Unveiling the Heart of the Matter: Echocardiographic Insights into Diastolic Function and Left Ventricular and Atrial Changes in HIV Patients with Controlled Viremia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Echocardiographic Measurements
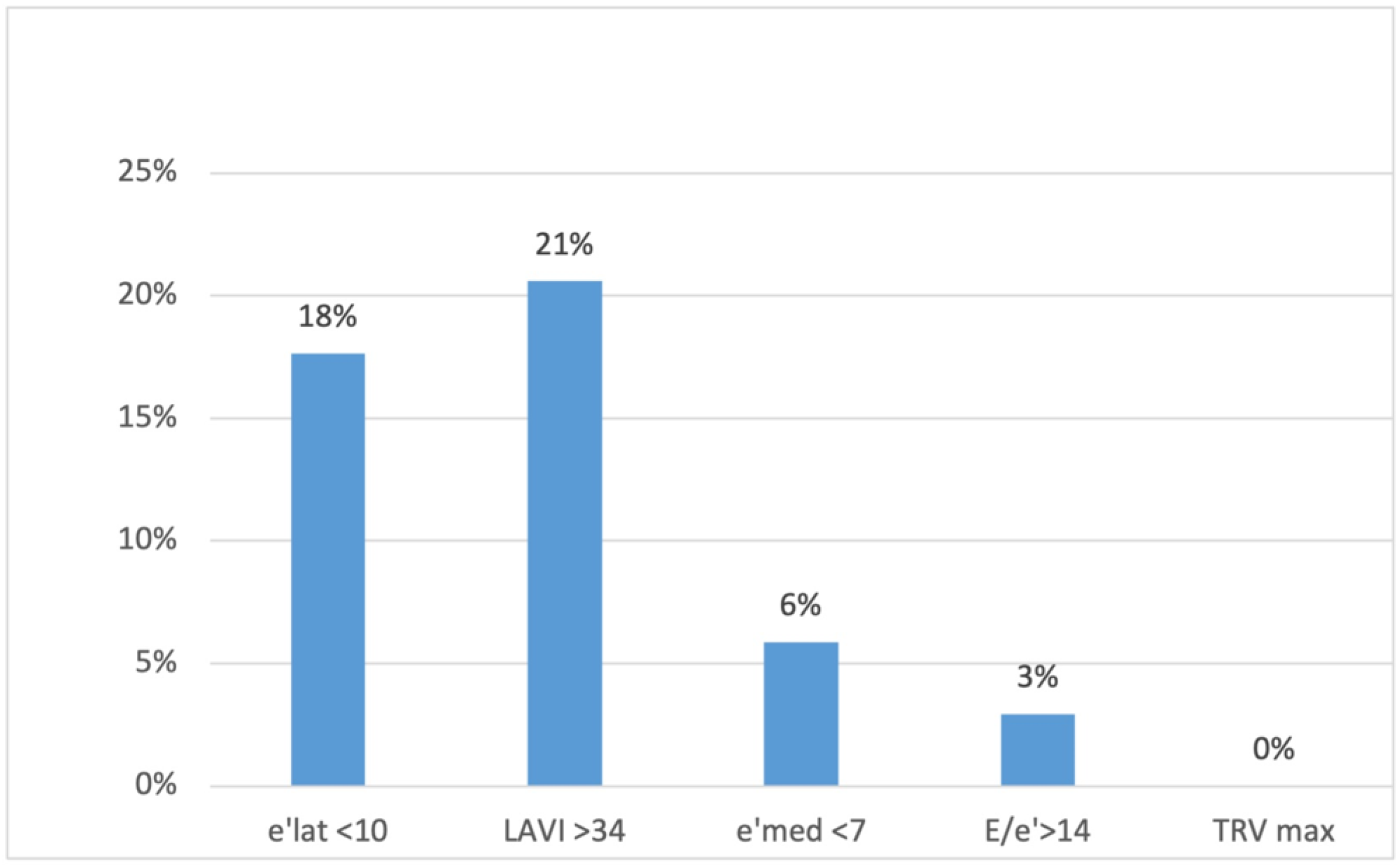
- e′, early annular velocity of a mitral ring in tissue Doppler on the septum (e′ med) and lateral wall (e′ lat) of the left ventricle in four-chamber view (e′ med < 7 cm/s or e′ lat < 10 cm/s);
- Average E/e′ ratio (E, peak early transmitral flow velocity) >14;
- Maximum velocity of tricuspid regurgitation (TR V max) in Doppler >2.8 m/s;
- Left atrial volume index (LAVI, left atrium volume measured in four-chamber and two-chamber views indexed to the body surface) >34 cm3/m2.
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organisation. Available online: https://www.who.int/news-room/fact-sheets/detail/hiv-aids?gclid=CjwKCAjwp8OpBhAFEiwAG7NaErIw024CLNz8EZtzLhc-31J-Pq3mvyJPlqJ3E376-xP40F_SIiZFfBoC9I0QAvD_BwE (accessed on 19 October 2023).
- Trickey, A.; Sabin, C.; Burkholder, G.; Crane, H.; Monforte, A.D.; Egger, M.; Gill, M.J.; Grabar, S.; Guest, J.L.; Jarrin, I.; et al. Life expectancy after 2015 of adults with HIV on long-term antiretroviral therapy in Europe and North America: A collaborative analysis of cohort studies. Lancet HIV 2023, 10, e295–e307. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results; Institute for Health Metrics and Evaluation (IHME): Seattle, WA, USA, 2020; Available online: https://vizhub.healthdata.org/gbd-results/ (accessed on 5 January 2024).
- Shah, A.S.; Stelzle, D.; Lee, K.K.; Beck, E.J.; Alam, S.; Clifford, S.; Longenecker, C.T.; Strachan, F.; Bagchi, S.; Whiteley, W.; et al. Global Burden of Atherosclerotic Cardiovascular Disease in People Living with HIV: Systematic Review and Meta-Analysis. Circulation 2018, 138, 1100–1112. [Google Scholar] [CrossRef] [PubMed]
- Jachymek, M.; Braksator, M.; Parczewski, M.; Peregud-Pogorzelska, M.; Kaźmierczak, J. Cardiovascular disease and HIV infection. HIV AIDS Rev. Int. J. HIV-Related Probl. 2021, 20, 85–89. [Google Scholar] [CrossRef]
- Ntsekhe, M.; Baker, J.V. Cardiovascular Disease among Persons Living with HIV: New Insights into Pathogenesis and Clinical Manifestations in a Global Context. Circulation 2023, 147, 83–100. [Google Scholar] [CrossRef]
- Ruamtawee, W.; Tipayamongkholgul, M.; Aimyong, N.; Manosuthi, W. Prevalence and risk factors of cardiovascular disease among people living with HIV in the Asia-Pacific region: A systematic review. BMC Public Health 2023, 23, 477. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Okeke, N.L.; Craig, D.M.; Muehlbauer, M.J.; Ilkayeva, O.; Clement, M.E.; Naggie, S.; Shah, S.H. Metabolites predict cardiovascular disease events in persons living with HIV: A pilot case–control study. Metabolomics 2018, 14, 23. [Google Scholar] [CrossRef]
- Kingery, J.R.; Goyal, P.; Hosalli, R.; Lee, M.H.; Desderius, B.; Kalokola, F.; Makubi, A.; Fadhil, S.; Kapiga, S.; Karmali, D.; et al. Human Immunodeficiency Virus–Associated Myocardial Diastolic Dysfunction and Soluble ST2 Concentration in Tanzanian Adults: A Cross-Sectional Study. J. Infect. Dis. 2021, 223, 83–93. [Google Scholar] [CrossRef]
- Pan, S.; Bai, J. Factors influencing left ventricular diastolic dysfunction on echocardiography of people living with HIV in Kunming, China. Int. J. STD AIDS 2023, 30, 9564624231204635. [Google Scholar] [CrossRef]
- Freiberg, M.S.; Chang, C.-C.H.; Skanderson, M.; Patterson, O.V.; DuVall, S.L.; Brandt, C.A.; So-Armah, K.A.; Vasan, R.S.; Oursler, K.A.; Gottdiener, J.; et al. Association Between HIV Infection and the Risk of Heart Failure with Reduced Ejection Fraction and Preserved Ejection Fraction in the Antiretroviral Therapy Era: Results from the Veterans Aging Cohort Study. JAMA Cardiol. 2017, 2, 536–546. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Devereux, R.B.; Alonso, D.R.; Lutas, E.M.; Gottlieb, G.J.; Campo, E.; Sachs, I.; Reichek, N. Echocardiographic assessment of left ventricular hypertrophy: Comparison to necropsy findings. Am. J. Cardiol. 1986, 57, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Gaasch, W.H.; Zile, M.R. Left Ventricular Structural Remodeling in Health and Disease: With Special Emphasis on Volume, Mass, and Geometry. J. Am. Coll. Cardiol. 2011, 58, 1733–1740. [Google Scholar] [CrossRef]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F.; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J.—Cardiovasc. Imaging 2016, 17, 1321–1360. [Google Scholar] [CrossRef] [PubMed]
- Okeke, N.L.; Alenezi, F.; Bloomfield, G.S.; Dunning, A.; Clement, M.E.; Shah, S.H.; Naggie, S.; Velazquez, E.J. Determinants of Left Ventricular Hypertrophy and Diastolic Dysfunction in an HIV Clinical Cohort. J. Card. Fail. 2018, 24, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Mondy, K.E.; Gottdiener, J.; Overton, E.T.; Henry, K.; Bush, T.; Conley, L.; Hammer, J.; Carpenter, C.C.; Kojic, E.; Patel, P.; et al. High Prevalence of Echocardiographic Abnormalities among HIV-infected Persons in the Era of Highly Active Antiretroviral Therapy. Clin. Infect. Dis. 2010, 52, 378–386. [Google Scholar] [CrossRef]
- Arodiwe, I.O.; Eke, C.B.; Arodiwe, E.B. Left ventricular hypertrophy in African children infected with HIV/AIDS: A case control study. Pan Afr. Med. J. 2023, 45, 110. [Google Scholar] [CrossRef]
- Zhang, Y.; Qiao, S.; Hao, H.; Li, Q.; Bao, X.; Wang, K.; Gu, R.; Li, G.; Kang, L.; Wu, H.; et al. The predictive value of relative wall thickness on the prognosis of the patients with ST-segment elevation myocardial infarction. BMC Cardiovasc. Disord. 2023, 23, 383. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Shimabukuro, M.; Abe, M.; Arakaki, T.; Arasaki, O.; Ueda, S. Comparison of the prognostic values of three calculation methods for echocardiographic relative wall thickness in acute decompensated heart failure. Cardiovasc. Ultrasound 2019, 17, 30. [Google Scholar] [CrossRef]
- Biton, Y.; Goldenberg, I.; Kutyifa, V.; Baman, J.R.; Solomon, S.; Moss, A.J.; Szepietowska, B.; McNitt, S.; Polonsky, B.; Zareba, W.; et al. Relative Wall Thickness and the Risk for Ventricular Tachyarrhythmias in Patients with Left Ventricular Dysfunction. J. Am. Coll. Cardiol. 2016, 67, 303–312. [Google Scholar] [CrossRef]
- Tezuka, Y.; Iguchi, M.; Hamatani, Y.; Ogawa, H.; Esato, M.; Tsuji, H.; Wada, H.; Hasegawa, K.; Abe, M.; Lip, G.Y.H.; et al. Association of relative wall thickness of left ventricle with incidence of thromboembolism in patients with non-valvular atrial fibrillation: The Fushimi AF Registry. Eur. Heart J.—Qual. Care Clin. Outcomes 2020, 6, 273–283. [Google Scholar] [CrossRef]
- Woldu, B.; Temu, T.M.; Kirui, N.; Christopher, B.; Ndege, S.; Post, W.S.; Kamano, J.; Bloomfield, G.S. Diastolic dysfunction in people with HIV without known cardiovascular risk factors in Western Kenya. Open Heart 2022, 9, e001814. [Google Scholar] [CrossRef] [PubMed]
- Luo, L.; Zeng, Y.; Li, T.; Lv, W.; Wang, H.; Guo, F.; Han, Y.; Xie, J.; Qiu, Z.; Li, Y.; et al. Prospective Echocardiographic Assessment of Cardiac Structure and Function in Chinese Persons Living with HIV. Clin. Infect. Dis. 2014, 58, 1459–1466. [Google Scholar] [CrossRef]
- Hu, X.; Zhang, Y.; Zhang, T.; Li, W.; Han, J.; Zhang, X.; Meng, F. Echocardiographic assessment of left cardiac structure and function in antiretroviral therapy (ART)-naïve people living with HIV/AIDS. Immunity Inflamm. Dis. 2023, 11, e799. [Google Scholar] [CrossRef]
- Wu, K.C.; Haberlen, S.; Plankey, M.W.; Palella, F.J.; Piggott, D.; Kirk, G.D.; Margolick, J.B.; Post, W.S. Human immunodeficiency viral infection and differences in interstitial ventricular fibrosis and left atrial size. Eur. Heart J.—Cardiovasc. Imaging 2021, 22, 888–895. [Google Scholar] [CrossRef] [PubMed]
- Hutchins, E.; Wang, R.; Rahmani, S.; Nakanishi, R.; Haberlen, S.; Kingsley, L.; Witt, M.D.; Palella, F.J.; Jacobson, L.; Budoff, M.J.; et al. HIV Infection Is Associated with Greater Left Ventricular Mass in the Multicenter AIDS Cohort Study. AIDS Res. Hum. Retrovir. 2019, 35, 755–761. [Google Scholar] [CrossRef] [PubMed]
- Krebs-Demmer, L.; Ronit, A.; Sigvardsen, P.; Lebech, A.; Gerstoft, J.; Knudsen, A.; Fuchs, A.; Kühl, J.; Nordestgaard, B.; Kofoed, K.; et al. Cardiac chamber volumes and left ventricular mass in people living with HIV and matched uninfected controls. HIV Med. 2020, 21, 625–634. [Google Scholar] [CrossRef]
- La Fazia, V.M.; Pierucci, N.; Mohanty, S.; Gianni, C.; Della Rocca, D.G.; Compagnucci, P.; MacDonald, B.; Mayedo, A.; Torlapati, P.G.; Bassiouny, M.; et al. Catheter ablation approach and outcome in HIV+ patients with recurrent atrial fibrillation. J. Cardiovasc. Electrophysiol. 2023, 34, 2527–2534. [Google Scholar] [CrossRef]
- Athanasiadi, E.; Bonou, M.; Basoulis, D.; Kapelios, C.J.; Masoura, C.; Skouloudi, M.; Mavrogeni, S.; Aggeli, C.; Psichogiou, M.; Barbetseas, J. Subclinical Left Ventricular Systolic Dysfunction in HIV Patients: Prevalence and Associations with Carotid Atherosclerosis and Increased Adiposity. J. Clin. Med. 2022, 11, 1804. [Google Scholar] [CrossRef]
- Liao, C.-T.; Toh, H.S.; Chang, W.-T.; Yang, C.-T.; Chen, Z.-C.; Tang, H.-J.; Strong, C. Assessment of subclinical cardiac dysfunction by speckle-tracking echocardiography among people living with human immunodeficiency virus. Front. Cardiovasc. Med. 2023, 10, 1200418. [Google Scholar] [CrossRef]

| Inclusion criteria |
| Age 35–50 years Confirmed infection with HIV-1 (molecular method or Western blotting test) Treatment with antiretroviral therapy Undetectable HIV-1 viral load (defined as serum HIV-RNA levels < 50 copies/mL) for at least 6 months before study enrollment |
| Exclusion criteria |
| Prior diagnosis of ischemic heart disease confirmed by coronary angiography Type 2 diabetes mellitus Ineffective antiretroviral therapy (HIV-1 viral load > 50 copies/mL) Low adherence to antiretroviral therapy (<80% in the last year before enrolment in the study, based on the number of packs dispensed) |
| Characteristic | Mean (±SD)/Median (IQR)/N (%) |
|---|---|
| Number of patients | 34 |
| Sex (%men) | 29 (85.3%) |
| Age (years) | 41.2 (±5.95) |
| Weight (kg) | 78.3 (±12.99) |
| Height (m) | 1.75 (±0.07) |
| BMI (kg/m2) | 25.65 (±4.1) |
| Smoking | 12 (35.3%) |
| Antihypertensive drugs | 4 (11.8%) |
| Systolic blood pressure (mmHg) | 135 (±11.4) |
| Time from diagnosis (months) | 135 (±86.9) |
| Total cholesterol (mg/dL) | 176 (±36.01) |
| High-density cholesterol (mg/dL) | 46.2 (39.9–64.1) |
| Non-high-density cholesterol (mg/dL) | 126.5 (±36.9) |
| Baseline CD4+ count (cells/μL) | 406 (191–590) |
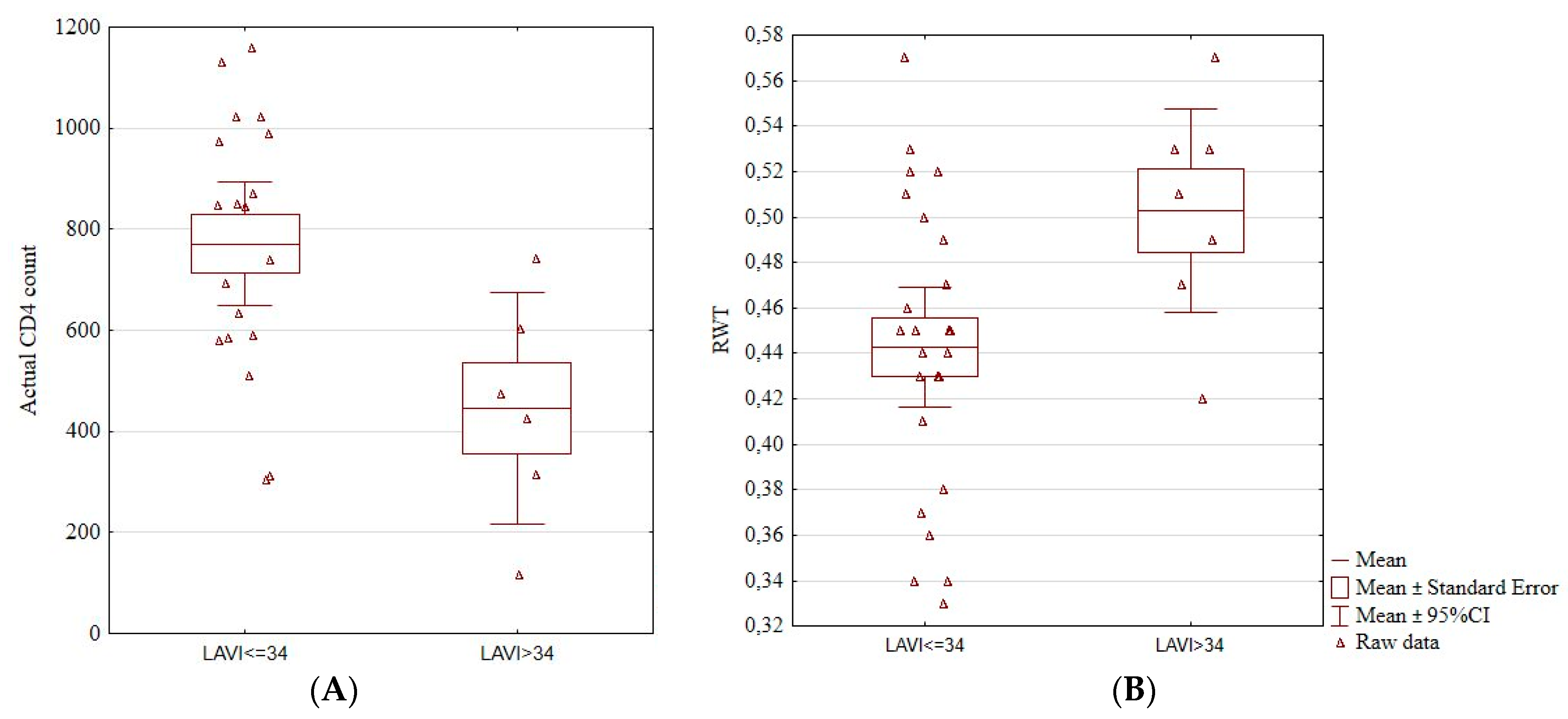
| Actual CD4+ count (cells/μL) | 712 (±291.21) |
| Immunological reconstruction >500 cells/μL | 21 (61.8%) |
| Immunological reconstruction >800 cells/μL | 11 (32.4%) |
| Echocardiographic Measurement | Mean (±SD)/Median (IQR)/N (%) |
|---|---|
| Aortic diameter (mm) | 29 (24–39) |
| Left atrium diameter (mm) | 36.35 (±4.53) |
| IVSd (mm) | 10 (8–15) |
| LVEDD (mm) | 46 (20–58) |
| LVPWd (mm) | 10 (8–13) |
| LVH (n, %) | 1 (2.94%) |
| LVMI (g/m2) | 90.38 (±14.99) |
| RWT | 0.46 (±0.06) |
| Concentric remodeling (n, %) | 26 (76.47%) |
| Left atrium area (cm2) | 16.79 (±3.36) |
| LAVI (cm3/kg) | 27.35 (±7.63) |
| LVEF (%) | 61.3 (57.8–66.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jachymek, M.; Peregud-Pogorzelska, M.; Parczewski, M.; Dembowska, A.; Wójcik, Ł.; Aksak-Wąs, B. Unveiling the Heart of the Matter: Echocardiographic Insights into Diastolic Function and Left Ventricular and Atrial Changes in HIV Patients with Controlled Viremia. J. Clin. Med. 2024, 13, 463. https://doi.org/10.3390/jcm13020463
Jachymek M, Peregud-Pogorzelska M, Parczewski M, Dembowska A, Wójcik Ł, Aksak-Wąs B. Unveiling the Heart of the Matter: Echocardiographic Insights into Diastolic Function and Left Ventricular and Atrial Changes in HIV Patients with Controlled Viremia. Journal of Clinical Medicine. 2024; 13(2):463. https://doi.org/10.3390/jcm13020463
Chicago/Turabian StyleJachymek, Magdalena, Małgorzata Peregud-Pogorzelska, Miłosz Parczewski, Aneta Dembowska, Łukasz Wójcik, and Bogusz Aksak-Wąs. 2024. "Unveiling the Heart of the Matter: Echocardiographic Insights into Diastolic Function and Left Ventricular and Atrial Changes in HIV Patients with Controlled Viremia" Journal of Clinical Medicine 13, no. 2: 463. https://doi.org/10.3390/jcm13020463
APA StyleJachymek, M., Peregud-Pogorzelska, M., Parczewski, M., Dembowska, A., Wójcik, Ł., & Aksak-Wąs, B. (2024). Unveiling the Heart of the Matter: Echocardiographic Insights into Diastolic Function and Left Ventricular and Atrial Changes in HIV Patients with Controlled Viremia. Journal of Clinical Medicine, 13(2), 463. https://doi.org/10.3390/jcm13020463






