Goal-Directed Fluid Therapy Using Pulse Pressure Variation in Thoracic Surgery Requiring One-Lung Ventilation: A Randomized Controlled Trial
Abstract
1. Introduction
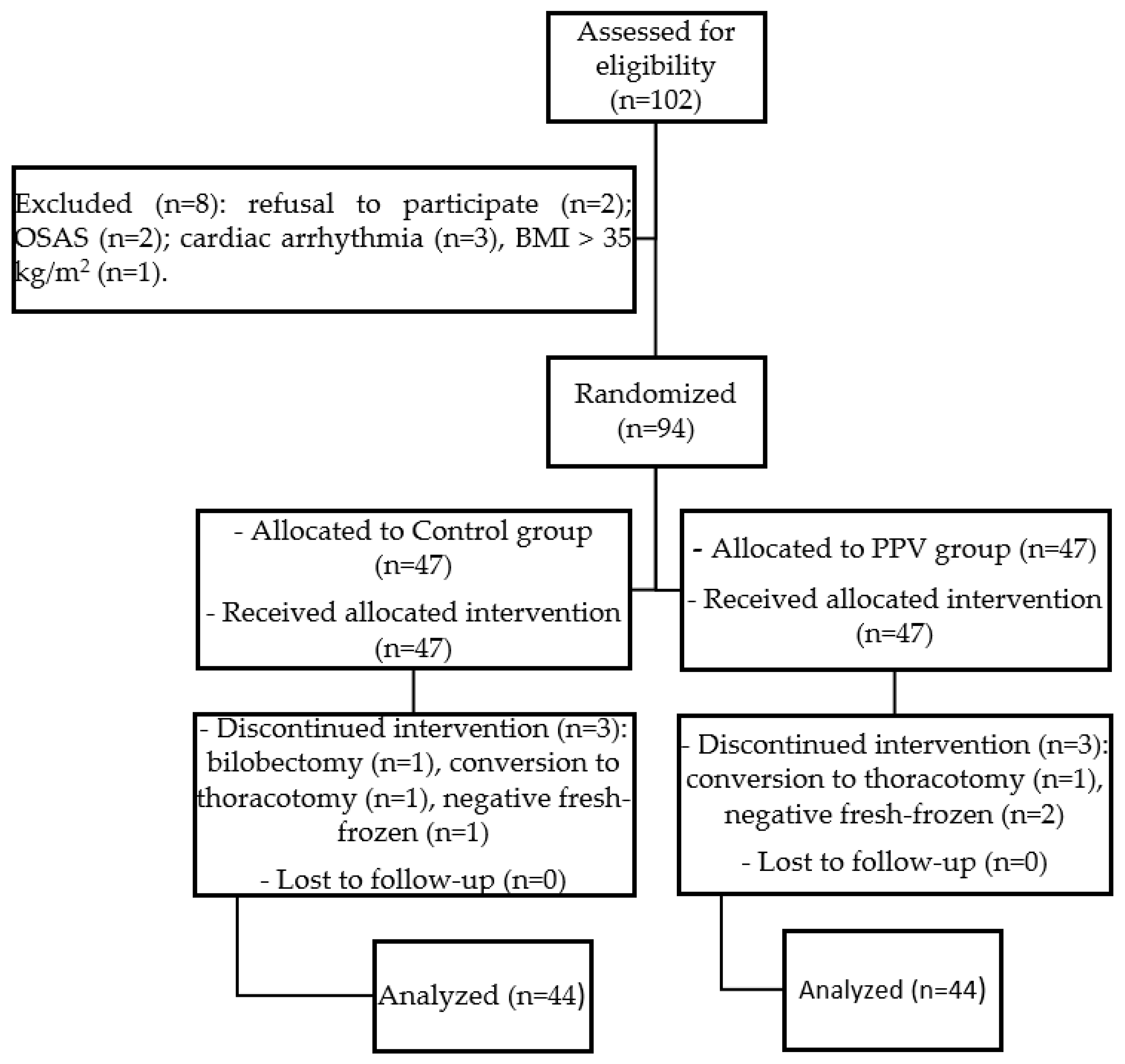
2. Materials and Methods
2.1. Ethical Statement
2.2. Patients
2.3. Randomization and Masking
2.4. Anesthesia and Monitoring
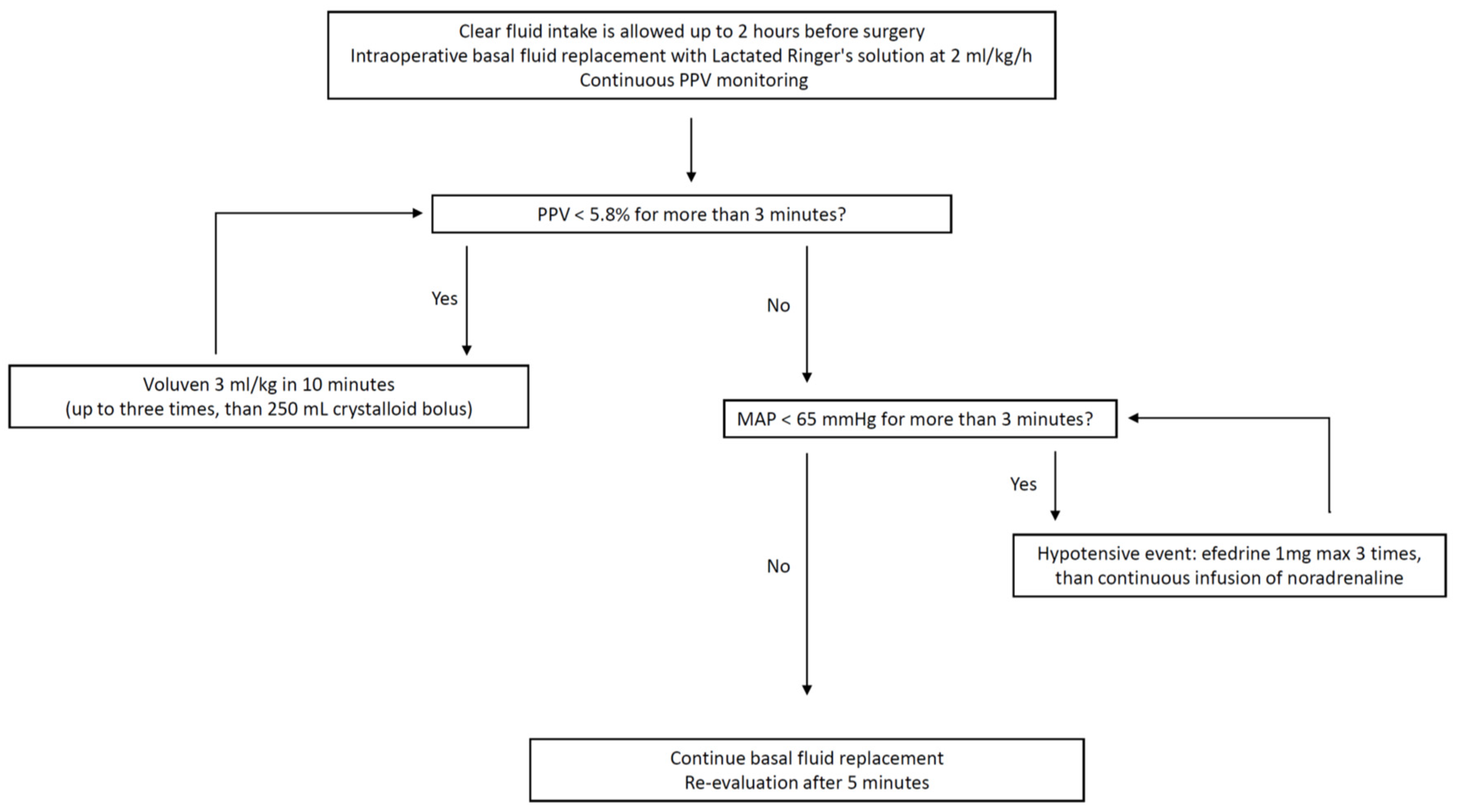
2.5. Intervention Protocol
2.6. Primary and Secondary Outcomes
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, E.H. Optimal fluid therapy for thoracic surgery. J. Thorac. Dis. 2019, 11, 1753–1755. [Google Scholar] [CrossRef] [PubMed]
- Alam, N.; Park, B.J.; Wilton, A.; Seshan, V.E.; Bains, M.S.; Downey, R.J.; Flores, R.M.; Rizk, N.; Rusch, V.W.; Amar, D. Incidence and risk factors for lung injury after lung cancer resection. Ann. Thorac. Surg. 2007, 84, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Licker, M.; de Perrot, M.; Spiliopoulos, A.; Robert, J.; Diaper, J.; Chevalley, C.; Tschopp, J.M. Risk factors for acute lung injury after thoracic surgery for lung cancer. Anesth. Analg. 2003, 97, 1558–1565. [Google Scholar] [CrossRef] [PubMed]
- Arslantas, M.K.; Kara, H.V.; Tuncer, B.B.; Yildizeli, B.; Yuksel, M.; Bostanci, K.; Bekiroglu, N.; Kararmaz, A.; Cinel, I.; Batirel, H.F. Effect of the amount of intraoperative fluid administration on postoperative pulmonary complications following anatomic lung resections. J. Thorac. Cardiovasc. Surg. 2015, 149, 314–320. [Google Scholar] [CrossRef]
- Batchelor, T.J.P.; Rasburn, N.J.; Abdelnour-Berchtold, E.; Brunelli, A.; Cerfolio, R.J.; Gonzalez, M.; Ljungqvist, O.; Petersen, R.H.; Popescu, W.M.; Slinger, P.D.; et al. Guidelines for enhanced recovery after lung surgery: Recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur. J. Cardiothorac. Surg. 2019, 55, 91–115. [Google Scholar] [CrossRef]
- Chau, E.H.; Slinger, P. Perioperative fluid management for pulmonary resection surgery and esophagectomy. Semin. Cardiothorac. Vasc. Anesth. 2014, 18, 36–44. [Google Scholar] [CrossRef]
- Licker, M.; Triponez, F.; Ellenberger, C.; Karenovics, W. Less Fluids and a More Physiological Approach. Turk. J. Anaesthesiol. Reanim. 2016, 44, 230–232. [Google Scholar] [CrossRef]
- Evans, R.G.; Naidu, B. Does a conservative fluid management strategy in the perioperative management of lung resection patients reduce the risk of acute lung injury? Interact. Cardiovasc. Thorac. Surg. 2012, 15, 498–504. [Google Scholar] [CrossRef]
- Assaad, S.; Popescu, W.; Perrino, A. Fluid management in thoracic surgery. Curr. Opin. Anaesthesiol. 2013, 26, 31–39. [Google Scholar] [CrossRef]
- Şentürk, M.; Bingül, E.S.; Turhan, Ö. Should fluid management in thoracic surgery be goal directed? Curr. Opin. Anaesthesiol. 2022, 35, 89–95. [Google Scholar] [CrossRef]
- Tote, S.P.; Grounds, R.M. Performing perioperative optimization of the high-risk surgical patient. Br. J. Anaesth. 2006, 97, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Rollins, K.E.; Lobo, D.N. Intraoperative Goal-directed Fluid Therapy in Elective Major Abdominal Surgery: A Meta-analysis of Randomized Controlled Trials. Ann. Surg. 2016, 263, 465–476. [Google Scholar] [CrossRef]
- Sun, Y.; Chai, F.; Pan, C.; Romeiser, J.L.; Gan, T.J. Effect of perioperative goal-directed hemodynamic therapy on postoperative recovery following major abdominal surgery–A systematic review and meta-analysis of randomized controlled trials. Crit. Care 2017, 21, 141. [Google Scholar] [CrossRef]
- Hamilton, M.A.; Cecconi, M.; Rhodes, A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth. Analg. 2011, 112, 1392–1402. [Google Scholar] [CrossRef]
- Osawa, E.A.; Rhodes, A.; Landoni, G.; Galas, F.R.; Fukushima, J.T.; Park, C.H.; Almeida, J.P.; Nakamura, R.E.; Strabelli, T.M.; Pileggi, B.; et al. Effect of Perioperative Goal-Directed Hemodynamic Resuscitation Therapy on Outcomes Following Cardiac Surgery: A Randomized Clinical Trial and Systematic Review. Crit. Care. Med. 2016, 44, 724–733. [Google Scholar] [CrossRef]
- Zhang, J.; Chen, C.Q.; Lei, X.Z.; Feng, Z.Y.; Zhu, S.M. Goal-directed fluid optimization based on stroke volume variation and cardiac index during one-lung ventilation in patients undergoing thoracoscopy lobectomy operations: A pilot study. Clinics 2013, 68, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Shu, S.H.; Wang, D.; Chai, X.Q.; Xie, Y.H.; Zhou, W.D. Goal-directed fluid restriction using stroke volume variation and cardiac index during one-lung ventilation: A randomized controlled trial. J. Thorac. Dis. 2017, 9, 2992–3004. [Google Scholar] [CrossRef] [PubMed]
- Suehiro, K.; Okutani, R. Influence of tidal volume for stroke volume variation to predict fluid responsiveness in patients undergoing one-lung ventilation. J. Anesth. 2011, 25, 777–780. [Google Scholar] [CrossRef]
- Rathore, A.; Singh, S.; Lamsal, R.; Taank, P.; Paul, D. Validity of Pulse Pressure Variation (PPV) Compared with Stroke Volume Variation (SVV) in Predicting Fluid Responsiveness. Turk. J. Anaesthesiol. Reanim. 2017, 45, 210–217. [Google Scholar] [CrossRef]
- Malbouisson, L.M.S.; Silva, J.M., Jr.; Carmona, M.J.C.; Lopes, M.R.; Assunção, M.S.; Valiatti, J.L.D.S.; Simões, C.M.; Auler, J.O.C., Jr. A pragmatic multi-center trial of goal-directed fluid management based on pulse pressure variation monitoring during high-risk surgery. BMC. Anesthesiol. 2017, 17, 70. [Google Scholar] [CrossRef]
- Lopes, M.R.; Oliveira, M.A.; Pereira, V.O.; Lemos, I.P.; Auler, J.O., Jr.; Michard, F. Goal-directed fluid management based on pulse pressure variation monitoring during high-risk surgery: A pilot randomized controlled trial. Crit. Care 2007, 11, R100. [Google Scholar] [CrossRef]
- Lee, J.H.; Jeon, Y.; Bahk, J.H.; Gil, N.S.; Hong, D.M.; Kim, J.H.; Kim, H.J. Pulse pressure variation as a predictor of fluid responsiveness during one-lung ventilation for lung surgery using thoracotomy: Randomised controlled study. Eur. J. Anaesthesiol. 2011, 28, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Miñana, A.; Parra, M.J.; Carbonell, J.; Soro, M.; Belda, J.; Ferrando, C. Validation study of the dynamic parameters of pulse wave in pulmonary resection surgery. Rev. Esp. Anestesiol. Reanim. (Engl. Ed.) 2020, 67, 55–62. [Google Scholar] [CrossRef]
- Ismail, M.; Nachira, D. Devising the guidelines: The concept of uniportal video-assisted thoracic surgery-instrumentation and operatory room staff. J. Thorac. Dis. 2019, 11, S2079–S2085. [Google Scholar] [CrossRef] [PubMed]
- Nachira, D.; Punzo, G.; Calabrese, G.; Sessa, F.; Congedo, M.T.; Beccia, G.; Aceto, P.; Kuzmych, K.; Cambise, C.; Sassorossi, C.; et al. The Efficacy of Continuous Serratus Anterior and Erector Spinae Plane Blocks vs Intercostal Nerve Block in Uniportal-Vats Surgery: A Propensity-Matched Prospective Trial. J. Clin. Med. 2024, 13, 606. [Google Scholar] [CrossRef]
- The European Medicines Agency: New Review of Hydroxyethyl Starch-Containing Solutions for Infusion Started. 2013. Available online: https://www.ema.europa.eu/documents/referral/hydroxyethyl-starch-article-107i-procedure-review-started_en.pdf (accessed on 1 July 2024).
- FDA Safety Communication: Boxed Warning on Increased Mortality and Severe Injury; and Additional Warning on Risk of Bleeding; for Use of Hydroxyethyl Starch Solutions in Some Settings. 2013. Available online: https://www.fffenterprises.com/assets/downloads/Article-FDASafetyCommunicationBoxedWarning6-13.pdf (accessed on 1 July 2024).
- Piccioni, F.; Spagnesi, L.; Pelosi, P.; Bignami, E.; Guarnieri, M.; Fumagalli, L.; Polati, E.; Schweiger, V.; Comi, D.; D’Andrea, R.; et al. Postoperative pulmonary complications and mortality after major abdominal surgery. An observational multicenter prospective study. Minerva Anestesiol. 2023, 89, 964–976. [Google Scholar] [CrossRef] [PubMed]
- Perilli, V.; Aceto, P.; Ancona, P.; De Cicco, R.; Papanice, D.; Magalini, S.; Pepe, G.; Cozza, V.; Gui, D.; Lai, C.; et al. Role of surgical setting and patients-related factors in predicting the occurrence of postoperative pulmonary complications after abdominal surgery. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 547–550. [Google Scholar] [CrossRef]
- Kan, C.F.K.; Skaggs, J.D. Current Commonly Used Dynamic Parameters and Monitoring Systems for Perioperative Goal-Directed Fluid Therapy: A Review. Yale J. Biol. Med. 2023, 96, 107–123. [Google Scholar] [CrossRef]
- Jeong, D.M.; Ahn, H.J.; Park, H.W.; Yang, M.; Kim, J.A.; Park, J. Stroke Volume Variation and Pulse Pressure Variation Are Not Useful for Predicting Fluid Responsiveness in Thoracic Surgery. Anesth. Analg. 2017, 125, 1158–1165. [Google Scholar] [CrossRef]
- Choi, K.H.; Shim, J.K.; Kim, D.W.; Byun, C.S.; Park, J.H. Dynamic Indices Fail to Predict Fluid Responsiveness in Patients Undergoing One-Lung Ventilation for Thoracoscopic Surgery. J. Clin. Med. 2021, 10, 2335. [Google Scholar] [CrossRef]
- Fu, Q.; Duan, M.; Zhao, F.; Mi, W. Evaluation of stroke volume variation and pulse pressure variation as predictors of fluid responsiveness in patients undergoing protective one-lung ventilation. Drug Discov. Ther. 2015, 9, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Piccioni, F.; Bernasconi, F.; Tramontano, G.T.A.; Langer, M. A systematic review of pulse pressure variation and stroke volume variation to predict fluid responsiveness during cardiac and thoracic surgery. J. Clin. Monit. Comput. 2017, 31, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Feng, Z.; Cai, J.; Duan, M.; Li, H.; Dai, Z.; Lv, H.; Xu, Z.; Wang, H.; Chen, Y. Accuracy of stroke volume variation and pulse pressure variation in predicting fluid responsiveness undergoing one-lung ventilation during thoracic surgery: A systematic review and meta-analysis. Ann. Transl. Med. 2023, 11, 19. [Google Scholar] [CrossRef] [PubMed]
- Haas, S.; Eichhorn, V.; Hasbach, T.; Trepte, C.; Kutup, A.; Goetz, A.E.; Reuter, D.A. Goal-directed fluid therapy using stroke volume variation does not result in pulmonary fluid overload in thoracic surgery requiring one-lung ventilation. Crit. Care. Res. Pract. 2012, 2012, 687018. [Google Scholar] [CrossRef][Green Version]
- Piccioni, F.; Langiano, N.; Bignami, E.; Guarnieri, M.; Proto, P.; D’Andrea, R.; Mazzoli, C.A.; Riccardi, I.; Bacuzzi, A.; Guzzetti, L.; et al. One-Lung Ventilation Investigators Group (Supplementary Appendix S1). One-Lung Ventilation and Postoperative Pulmonary Complications After Major Lung Resection Surgery. A Multicenter Randomized Controlled Trial. J. Cardiothorac. Vasc. Anesth. 2023, 37, 2561–2571. [Google Scholar] [CrossRef]


| Near-Zero Group (n = 44) | PPV Group (n = 44) | t or χ2 | p | |
|---|---|---|---|---|
| Age, years | 68.93 (8.71) | 66.82 (11.53) | 0.97 | 0.33 |
| BMI | 25.20 (3.88) | 26.00 (4.11) | −0.93 | 0.35 |
| NYHA class (I/II/III) | 30/13/1 | 27/17/0 | 1.69 | 0.43 |
| ASA score, II/III | 30/14 | 29/15 | 0.05 | 0.82 |
| AH (Y/N) | 14/30 | 31/13 | 0.05 | 0.82 |
| IHD (Y/N) | 3/41 | 2/42 | 0.21 | 0.64 |
| DM II (Y/N) | 6/38 | 5/39 | 0.10 | 0.75 |
| Bronchial Asthma (Y/N) | 0/44 | 2/42 | 2.05 | 0.15 |
| COPD (Y/N) | 23/21 | 24/20 | 0.04 | 0.83 |
| VHD (Y/N) | 2/42 | 1/43 | 0.34 | 0.56 |
| CKD (Y/N) | 2/42 | 2/42 | 0.00 | 1.00 |
| CV (Y/N) | 1/43 | 0/44 | 1.01 | 0.31 |
| PVD | 3/41 | 1/43 | 1.05 | 0.31 |
| FVC | 3.49 (0.93) | 3.33 (0.81) | 0.85 | 0.40 |
| FEV1 | 2.58 (0.69) | 2.50 (0.68) | 0.54 | 0.59 |
| FEV1/FVC (%) | 74.42 (7.66) | 75.16 (8.08) | −0.45 | 0.66 |
| DLCO (%) | 78.80 (7.07) | 79.62 (7.57) | −0.52 | 0.60 |
| Hemoglobin, gr/dL | 13.59 (1.47) | 13.65 (1.69) | −0.20 | 0.84 |
| Creatinine, mg/dL | 1.69 (3.79) | 0.89 (0.21) | 1.39 | 0.17 |
| BUN, mg/dL | 18.55 (7.21) | 18.39 (5.47) | 0.11 | 0.91 |
| Near-Zero Group (n = 44) | PPV Group (n = 44) | t or χ2 | p | |
|---|---|---|---|---|
| Duration of surgery, min | 154.16 ± 44.25 | 170.82 ± 46.38 | −1.72 | 0.09 |
| Duration of OLV, min | 121.66 ± 38.73 | 137.29 ± 41.79 | −1.82 | 0.07 |
| Blood loss, mL | 52.50 ± 104.97 | 47.27 | 0.27 | 0.79 |
| Crystalloids, mL | 890 ± 459.31 | 1145 ± 470.21 | −2.57 | 0.01 |
| Colloids, mL | 18.18 ± 94.68 | 162.50 ± 278.31 | −3.26 | 0.002 |
| RBC units, n | 0 | 0 | - | - |
| Urine output, mL | 324.54 ± 222.63 | 357.95 ± 233.14 | −0.69 | 0.49 |
| Hypotensive events | 2.14 ± 2.16 | 1.48 ± 1.87 | 1.53 | 0.13 |
| Noradrenaline use, Y/N | 8/36 | 7/37 | 0.08 | 0.78 |
| Extubation time, min | 12.70 ± 4.77 | 12.41 ± 4.64 | 0.29 | 0.77 |
| PONV, Y/N | 1/43 | 2/42 | 0.34 | 0.56 |
| NPRS | 1.89 ± 1.79 | 1.41 ± 1.47 | 1.35 | 0.17 |
| PPCs, Y/N | 9/35 | 7/37 | 0.31 | 0.58 |
| LOS, days | 4.25 ± 1.83 | 4.25 ± 1.59 | 0.00 | 1.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Punzo, G.; Beccia, G.; Cambise, C.; Iacobucci, T.; Sessa, F.; Sgreccia, M.; Sacco, T.; Leone, A.; Congedo, M.T.; Meacci, E.; et al. Goal-Directed Fluid Therapy Using Pulse Pressure Variation in Thoracic Surgery Requiring One-Lung Ventilation: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 5589. https://doi.org/10.3390/jcm13185589
Punzo G, Beccia G, Cambise C, Iacobucci T, Sessa F, Sgreccia M, Sacco T, Leone A, Congedo MT, Meacci E, et al. Goal-Directed Fluid Therapy Using Pulse Pressure Variation in Thoracic Surgery Requiring One-Lung Ventilation: A Randomized Controlled Trial. Journal of Clinical Medicine. 2024; 13(18):5589. https://doi.org/10.3390/jcm13185589
Chicago/Turabian StylePunzo, Giovanni, Giovanna Beccia, Chiara Cambise, Tiziana Iacobucci, Flaminio Sessa, Mauro Sgreccia, Teresa Sacco, Angela Leone, Maria Teresa Congedo, Elisa Meacci, and et al. 2024. "Goal-Directed Fluid Therapy Using Pulse Pressure Variation in Thoracic Surgery Requiring One-Lung Ventilation: A Randomized Controlled Trial" Journal of Clinical Medicine 13, no. 18: 5589. https://doi.org/10.3390/jcm13185589
APA StylePunzo, G., Beccia, G., Cambise, C., Iacobucci, T., Sessa, F., Sgreccia, M., Sacco, T., Leone, A., Congedo, M. T., Meacci, E., Margaritora, S., Sollazzi, L., & Aceto, P. (2024). Goal-Directed Fluid Therapy Using Pulse Pressure Variation in Thoracic Surgery Requiring One-Lung Ventilation: A Randomized Controlled Trial. Journal of Clinical Medicine, 13(18), 5589. https://doi.org/10.3390/jcm13185589






