Abstract
Odontoid fractures (OFs) represent up to 15% of all cervical fractures encountered and present most commonly amongst elderly patients, typically in the setting of low energy trauma such as falls. The Anderson and D’Alonzo classification and Roy-Camille subtype description are the most clinically noteworthy descriptions of OFs used. Even though most patients will not present with neurological injury, mechanical instability can occur with type II and type III (Anderson and D’Alonzo) fractures, particularly if the transverse ligament of the atlas is ruptured; however, this is very rare. Conservative treatment is usually employed for type I and type III injuries, and to a varying degree for non-displaced type II injuries. Surgical treatment is typically reserved for type II fractures, patients with neurological injury, and in the setting of other associated fractures or ligamentous injury. Anterior screw fixation is a viable option in the setting of a favorable fracture line orientation in type II fractures, whereas posterior C1–C2 screw fixation is an option for any type II or type III fracture presentation. There is evidence that surgery for type II fractures has higher rates of union and lower mortality than nonoperative treatments. While surgical options have increased over the decades and the management of OF has been optimized by considering fracture subtypes and patient factors, there remains a significant morbidity and mortality associated with OFs. The aging population and changing demographics suggest that there will be an ongoing rise in the incidence of OFs. Therefore, the appropriate management of these cases will be essential for ensuring optimization of health care resources and the quality of life of affected patients
1. Introduction
Odontoid Fractures (OF), or fractures of the dens of C2, represent one of the most common types of cervical fractures, and certainly the most common fracture encountered in the upper cervical spine and cranio-cervical junction (CCJ) [1]. These fractures occur frequently amongst the elderly following relatively minor falls [2,3], but can also occur in younger patients, typically from high velocity trauma, such as in motor vehicle accidents [4]. Despite their sensitive anatomical location—adjacent to the upper cervical spinal cord and the lower brainstem—these fractures are not frequently associated with neurological injury [5], unless associated with a significant subluxation.
Given the predominant prevalence of OFs amongst elderly patients, the rising aging population will result in increased encounter rates in clinical practice [3,6]. While this clearly presents a challenge to the health care system, the rise in anticipated cases is further complicated by the controversy surrounding the best strategy for their management [7,8]. Given that OFs vary in type, it is clear that minor fractures (i.e., non-displaced stable fractures, neurologically asymptomatic) are typically treated non-operatively; however, management challenges arise with OFs that are more serious and where clear therapeutic guidance regarding the relative benefits of operative and non-operative management remain unclear.
In an attempt to provide a framework for helping clinicians and surgeons in their decision-making when encountering these fractures, this review seeks to provide the reader with the current state of the art on OFs. For simplicity, fracture types in this article refer to the classification proposed by Anderson and D’Alonzo [9].
2. Classification and Imaging
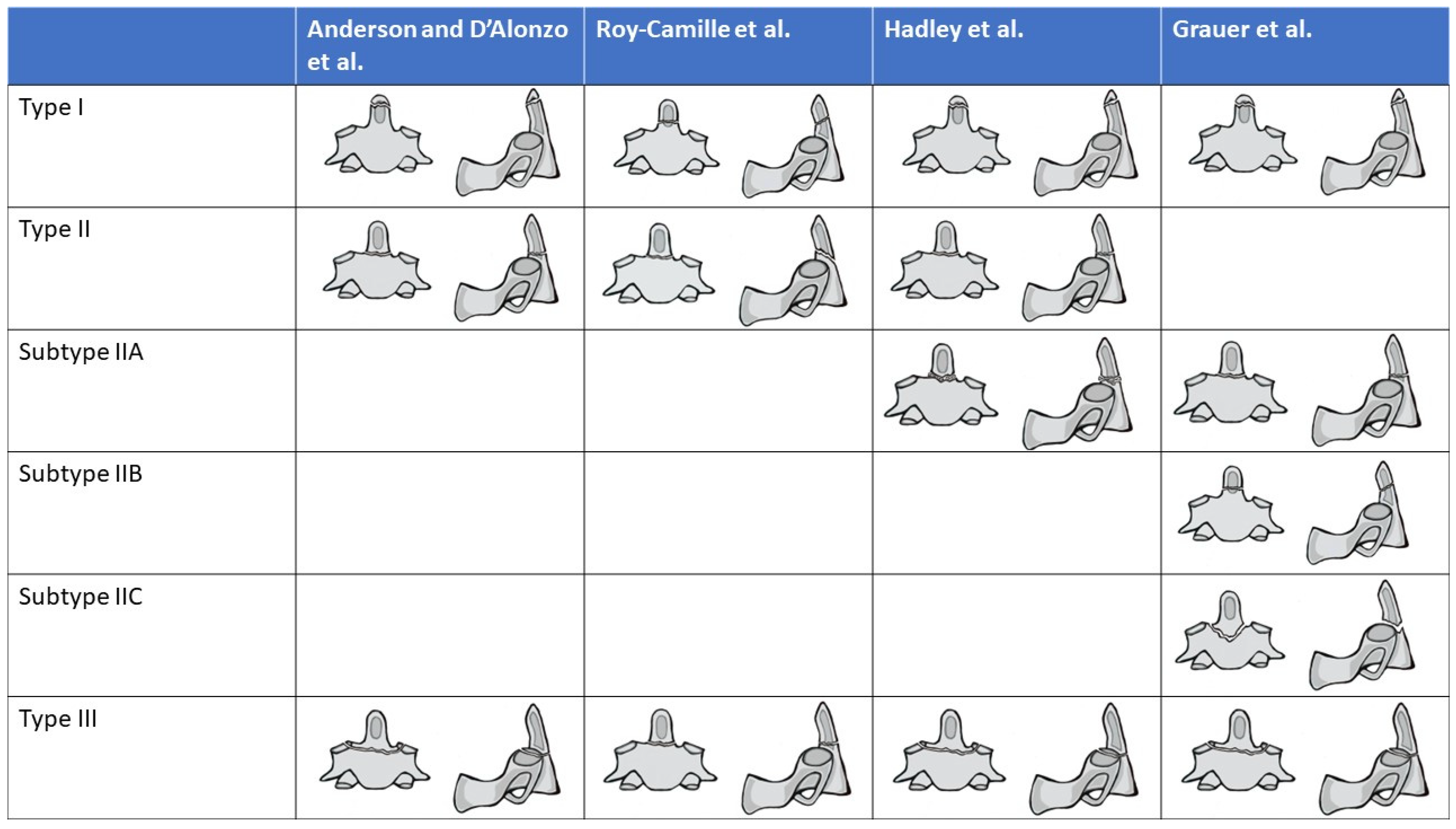
While an initial classification was proposed by Schatzker et al. in 1970 [10], the most commonly used system for classifying OFs was described by Anderson and D’Alonzo [9] a few years later. Here, the authors separate the fracture into three different types: type I, which are fractures of the tip and above the C1 transverse ligament; type II, which are transverse or oblique fractures through the base of the odontoid (at least one end of the fracture line below the transverse ligament); and type III, which are fractures just below the base of the odontoid which by definition run through the body of the C2 vertebral body (Figure 1). Multiple additional classifications have been proposed in the literature, which focus on modifications of Anderson and D’Alonzo’s description, rather than completely different descriptions, including Hadley [11,12,13], (Figure 1 and Table 1). With regard to the AO Spine classification of upper cervical injuries, all isolated odontoid fractures are considered Type A fractures [14].
Figure 1.
Classification of Odontoid Fractures according to Anderson and D’Alonzo. Sub-classifications of type II fractures according to Roy-Camille, Hadley, and Grauer. Type IV of Roy-Camille classification is not shown in this figure [9,11,12,13].

Table 1.
Description of Odontoid Fracture Classifications or New Fracture Types.
3. Pathophysiology
Fractures of the odontoid occur almost exclusively due to trauma, though very rarely fractures may occur due to pathologic causes, such as metastatic disease. Typically, low velocity trauma, such as falls, involving the head and neck, which result in sudden hyper-flexion or hyper-extension, are associated with fractures in the elderly with bone fragility. Type II fractures, according to the Anderson D’Alonzo classification, are the most common type given the mechanical vulnerability of the odontoid at its base. This vulnerability of the base is multifactorial: (1) this region is subject to high biomechanical stress, since it is situated between transverse ligaments of C1 above and the C2 vertebral body below; (2) the presence of sub-dental synchondrosis between the dens and C2 body ossification centers, which represents a weak point across the dens [15]; (3) it represents a watershed area, resulting in limited a regenerative capacity and less trabecular bone [16,17], (4) degeneration of the atlanto-odontoid joint and associated local reactive osteosclerosis, increasing C1–C2 rigidity and odontoid bone fragility [2]. While these factors are important, it is also clear that the high level of rotatory mobility of the C1–C2 joint (over 45°) [18] places significant stress on the odontoid, which acts as pivot point. Ultimately, OFs in younger patients are usually the result of high velocity accidents and the abovementioned factors play less of a role. Indeed, younger patients frequently presents with odontoid subluxation and consequently more severe neurological deficit, as well as other cervical spine fractures, particularly C1 fractures.
4. Epidemiology
OFs are one of the most common fractures of the upper cervical spine, estimated to represent 9–15% of all cervical fractures [19,20], and occurring more commonly among men in younger cohorts [21,22]. The mean age of injury is not an accurate epidemiological measure, as the occurrence of these fractures is typically bimodal and slanted towards older age, with a smaller peak in young adults (20–30 years of age) typically due to high-speed trauma and a larger peak amongst elderly patients (80 years of age) typically due to falls [3,23]. Due to the nature of their occurrence in the elderly (fragility of bone), it is not surprising that there is substantial increase in the incidence of fractures with increasing age. When looking at C2 fractures in general, an incidence of 0.71/10,000, 2.23/10,000, and 5.67/10,000 person-years has been reported in patients 65–74, 75–84, and over 85 years of age, respectively [3]. OFs are the most common type of fracture occurring at C2 level. OF fractures are also the most common fracture of the atlantoaxial junction, with isolated OFs representing approximately half of the fractures in this region [4]. It has been shown that the rate of incidence has increased over the years and will likely continue to increase with the shifting demographics towards larger cohorts of seniors in many of the developed economies [3,6,23,24].
Large national registry studies have shown that the vast majority of OFs are type II (60–80%) and type III (20–39%), with type I (0–4%) fractures occurring much less frequently [1,23,25,26,27]. As for type II fractures, the most common type of sub-classification (Roy-Camille) appears to be the oblique posterior variant [4] (Figure 1).
5. Risk Factors
There are some factors that have been shown to predispose individuals to odontoid fractures. These have been classified into medical and physiological factors, and other factors (such as metastatic disease).
5.1. Medical and Physiological
One of the clearest risk factors associated with OFs is age. Multiple studies have shown that the incidence of OFs rises progressively in older adults, with incidence rising with each sequential decade and peaking in the 80s–90s [23,27]. This is likely related to the quality of bone, which becomes more fragile with advancing age. Younger adults who present with odontoid fractures manifest with this fracture due to their propensity for high velocity injuries. The actual factors behind age as a risk factor are likely multiple, including higher risk for low energy falls from other conditions associated with age as well as increased frailty [28]. However, there are also other factors, such as accumulated degenerative changes in the cervical spine that can alter biomechanical forces and flexibility. It has been shown, for example, that significant atlanto-odontoid osteoarthritis in the presence of normal lateral atlantoaxial joints increases the risk of sustaining Type II OFs [2,29]. Others have shown that retro-dens synovitis is more common amongst patients with OF [30].
The fragility of bone, due to osteoporosis, is another important contributor predisposing to OFs [29,31], and it has been shown that the cervical bone mineral density is an independent significant risk factor for odontoid fractures but not for other fractures of the cervical spine [32]. It has also been shown that odontoid cysts predispose one to OF [30], and specifically Type II OF factures [32]. This fragility can also predispose an individual to pseudoarthrosis with both conservative management or surgical fixation [33].
Bone fragility may also arise from other conditions such as rheumatoid arthritis and ankylosing spondylitis [34,35,36]. While patients with ankylosing spondylitis present with OFs due to low energy trauma, patients with rheumatoid arthritis typically present with atraumatic fractures. The risk associated with ankylosing spondylitis is related to the rigidity and brittleness of the fused spine, which leads to the spine behaving much like an osteoporotic long bone rather than an elastic spine [34]. Moreover, given that ankylosing spondylitis typically spares the cranio-cervical junction and rigidifies the rest of the spine, the C1–C2 region becomes a transitional area which undergoes an increased biomechanical stress. The reason behind atraumatic fractures amongst patients with rheumatoid arthritis is less well known.
5.2. Other Rare Risk Factors
A rare but important risk factor for OF is metastatic disease of the C2 vertebra or an odontoid peg leading to a pathologic fracture. Such cases may not be associated with trauma, but due to pain are often treated with a combination of vertebroplasty and stabilization [37,38].
Rarer risk factors for OF include congenital malformations of the cervical region, particularly in the C1–C2 region, which can alter the biomechanics and stress forces related to the odontoid [39]. While many such congenital conditions (Klippel–Feil Syndrome, Down’s Syndrome) exist, literature more substantial than case reports that discuss this topic is practically non-existent. One exception is a small report suggesting that ponticulus posticus anomaly may increase the risk for Type II OFs [40].
It is important to note that while other notable developmental anomalies of the odontoid exist, such as os odontoideum, persistent ossiculum terminale, and odontoid aplasia, these have not been shown to predispose individuals to OF, but may, however, increase atlantoaxial instability [41,42].
6. Clinical Presentation
The typical presentation of OF is an elderly patient who arrives at the emergency department after an accidental fall from standingand who presents with neck pain, particularly with movement. The other less common group of individuals who present are patients having sustained high energy trauma such as from a motor vehicle accident; these OFs are, however, typically associated with multiple other injuries. Despite suffering from mechanical instability, neurological injury is present in only a minority of patients, with most studies reporting an incidence of ≤13% [5,43,44], and a single smaller and older study reporting a rate of 29% [45]. SCI in this setting has been shown to present more commonly amongst males, younger patients, those having sustained higher velocity injuries, and those with narrower C2 canal size [5,43]. It is noteworthy that the presence of neurological injury is also associated with a high rate of mortality [43].
It has been shown that a large proportion of patients with diagnosed OFs after cervical trauma show evidence of non-acute injury, suggesting the trauma experienced is rather “acute-on-chronic” [46]. Indeed, it has been estimated that up to 40% of geriatric odontoid fractures are not diagnosed [47]. For patients encountered with trauma and in whom previous non-union of an OF is observed, the incidence of neurological injury has been reported at 17.5% [46].
Besides a detailed neurological exam, the initial work-up typically involves radiographs, including lateral imaging and open mouth views which allow for a clear view of the odontoid. However, these may miss non-displaced OFs, and therefore the gold standard radiological exam is a cervical CT scan. If significant odontoid displacement is observed or the patient presents with a neurological injury, it is important and useful to assess the degree of cord compression as well as the integrity of associated cranio-cervical junction ligaments, most importantly the alar and cruciate (notable the transverse component) ligaments [48,49]. It has been reported that the transverse atlanto-ligament is ruptured in ~10% of patients and it has been suggested that if there is >3 mm separation between C1 and the dens, as measured by the atlanto-dental interval (ADI), it is suggestive of transverse ligament injury [49,50,51]. This indicates the presence of potential atlanto-occipital dissociation injuries. Indications for MRI evaluation include assessment of the age of the fracture, assessment of ligamentous injury, and assessment of the spinal cord [7].
7. Treatment
The treatment of odontoid fractures can be conservative or surgical, and the choice is dependent on the type of fracture, presence of spinal instability, and patient factors; that is to say, some patients could have radiological and mechanical indication for fixation, but patient factors are not conducive to operative treatment. The aim of all treatment options remains the same and includes spine realignment, stabilization and fusion, and decompression (if needed). Generally speaking, a strong indication for surgical treatment is spinal cord injury and a high risk of non-union, whereas strong contraindications for surgical treatment include patients with limited life expectancy (for example due to advanced dementia), and significant medical risks associated with potential surgical treatment. The various treatment options are discussed in further detail below. It is important to note, that this section focuses mostly on OFs in the elderly population.
8. Surgery
When considering isolated odontoid fractures without other associated injuries to the cranio-cervical junction, surgical treatment is generally reserved for patients with OF type II fractures, whereas type I and III fractures are generally treated with non-operative treatment [13]. Particular attention must be paid to type I fractures, because sometimes they are associated with C0–C1 vertical instability or ligamentous injury (e.g., apical and alar ligaments) which require a cranio-cervical junction fusion [7]. In rare cases, type III fractures may also be treated surgically. Typically, this is for cases where type III fractures are higher in the body and shallow, and therefore behave more like type II fractures [52]. According to some authors [53,54,55], an association between conservative treatment of type III OF and non-union with displacement was observed in patients older than 40 years of age, with translation >5 mm, and angulation >10°. Furthermore, some patients who cannot tolerate long-term solid external fixation can be good candidates for surgery. Likewise, some surgeons treat OF type II fractures non-operatively initially, rather than surgically, if no neurological symptoms are associated [56].
Another fundamental variable that should be taken into account is patient age. In fact, there are substantial differences in terms of surgical or non-operative indications for elderly patients and younger ones. In elderly patients, for whom the non-operative treatment may be preferred due to comorbidities, the non-union rates are generally higher with hard collars compared to the younger population, and halo vest fixation is practically abandoned in this population [57,58]. Also, the choice of surgical technique may lead to different results in the elderly. For instance, as highlighted by Texakalidis et al., anterior dens screw fixation showed lower rates of fusion and higher reoperation rates in patients older than 60 years of age. Hence, posterior fixation is preferable for this population [59]. On the other hand, younger patients are more likely male with motor vehicle collision as the mechanism of injury and present generally with more severe trauma, neurological deficit, and other associated lesions. However, the non-union rates are significantly lower at follow-up compared to elderly counterparts. Indeed, external fixation with halo vests can be a viable option for younger patients with low non-union rates [57].
When surgery is undertaken, multiple surgical options exist and are listed in Table 2. It is important to note that for all surgical procedures, wearing a hard collar in the postoperative period might be recommended to increase the fusion rate, even though this measure is controversial. This, however, comes with the risk of hard collars b, which will be discussed further in the non-operative treatment section.

Table 2.
Surgical Techniques for Managing Odontoid Fractures.
8.1. Anterior Approach
The anterior peg screw fixation allows for stabilization of OFs by the insertion of a lag screw across the fracture line. Unlike posterior C1–C2 fixation, it maintains rotation at the level of the C1–C2 joints by restoration of dens anatomy and alignment [59]. The choice for an anterior approach with an odontoid screw is typically reserved for Roy-Camille type IIA and type IIC (Table 1) fractures, where the obliquity of the fracture is perpendicular to the anterior screw insertion. However, it may also be used in Roy-Camille type IIC fractures, where the fractures line is horizontal. The success of the technique requires that the odontoid is reduced and well aligned; this may be aided by intraoperative transoral digital reduction [62]. Sometimes screw insertion is supported with bone cement, particularly in patients with osteoporosis or lytic metastatic disease [61]. In other instances, anterior trans-articular screws may be performed in isolation or may also be added if it is deemed that the odontoid screw fixation is suboptimal, or for a stronger fixation in osteoporotic patients [60]. Minimally invasive approaches to performing anterior screw fixation have been reported as a safe and effective way to achieve satisfactory fusion [63]. However, according to a recent meta-analysis published by Texakadilis et al., anterior dens screw fixation is associated with statistically significantly lower odds of fusion and higher odds of reoperation compared to C1–C2 arthrodesis. This is particularly true for patients older than 60 years [59]. Another meta-analysis performed by Lvov et al. demonstrated that double screw dens fixation in elderly patients results in higher risks of postoperative cut-out. This study showed also that patient age is a major risk factor of fracture non-union and that the fusion rate did not depend on the technique [64].
Anterior screw fixation is contraindicated in patients with transverse ligament injury, as well as for comminuted fractures, and it is important to note that even with a clinical and radiological indication, technical issues may prevent access for anterior screw placement. These include inability to reduce the fracture, or body habitus restrictions, such as a short neck, barrel-shaped chest, or cervical or thoracic deformity [65].
8.2. Posterior Approach
Posterior surgery can be undertaken for any of the odontoid fracture types and can be performed in different ways. In 1992, Magerl and Jeanneret described for the first time a technique to realize posterior arthrodesis for odontoid fractures.
The classic Magerl technique consists of placing screws along a trans-articular trajectory, inserting a bone graft in the interlaminar space, and additionally securing it with a wire or hook system. Fully threaded screws are often employed, with the primary reliance on fusion in the interlaminar space. Its advantages include that it requires the placement of only two screws without the need for rods, which reduces operative time. However, it permanently fuses the C1–C2 articulation. It is also important to note that this technique is generally contraindicated in patients with high-riding vertebral arteries because, in these cases, the vertebral artery location is typically more medial and more posterior, and reducing the size of the isthmus increases the risk of injury to the artery during screw insertion [66]. However, techniques for mobilizing the artery to allow for the Magerl trans-articular fixation have been described [66].
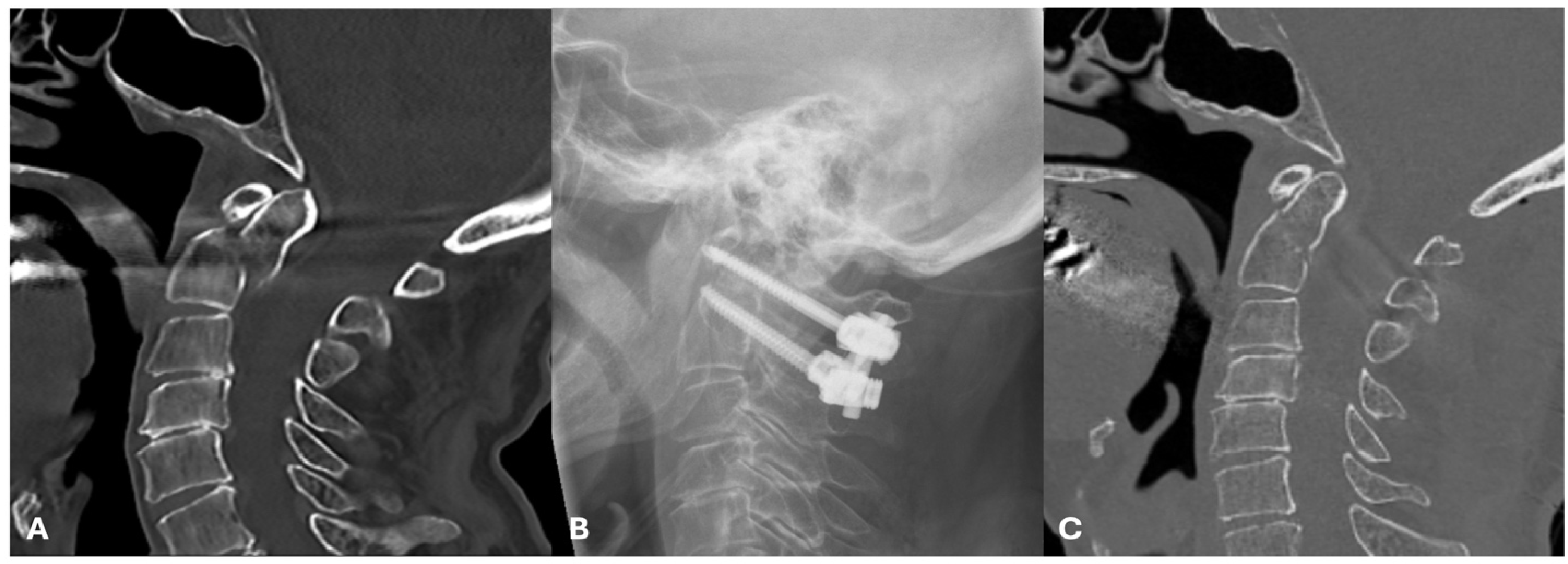
At the present time however, the Goel-Harms technique involving C1 and C2 screws with or without the placement of a bone graft in between the posterior elements of C1–C2 is the most common technique [67,68,69] (Figure 2). This technique represents an alternative to the Magerl technique and involves placement of bilateral C1 lateral mass screws, and C2 pedicle or pars screws, fixed by rods. Some studies have shown that this technique provides the highest rate of union, while others suggest Magerl’s technique is superior. The benefit of the Goel-Harms technique is also that the construct can be removed in younger patients with eventual odontoid union to improve the loss of cervical rotation from fixation [70].
Figure 2.
Clinical Case of an Anderson and D’Alonzo type II, Roy-Camille type II odontoid fracture: (A) Sagittal CT showing the OF, with some minor posterior displacement of C1 relative to C2, (B) postoperative lateral radiograph, showing a posterior C1–C2 fixation using the Harms-Goel technique, and (C) postoperative midline sagittal CT of the cervical spine showing good realignment of the odontoid post fixation.
Posterior surgery before the Magerl and Harms Goel techniques involved wiring or clamping and the placement of bone grafts. An alternative to these methods is stand-alone screw instrumentation, which, due to the compressive effect on the lateral masses, leads to their ankylosis. These techniques can be performed percutaneously or minimally invasively through a transmuscular approach [71,72]. Many different variations of wiring techniques have been reported, but this practice has largely been abandoned in developed countries. In countries with limited resources and in situation where screw placement may not be possible, wiring of the posterior element remains an option. However, for these techniques, the posterior arch of C1 needs to be intact [47]. Iyer et al. [47] provides a brief review detailing these techniques.
9. Non-Operative Treatment
Non-operative management is a viable treatment option in the majority of isolated odontoid fractures, even type II, which are often treated surgically. Typically, this involves a hard collar or halo vest placement, with the latter becoming rarely used because of its morbidity, especially amongst the elderly. However, even the use of hard collars is not without morbidity [73]. Before the placement of rigid collars, attempts are typically made to align fractures with traction, if necessary. The goal of the non-operative treatment is to achieve a fibrous non-union between the two fragments and therefore a “relative stability” of the odontoid. A systematic review including 714 cases with treatment by halo vest or hard collar showed no significant difference in failure rates, but did show a higher rate of complications associated with halo vests [74], supporting the preferential use of hard collars if external immobilization is sought. Of note, the failure rate with non-operative treatment for type II OFs was higher than for type III (20% vs. 7%), and only a single patient in this review was noted to have neurological deterioration with non-operative treatment.
There is an increased consideration for not placing any immobilization devices in patients treated conservatively, and this has resulted in the formulation of a randomized control trial (DENS) to assess collar vs. no collar treatment [75].
10. Outcomes and Complications
The clinical outcome and rate of complications depend on a number of factors, including patient-related factors, the type of fracture, and whether treatment is operative or non-operative. Furthermore, when surgery is performed, the outcomes and complications can vary from anterior and posterior surgery. While many factors can be considered when discussing outcome, the most relevant points related to OFs include rates of union or mechanical stability, wound complications, neck pain, mortality and neurological function. However, it is important to note, as mentioned previously, that short term morbidity and mortality is considerably higher in patients with neurological injury following OFs, regardless of treatment [5,43].
For simplicity, the discussion of outcome and complications is segregated below into two sections: operative vs. nonoperative management and anterior vs. posterior.
10.1. Operative vs. Nonoperative Management
Multiple studies have been conducted to assess the relative merits between operative vs. nonoperative treatment; however, the findings of individual studies have been limited by the lack of randomization, which has a significant impact in selection bias in this largely old and fragile population cohort. Systematic reviews [56,76,77,78,79,80,81], have also been somewhat limited in showing a clear efficacy of one treatment over the other. From these reviews, it appears that there may be a slight survival advantage in operatedpatients; however, since there is an absence of RCTs, this may be due to selection bias. A more consistent finding from these reviews is the higher rate of union with surgical treatment. The most recent meta-analysis showed that fracture stability was observed in 82% and 53% of surgically and conservatively treated patients, respectively [80]. However, the importance of non-union is questionable, while a few patients will suffer from chronic pain due to non-union [45], there is a lack of evidence that non-union results in a worse clinical or function outcome in the elderly [56]. Indeed, many of these patients will develop a malunion, or fibrous non-union, without instability objectified on dynamic imaging, and a systematic review on this population supports these fibrous non-union are generally safe and well tolerated by patients [82]. Though union rates are higher with surgery, it has been shown that delay in the initiation of surgery (>3–7 days) is a significant factor influencing non-union [47,83].
It is clear that to definitively determine whether surgery or conservative management is superior, randomized trials are necessary. In 2014, such a study was proposed and registered [84], but no results have yet been reported.
10.2. Anterior vs. Posterior Surgery
Although indications for anterior or posterior surgery vary, multiple studies and systematic reviews have been carried out to assess the relative superiority of one surgery over the other [59,85,86]. These reviews indicate that posterior fusion has higher union rates, and lower reoperation rates, than anterior screw placement in patients >60 years [59]. However, there do not appear to be differences in mortality. While the occurrence of adverse events was not shown to be different, it is worthy to note that the types of complication between the surgery types differ. In anterior surgery, as with ACDFs, dysphagia and recurrent laryngeal nerve injury complications may occur, while wound infection is extremely rare, but not uncommon with posterior surgery.
11. Conclusions
The number of OFs will continue to rise in populations with aging demographics, and therefore result in an increased health care cost burden. While the management of certain types of fractures are relatively standardized, such as non-operative treatment for type I fractures, the treatment strategy of type II fractures remains variable, with both non-operative and operative treatments being employed, largely due to the heterogenic clinical and radiological variables to consider. Regardless of the treatment, given the advanced age of most patients suffering from OFs, morbidities and mortality are not insignificant, even if optimal treatment strategies are employed. Despite some evidence showing that surgery for type II fractures offers more favorable outcomes, there exists no randomized control studies to support this, and further work in standardizing who benefits most from surgery is necessary.
Author Contributions
Conceptualization, A.N.; validation, M.K. and E.T.; writing—original draft preparation, A.N., G.M., A.M. and M.D.B.; writing—review and editing, A.N., B.D., N.P. and M.D.B.; visualization, M.D.B., A.N. and I.J.; supervision, K.S., E.T. and M.K.; project administration, M.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Not applicable for this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Fredø, H.L.; Rizvi, S.A.M.; Lied, B.; Rønning, P.; Helseth, E. The epidemiology of traumatic cervical spine fractures: A prospective population study from Norway. Scand. J. Trauma Resusc. Emerg. Med. 2012, 20, 85. [Google Scholar] [CrossRef] [PubMed]
- Lakshmanan, P.; Jones, A.; Howes, J.; Lyons, K. CT evaluation of the pattern of odontoid fractures in the elderly—Relationship to upper cervical spine osteoarthritis. Eur. Spine J. 2005, 14, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Zusman, N.L.; Ching, A.C.; Hart, R.A.; Yoo, J.U. Incidence of second cervical vertebral fractures far surpassed the rate predicted by the changing age distribution and growth among elderly persons in the United States (2005–2008). Spine 2013, 38, 752–756. [Google Scholar] [CrossRef] [PubMed]
- Charles, Y.P.; Ntilikina, Y.; Blondel, B.; Fuentes, S.; Allia, J.; Bronsard, N.; Lleu, M.; Nicot, B.; Challier, V.; Godard, J. Mortality, complication, and fusion rates of patients with odontoid fracture: The impact of age and comorbidities in 204 cases. Arch. Orthop. Trauma Surg. 2019, 139, 43–51. [Google Scholar] [CrossRef]
- Harrop, J.; Sharan, A.; Przybylski, G. Epidemiology of spinal cord injury after acute odontoid fractures. Neurosurg. Focus 2000, 8, e4. [Google Scholar] [CrossRef]
- Smith, H.E.; Kerr, S.M.; Fehlings, M.G.; Chapman, J.; Maltenfort, M.; Zavlasky, J.; Harris, E.; Albert, T.J.; Harrop, J.; Hilibrand, A.S. Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a model system spine injury tertiary referral center. Clin. Spine Surg. 2010, 23, 501–505. [Google Scholar] [CrossRef]
- Gonschorek, O.; Vordemvenne, T.; Blattert, T.; Katscher, S.; Schnake, K.J.; Spine Section of the German Society for Orthopaedics and Trauma. Treatment of odontoid fractures: Recommendations of the spine section of the German Society for orthopaedics and trauma (DGOU). Glob. Spine J. 2018, 8, 12S–17S. [Google Scholar] [CrossRef]
- Smith, J.S.; Kepler, C.K.; Kopjar, B.; Harrop, J.S.; Arnold, P.; Chapman, J.R.; Fehlings, M.G.; Vaccaro, A.R.; Shaffrey, C.I. Effect of type II odontoid fracture nonunion on outcome among elderly patients treated without surgery: Based on the AOSpine North America geriatric odontoid fracture study. Spine 2013, 38, 2240–2246. [Google Scholar]
- Anderson, L.D.; D’alonzo, R.T. Fractures of the odontoid process of the axis. J. Bone Joint Surg. Am. 1974, 56, 1663–1674. [Google Scholar] [CrossRef]
- Schatzker, J.; Rorabeck, C.H.; Waddell, J.P. Fractures of the dens [odontoid process] an analysis of thirty-seven cases. J. Bone Jt. Surgery. Br. Vol. 1971, 53, 392–405. [Google Scholar] [CrossRef]
- Hadley, M.N.; Browner, C.M.; Liu, S.S.; Sonntag, V.K. New subtype of acute odontoid fractures (type IIA). Neurosurgery 1988, 22, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Roy-Camille, R.; Saillant, G.; Judet, T.; De Botton, G.; Michel, G. Trans. Factors of severity in the fractures of the odontoid process. Rev. Chir. Orthop. Reparatrice L’appareil Mot. 1980, 66, 183–186. [Google Scholar]
- Grauer, J.N.; Shafi, B.; Hilibrand, A.S.; Harrop, J.S.; Kwon, B.K.; Beiner, J.M.; Albert, T.J.; Fehlings, M.G.; Vaccaro, A.R. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005, 5, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Lambrechts, M.J.; Karamian, B.A.; Canseco, J.A.; Oner, C.; Vialle, E.; Rajasekaran, S.; Dvorak, M.R.; Benneker, L.M.; Kandziora, F. AO Spine upper cervical injury classification system: A description and reliability study. Spine J. 2022, 22, 2042–2049. [Google Scholar] [CrossRef]
- Offiah, C.E.; Day, E. The craniocervical junction: Embryology, anatomy, biomechanics and imaging in blunt trauma. Insights Into Imaging 2017, 8, 29–47. [Google Scholar] [CrossRef]
- Maak, T.G.; Grauer, J.N. The contemporary treatment of odontoid injuries. Spine 2006, 31, S53–S60. [Google Scholar] [CrossRef]
- Govender, S. Fractures of the odontoid process: An angiographic and clinical study. J. Bone Jt. Surg. Br. Vol. 2000, 82, 1143–1147. [Google Scholar] [CrossRef]
- Bogduk, N.; Mercer, S. Biomechanics of the cervical spine. I: Normal kinematics. Clin. Biomech. 2000, 15, 633–648. [Google Scholar] [CrossRef]
- Alluri, R.; Bouz, G.; Solaru, S.; Kang, H.; Wang, J.; Hah, R.J. A nationwide analysis of geriatric odontoid fracture incidence, complications, mortality, and cost. Spine 2021, 46, 131–137. [Google Scholar] [CrossRef]
- Mathkour, M.; Cardona, J.J.; Chaiyamoon, A.; Glynn, R.M.; Jenkins, S.; Graham, R.A.; Johal, J.; Gardner, B.; Iwanaga, J.; Dumont, A.S. Classifications of Odontoid Process Fractures: A Systematic Review and Proposal of a New Simplified Classification System Based on Embryology. Cureus 2022, 14, e32520. [Google Scholar] [CrossRef]
- Rizvi, S.A.M.; Helseth, E.; Rønning, P.; Mirzamohammadi, J.; Harr, M.E.; Brommeland, T.; Aarhus, M.; Høstmælingen, C.T.; Ølstørn, H.; Rydning, P.N.F. Odontoid fractures: Impact of age and comorbidities on surgical decision making. BMC Surg. 2020, 20, 236. [Google Scholar] [CrossRef]
- Falavigna, A.; Righesso, O.; Da Silva, P.G.; Siri, C.R.; Daniel, J.W.; Veiga JC, E.; De Azevedo GB, L.; Carelli, L.E.; Yurac, R.; Chavez, F.A.S. Management of type II odontoid fractures: Experience from Latin American Spine Centers. World Neurosurg. 2017, 98, 673–681. [Google Scholar] [CrossRef]
- Robinson, A.-L.; Olerud, C.; Robinson, Y. Epidemiology of C2 fractures in the 21st century: A national registry cohort study of 6,370 patients from 1997 to 2014. Adv. Orthop. 2017, 2017, 6516893. [Google Scholar] [CrossRef]
- Fehlings, M.G.; Tetreault, L.; Nater, A.; Choma, T.; Harrop, J.; Mroz, T.; Santaguida, C.; Smith, J.S. The aging of the global population: The changing epidemiology of disease and spinal disorders. Neurosurgery 2015, 77, S1–S5. [Google Scholar] [CrossRef]
- Salottolo, K.; Betancourt, A.; Banton, K.L.; Acuna, D.; Panchal, R.; Bar-Or, D.; Palacio, C.H. Epidemiology of C2 fractures and determinants of surgical management: Analysis of a national registry. Trauma Surg. Acute Care Open 2023, 8, e001094. [Google Scholar] [CrossRef]
- Aleissa, S.I.; Alhandi, A.A.; Bugis, A.A.; Alsalamah, R.K.; Alsheddi, A.; Almubarak, A.K.; Alassiri, S.S.; Konbaz, F.M. The incidence of odontoid fractures following trauma in a major trauma center, a retrospective study. J. Craniovertebral Junction Spine 2020, 11, 71. [Google Scholar]
- Robinson, A.-L.; Möller, A.; Robinson, Y.; Olerud, C. C2 fracture subtypes, incidence, and treatment allocation change with age: A retrospective cohort study of 233 consecutive cases. BioMed Res. Int. 2017, 2017, 8321680. [Google Scholar] [CrossRef]
- Alas, H.; Segreto, F.A.; Chan, H.Y.; Brown, A.E.; Pierce, K.E.; Bortz, C.A.; Horn, S.R.; Varlotta, C.G.; Baker, J.F.; Passias, P.G. Association between frailty status and odontoid fractures after traumatic falls: Investigation of varying injury mechanisms among 70 elderly odontoid fracture patients. J. Orthop. Trauma 2019, 33, e484–e488. [Google Scholar] [CrossRef]
- Watanabe, M.; Sakai, D.; Yamamoto, Y.; Nagai, T.; Sato, M.; Mochida, J. Analysis of predisposing factors in elderly people with type II odontoid fracture. Spine J. 2014, 14, 861–866. [Google Scholar] [CrossRef]
- Shinseki, M.S.; Zusman, N.L.; Hiratzka, J.; Marshall, L.M.; Yoo, J.U. Association between advanced degenerative changes of the atlanto-dens joint and presence of dens fracture. J. Bone Joint Surg. Am. 2014, 96, 712–717. [Google Scholar] [CrossRef]
- Emohare, O.; Dittmer, A.; Morgan, R.A.; Switzer, J.A.; Polly, D.W. Osteoporosis in acute fractures of the cervical spine: The role of opportunistic CT screening. J. Neurosurg. Spine 2015, 23, 1–7. [Google Scholar] [CrossRef]
- Kaesmacher, J.; Schweizer, C.; Valentinitsch, A.; Baum, T.; Rienmüller, A.; Meyer, B.; Kirschke, J.S.; Ryang, Y.M. Osteoporosis is the most important risk factor for odontoid fractures in the elderly. J. Bone Miner. Res. 2017, 32, 1582–1588. [Google Scholar] [CrossRef]
- Kohlhof, H.; Seidel, U.; Hoppe, S.; Keel, M.J.; Benneker, L.M. Cement-augmented anterior screw fixation of Type II odontoid fractures in elderly patients with osteoporosis. Spine J. 2013, 13, 1858–1863. [Google Scholar] [CrossRef]
- Miao, J.; Chen, Y.; Zhang, B.; Li, T.; Luo, Y.; Shi, L.; Shi, J.; Chen, D. Surgical treatment for odontoid fractures in patients with long-standing ankylosing spondylitis: A report of 3 cases and review of the literature. World Neurosurg. 2018, 116, 88–93. [Google Scholar] [CrossRef]
- Lewandrowski, K.-U.; Park, P.P.; Baron, J.M.; Curtin, S.L. Atraumatic odontoid fractures in patients with rheumatoid arthritis. Spine J. 2006, 6, 529–533. [Google Scholar] [CrossRef]
- Coyne, T.J.; Fehlings, M.G.; Wallace, M.C.; Bernstein, M.; Tator, C.H. C1–C2 posterior cervical fusion: Long-term evaluation of results and efficacy. Neurosurgery 1995, 37, 688–693. [Google Scholar] [CrossRef]
- Blondel, B.; Litre, F.; Graillon, T.; Adetchessi, T.; Dufour, H.; Fuentes, S. Metastatic odontoid fracture management by anterior screw fixation and kyphoplasty. Neurochirurgie 2013, 59, 191–194. [Google Scholar] [CrossRef]
- Lally, J.; Cossrow, J.; Dalinka, M. Odontoid fractures in metastatic breast carcinoma. Am. J. Roentgenol. 1977, 128, 817–820. [Google Scholar] [CrossRef]
- Cusick, J.F.; Yoganandan, N. Biomechanics of the cervical spine 4: Major injuries. Clin. Biomech. 2002, 17, 1–20. [Google Scholar] [CrossRef]
- Ozdemir, B.; Kanat, A.; Durmaz, S.; Batcik, O.E.; Gundogdu, H. Introducing a new possible predisposing risk factor for odontoid type 2 fractures after cervical trauma; Ponticulus posticus anomaly of C1 vertebra. J. Clin. Neurosci. 2022, 96, 194–198. [Google Scholar] [CrossRef]
- Arvin, B.; Fournier-Gosselin, M.-P.; Fehlings, M.G. Os odontoideum: Etiology and surgical management. Neurosurgery 2010, 66, A22–A31. [Google Scholar] [CrossRef]
- Smoker, W. Craniovertebral junction: Normal anatomy, craniometry, and congenital anomalies. Radiographics 1994, 14, 255–277. [Google Scholar] [CrossRef]
- Patel, A.; Smith, H.E.; Radcliff, K.; Yadlapalli, N.; Vaccaro, A.R. Odontoid fractures with neurologic deficit have higher mortality and morbidity. Clin. Orthop. Relat. Res. 2012, 470, 1614–1620. [Google Scholar] [CrossRef]
- Müller, E.; Wick, M.; Russe, O.; Muhr, G. Management of odontoid fractures in the elderly. Eur. Spine J. 1999, 8, 360–365. [Google Scholar] [CrossRef]
- Ryan, M.D.; Taylor, T. Odontoid fractures in the elderly. J. Spinal Disord. 1993, 6, 397–401. [Google Scholar] [CrossRef]
- Kepler, C.K.; Vaccaro, A.R.; Dibra, F.; Anderson, D.G.; Rihn, J.A.; Hilibrand, A.S.; Harrop, J.S.; Albert, T.J.; Radcliff, K.E. Neurologic injury because of trauma after type II odontoid nonunion. Spine J. 2014, 14, 903–908. [Google Scholar] [CrossRef]
- Iyer, S.; Hurlbert, R.J.; Albert, T.J. Management of odontoid fractures in the elderly: A review of the literature and an evidence-based treatment algorithm. Neurosurgery 2018, 82, 419–430. [Google Scholar] [CrossRef]
- Siddiqui, J.; Grover, P.J.; Makalanda, H.L.; Campion, T.; Bull, J.; Adams, A. The spectrum of traumatic injuries at the craniocervical junction: A review of imaging findings and management. Emerg. Radiol. 2017, 24, 377–385. [Google Scholar] [CrossRef]
- Jain, N.; Verma, R.; Garga, U.N.; Baruah, B.P.; Jain, S.K.; Bhaskar, S.N. CT and MR imaging of odontoid abnormalities: A pictorial review. Indian J. Radiol. Imaging 2016, 26, 108–119. [Google Scholar] [CrossRef]
- Sayama, C.M.; Fassett, D.R.; Apfelbaum, R.I. The utility of MRI in the evaluation of odontoid fractures. Clin. Spine Surg. 2008, 21, 524–526. [Google Scholar] [CrossRef]
- Endler, C.H.; Ginzburg, D.; Isaak, A.; Faron, A.; Mesropyan, N.; Kuetting, D.; Pieper, C.C.; Kupczyk, P.A.; Attenberger, U.I.; Luetkens, J.A. Diagnostic Benefit of MRI for Exclusion of Ligamentous Injury in Patients with Lateral Atlantodental Interval Asymmetry at Initial Trauma CT. Radiology 2021, 300, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, G. Surgical management of odontoid fractures. Injury 2005, 36, S54–S64. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.R.; White, A., 3rd. Fractures of the dens. A multicenter study. J. Bone Joint Surg. Am. 1985, 67, 1340–1348. [Google Scholar] [CrossRef] [PubMed]
- Ekong, C.E.; Schwartz, M.L.; Tator, C.H.; Rowed, D.W.; Edmonds, V.E. Odontoid fracture: Management with early mobilization using the halo device. Neurosurgery 1981, 9, 631–637. [Google Scholar] [CrossRef]
- Guo, Q.; Wang, L.; Lu, X.; Guo, X.; Ni, B. Posterior Temporary Fixation Versus Nonoperative Treatment for Anderson–D’Alonzo Type III Odontoid Fractures: Functional Computed Tomography Evaluation of C1–C2 Rotation. World Neurosurg. 2017, 100, 675–680. [Google Scholar] [CrossRef]
- Robinson, Y.; Robinson, A.-L.; Olerud, C. Systematic review on surgical and nonsurgical treatment of type II odontoid fractures in the elderly. BioMed Res. Int. 2014, 2014, 231948. [Google Scholar] [CrossRef]
- Cloney, M.B.; Thirunavu, V.; Roumeliotis, A.; Texakalidis, P.; Swong, K.; El Tecle, N.; Dahdaleh, N.S. Traumatic Dens Fracture Patients Comprise Distinct Subpopulations Distinguished by Differences in Age, Sex, Injury Mechanism and Severity, and Outcome. World Neurosurg. 2023, 178, e128–e134. [Google Scholar] [CrossRef]
- Avila, M.J.; Farber, S.H.; Rabah, N.M.; Hopp, M.J.; Chapple, K.M.; Hurlbert, R.J.; Tumialán, L.M. Nonoperative versus operative management of type II odontoid fracture in older adults: A systematic review and meta-analysis. J. Neurosurg. Spine 2023, 40, 45–53. [Google Scholar] [CrossRef]
- Texakalidis, P.; Matsoukas, S.; Karras, C.L.; Frankel, H.G.; Swong, K.; Stricsek, G.P.; Dahdaleh, N.S. Outcomes following anterior odontoid screw versus posterior arthrodesis for odontoid fractures: A systematic review and meta-analysis. J. Neurosurg. Spine 2023, 39, 196–205. [Google Scholar] [CrossRef]
- Lehman, R.; Riew, D.; Schnake, K. Occipitocervical trauma. In AO Surgery Reference; Vialle, L., Ed.; AO Foundation: Davos, Switzerland, 2023; Available online: https://surgeryreference.aofoundation.org/spine/trauma/occipitocervical (accessed on 18 September 2024).
- Schwarz, F.; Mclean, A.L.; Waschke, A.; Kalff, R. Cement-augmented anterior odontoid screw fixation in elderly patients with odontoid fracture. Clin. Neurol. Neurosurg. 2018, 175, 144–148. [Google Scholar] [CrossRef]
- Elias, W.J.; Ireland, P.; Chadduck, J.B. Transoral digitally manipulated reduction of a ventrally displaced type II odontoid fracture to aid in screw fixation: Case illustration. J. Neurosurg. Spine 2006, 4, 82. [Google Scholar] [CrossRef] [PubMed]
- Fazzolari, B.; Jannelli, G.; Conti, E.; Delitala, A.; Tessitore, E.; Brunori, A. Clinical and radiological outcome after minimally invasive surgical approach for type II unstable odontoid fractures. Neurochirurgie 2021, 67, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Lvov, I.; Grin, A.; Talypov, A.; Godkov, I.; Kordonskiy, A.; Khushnazarov, U.; Smirnov, V.; Krylov, V. The impact of odontoid screw fixation techniques on screw-related complications and fusion rates: A systematic review and meta-analysis. Eur. Spine J. 2021, 30, 475–497. [Google Scholar] [CrossRef] [PubMed]
- Dailey, A.T.; Hart, D.; Finn, M.A.; Schmidt, M.H.; Apfelbaum, R.I. Anterior fixation of odontoid fractures in an elderly population. J. Neurosurg. Spine 2010, 12, 1–8. [Google Scholar] [CrossRef]
- Goel, A.; Rangnekar, R.; Shah, A.; Rai, S.; Vutha, R. Mobilization of the vertebral artery—Surgical option for C2 screw fixation in cases with “high riding” vertebral artery. Oper. Neurosurg. 2020, 18, 648–651. [Google Scholar] [CrossRef]
- Harms, J.; Melcher, R.P. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine 2001, 26, 2467–2471. [Google Scholar] [CrossRef]
- Du, Y.-Q.; Li, T.; Ma, C.; Qiao, G.-Y.; Yin, Y.-H.; Yu, X.-G. Biomechanical evaluation of two alternative techniques to the Goel-Harms technique for atlantoaxial fixation: C1 lateral mass–C2 bicortical translaminar screw fixation and C1 lateral mass–C2/3 transarticular screw fixation. J. Neurosurg. Spine 2020, 32, 682–688. [Google Scholar] [CrossRef]
- Goel, A.; Laheri, V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir. 1994, 129, 47–53. [Google Scholar] [CrossRef]
- Menendez, J.A.; Wright, N.M. Techniques of posterior C1–C2 stabilization. Neurosurgery 2007, 60, S1–S103. [Google Scholar] [CrossRef]
- Meyer, M.; Farah, K.; Graillon, T.; Dufour, H.; Blondel, B.; Fuentes, S. Minimally Invasive Percutaneous C1-C2 Fixation Using an Intraoperative Three-Dimensional Imaging–Based Navigation System for Management of Odontoid Fractures. World Neurosurg. 2020, 137, 266–271. [Google Scholar] [CrossRef]
- Dimitriou, J.; Garvayo, M.; Coll, J.B. Minimally invasive posterior percutaneous transarticular C1–C2 screws: How I do it. Acta Neurochir. 2020, 162, 2047–2050. [Google Scholar] [CrossRef] [PubMed]
- Brannigan, J.F.; Dohle, E.; Critchley, G.R.; Trivedi, R.; Laing, R.J.; Davies, B.M. Adverse events relating to prolonged hard collar immobilisation: A systematic review and meta-analysis. Glob. Spine J. 2022, 12, 1968–1978. [Google Scholar] [CrossRef] [PubMed]
- Waqar, M.; Van-Popta, D.; Barone, D.G.; Sarsam, Z. External immobilization of odontoid fractures: A systematic review to compare the halo and hard collar. World Neurosurg. 2017, 97, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Woodfield, J.; Edlmann, E.; Black, P.L.; Boyd, J.; Copley, P.C.; Cranswick, G.; Eborall, H.; Keerie, C.; Khan, S.; Lawton, J. Duration of External Neck Stabilisation (DENS) following odontoid fracture in older or frail adults: Protocol for a randomised controlled trial of collar versus no collar. BMJ Open 2022, 12, e057753. [Google Scholar] [CrossRef]
- Sarode, D.P.; Demetriades, A.K. Surgical versus nonsurgical management for type II odontoid fractures in the elderly population: A systematic review. Spine J. 2018, 18, 1921–1933. [Google Scholar] [CrossRef]
- Fan, L.; Ou, D.; Huang, X.; Pang, M.; Chen, X.-X.; Yang, B.; Wang, Q.-Y. Surgery vs conservative treatment for type II and III odontoid fractures in a geriatric population: A meta-analysis. Medicine 2019, 98, e10281. [Google Scholar] [CrossRef]
- Schroeder, G.D.; Kepler, C.K.; Kurd, M.F.; Paul, J.T.; Rubenstein, R.N.; Harrop, J.S.; Brodke, D.S.; Chapman, J.R.; Vaccaro, A.R. A systematic review of the treatment of geriatric type II odontoid fractures. Neurosurgery 2015, 77, S6–S14. [Google Scholar] [CrossRef]
- Huybregts, J.G.; Jacobs, W.C.; Vleggeert-Lankamp, C.L. The optimal treatment of type II and III odontoid fractures in the elderly: A systematic review. Eur. Spine J. 2013, 22, 1–13. [Google Scholar] [CrossRef]
- Huybregts, J.G.; Barot, K.A.; Recio, C.; Doucette, J.; Mekary, R.A.; Vleggeert-Lankamp, C.L. The optimal treatment of type II and III odontoid fractures in the elderly: An updated meta-analysis. Eur. Spine J. 2023, 32, 3434–3449. [Google Scholar] [CrossRef]
- Pommier, B.; Ollier, E.; Pelletier, J.-B.; Castel, X.; Vassal, F.; Tetard, M.-C. Conservative versus surgical treatment for odontoid fracture: Is the surgical treatment harmful? Systematic review and meta-analysis. World Neurosurg. 2020, 141, 490–499.e2. [Google Scholar] [CrossRef]
- Florman, J.E.; Gerstl, J.V.; Kilgallon, J.L.; Riesenburger, R.I. Fibrous nonunion of odontoid fractures: Is it safe to accept nonoperative management? A systematic review. World Neurosurg. 2022, 164, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Ricciardi, L.; Trungu, S.; Scerrati, A.; De Bonis, P.; Rustemi, O.; Mazzetto, M.; Lofrese, G.; Cultrera, F.; Barrey, C.Y.; Di Bartolomeo, A. Odontoid screw placement for Anderson type II odontoid fractures: How do duration from injury to surgery and clinical and radiological factors influence the union rate? A multicenter retrospective study. J. Neurosurg. Spine 2020, 34, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Huybregts, J.G.; Jacobs, W.C.; Peul, W.C.; Vleggeert-Lankamp, C.L. Rationale and design of the INNOVATE Trial: An international cooperative study on surgical versus conservative treatment for odontoid fractures in the elderly. BMC Musculoskelet. Disord. 2014, 15, 7. [Google Scholar] [CrossRef] [PubMed]
- Bao, X.; Chen, Y.; Guo, C.; Xu, S. Comparison of anterior and posterior approaches in Treating odontoid fractures: A meta-analysis and systematic review. Front. Surg. 2023, 10, 1125665. [Google Scholar] [CrossRef]
- Shen, Y.; Miao, J.; Li, C.; Fang, L.; Cao, S.; Zhang, M.; Yan, J.; Kuang, Y. A meta-analysis of the fusion rate from surgical treatment for odontoid factures: Anterior odontoid screw versus posterior C1–C2 arthrodesis. Eur. Spine J. 2015, 24, 1649–1657. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).