Development of a Risk Predictive Model for Erectile Dysfunction at 12 Months after COVID-19 Recovery: A Prospective Observational Study
Abstract
1. Introduction
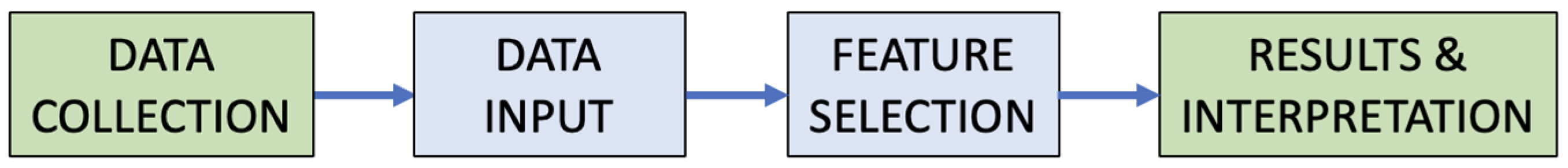
2. Materials and Methods
2.1. Study Design
2.2. Outcomes
2.3. Data Collection
2.4. Data Analysis
2.4.1. Test of Proportions
- p = proportion of the sample
- x1 = success in the no past history of COVID-19 cohort
- x2 = success in the past history of COVID-19 cohort
- n1 = observations in the no past history of COVID-19 cohort
- n2 = observations in the past history of COVID-19 cohort
2.4.2. Regression Model
3. Results
3.1. Descriptive Analysis
3.2. Test of Proportions
3.3. Regression Model
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldstein, I.; Goren, A.; Li, V.W.; Tang, W.Y.; Hassan, T.A. Epidemiology update of erectile dysfunction in eight countries with high burden. Sex. Med. Rev. 2020, 8, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Aytac, I.A.; Mckinlay, J.B.; Krane, R.J. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999, 84, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Zhao, L.; Wu, H.; Cao, M.; Jiang, H. Sexual life and medication taking behaviours in young men: An online survey of 92620 respondents in China. Int. J. Clin. Pract. 2020, 74, e13417. [Google Scholar] [CrossRef]
- Rojanasarot, S.; Bhattacharyya, S.K.; Burnett, A.L. Cost of lost productivity due to erectile dysfunction and impact of employer benefit exclusion of penile prosthesis implantation treatment. J. Occup. Environ. Med. 2022, 64, 403–408. [Google Scholar] [CrossRef]
- Lamers, M.M.; Haagmans, B.L. SARS-CoV-2 pathogenesis. Nat. Rev. Microbiol. 2022, 20, 270–284. [Google Scholar] [CrossRef] [PubMed]
- Qu, G.; Zhen, Q.; Wang, W.; Fan, S.; Wu, Q.; Zhang, C.; Li, B.; Liu, G.; Yu, Y.; Li, Y.; et al. Health-related quality of life of COVID-19 patients after discharge: A multicentre follow-up study. J. Clin. Nurs. 2021, 30, 1742–1750. [Google Scholar] [CrossRef]
- Tamayo-Velasco, Á.; Bombín-Canal, C.; Cebeira, M.J.; Sánchez-De Prada, L.; Miramontes-González, J.P.; Martin-Fernández, M.; Peñarrubia-Ponce, M.J. Full characterisation of thrombotic events in all hospitalised COVID-19 patients in a Spanish tertiary hospital during the first 18 months of the pandemic. J. Clin. Med. 2022, 11, 3443. [Google Scholar] [CrossRef]
- Tamayo-Velasco, Á.; Martínez-Paz, P.; Peñarrubia-Ponce, M.J.; de la Fuente, I.; Pérez-Gonzalez, S.; Fernandez, I.; Dueñas, C.; Gómez-Sánchez, E.; Lorenzo-López, M.; Gómez-Pesquera, E.; et al. HGF, IL-1α, and IL-27 are robust biomarkers in early severity stratification of COVID-19 patients. J. Clin. Med. 2021, 10, 2017. [Google Scholar] [CrossRef]
- Stylianou, T.; Ntelas, K. Impact of COVID-19 pandemic on mental health and socioeconomic aspects in Greece. Int. J. Environ. Res. Public Health 2023, 20, 1843. [Google Scholar] [CrossRef]
- Yong, S.J. Long COVID or post-COVID-19 syndrome: Putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef]
- Iba, T.; Levy, J.H. Thrombosis and thrombocytopenia in COVID-19 and after COVID-19 vaccination. Trends Cardiovasc. Med. 2022, 32, 249–256. [Google Scholar] [CrossRef]
- Sansone, A.; Mollaioli, D.; Ciocca, G.; Colonnello, E.; Limoncin, E.; Balercia, G.; Jannini, E.A. “Mask up to keep it up”: Preliminary evidence of the association between erectile dysfunction and COVID-19. Andrology 2021, 9, 1053–1059. [Google Scholar] [CrossRef]
- Hebert, K.J.; Matta, R.; Horns, J.J.; Paudel, N.; Das, R.; McCormick, B.J.; Myers, J.B.; Hotaling, J.M. Prior COVID-19 infection associated with increased risk of newly diagnosed erectile dysfunction. Int. J. Impot. Res. 2023, 36, 521–525. [Google Scholar] [CrossRef]
- Zhang, J.; Shi, W.; Zou, M.; Zeng, Q.; Feng, Y.; Luo, Z.; Gan, H. Prevalence and risk factors of erectile dysfunction in COVID-19 patients: A systematic review and meta-analysis. J. Endocrinol. Investig. 2023, 46, 795–804. [Google Scholar] [CrossRef] [PubMed]
- Gök, A.; Altan, M.; Dogan, A.E.; Eraslan, A.; Uysal, F.S.; Öztürk, U.; Saguner, A.M.; İmamoğlu, M.A. Does post-COVID-19 erectile dysfunction improve over time? J. Clin. Med. 2023, 12, 1241. [Google Scholar] [CrossRef] [PubMed]
- Maestre-Muñiz, M.M.; Arias, A.; Mata-Vázquez, E.; Martin-Toledano, M.; Lopez-Larramona, G.; Ruiz-Chicote, A.M.; Nieto-Sandoval, B.; Lucendo, A.J. Long-term outcomes of patients with Coronavirus Disease 2019 at one year after hospital discharge. J. Clin. Med. 2021, 10, 2945. [Google Scholar] [CrossRef] [PubMed]
- Jannini, E.A. SM = SM: The interface of systems medicine and sexual medicine for facing non-communicable diseases in a gender-dependent manner. Sex. Med. Rev. 2017, 5, 349–364. [Google Scholar] [CrossRef]
- Rosen, R.C.; Cappelleri, J.C.; Smith, M.D.; Lipsky, J.; Peña, B.M. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int. J. Impot. Res. 1999, 11, 319–326. [Google Scholar] [CrossRef]
- Zhang, K.; Stricker, P.; Löhr, M.; Stehling, M.; Suberville, M.; Cussenot, O.; Lunelli, L.; Ng, C.F.; Teoh, J.; Laguna, P.; et al. A multi-center international study to evaluate the safety, functional and oncological outcomes of irreversible electroporation for the ablation of prostate cancer. Prostate Cancer Prostatic Dis. 2024, 27, 525–530. [Google Scholar] [CrossRef]
- Kim, J.K.; Lee, Y.J.; Kim, H.; Song, S.H.; Jeong, S.J.; Byun, S.S. A prospectively collected observational study of pelvic floor muscle strength and erectile function using a novel personalized extracorporeal perineometer. Sci. Rep. 2021, 11, 18389. [Google Scholar] [CrossRef]
- Inman, B.A.; St Sauver, J.L.; Jacobson, D.J.; Mcgree, M.E.; Nehra, A.; Lieber, M.M.; Roger, V.L.; Jacobsen, S.J. A Population-Based, Longitudinal Study of Erectile Dysfunction and Future Coronary Artery Disease. Mayo Clin. Proc. 2009, 84, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Ho, T.K. Machine learning made easy: A review of scikit-learn package in python programming language. J. Educ. Behav. Stat. 2019, 44, 348–361. [Google Scholar] [CrossRef]
- Kresch, E.; Achua, J.; Saltzman, R.; Khodamoradi, K.; Arora, H.; Ibrahim, E.; Kryvenko, O.N.; Almeida, V.W.; Firdaus, F.; Hare, J.M.; et al. COVID-19 Endothelial Dysfunction Can Cause Erectile Dysfunction: Histopathological, Immunohistochemical, and Ultrastructural Study of the Human Penis. World J. Mens. Health 2021, 39, 466–469. [Google Scholar] [CrossRef]
- Sansone, A.; Mollaioli, D.; Ciocca, G.; Limoncin, E.; Colonnello, E.; Vena, W.; Jannini, E.A. Addressing male sexual and reproductive health in the wake of COVID-19 outbreak. J. Endocrinol. Investig. 2021, 44, 223–231. [Google Scholar] [CrossRef] [PubMed]
- McCabe, M.P.; Sharlip, I.D.; Lewis, R.; Atalla, E.; Balon, R.; Fisher, A.D.; Laumann, E.; Lee, S.W.; Segraves, R.T. Risk factors for sexual dysfunction among women and men: A consensus statement form the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016, 13, 153–167. [Google Scholar] [CrossRef]
- Romero-Rodríguez, E.; Pérula-de Torres, L.Á.; Castro-Jiménez, R.; Gonzalez-Lama, J.; Jimenez-Garcia, C.; Gonzalez-Bernal, J.J.; González-Santos, J.; Vélez-Santamaría, R.; Sánchez-González, E.; Santamaría-Peláez, M. Hospital admission and vaccination as predictive factors of long COVID-19 symptoms. Front. Med. 2022, 9, 1016013. [Google Scholar] [CrossRef]
- Mehta, P.; Chakraborty, A.; Andrabi, S.W.; Sharma, B.; Kumar, R.; Bhaskar, L.V.K.S.; Rajender, S. COVID-19 vaccination does not affect male sexual functions. Reprod. Biol. Endocrinol. 2023, 21, 3. [Google Scholar] [CrossRef]
- Diaz, P.; Zizzo, J.; Blachman-Braun, R.; Gandhi, D.A.; Reddy, R.; Zucker, I.J.; Dullea, A.; Khodamoradi, K.; Ramasamy, R. COVID-19 vaccination not associated with increased risk of erectile dysfunction. Andrologia 2022, 54, e14563. [Google Scholar] [CrossRef]
- Yannas, D.; Frizza, F.; Vignozzi, L.; Corona, G.; Maggi, M.; Rastrelli, G. Erectile dysfunction is a hallmark of cardiovascular disease: Unavoidable matter of fact or opportunity to improve men’s health? J. Clin. Med. 2021, 10, 2221. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Map-Johns Hopkins Coronavirus Resource Centre [Internet]. Available online: https://coronavirus.jhu.edu/map.html (accessed on 21 May 2024).
- Ghasemiyeh, P.; Mohammadi-Samani, S. Lessons we learned during the past four challenging years in the COVID-19 era: Pharmacotherapy, long COVID complications, and vaccine development. Virol. J. 2024, 21, 98. [Google Scholar] [CrossRef]
- Hu, X.; Hu, Z.; Xu, T.; Zhang, K.; Lu, H.H.; Zhao, J.; Boerwinkle, E.; Jin, L.; Xiong, M. Equilibrium points and their stability of COVID-19 in US. Sci. Rep. 2024, 14, 1628. [Google Scholar] [CrossRef] [PubMed]

| Factor 1/Factor 2 | Variable to Predict | |
|---|---|---|
| Ed | ||
| Model | Logistic Regression for Selection of 5 Attributes | AUC, ROC |
| … | … | |
| Logistic Regression for Selection of 40 Attributes | AUC, ROC | |
| Variable | History of COVID-19 | |
|---|---|---|
| No (n = 195) | Yes (n = 166) | |
| Age (year, interquartile range) | 55 (15) | 55 (14) |
| BMI (kg/m2, interquartile range) | 26.3 (5) | 28 (6) |
| Smoking (case, %) | 94 (48.5) | 100 (51.5) |
| Pack-year (pack year, interquartile range) | 18 (14) | 25.5 (25) |
| Ischemic heart disease (case, %) | 5 (25) | 15 (75) |
| Hypertension (case, %) | 45 (44.1) | 57 (55.9) |
| Heart failure (case, %) | 1 (16.7) | 5 (83.3) |
| PAD (case, %) | 4 (50) | 4 (50) |
| Diabetes (case, %) | 10 (33.3) | 20 (66.7) |
| Hypothyroidism (case, %) | 6 (60) | 4 (40) |
| CKD (case, %) | 6 (75) | 2 (25) |
| Cancer (case, %) | 6 (40) | 9 (60) |
| Anxiety/Depression (case, %) | 6 (23.1) | 20 (76.9) |
| Beta blockers (case, %) | 6 (18.8) | 26 (81.3) |
| NOAs (case, %) | 1 (16.7) | 5 (83.3) |
| Antiplatelet therapy (case, %) | 12 (37.5) | 20 (62.5) |
| Erectile dysfunction * (case, %) | 83 (44.1) | 105 (55.9) |
| SARS-CoV-2 vaccination (case, %) | 191 (54.6) | 159 (45.4) |
| Statistic | Values |
|---|---|
| No past history of COVID-19 | 83 |
| Past history of COVID-19 | 105 |
| N No past history of COVID-19 | 193 |
| N past history of COVID-19 cohort | 164 |
| P No past history of COVID-19 % | 43 |
| P Past history of COVID-19 % | 64 |
| N | 357 |
| p-value | 7.4 × 10−5 |
| z-value | −3.9640 |
| Erectile Dysfunction Predictive Model | ||
|---|---|---|
| Index | Variable | |
| 1 | Diabetes | 3.7 |
| 2 | Autoimmune disease | 2.5 |
| 3 | Beta blockers | 2.3 |
| 4 | PAD | 1.8 |
| 5 | Cancer | 1.8 |
| 6 | Hypertension | 1.8 |
| 7 | Stroke | 1.7 |
| 8 | Chronic kidney failure | 1.7 |
| 9 | Acenocumarol | 1.7 |
| 10 | Antiplatelet therapy | 1.5 |
| 11 | Anxiety/Depression | 1.5 |
| 12 | COPD | 1.4 |
| 13 | Alcohol | 1.3 |
| 14 | History of COVID-19 | 1.3 |
| 15 | Hypothyroidism | 1.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Natal Alvarez, F.; Conde Redondo, M.C.; Sierrasesumaga Martin, N.; Garcia Viña, A.; Marfil Peña, C.; Bahillo Martinez, A.; Jojoa, M.; Tamayo Gomez, E. Development of a Risk Predictive Model for Erectile Dysfunction at 12 Months after COVID-19 Recovery: A Prospective Observational Study. J. Clin. Med. 2024, 13, 5757. https://doi.org/10.3390/jcm13195757
Natal Alvarez F, Conde Redondo MC, Sierrasesumaga Martin N, Garcia Viña A, Marfil Peña C, Bahillo Martinez A, Jojoa M, Tamayo Gomez E. Development of a Risk Predictive Model for Erectile Dysfunction at 12 Months after COVID-19 Recovery: A Prospective Observational Study. Journal of Clinical Medicine. 2024; 13(19):5757. https://doi.org/10.3390/jcm13195757
Chicago/Turabian StyleNatal Alvarez, Fernando, Maria Consuelo Conde Redondo, Nicolas Sierrasesumaga Martin, Alejandro Garcia Viña, Carmen Marfil Peña, Alfonso Bahillo Martinez, Mario Jojoa, and Eduardo Tamayo Gomez. 2024. "Development of a Risk Predictive Model for Erectile Dysfunction at 12 Months after COVID-19 Recovery: A Prospective Observational Study" Journal of Clinical Medicine 13, no. 19: 5757. https://doi.org/10.3390/jcm13195757
APA StyleNatal Alvarez, F., Conde Redondo, M. C., Sierrasesumaga Martin, N., Garcia Viña, A., Marfil Peña, C., Bahillo Martinez, A., Jojoa, M., & Tamayo Gomez, E. (2024). Development of a Risk Predictive Model for Erectile Dysfunction at 12 Months after COVID-19 Recovery: A Prospective Observational Study. Journal of Clinical Medicine, 13(19), 5757. https://doi.org/10.3390/jcm13195757






