Introduction of a Post-Anaesthesia Care Unit in a Teaching Hospital Is Associated with a Reduced Length of Hospital Stay in Noncardiac Surgery: A Single-Centre Interrupted Time Series Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patient Selection
- (1)
- Thyroidectomy
- (2)
- Parathyroidectomy
- (3)
- Video-Assisted Thoracoscopic Surgery (VATS) for (bi)lobectomy
- (4)
- Open (bi)lobectomy
- (5)
- Endovascular aortic repair (EVAR) or Covered Endovascular Reconstruction of Aortic Bifurcation (CERAB)
- (6)
- Laparoscopic colonic or rectal resection
- (7)
- Cystectomy with urinary diversion
- (8)
- Debulking for endometrial or ovarian carcinoma
- (9)
- Hip fracture surgery
- (10)
- Revision of total hip or total knee arthroplasty
- (11)
- Arterial revascularization or embolectomy of the lower limb.
2.3. Preoperative Care
2.4. Postoperative Care Setting
2.5. Data Collection
2.6. Outcomes
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
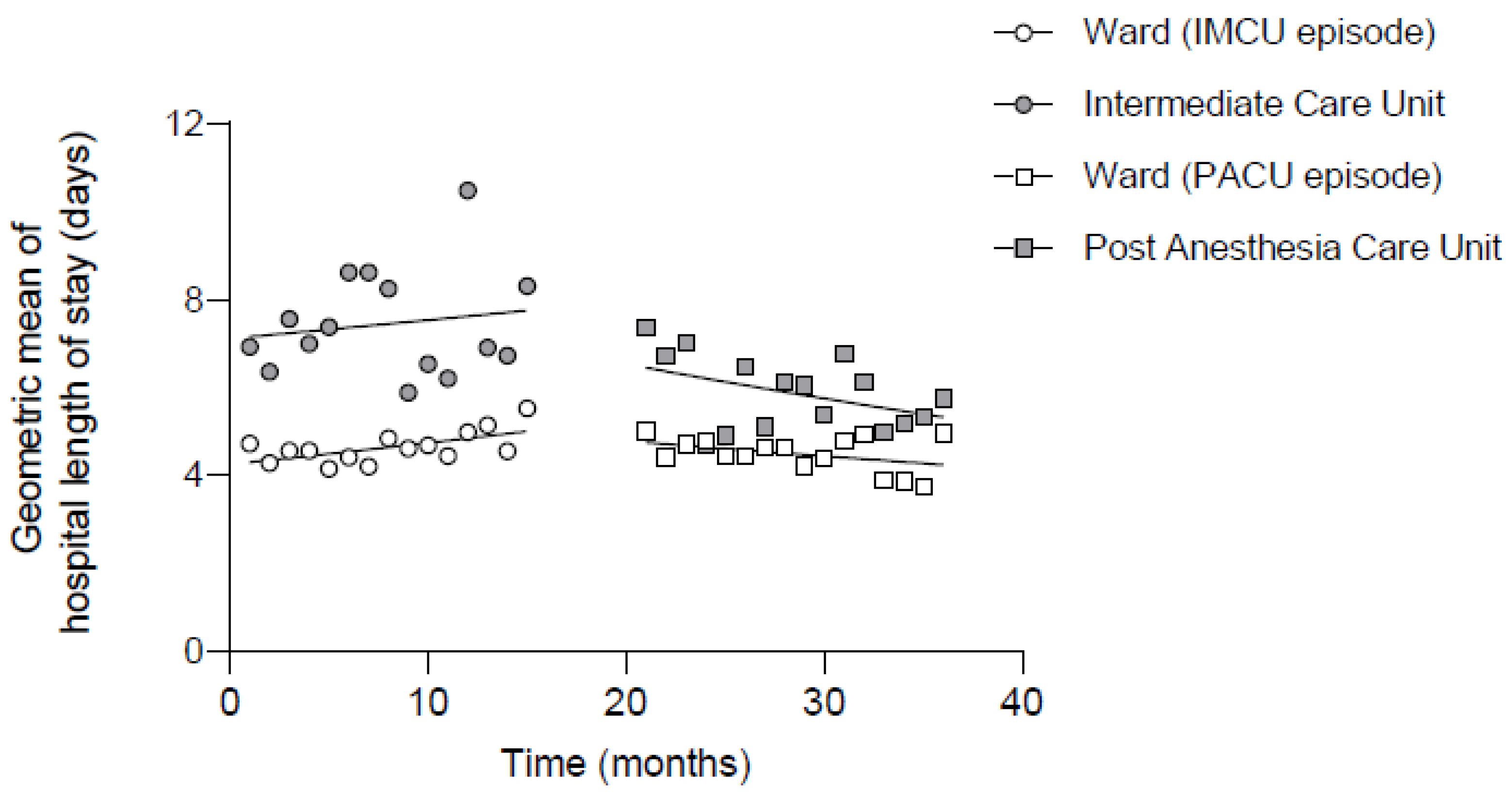
3.2. Hospital Length of Stay
3.3. Segmented Regression Analysis
3.4. Duration of Stay in the IMCU or PACU
3.5. ICU Admissions and Postoperative Complications
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Li, G.; Warner, M.; Lang, B.H.; Huang, L.; Sun, L.S. Epidemiology of Anesthesia-related Mortality in the United States, 1999–2005. Anesthesiology 2009, 110, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Bainbridge, D.; Martin, J.; Arango, M.; Cheng, D. Perioperative and anaesthetic-related mortality in developed and developing countries: A systematic review and meta-analysis. Lancet 2012, 380, 1075–1081. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, H.A.; Saied, N.N.; Kokoefer, A.S.; Saffour, L.; Zoller, J.K.; Helwani, M.A. Incidence and prediction of intraoperative and postoperative cardiac arrest requiring cardiopulmonary resuscitation and 30-day mortality in non-cardiac surgical patients. PLoS ONE 2020, 15, e0225939. [Google Scholar] [CrossRef] [PubMed]
- Pearse, R.M.; Moreno, R.P.; Bauer, P.; Pelosi, P.; Metnitz, P.; Spies, C.; Vallet, B.; Vincent, J.L.; Hoeft, A.; Rhodes, A.; et al. Mortality after surgery in Europe: A 7 day cohort study. Lancet 2012, 380, 1059–1065. [Google Scholar] [CrossRef]
- Devereaux, P.J.; Biccard, B.M.; Sigamani, A.; Xavier, D.; Chan, M.T.V.; Srinathan, S.K.; Walsh, M.; Abraham, V.; Pearse, R.; Wang, C.Y.; et al. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA 2017, 317, 1642–1651. [Google Scholar] [CrossRef]
- Devereaux, P.J.; Sessler, D.I. Cardiac Complications in Patients Undergoing Major Noncardiac Surgery. N. Engl. J. Med. 2015, 373, 2258–2269. [Google Scholar] [CrossRef]
- Pearse, R.M.; Harrison, D.A.; James, P.; Watson, D.; Hinds, C.; Rhodes, A.; Grounds, R.M.; Bennett, E.D. Identification and characterisation of the high-risk surgical population in the United Kingdom. Crit. Care 2006, 10, 10–15. [Google Scholar] [CrossRef]
- Liem, V.G.B.; Hoeks, S.E.; Mol, K.H.J.M.; Potters, J.W.; Grüne, F.; Stolker, R.J.; Van Lier, F. Postoperative Hypotension after Noncardiac Surgery and the Association with Myocardial Injury. Anesthesiology 2020, 133, 510–522. [Google Scholar] [CrossRef]
- Sessler, D.I.; Meyhoff, C.S.; Zimmerman, N.M.; Mao, G.; Leslie, K.; Vásquez, S.M.; Balaji, P.; Alvarez-Garcia, J.; Cavalcanti, A.B.; Parlow, J.L.; et al. Period-dependent Associations between Hypotension during and for Four Days after Noncardiac Surgery and a Composite of Myocardial Infarction and Death: A Substudy of the POISE-2 Trial. Anesthesiology 2018, 128, 317–327. [Google Scholar] [CrossRef]
- Bolden, N.; Posner, K.L.; Domino, K.B.; Auckley, D.; Benumof, J.L.; Herway, S.T.; Hillman, D.; Mincer, S.L.; Overdyk, F.; Samuels, D.J.; et al. Postoperative Critical Events Associated with Obstructive Sleep Apnea: Results from the Society of Anesthesia and Sleep Medicine (SASM) OSA Registry Corresponding. Anesth. Analg. 2020, 131, 1032–1041. [Google Scholar] [CrossRef]
- Dion, D.; Drudi, L.M.; Beaudoin, N.; Blair, J.F.; Elkouri, S. Safety of transition from a routine to a selective intensive care admission pathway after elective open aneurysm repair. Can. J. Surg. 2021, 64, E3–E8. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.C.; Moonesinghe, S.R. Introduction to the postanaesthetic care unit. Perioper. Med. 2013, 2, 5. [Google Scholar] [CrossRef]
- Ludbrook, G.; Lloyd, C.; Story, D.; Maddern, G.; Riedel, B.; Richardson, I.; Scott, D.; Louise, J.; Edwards, S. The effect of advanced recovery room care on postoperative outcomes in moderate-risk surgical patients: A multicentre feasibility study. Anaesthesia 2021, 76, 480–488. [Google Scholar] [CrossRef]
- Probst, S.; Cech, C.; Haentschel, D.; Scholz, M.; Ender, J. A specialized post-anaesthetic care unit improves fast-track management in cardiac surgery: A prospective randomized trial. Crit. Care 2014, 18, 468. [Google Scholar] [CrossRef]
- Mascha, E.J.; Sessler, D.I. Segmented Regression and Difference-in-Difference Methods: Assessing the Impact of Systemic Changes in Health Care. Anesth. Analg. 2019, 129, 618–633. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Halvorsen, S.; Mehilli, J.; Cassese, S.; Hall, T.S.; Abdelhamid, M.; Barbato, E.; De Hert, S.; de Laval, I.; Geisler, T.; Hinterbuchner, L.; et al. 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery. Eur. Heart J. 2022, 43, 3826–3924. [Google Scholar] [CrossRef]
- De Hert, S.; Staender, S.; Fritsch, G.; Hinkelbein, J.; Afshari, A.; Bettelli, G.; Bock, M.; Chew, M.S.; Coburn, M.; De Robertis, E.; et al. Pre-operative evaluation of adults undergoing elective noncardiac surgery: Updated guideline from the European Society of Anaesthesiology. Eur. J. Anaesthesiol. 2018, 35, 407–465. [Google Scholar] [CrossRef] [PubMed]
- Thenuwara, K.N.; Yoshimura, T.; Nakata, Y.; Dexter, F. Time to recovery after general anesthesia at hospitals with and without a phase I post-anesthesia care unit: A historical cohort study. Can. J. Anesth. 2018, 65, 1296–1302. [Google Scholar] [CrossRef] [PubMed]
- Ender, J.; Borger, M.A.; Scholz, M.; Funkat, A.K.; Anwar, N.; Sommer, M.; Mohr, F.W.; Fassl, J. Cardiac Surgery Fast-track Treatment in a Postanesthetic Care Unit: Six-month Results of the Leipzig Fast-track Concept. Anesthesiology 2008, 109, 61–66. [Google Scholar] [CrossRef]
- Lloyd, C.; Ludbrook, G.; Story, D.; Maddern, G. Organisation of delivery of care in operating suite recovery rooms within 48 hours postoperatively and patient outcomes after adult non-cardiac surgery: A systematic review. BMJ Open 2020, 10, e027262. [Google Scholar] [CrossRef] [PubMed]
- Leaman, E.E.; Ludbrook, G.L. The Cost-Effectiveness of Early High-Acuity Postoperative Care for Medium-Risk Surgical Patients. Anesth. Analg. 2023, 10, 1213. [Google Scholar] [CrossRef] [PubMed]
- Ludbrook, G.; Grocott, M.P.W.; Heyman, K.; Clarke-errey, S.; Royse, C.; Sleigh, J.; Solomon, L.B. Outcomes of Postoperative Overnight High-Acuity Care in Medium-Risk Patients Undergoing Elective and Unplanned Noncardiac Surgery. JAMA Surg. 2023, 158, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Eichenberger, A.-S.; Haller, G.; Cheseaux, N.; Lechappe, V.; Garnerin, P.; Walder, B. A clinical pathway in a post-anaesthesia care unit to reduce length of stay, mortality and unplanned intensive care unit admission. Eur. J. Anaesthesiol. 2011, 28, 859–866. [Google Scholar] [CrossRef]


| Intermediate Care Unit (IMCU) | Post-Anaesthesia Care Unit (PACU) | |
|---|---|---|
| Nurse to patient ratio | 1:3 to 1:4 | 1:2 to 1:4 |
| Beds available | 9 | 8 |
| Opening hours | 7 days per week, 24 h per day | Monday morning to saturday afternoon, 24 h per day |
| Admission | After a recovery period in the recovery room | Direct postoperatively |
| Medical supervision | Surgical staff | Anesthesiologist in collaboration with surgical staff |
| Catecholamines | Yes | Yes |
| (Non-)invasive ventilation or high-flow nasal oxygen | No | Yes |
| Duration of stay | Overnight | Individualized, based on the estimation of the anaesthesiologist |
| Intermediate Care Unit Episode (n = 1746) | Post Anaesthesia Care Unit Episode (n = 1554) | |
|---|---|---|
| Age | 71 (61–80) | 72 (62–81) |
| Gender (male/female) | 44%/56% | 42%/58% |
| ASA-PS class | 3 (2–3) | 3 (2–3) |
| BMI | 25 (23–29) | 25 (23–29) |
| Number of different medications | 4 (1–9) | 5 (1–11) |
| Pre-existing conditions | ||
| Coronary artery disease | 212 (12%) | 164 (11%) |
| Congestive heart failure | 114 (7%) | 108 (7%) |
| Valvular heart disease | 83 (5%) | 98 (6%) |
| Atrial fibrillation | 147 (8%) | 160 (10%) |
| Insulin-dependent diabetes mellitus | 127 (7%) | 80 (5%) |
| COPD | 132 (8%) | 97 (6%) |
| Respiratory insufficiency other than COPD | 73 (4%) | 79 (5%) |
| Chronic renal failure | 187 (11%) | 162 (10%) |
| Stroke | 103 (6%) | 117 (8%) |
| Anaemia | 238 (14%) | 234 (15%) |
| Type of surgery | ||
| Thyroidectomy | 110 (6%) | 91 (6%) |
| Parathyroidectomy | 33 (2%) | 29 (2%) |
| VATS (bi)lobectomy | 70 (4%) | 73 (5%) |
| Open (bi)lobectomy | 36 (2%) | 34 (2%) |
| Endovascular aortic aneurysm repair | 153 (9%) | 115 (7%) |
| Laparoscopic colorectal resection | 388 (22%) | 295 (19%) |
| Cystectomy with urinary diversion | 80 (5%) | 85 (6%) |
| Debulking for ovarian of uterine malignancy | 74 (4%) | 76 (5%) |
| Hip fracture repair | 523 (30%) | 578 (37%) |
| Revision of total knee or total hip arthroplasty | 133 (8%) | 105 (7%) |
| Revascularization of the lower extremity | 146 (8%) | 73 (5%) |
| Surgical duration (minutes) | 91 (54–151) | 78 (50–142) |
| Parameter | Geometric Mean Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| PACU episode (vs. IMCU episode) | 0.97 | 0.86–1.10 | 0.618 |
| Postoperative admission to monitored ward | 1.51 | 1.41–1.62 | <0.001 |
| Interaction postoperative admission to monitored ward during PACU episode | 0.80 | 0.73–0.88 | <0.001 |
| Time during IMCU episode (per additional month) | 1.00 | 1.00–1.01 | 0.374 |
| Time during PACU episode (per additional month) | 0.99 | 0.98–1.00 | 0.034 |
| Age (per additional year) | 1.01 | 1.01–1.01 | <0.001 |
| Gender (male) | 1.02 | 0.97–1.08 | 0.377 |
| BMI (per additional kg/m2) | 0.99 | 0.98–0.99 | <0.001 |
| Number of different medications (per additional medicament) | 1.00 | 1.00–1.00 | 0.949 |
| ASA-PS Class | |||
| ASA-PS 1 | 0.79 | 0.70–0.90 | <0.001 |
| ASA-PS 2 | 0.92 | 0.87–0.98 | 0.006 |
| ASA-PS 3 | Reference | - | - |
| ASA-PS 4 | 1.15 | 1.05–1.26 | 0.003 |
| ASA-PS 5 | 1.09 | 0.61–1.93 | 0.777 |
| Pre-existing conditions | |||
| Myocardial ischemia | 0.98 | 0.90–1.06 | 0.573 |
| Decompensated heart failure | 1.14 | 1.03–1.27 | 0.013 |
| Valvular heart disease | 1.01 | 0.91–1.12 | 0.869 |
| Atrial fibrillation | 1.11 | 1.01–1.21 | 0.024 |
| COPD | 0.98 | 0.89–1.08 | 0.714 |
| Respiratory insufficiency other than COPD | 1.11 | 0.99–1.24 | 0.073 |
| Chronic renal failure | 1.02 | 0.94–1.11 | 0.642 |
| Insulin-dependent diabetes mellitus | 1.16 | 1.05–1.29 | 0.003 |
| Anaemia | 1.14 | 1.06–1.22 | <0.001 |
| Stroke | 1.06 | 0.97–1.17 | 0.216 |
| Surgery type | |||
| Thyroidectomy | 0.33 | 0.29–0.36 | <0.001 |
| Parathyroidectomy | 0.36 | 0.30–0.43 | <0.001 |
| VATS (bi)lobectomy | 0.79 | 0.70–0.90 | <0.001 |
| Open (bi)lobectomy | 1.01 | 0.85–1.19 | 0.938 |
| Endovascular aortic aneurysm repair | 0.34 | 0.31–0.38 | <0.001 |
| Laparoscopic colorectal resection | 0.96 | 0.89–1.04 | 0.351 |
| Cystectomy with urinary diversion | 0.85 | 0.74–0.98 | 0.023 |
| Debulking for ovarian of uterine malignancy | 0.81 | 0.71–0.91 | 0.001 |
| Hip fracture repair | Reference | - | - |
| Revision of total knee or total hip arthroplasty | 0.73 | 0.66–0.81 | <0.001 |
| Revascularization of the lower extremity | 0.58 | 0.52–0.64 | <0.001 |
| Surgical duration (per additional minute) | 1.00 | 1.00–1.00 | <0.001 |
| Intermediate Care Unit Episode (n = 1746) | Post Anaesthesia Care Unit Episode (n = 1554) | p-Value | |
|---|---|---|---|
| All surgical procedures | 678 (39%) | 625 (40%) | 0.433 |
| Thyroidectomy | 36 (33%) | 21 (23%) | 0.158 |
| Parathyroidectomy | 30 (91%) | 9 (31%) | <0.001 |
| VATS (bi)lobectomy | 67 (96%) | 73 (100%) | 0.115 |
| Open (bi)lobectomy | 34 (94%) | 34 (100%) | 0.493 |
| Endovascular aortic aneurysm repair | 76 (50%) | 72 (63%) | 0.047 |
| Laparoscopic colorectal resection | 86 (22%) | 81 (28%) | 0.127 |
| Cystectomy with urinary diversion | 30 (38%) | 60 (71%) | <0.001 |
| Debulking for ovarian of uterine malignancy | 23 (31%) | 40 (53%) | 0.008 |
| Hip fracture repair | 179 (34%) | 165 (29%) | 0.044 |
| Revision of total knee or total hip arthroplasty | 39 (29%) | 32 (31%) | 0.887 |
| Revascularization of the lower extremity | 78 (53%) | 38 (52%) | 0.886 |
| Intermediate Care Unit Episode (n = 1746) | Post-Anaesthesia Care Unit Episode (n = 1554) | p-Value | |
|---|---|---|---|
| Any postoperative complication | 148 (8.5%) | 149 (9.6%) | 0.273 |
| Myocardial ischemia | 23 (1.3%) | 12 (0.7%) | 0.172 |
| Decompensated heart failure | 33 (1.9%) | 23 (1.4%) | 0.419 |
| New-onset atrial fibrillation | 34 (1.9%) | 48 (3.1%) | 0.043 |
| PPC | 57 (3.3%) | 48 (3.1%) | 0.843 |
| Stroke | 9 (0.5%) | 13 (0.8%) | 0.289 |
| AKI | 48 (2.7%) | 35 (2.3%) | 0.375 |
| Need for RRT | 1 (0.1%) | 1 (0.1%) | 1.000 |
| Pulmonary embolism | 11 (0.6%) | 13 (0.8%) | 0.542 |
| ICU admission | 69 (4.0%) | 63 (4.1%) | 0.929 |
| ICU admission for medical indication | 67 (3.8%) | 41 (2.6%) | 0.062 |
| Reoperation | 119 (6.8%) | 108 (6.9%) | 0.891 |
| Readmission | 258 (14.7%) | 188 (12.1%) | 0.032 |
| Mortality at 30 days | 49 (2.8%) | 42 (2.7%) | 0.915 |
| Mortality at 3 months | 103 (5.9%) | 80 (5.1%) | 0.361 |
| Mortality at 1 year | 188 (10.8%) | 138 (8.9%) | 0.070 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koning, N.J.; Lokin, J.L.C.; Roovers, L.; Kallewaard, J.W.; van Harten, W.H.; Kalkman, C.J.; Preckel, B. Introduction of a Post-Anaesthesia Care Unit in a Teaching Hospital Is Associated with a Reduced Length of Hospital Stay in Noncardiac Surgery: A Single-Centre Interrupted Time Series Analysis. J. Clin. Med. 2024, 13, 534. https://doi.org/10.3390/jcm13020534
Koning NJ, Lokin JLC, Roovers L, Kallewaard JW, van Harten WH, Kalkman CJ, Preckel B. Introduction of a Post-Anaesthesia Care Unit in a Teaching Hospital Is Associated with a Reduced Length of Hospital Stay in Noncardiac Surgery: A Single-Centre Interrupted Time Series Analysis. Journal of Clinical Medicine. 2024; 13(2):534. https://doi.org/10.3390/jcm13020534
Chicago/Turabian StyleKoning, Nick J., Joost L. C. Lokin, Lian Roovers, Jan Willem Kallewaard, Wim H. van Harten, Cor J. Kalkman, and Benedikt Preckel. 2024. "Introduction of a Post-Anaesthesia Care Unit in a Teaching Hospital Is Associated with a Reduced Length of Hospital Stay in Noncardiac Surgery: A Single-Centre Interrupted Time Series Analysis" Journal of Clinical Medicine 13, no. 2: 534. https://doi.org/10.3390/jcm13020534
APA StyleKoning, N. J., Lokin, J. L. C., Roovers, L., Kallewaard, J. W., van Harten, W. H., Kalkman, C. J., & Preckel, B. (2024). Introduction of a Post-Anaesthesia Care Unit in a Teaching Hospital Is Associated with a Reduced Length of Hospital Stay in Noncardiac Surgery: A Single-Centre Interrupted Time Series Analysis. Journal of Clinical Medicine, 13(2), 534. https://doi.org/10.3390/jcm13020534






