Return to Work Following Anterior Lumbar Interbody Fusion with Percutaneous Posterior Pedicle Fixation: A Retrospective Analysis from Two Academic Centers in Germany
Abstract
1. Introduction
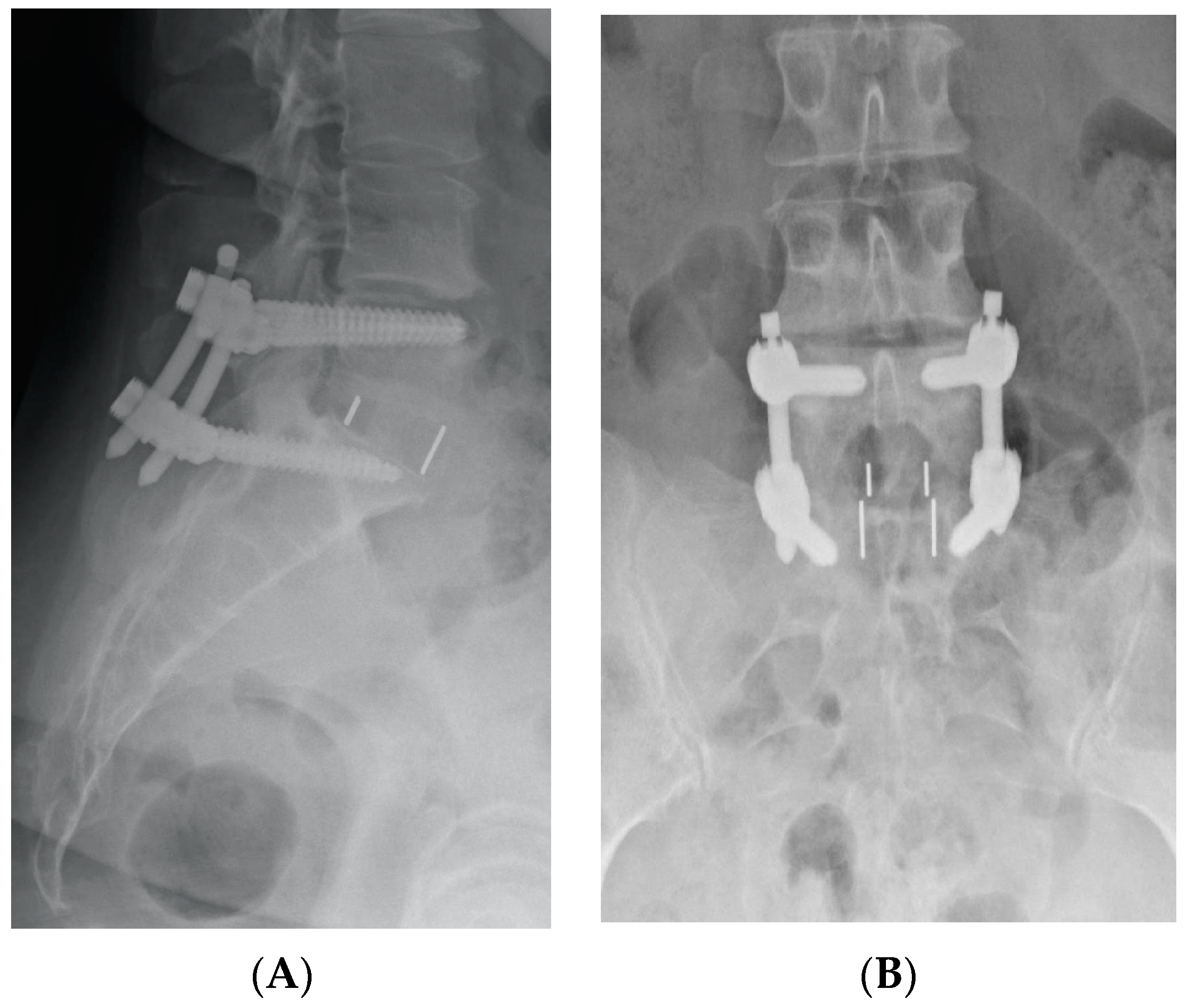
2. Materials and Methods
- Age: 18–65 years.
- Spine pathology: degenerative disc disease, trauma, infection.
- Affected levels: 1 and 2 levels.
- At least 1 year follow-up.
- Patients with no significant mental impairments that could interfere with their ability to participate in the study and participate in a postoperative telephone interview were included.
- A detailed interview guide with scripted questions was developed to ensure all participants were asked the same questions in the same order. This minimized interviewer bias and ensured comprehensive coverage of relevant topics.
- Uniform instructions were provided to all participants at the beginning of the interview, explaining the purpose, duration, and guidelines. Interviewers were trained to avoid leading questions to prevent bias.
- A standardized form was used for recording responses, ensuring consistent data capture.
- At the end of the questionnaire, patients could answer free-text questions and add comments on difficulties encountered during their postoperative recovery.
Statistical Analysis
- Mann–Whitney U: The test was used for comparing two independent groups on ordinal or non-normally distributed continuous variables. This nonparametric test was selected as it does not assume a normal distribution of data.
- Kruskal–Wallis tests: These were employed for data that did not follow a normal distribution.
- The Shapiro–Wilk test: This test was conducted to test the normality of data distributions. Nonparametric tests were employed where data deviated from normality, as these tests do not rely on assumptions of normal distribution.
3. Results
3.1. Patients Enrollment
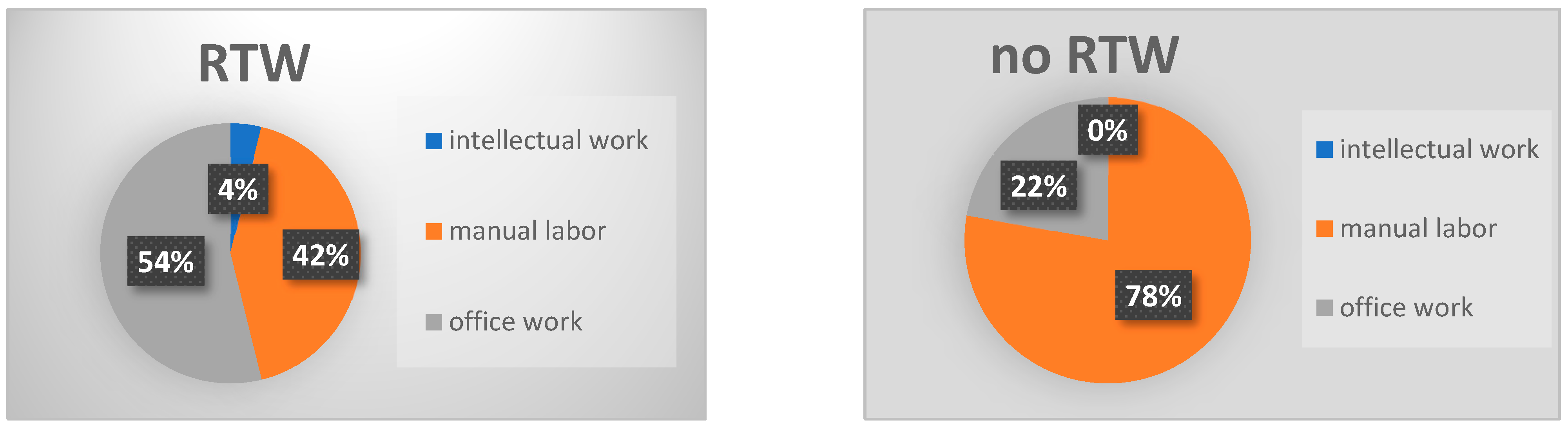
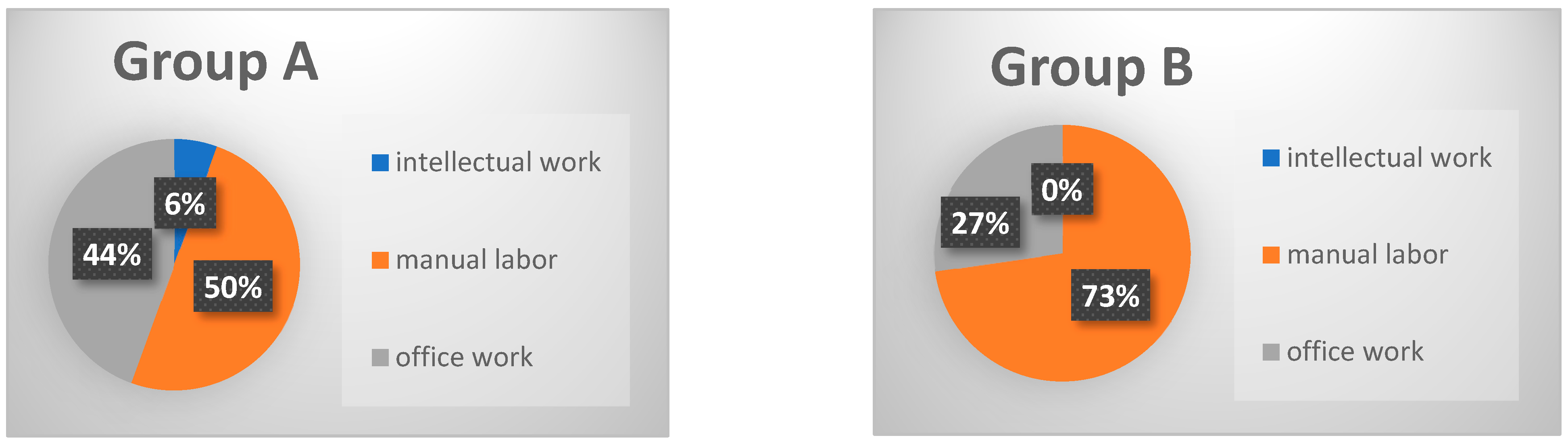
3.2. Return to Work
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [PubMed]
- Andersson, G.B. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef] [PubMed]
- Patrick, N.; Emanski, E.; Knaub, M.A. Acute and chronic low back pain. Med. Clin. N. Am. 2014, 98, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.I.; Mirza, S.K.; Spina, N.; Spiker, W.R.; Lawrence, B.; Brodke, D.S. Trends in Lumbar Fusion Procedure Rates and Associated Hospital Costs for Degenerative Spinal Diseases in the United States, 2004 to 2015. Spine 2019, 44, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Rajaee, S.S.; Bae, H.W.; Kanim, L.E.A.; Delamarter, R.B. Spinal fusion in the United States: Analysis of trends from 1998 to 2008. Spine 2012, 37, 67–76. [Google Scholar] [CrossRef]
- Mummaneni, P.V.; Haid, R.W.; Rodts, G.E. Lumbar interbody fusion: State-of-the-art technical advances. J. Neurosurg. Spine 2004, 1, 24–30. [Google Scholar] [CrossRef]
- Malham, G.M.; Parker, R.M.; Ellis, N.J.; Blecher, C.M.; Chow, F.Y.; Claydon, M.H. Anterior lumbar interbody fusion using recombinant human bone morphogenetic protein-2: A prospective study of complications. J. Neurosurg. Spine 2014, 21, 851–860. [Google Scholar] [CrossRef]
- Rao, P.J.; Maharaj, M.M.; Phan, K.; Lakshan Abeygunasekara, M.; Mobbs, R.J. Indirect foraminal decompression after anterior lumbar interbody fusion: A prospective radiographic study using a new pedicle-to-pedicle technique. Spine J. 2015, 15, 817–824. [Google Scholar] [CrossRef]
- Mobbs, R.J.; Phan, K.; Daly, D.; Rao, P.J.; Lennox, A. Approach-Related Complications of Anterior Lumbar Interbody Fusion: Results of a Combined Spine and Vascular Surgical Team. Glob. Spine J. 2016, 6, 147–154. [Google Scholar] [CrossRef]
- Hsieh, P.C.; Koski, T.R.; O’Shaughnessy, B.A.; Sugrue, P.; Salehi, S.; Ondra, S.; Liu, J.C. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: Implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J. Neurosurg. Spine 2007, 7, 379–386. [Google Scholar] [CrossRef]
- Ajiboye, R.M.; Alas, H.; Mosich, G.M.; Sharma, A.; Pourtaheri, S. Radiographic and Clinical Outcomes of Anterior and Transforaminal Lumbar Interbody Fusions: A Systematic Review and Meta-analysis of Comparative Studies. Clin. Spine Surg. 2018, 31, E230–E238. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Rogers, P.; Rao, P.J.; Mobbs, R.J. Influence of Obesity on Complications, Clinical Outcome, and Subsidence After Anterior Lumbar Interbody Fusion (ALIF): Prospective Observational Study. World Neurosurg. 2017, 107, 334–341. [Google Scholar] [CrossRef]
- Singh, S.; McIntosh, G.; Dea, N.; Hall, H.; Paquet, J.; Abraham, E.; Bailey, C.S.; Weber, M.H.; Johnson, M.G.; Nataraj, A.; et al. Effects of Workload on Return to Work After Elective Lumbar Spine Surgery. Glob. Spine J. 2024, 14, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Chen, C.; Jiang, J.; Zhou, L. Predictors of return to work after spinal surgery: Systematic review and Meta-analysis. J. Orthop. Surg. Res. 2024, 19, 504. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Borgman, B.; Vertuani, S.; Nilsson, J. A systematic literature review of time to return to work and narcotic use after lumbar spinal fusion using minimal invasive and open surgery techniques. BMC Health Serv. Res. 2017, 17, 446. [Google Scholar] [CrossRef] [PubMed]
- Halicka, M.; Duarte, R.; Catherall, S.; Maden, M.; Coetsee, M.; Wilby, M.; Brown, C. Systematic Review and Meta-Analysis of Predictors of Return to Work After Spinal Surgery for Chronic Low Back and Leg Pain. J. Pain 2022, 23, 1318–1342. [Google Scholar] [CrossRef]
- Singh, S.; Ailon, T.; McIntosh, G.; Dea, N.; Paquet, J.; Abraham, E.; Bailey, C.S.; Weber, M.H.; Johnson, M.G.; Nataraj, A.; et al. Time to return to work after elective lumbar spine surgery. J. Neurosurg. Spine 2022, 36, 168–176. [Google Scholar] [CrossRef]
- Lee, Y.-P.; Farhan, S.-D.; Kiester, D.; Rosen, C.; Pendi, A.; Bhatia, N. Variables Affecting Return to Work After Spinal Surgery in a Non-workers’ Compensation Population: A Retrospective Cohort Study. J. Am. Acad. Orthop. Surg. 2017, 25, e282–e288. [Google Scholar] [CrossRef]
- Brooks, R. EuroQol: The current state of play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Buchholz, I.; Janssen, M.F.; Kohlmann, T.; Feng, Y.-S. A Systematic Review of Studies Comparing the Measurement Properties of the Three-Level and Five-Level Versions of the EQ-5D. PharmacoEconomics 2018, 36, 645–661. [Google Scholar] [CrossRef]
- Claudia Gaspar, D.H. Bedeutung der Arbeit Ein Kooperationsprojekt von GfK Verein und Bertelsmann Stiftung. Master’s Thesis, University of Applied Sciences, Vienna, Austria, 2015. [Google Scholar]
- Stergiou-Kita, M.; Grigorovich, A.; Tseung, V.; Milosevic, E.; Hebert, D.; Phan, S.; Jones, J. Qualitative meta-synthesis of survivors’ work experiences and the development of strategies to facilitate return to work. J. Cancer Surviv. 2014, 8, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, F.; Setzer, M.; Prinz, V.; Jussen, D.; Marquardt, G.; Gessler, F.; Czabanka, M.; Freiman, T.; Dubinski, D.; Won, S.-Y.; et al. The Beneficial Effect of Preoperative Exercise on Postoperative Clinical Outcome, Quality of Life and Return to Work after Microsurgical Resection of Spinal Meningiomas. J. Clin. Med. 2023, 12, 2804. [Google Scholar] [CrossRef] [PubMed]
- Behmanesh, B.; Gessler, F.; Won, S.-Y.; Dubinski, D.; Quick-Weller, J.; Imoehl, L.; Seifert, V.; Marquardt, G. Return to work and clinical outcome after surgical treatment and conservative management of patients with intramedullary spinal cord ependymoma. Sci. Rep. 2020, 10, 2335. [Google Scholar] [CrossRef] [PubMed]
- Liedberg, G.M.; Björk, M.; Dragioti, E.; Turesson, C. Qualitative Evidence from Studies of Interventions Aimed at Return to Work and Staying at Work for Persons with Chronic Musculoskeletal Pain. J. Clin. Med. 2021, 10, 1247. [Google Scholar] [CrossRef]
- Crandall, D.; Schmidt, K.; Revella, J.; Chang, M.; Datta, J.; Crowder, T.; McLemore, R. Primary Versus Revision Spine Surgery: Long-Term Work Status and Outcomes. Spine J. 2011, 11, S48–S49. [Google Scholar] [CrossRef]
- Asher, A.L.; Devin, C.J.; Archer, K.R.; Chotai, S.; Parker, S.L.; Bydon, M.; Nian, H.; Harrell, F.E.; Speroff, T.; Dittus, R.S.; et al. An analysis from the Quality Outcomes Database, Part 2. Predictive model for return to work after elective surgery for lumbar degenerative disease. J. Neurosurg. Spine 2017, 27, 370–381. [Google Scholar] [CrossRef]
- Heo, M.; Allison, D.B.; Faith, M.S.; Zhu, S.; Fontaine, K.R. Obesity and Quality of Life: Mediating Effects of Pain and Comorbidities. Obes. Res. 2003, 11, 209–216. [Google Scholar] [CrossRef]
- Ford, E.S.; Moriarty, D.G.; Zack, M.M.; Mokdad, A.H.; Chapman, D.P. Self-Reported Body Mass Index and Health-Related Quality of Life: Findings from the Behavioral Risk Factor Surveillance System. Obes. Res. 2001, 9, 21–31. [Google Scholar] [CrossRef]
- Fosdahl, M.A.; Berg, B.; Risberg, M.A.; Øiestad, B.E.; Holm, I. Body Mass Index, Quality of Life and Activity Limitation Trajectories over 2 Years in Patients with Knee or Hip Osteoarthritis: A Dual Trajectory Approach Based on 4265 Patients Included in the AktivA Quality Register. J. Clin. Med. 2023, 12, 7094. [Google Scholar] [CrossRef]
- Bakbergenuly, I.; Hoaglin, D.C.; Kulinskaya, E. Methods for estimating between-study variance and overall effect in meta-analysis of odds ratios. Res. Synth. Methods 2020, 11, 426–442. [Google Scholar] [CrossRef]
- Schade, V.; Semmer, N.; Main, C.J.; Hora, J.; Boos, N. The impact of clinical, morphological, psychosocial and work-related factors on the outcome of lumbar discectomy. Pain 1999, 80, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.-C.; Öhrvik, J.; Söderlund, A. Associations among pain, disability and psychosocial factors and the predictive value of expectations on returning to work in patients who undergo lumbar disc surgery. Eur. Spine J. 2016, 25, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Clifford, K.; Woodfield, J.C.; Tait, W.; Campbell, H.A.; Baldi, J.C. Association of Preoperative High-Intensity Interval Training With Cardiorespiratory Fitness and Postoperative Outcomes Among Adults Undergoing Major Surgery. JAMA Netw. Open 2023, 6, e2320527. [Google Scholar] [CrossRef] [PubMed]
- Pillastrini, P.; Ferrari, S.; Rattin, S.; Cupello, A.; Villafañe, J.H.; Vanti, C. Exercise and tropism of the multifidus muscle in low back pain: A short review. J. Phys. Ther. Sci. 2015, 27, 943–945. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Romero, E.A.; Alonso Pérez, J.L.; Muñoz Fernández, A.C.; Battaglino, A.; Castaldo, M.; Cleland, J.A.; Villafañe, J.H. Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain. Diagnostics 2021, 11, 632. [Google Scholar] [CrossRef]
- Castaldo, M.; Ge, H.-Y.; Chiarotto, A.; Villafane, J.H.; Arendt-Nielsen, L. Myofascial trigger points in patients with whiplash-associated disorders and mechanical neck pain. Pain Med. 2014, 15, 842–849. [Google Scholar] [CrossRef]
- Hartman, T.J.; Nie, J.W.; MacGregor, K.R.; Oyetayo, O.O.; Zheng, E.; Singh, K. Correlation of mental health with physical function, pain, and disability following anterior lumbar interbody fusion. Acta Neurochir. 2023, 165, 341–349. [Google Scholar] [CrossRef]

| Group A | ||||||
|---|---|---|---|---|---|---|
| RTW | NO RTW | p < 0.05 | Group A | Group B | p < 0.05 | |
| N | 27 | 9 | 36 | 33 | 0.0001 | |
| Median age in yrs | 44 | 51.5 | 0.4 | 50 | 60 | 0.0001 |
| Sex, female, no. (%) | 16 (59) | 7 (77.8) | 0.4 | 23 (63.9) | 17 (51.5) | 0.3 |
| Previous spine surgery, no. (%) | 13 (48) | 5 (55.5) | 0.9 | 14 (47.2) | 19 (57.6) | 0.5 |
| Smoking, no. (%) | 10 (37) | 7 (77.8) | 0.05 | 17 (47.2) | 13 (39.4) | 0.6 |
| Coronary heart disease, no. (%) | 0 | 0 | 0 | 5 (15.2) | 0.02 | |
| Arterial hypertension, no. (%) | 7 (26) | 3 (33.3) | 0.9 | 10 (27.8) | 22 (66.7) | 0.0007 |
| Obesity, no. (%) | 7 (26) | 5 (55.5) | 0.2 | 12 (33.3) | 16 (48.5) | 0.2 |
| Diabetes mellitus, no. (%) | 3 (11) | 1 (11.1) | 0.9 | 4 (11.1) | 5 (15.2) | 0.7 |
| Immunosuppression, no. (%) | 0 | 0 | 0 | 3 (9.1) | 0.1 | |
| Alcohol abuse, no. (%) | 4 (15) | 1 (11.1) | 0.9 | 5 (13.9) | 2 (6.1) | 0.4 |
| Cancer, no. (%) | 0 | 0 | 0 | 3 (9.1) | 0.1 | |
| Operations on the musculoskeletal system, no. (%) | 1 (4) | 3 (33.3) | 0.04 | 4 (11.1) | 11 (33.3) | 0.04 |
| Pulmonary disease, no. (%) | 2 (7) | 1 (11.1) | 1.0 | 3 (8.3) | 7 (21.2) | 0.2 |
| Sports activity, no. (%) | 17 (63) | 4 (44.4) | 0.4 | 21 (58.3) | 14 (42.4) | 0.3 |
| Postoperative rehabilitation (%) | 26 (96) | 9 (100) | 1.0 | 35 (97) | 33 (100) | 1.0 |
| Disability pension | 0 | 27 (81.8) | 0.0001 | |||
| Group A | ||||||
|---|---|---|---|---|---|---|
| RTW | NO RTW | p-Value | Group A | Group B | p-Value | |
| N | 27 | 9 | 36 | 33 | ||
| Indication for surgery | ||||||
| Degenerative spine disease, no. (%) | 20 (74) | 9 (100) | 0.1 | 29 (80.6) | 30 (90.9) | 0.3 |
| Infection, no. (%) | 6 (22) | 0 | 0.3 | 6 (16.7) | 3 (9.1) | 0.5 |
| Trauma, no. (%) | 1 (4) | 0 | 1.0 | 1 (2.8) | 1 (3.0) | |
| >1 Segment fused, no. (%) | 6 (22) | 3 (33.3) | 0.6 | 9 (25) | 13 (39.4) | 0.3 |
| Median duration of surgery in min. | 137 | 152 | 0.5 | 137 | 165 | 0.4 |
| Median preoperative segmental lordosis (°) | 17 | 21 | 0.2 | 18 | 18.6 | 0.2 |
| Median postoperative segmental lordosis (°) | 23 | 26 | 0.5 | 25 | 24.4 | 0.1 |
| Median preoperative L1-S1 LL (°) | 52 | 46 | 0.6 | 49 | 47.9 | 0.06 |
| Median postoperative L1-S1 LL (°) | 52 | 48 | 0.9 | 50.4 | 49 | 0.4 |
| Group A | |||||||
|---|---|---|---|---|---|---|---|
| EQ-5D-3L | Problem | RTW | NO RTW | p-Value | Group A | Group B | p-Value |
| Mobility, no. (%) | No problem | 15 (65) | 0 | 0.009 | 15 (41.7) | 4 (12.1) | 0.01 |
| Moderate problem | 9 (33) | 5 (55.5) | 14 (38.9) | 17 (51.5) | |||
| Extreme problem | 3 (11) | 4 (44.4) | 7 (17.4) | 12 (36.4) | |||
| Self-care, no. (%) | No problem | 26 (96) | 8 (88.9) | 0.7 | 34 (34.4) | 22 (66.7) | 0.04 |
| Moderate problem | 1 (4) | 1 (11.1) | 2 (5.6) | 9 (27.3) | |||
| Extreme problem | 0 | 0 | 0 | 2 (6.1) | |||
| Usual activity, no. (%) | No problem | 20 (74) | 0 | 0.002 | 20 (55.6) | 10 (30.3) | 0.05 |
| Moderate problem | 4 (15) | 6 (66.6) | 10 (27.8) | 15 45.5) | |||
| Extreme problem | 3 (11) | 3 (33.3) | 6 (16.7) | 8 (24.2) | |||
| Pain/discomfort, no. (%) | No problem | 10 (37) | 0 | 0.03 | 10 (27.8) | 4 (12.1) | 0.3 |
| Moderate problem | 13 (48) | 4 (44.4) | 17 (47.2) | 20 (60.6) | |||
| Extreme problem | 4 (15) | 5 (55.5) | 9 (25) | 9 (27.3) | |||
| Anxiety/stress, no. (%) | No problem | 21 (78) | 4 (44.4) | 0.2 | 25 (69.4) | 17 51.5) | 0.1 |
| Moderate problem | 3 (11) | 5 (55.5) | 8 (22.3) | 10 (30.3) | |||
| Extreme problem | 3 (11) | 0 | 3 (8.3) | 6 (18.2) | |||
| EQ VAS | 80 | 55 | 0.002 | 70 | 50 | 0.02 | |
| ODI | 12 | 50 | 0.0006 | 22 | 36 | 0.009 | |
| NRS back pain | 3 | 6.5 | 0.002 | 3 | 5 | 0.006 | |
| NRS leg pain | 0 | 6.5 | 0.003 | 2 | 3 | 0.1 | |
| Self-reported satisfaction | 25 (92.5) | 6 (66.6) | 0.009 | 31 (86.1) | 28 (84.8) | 1.0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Behmanesh, B.; Wempe, H.; Kilinc, F.; Dubinski, D.; Won, S.-Y.; Czabanka, M.; Setzer, M.; Schuss, P.; Schneider, M.; Freiman, T.; et al. Return to Work Following Anterior Lumbar Interbody Fusion with Percutaneous Posterior Pedicle Fixation: A Retrospective Analysis from Two Academic Centers in Germany. J. Clin. Med. 2024, 13, 5636. https://doi.org/10.3390/jcm13185636
Behmanesh B, Wempe H, Kilinc F, Dubinski D, Won S-Y, Czabanka M, Setzer M, Schuss P, Schneider M, Freiman T, et al. Return to Work Following Anterior Lumbar Interbody Fusion with Percutaneous Posterior Pedicle Fixation: A Retrospective Analysis from Two Academic Centers in Germany. Journal of Clinical Medicine. 2024; 13(18):5636. https://doi.org/10.3390/jcm13185636
Chicago/Turabian StyleBehmanesh, Bedjan, Helen Wempe, Fatma Kilinc, Daniel Dubinski, Sae-Yeon Won, Marcus Czabanka, Matthias Setzer, Patrick Schuss, Matthias Schneider, Thomas Freiman, and et al. 2024. "Return to Work Following Anterior Lumbar Interbody Fusion with Percutaneous Posterior Pedicle Fixation: A Retrospective Analysis from Two Academic Centers in Germany" Journal of Clinical Medicine 13, no. 18: 5636. https://doi.org/10.3390/jcm13185636
APA StyleBehmanesh, B., Wempe, H., Kilinc, F., Dubinski, D., Won, S.-Y., Czabanka, M., Setzer, M., Schuss, P., Schneider, M., Freiman, T., & Gessler, F. (2024). Return to Work Following Anterior Lumbar Interbody Fusion with Percutaneous Posterior Pedicle Fixation: A Retrospective Analysis from Two Academic Centers in Germany. Journal of Clinical Medicine, 13(18), 5636. https://doi.org/10.3390/jcm13185636








