Identification of Essential Features in Developing a Novel Femoral Stem Reflecting Anatomical Features of East Asian Population: A Morphological Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Radiographic Standardization
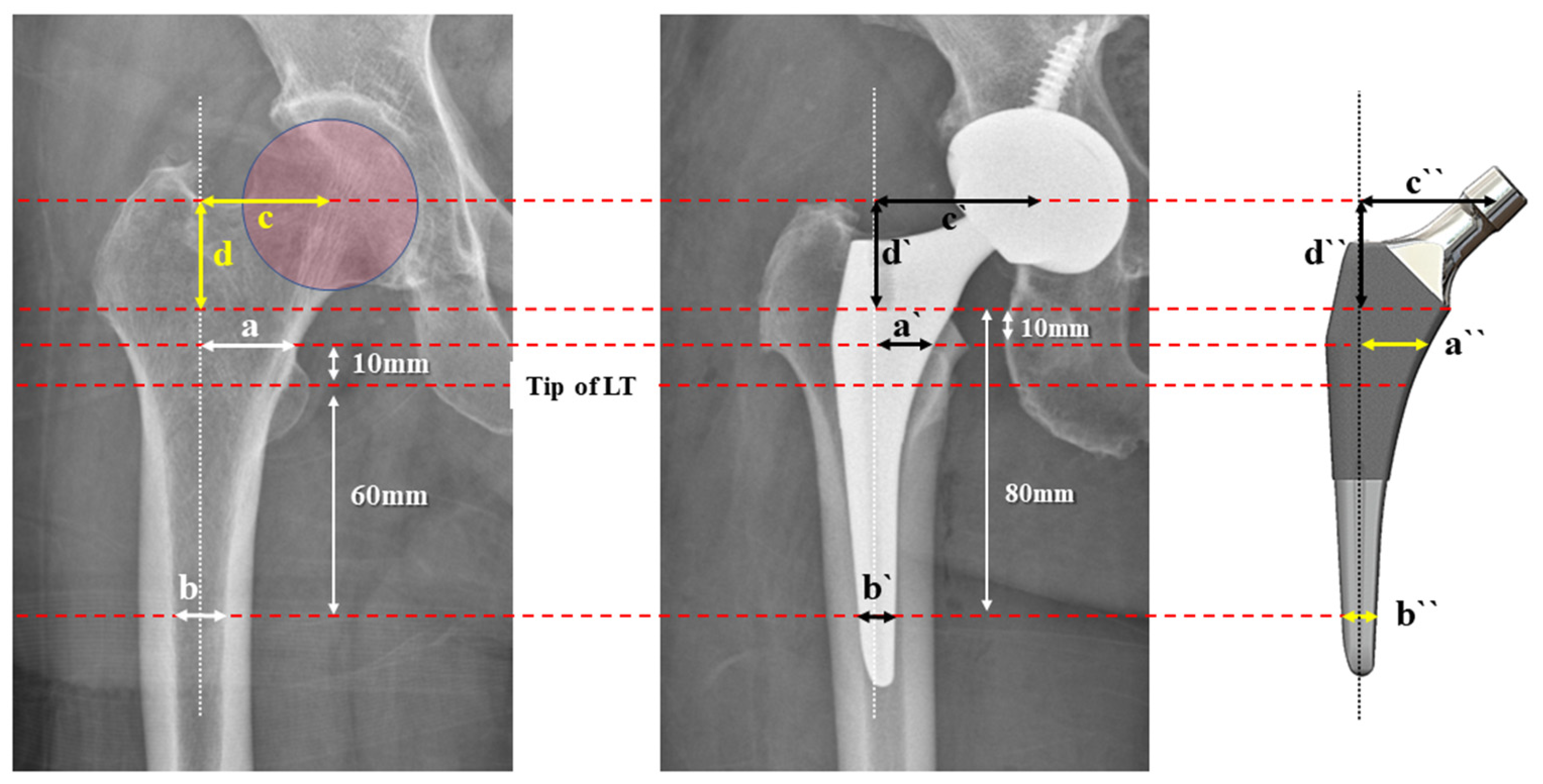
2.3. Radiographic Measurements
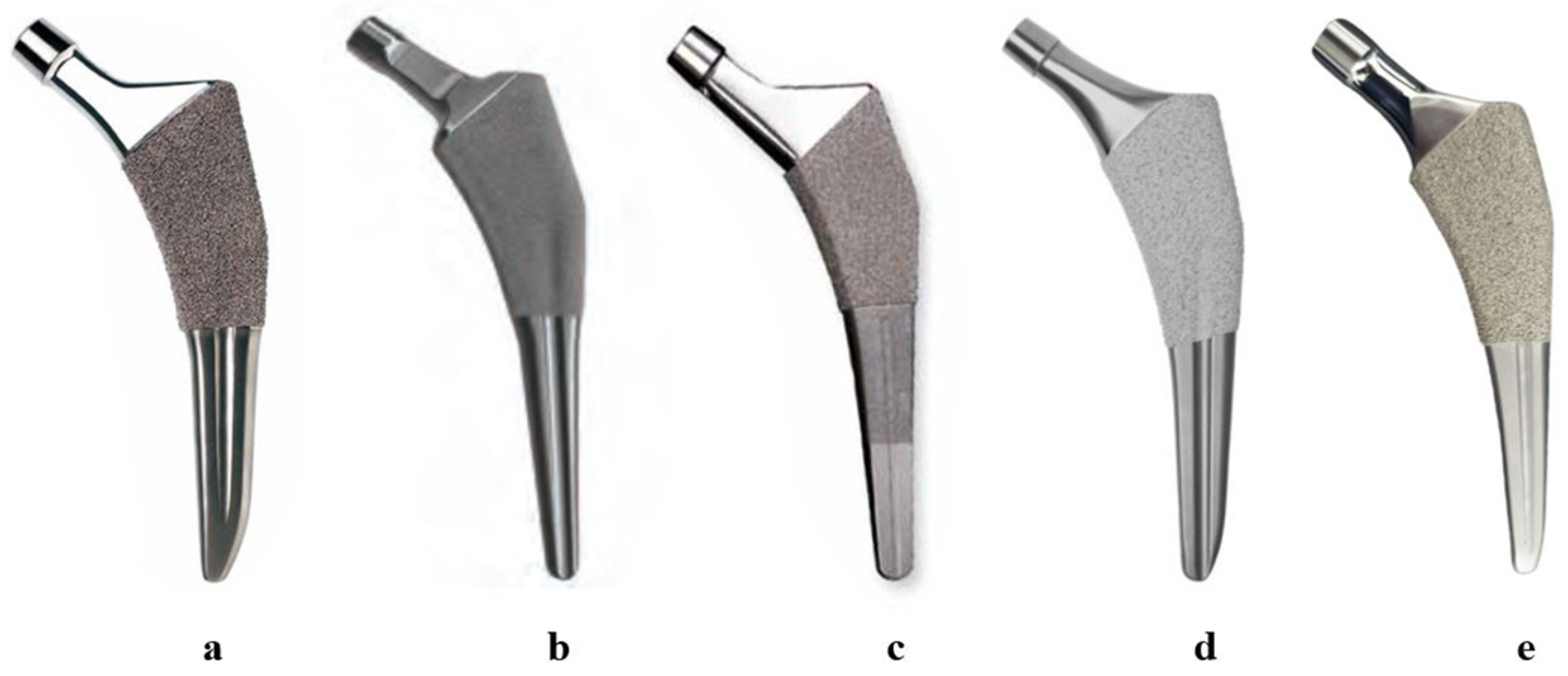
2.4. Femoral Stems for Evaluation
2.5. ML Width Analysis
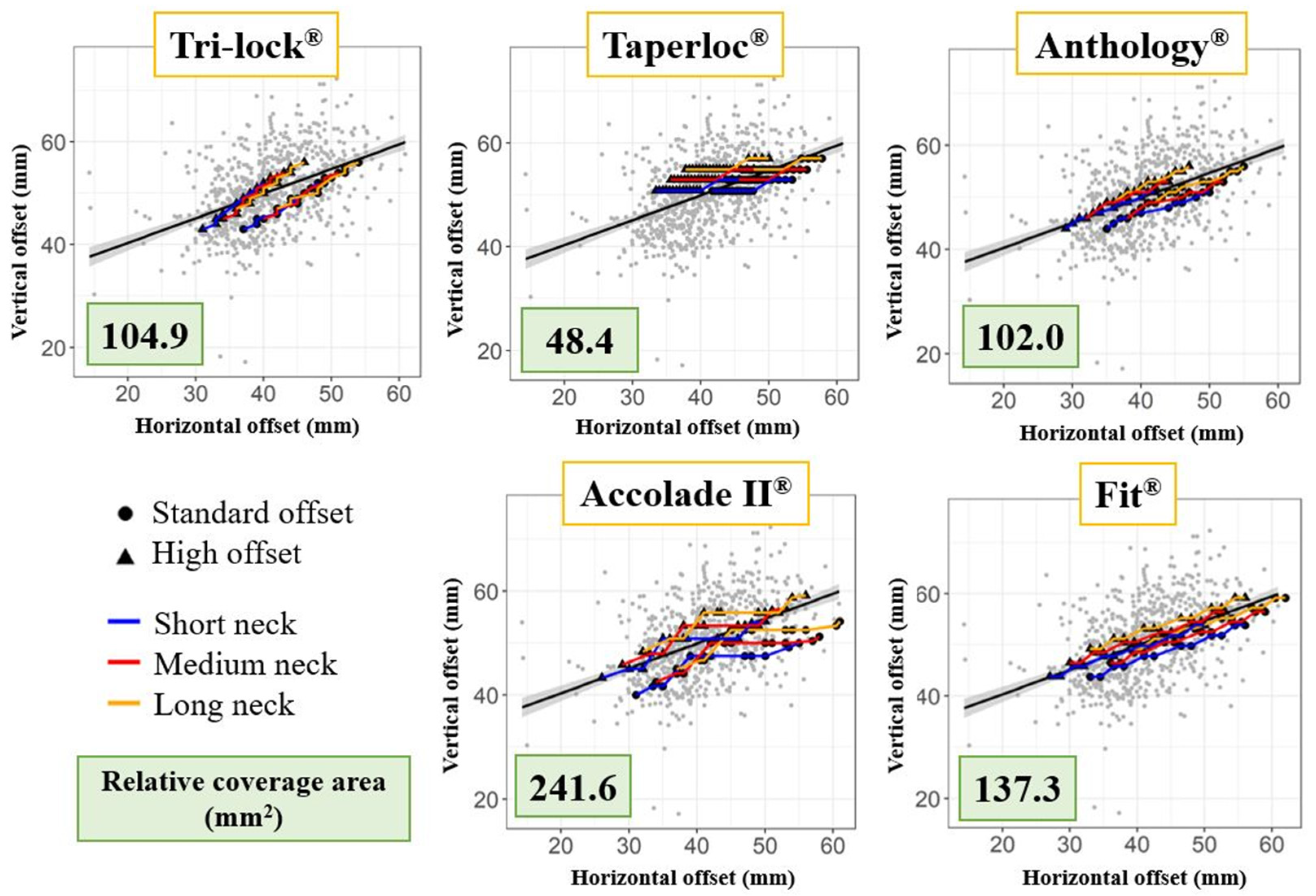
2.6. Offset Analysis
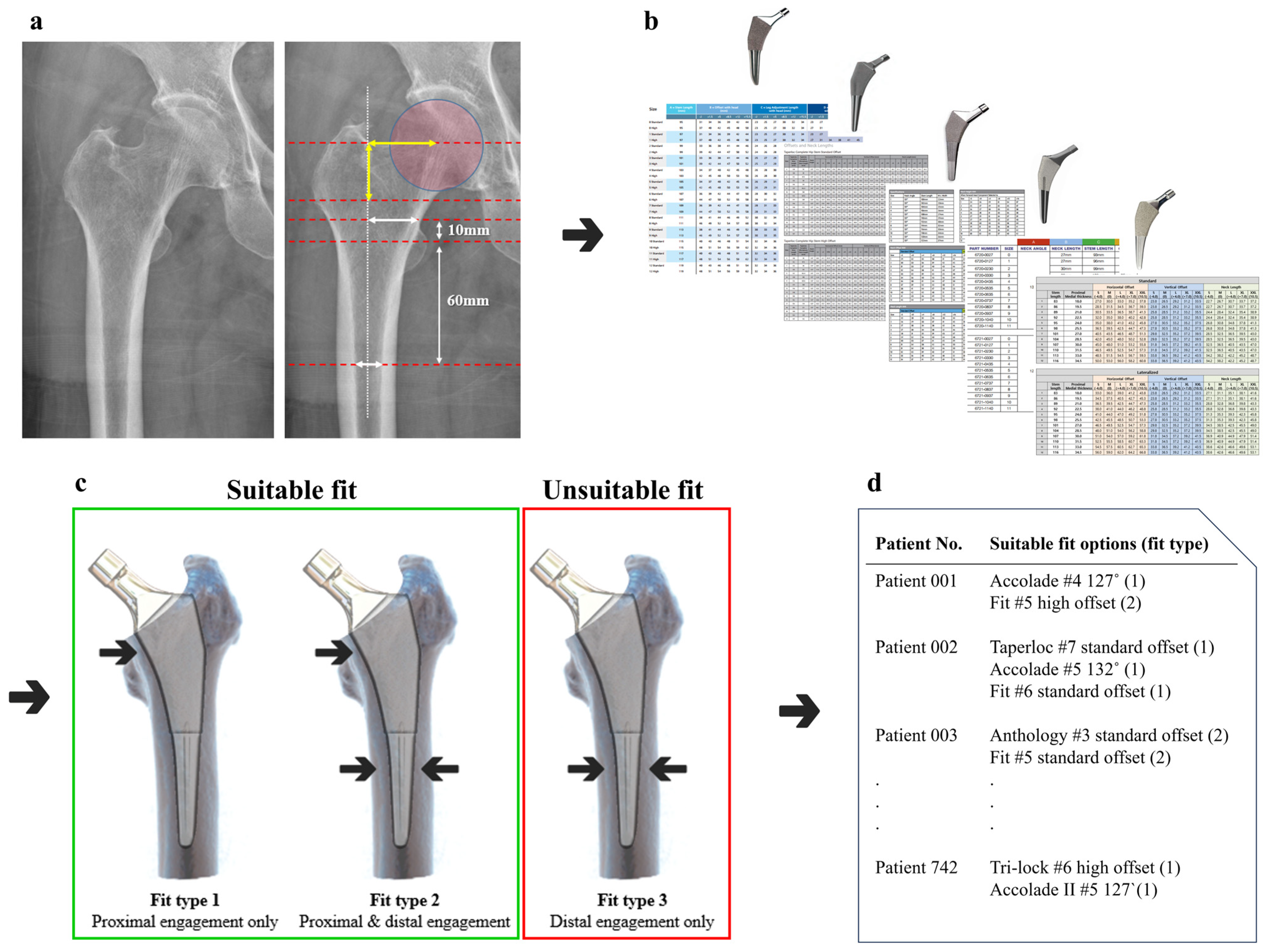
2.7. Fit Analysis Using R Coding
3. Results
3.1. ML Width Analysis
3.2. Offset Analysis
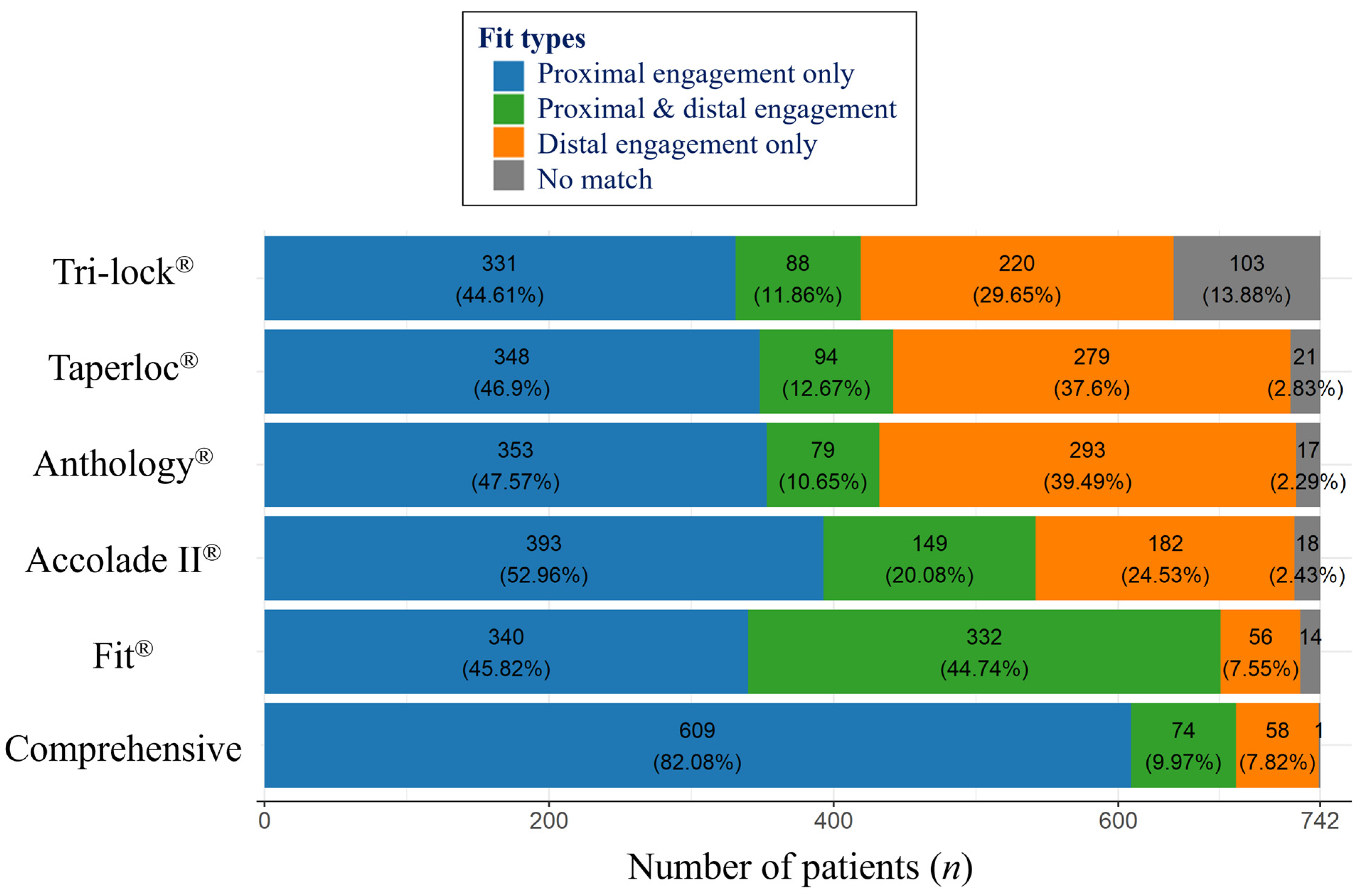
3.3. Fit Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brown, T.E.; Larson, B.; Shen, F.; Moskal, J.T. Thigh pain after cementless total hip arthroplasty: Evaluation and management. JAAOS-J. Am. Acad. Orthop. Surg. 2002, 10, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, S.; Hashimoto, S.; Matsumoto, T.; Takayama, K.; Niikura, T.; Kuroda, R. Risk factors of thigh pain following total hip arthroplasty with short, tapered-wedge stem. Int. Orthop. 2020, 44, 2553–2558. [Google Scholar] [CrossRef]
- Ha, Y.-C.; Koo, K.-H.; Jeong, S.-T.; Yoo, J.J.; Kim, Y.-M.; Kim, H.J. Cementless alumina-on-alumina total hip arthroplasty in patients younger than 50 years: A 5-year minimum follow-up study. J. Arthroplast. 2007, 22, 184–188. [Google Scholar] [CrossRef]
- Jo, W.-L.; Lee, Y.-K.; Ha, Y.-C.; Park, M.-S.; Lyu, S.-H.; Koo, K.-H. Frequency, developing time, intensity, duration, and functional score of thigh pain after cementless total hip arthroplasty. J. Arthroplast. 2016, 31, 1279–1282. [Google Scholar] [CrossRef]
- Park, C.-W.; Eun, H.-J.; Oh, S.-H.; Kim, H.-J.; Lim, S.-J.; Park, Y.-S. Femoral stem survivorship in Dorr type A femurs after total hip arthroplasty using a cementless tapered wedge stem: A matched comparative study with type B femurs. J. Arthroplast. 2019, 34, 527–533. [Google Scholar] [CrossRef]
- Dorr, L.D.; Faugere, M.-C.; Mackel, A.M.; Gruen, T.A.; Bognar, B.; Malluche, H.H. Structural and cellular assessment of bone quality of proximal femur. Bone 1993, 14, 231–242. [Google Scholar] [CrossRef]
- Kang, J.S.; Ko, S.H.; Na, Y.; Youn, Y.H. Clinical and radiological outcomes of rectangular tapered cementless stem according to proximal femoral geometry in elderly Asian patients. Hip Pelvis 2019, 31, 224–231. [Google Scholar] [CrossRef]
- Ishii, S.; Homma, Y.; Baba, T.; Ozaki, Y.; Matsumoto, M.; Kaneko, K. Does the canal fill ratio and femoral morphology of Asian females influence early radiographic outcomes of total hip arthroplasty with an uncemented proximally coated, tapered-wedge stem? J. Arthroplast. 2016, 31, 1524–1528. [Google Scholar] [CrossRef] [PubMed]
- Cooper, H.J.; Jacob, A.P.; Rodriguez, J.A. Distal fixation of proximally coated tapered stems may predispose to a failure of osteointegration. J. Arthroplast. 2011, 26, 78–83. [Google Scholar] [CrossRef]
- Lim, Y.W.; Huddleston III, J.I.; Goodman, S.B.; Maloney, W.J.; Amanatullah, D.F. Proximal femoral shape changes the risk of a leg length discrepancy after primary total hip arthroplasty. J. Arthroplast. 2018, 33, 3699–3703. [Google Scholar] [CrossRef]
- Mavčič, B.; Antolič, V. Cementless femoral stem fixation and leg-length discrepancy after total hip arthroplasty in different proximal femoral morphological types. Int. Orthop. 2021, 45, 891–896. [Google Scholar] [CrossRef] [PubMed]
- McConnell, J.S.; Syed, F.A.; Saunders, P.; Kattimani, R.; Ugwuoke, A.; Magra, M.; Young, S.K. Definition and validation of a system for classifying the undersized Corail femoral stem in total hip arthroplasty. HIP Int. 2021, 32, 1120700021996001. [Google Scholar] [CrossRef]
- Thiesen, D.M.; Ntalos, D.; Korthaus, A.; Petersik, A.; Frosch, K.-H.; Hartel, M.J. A comparison between Asians and Caucasians in the dimensions of the femoral isthmus based on a 3D-CT analysis of 1189 adult femurs. Eur. J. Trauma Emerg. Surg. 2021, 48, 2379–2386. [Google Scholar] [CrossRef]
- Noble, P.C.; Alexander, J.W.; Lindahl, L.J.; Yew, D.T.; Granberry, W.M.; Tullos, H.S. The anatomic basis of femoral component design. Clin. Orthop. Relat. Res. 1988, 235, 148–165. [Google Scholar] [CrossRef]
- Pi, Y.; Zhao, Y.; Wang, W.; He, Z.; Mao, X. Measurement of proximal femoral morphology and analysis of 500 cases in Hunan Province. Zhong Nan Da Xue Xue Bao. Yi Xue Ban J. Cent. South Univ. Med. Sci. 2013, 38, 925–930. [Google Scholar]
- Boese, C.K.; Jostmeier, J.; Oppermann, J.; Dargel, J.; Chang, D.-H.; Eysel, P.; Lechler, P. The neck shaft angle: CT reference values of 800 adult hips. Skelet. Radiol. 2016, 45, 455–463. [Google Scholar] [CrossRef]
- Lim, Y.W.; Chang, Y.J.; Kwon, S.Y.; Kim, Y.S. A simple method using a PACS to minimize leg length discrepancy in primary THA: A method to minimize leg length discrepancy. J. Arthroplast. 2013, 28, 1791–1795. [Google Scholar] [CrossRef]
- Oddy, M.; Jones, M.; Pendegrass, C.; Pilling, J.; Wimhurst, J. Assessment of reproducibility and accuracy in templating hybrid total hip arthroplasty using digital radiographs. J. Bone Jt. Surg. Br. Vol. 2006, 88, 581–585. [Google Scholar] [CrossRef]
- Wuestemann, T.; Hoare, S.G.; Petersik, A.; Hofstaetter, B.; Fehily, M.; Matsubara, M.; Markel, D.C. Bone morphology of the proximal femoral canal: Ethnicity related differences and the influence on cementless tapered wedge stem designs. HIP Int. 2021, 31, 482–491. [Google Scholar] [CrossRef]
- Nazari-Farsani, S.; Vuopio, M.E.; Aro, H.T. Bone mineral density and cortical-bone thickness of the distal radius predict femoral stem subsidence in postmenopausal women. J. Arthroplast. 2020, 35, 1877–1884.e1. [Google Scholar] [CrossRef]
- American Joint Replacement Registry (AJRR). 2021 Annual Report; American Academy of Orthopaedic Surgeons (AAOS): Rosemont, IL, USA, 2021. [Google Scholar]
- Faizan, A.; Wuestemann, T.; Nevelos, J.; Bastian, A.C.; Collopy, D. Development and verification of a cementless novel tapered wedge stem for total hip arthroplasty. J. Arthroplast. 2015, 30, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Wuestemann, T.; Bastian, A.; Schmidt, W.; Cedermark, C.; Streicher, R.; Parvizi, J.; Rothman, R. A novel technique for studying proximal femoral bone morphology for hip implant design. In Orthopaedic Proceedings; British Editorial Society of Bone and Joint Surgery: London, UK, 2011; pp. 156–157. [Google Scholar]
- Zanetti, E.M.; Bignardi, C. Mock-up in hip arthroplasty pre-operative planning. Acta Bioeng. Biomech. 2013, 15, 123–128. [Google Scholar] [PubMed]

| Patients, n | 742 |
| Men (%) | 313 (42.2%) |
| Women (%) | 429 (57.8%) |
| Average age ± SD (range), years | 63.98 ± 14.29 |
| Average BMI ± SD (range), kg/m2 | 23.73 ± 3.17 |
| Preoperative diagnosis, n | |
| ONFH | 147 (42.9%) |
| Secondary osteoarthritis | 68 (19.8%) |
| Primary osteoarthritis | 59 (17.2%) |
| Femur neck fracture | 55 (16.0%) |
| Rheumatoid arthritis | 7 (2.0%) |
| Intertrochanteric nonunion | 5 (1.5%) |
| DDH sequelae | 2 (0.6%) |
| Stem | Manufacturer | Available Conventional Stem Sizes |
|---|---|---|
| Tri-lock® | DePuy Orthopaedics | 10 (#1–#9) |
| Taperloc® | Biomet Orthopedics | 17 (#4–#20) |
| Anthology® | Smith and Nephew Inc. | 12 (#1–#12) |
| Accolade II® | Stryker Orthopaedics | 11 (#1–#11) |
| Fit® | Corentec | 12 (#1–#12) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bahk, J.H.; Han, S.-B.; Rhyu, K.H.; Yoo, J.J.; Lim, S.-J.; Park, K.K.; Kim, S.-M.; Lim, Y.W. Identification of Essential Features in Developing a Novel Femoral Stem Reflecting Anatomical Features of East Asian Population: A Morphological Study. J. Clin. Med. 2024, 13, 6030. https://doi.org/10.3390/jcm13206030
Bahk JH, Han S-B, Rhyu KH, Yoo JJ, Lim S-J, Park KK, Kim S-M, Lim YW. Identification of Essential Features in Developing a Novel Femoral Stem Reflecting Anatomical Features of East Asian Population: A Morphological Study. Journal of Clinical Medicine. 2024; 13(20):6030. https://doi.org/10.3390/jcm13206030
Chicago/Turabian StyleBahk, Ji Hoon, Seung-Beom Han, Kee Hyung Rhyu, Jeong Joon Yoo, Seung-Jae Lim, Kwan Kyu Park, Sang-Min Kim, and Young Wook Lim. 2024. "Identification of Essential Features in Developing a Novel Femoral Stem Reflecting Anatomical Features of East Asian Population: A Morphological Study" Journal of Clinical Medicine 13, no. 20: 6030. https://doi.org/10.3390/jcm13206030
APA StyleBahk, J. H., Han, S.-B., Rhyu, K. H., Yoo, J. J., Lim, S.-J., Park, K. K., Kim, S.-M., & Lim, Y. W. (2024). Identification of Essential Features in Developing a Novel Femoral Stem Reflecting Anatomical Features of East Asian Population: A Morphological Study. Journal of Clinical Medicine, 13(20), 6030. https://doi.org/10.3390/jcm13206030







