzhiev, A., Pereira-Filho, V. A., de Oliveira Gorla, L. F., Dediol, E., Kos, B., Rahman, T., Rahman, S. A., Samieirad, S., Aladelusi, T., Konstantinovic, V. S., Lazić, M., ... Sobrero, F. (2024). Management of Mandibular Condyle Fractures in Pediatric Patients: A Multicentric Retrospective Study with 180 Children and Adolescents. Journal of Clinical Medicine, 13(18), 5455. https://doi.org/10.3390/jcm13185455







