Abstract
The main objective was to perform a description of the potential biobehavioral factors that influence disability in patients with migraines and develop a multimodal physiotherapy treatment proposal incorporating therapeutic education and exercise prescription, applying a biobehavioral approach. This manuscript highlights the complex interplay between migraines and physical activity, with many migraine sufferers performing reduced physical activity, even during headache-free intervals. The kinesiophobia present in a significant portion of patients with migraine exacerbates functional disability and compromises quality of life. Psychological elements, especially pain catastrophizing, depression, and self-efficacy, further compound migraine-related disability. Addressing these issues requires a multidisciplinary approach that integrates physical activity and behavioral interventions. We propose a therapeutic education model of motor behavior that emphasizes the enhancement of therapeutic exercise outcomes. This model consists of the four following phases: (1) biobehavioral analysis of movement; (2) goal setting; (3) education about exercise benefits; and (4) movement education. A notable feature is the incorporation of motivational interviewing, a communication strategy that amplifies intrinsic motivation for change. Recent clinical guidelines have advocated for specific exercise modalities to ameliorate migraine symptoms. However, we highlight the importance of a tailored exercise prescription to maximize the benefits of exercise and reduce the possible adverse effects. The integration of exercise with other lifestyle recommendations, such as maintaining consistent sleep patterns and employing stress management techniques, is pivotal for improving outcomes in patients with migraine. Although evidence supports the benefits of these interventions in various painful conditions, further research is needed to establish their efficacy specifically for migraine management.
1. Introduction
Migraine is a debilitating neurological disorder [1], affecting over a billion individuals globally. It is frequently characterized by recurrent and taxing headaches, some of which are accompanied by an aura [2,3]. This disorder imposes a significant economic burden worldwide, detrimentally impacting the person with migraine’s quality of life, as well as their family, coworkers, and society at large [2,4,5].
In terms of prevalence, migraines are considered the second most significant contributor to disability on a global scale, and the foremost cause of disability among young women [6]. The profound effect of migraines on quality of life cannot be understated, due to its influence on professional spheres, family, and social relationships, resulting in pronounced emotional decline [7,8].
Migraine pathophysiology is associated with various alterations in both the central and peripheral nervous systems [1]. Neuroimaging and electrophysiological studies have identified both structural and functional aberrations in the brains of patients with migraine [9,10,11,12]. Spread depolarization appears to be the root cause of the aura and can also trigger trigeminal sensory activation, which is the underlying mechanism of headache pain [3]. Theoretical models applied to patients with migraines suggest that augmented and sustained pain perception induces neuroplastic changes in the central nervous system [13]. These changes potentially impact motor behavior and are influenced by contextual and cognitive–emotional factors (fear-avoidance beliefs, feelings of reduced self-efficacy, catastrophic cognition, and increased depressive symptoms) [14,15,16]. It is suggested that maladaptive changes in motor behavior can heighten disability levels and pain perception and can further reduce quality of life [17].
Understanding migraines from a biobehavioral perspective entails acknowledging their biological foundations and their interplay with psychological elements pertinent to patients’ symptomatology. Those with migraines frequently endure psychological distress, including symptoms of depression and anxiety, and they face societal stigma and misunderstanding [7,8,18,19]. Research has shown that psychological elements, such as anxiety, depression, and pain catastrophizing, show a robust relationship with migraine disability [20]. A meta-analysis performed by Waliszewska-Prosól et al. (2024) revealed that the pooled mean value for the MIDAS questionnaire score obtained by migraine patients in different studies was 36.8, with 62.3 for HIT-6 and 58.1 for HDI [21]. A score higher than 21 on the MIDAS questionnaire is considered a severe disability [22], more than 60 on the HIT-6 is regarded as a very severe disability [23], and more than 50% is also interpreted as a severe disability in the HDI questionnaire [24]. Considering the high disability present in these patients, and its association with the mentioned psychological factors, the management of these barriers might be crucial for decreasing the impact of this condition in patients’ lives.
The therapeutic landscape of migraines has been extensively researched and reviewed, covering both pharmacological and non-pharmacological treatments [3,25,26]. Although drugs are the typical treatment, they pose challenges, such as drug interactions, patient response variability, and safety concerns, which are intensified when polytherapy is required to address comorbidities or to achieve a sufficient therapeutic effect [26].
Given the heterogeneity in treatment response, it is important to consider the patients’ perspectives. Qualitative studies delving into the views of those with migraines have highlighted challenges in accessing healthcare, establishing relationships with providers, having aversions to prescribed medications, and a preference for non-drug treatments [25]. They have also highlighted the importance of understanding the social implications and diagnosis, as well as knowing the potential migraine triggers.
Beyond pharmacological approaches, behavioral interventions have emerged as a promising alternative that is backed by robust scientific evidence. Effective patient–healthcare provider communication is essential, recognizing individual factors influencing migraine onset and management [27]. Among behavioral strategies, exercise, notably aerobic, has been pinpointed as a promising preventive treatment, with significant symptomatic improvements having been observed [28]. Such is the impact of exercise on these patients that various scientific societies related to headaches have included exercise as part of their non-pharmacological treatment recommendations [29,30,31]. Moreover, multiple authors have highlighted the efficacy of behavioral interventions, such as relaxation and biofeedback, in migraine prevention and management [27,32,33]. When combined with pharmacotherapy, these techniques have proven particularly advantageous [27].
This manuscript will describe the potential biobehavioral factors influencing disability and other alterations affecting patients with migraine. Furthermore, it will detail a multimodal physiotherapy approach plan grounded in a biobehavioral framework, incorporating therapeutic education and an evidence-based exercise prescription.
2. Migraines and Physical Activity
The nexus between physical activity (PA) and migraines has been scrutinized in various scientific contexts. Though findings differ, creating a complex and intricate landscape, PA remains a pivotal topic in therapeutic and diagnostic approaches, particularly from a physiotherapy perspective.
The relationship between physical activity and migraines has been extensively investigated in numerous studies. While intense exercise can act as a trigger for attacks in certain individuals, it has also been shown to play a prophylactic role in reducing the frequency and severity of migraine episodes. In a comprehensive review, Amin et al. (2018) analyzed the evidence from epidemiological, therapeutic, and pathophysiological perspectives, highlighting that potential triggering mechanisms include the release of neuropeptides, such as calcitonin gene-related peptide (CGRP), and alterations in lactate metabolism during physical activity. However, regular exercise may also increase the migraine activation threshold, acting as a protective factor in individuals who engage in it frequently [34].
Regarding prevalence, Koppen and Van Veldhoven (2013) reported that approximately 38% of patients experienced exercise-induced migraines, with neck pain being a more common initial symptom in these episodes compared to their typical migraines [35]. However, Varkey et al. (2017) observed that after subjecting migraine patients to maximal exercise tests, not all experienced attacks, suggesting significant variability in individual susceptibility to exercise triggers [36]. This variability may be influenced by factors such as the baseline frequency of migraine attacks.
On the other hand, the intentional avoidance of exercise is a frequent phenomenon among migraine patients, as noted by Farris et al. (2018, 2019). These studies reveal that avoidance of physical activity, especially high-intensity exercise, is associated with a higher frequency of migraine attacks, suggesting that physical inactivity could contribute to the perpetuation of migraine episodes [37]. Additionally, patients who avoid physical activity tend to believe that exercise will worsen their symptoms, highlighting the need for interventions aimed at modifying these erroneous beliefs and promoting controlled physical activity as part of comprehensive migraine management [38].
Several researchers have evaluated the PA levels of patients with migraine in comparison to asymptomatic participants and those with other headache types. In this context, Rogers et al. (2020) compared PA levels among adolescents with migraines, those experiencing tension-type headaches, and headache-free controls. Those with migraines displayed reduced overall PA compared with those without headaches, not solely during headache episodes but also on days without headaches, suggesting a general reduction in PA for migraine-afflicted individuals [39]. Aligning with these findings, Stronks et al. discerned that patients with migraines, while having heart rates comparable to controls, were notably less physically active in their routine settings. Moreover, their bodily motion during activity was subpar compared with controls. These interictal phenomena of low physical activity reinforce the chronic impact of migraines on patients’ daily lives [40].
Physical inactivity seems to also contribute to migraine onset. As posited by Varkey et al., those with a sedentary lifestyle had a heightened probability of developing non-migraine headaches a decade later. Furthermore, reduced PA was correlated with a surge in both migraine and non-migraine headache prevalence [41]. Reinforcing these findings, recent research has illustrated that inactive individuals have a higher migraine prevalence compared with their active or highly active counterparts. Notably, population-based studies showed that PA levels were inversely associated with depression, anxiety, negative self-perceived health, and analgesic use [42], as well as headache disability [43].
Compelling data have also emerged from the ELSA-Brasil cohort studies [44,45], which pointed to a link between physical inactivity and the frequency of migraine attacks. These findings suggest that adhering to World Health Organization (WHO) PA guidelines could mitigate migraine occurrence, with leisure-time PA being especially significant [44]. Further findings from the same cohort (2022) highlighted that those meeting the WHO’s PA criteria had a decreased migraine occurrence. Moreover, the type and intensity of PA could have distinct roles concerning migraine subtype [45]. In the All of Us study, a prospective study with 6042 participants using wearable devices and analyzed during a 4-year period, each additional increment of 1000 daily steps beyond the sample median resulted in an 8% reduction in the incidence of migraines [46]. The study by Domingues et al. (2011) noted reduced functional disability in a sample of medical students with migraine who engaged in PA [47].
Conversely, Bond et al. found that women with obesity and migraines spent approximately 1.5 fewer hours per day performing PA compared with controls. Intriguingly, this reduced PA was not linked to the clinical characteristics of their migraines. This study accentuates the imperative to explore the barriers to PA in these women [48]. The migraine–body composition relationship extends beyond mere PA levels. A systematic review and meta-analysis identified a potential link between migraine and obesity, which may be influenced by gender and the frequency of migraine episodes [49]. Another meta-analysis highlighted that migraine risk is elevated in both individuals with obesity and in those below the normative weight [50].
3. Migraines, Kinesiophobia, and Physical Activity Avoidance Behavior
Kinesiophobia, defined as “an exaggerated, irrational, and debilitating fear of physical movement and activity stemming from a sense of vulnerability to painful or new injuries” [51,52] has been associated with functional disability and pain intensity [53,54]. Some authors have speculated that kinesiophobia impacts approximately 51% to 72% of individuals suffering from chronic pain [55,56,57].
Regarding prevalence, Benatto et al. (2019) reported kinesiophobia’s presence in approximately half of those with migraines, correlating with cutaneous allodynia severity. In this study, patients with migraine often believed that PA might not alleviate their pain, and those with kinesiophobia assumed exercise might be detrimental [58].
In relation to migraine symptoms, Altay and Celenay (2023) probed the relationship between cutaneous allodynia and kinesiophobia in individuals diagnosed with migraines. Their findings unveiled a correlation between the severity of cutaneous allodynia and kinesiophobia, gastrointestinal symptoms, and migraine-related disability [59].
Disability remains paramount in diagnostic and therapeutic strategies concerning migraines. Some observations have found that the presence of kinesiophobia is associated with higher levels of migraine-related disability, an augmented fear of falls, and dizziness-induced impairment [60].
PA avoidance behaviors are a pronounced trait amongst those with migraine. During migraine episodes, an exacerbation of pain linked to motion and a consequential avoidance of certain movements (such as head motion and forward inclination) have been identified. Notably, these manifestations were distinctively prevalent and specific in individuals with migraines, contrasting with other headache typologies [61]. Moreover, Farris et al. (2019) elucidated that anxiety sensitivity, or an apprehension regarding bodily sensations, might be correlated with deliberate PA evasion in women predisposed to migraines [38]. Such insights suggest that fear-based cognition could be pivotal in shaping the exercise and movement choices of these patients.
Extending the discourse to a broader paradigm, Ruscheweyh et al. (2019) probed the association between pain avoidance and resilience in migraine contexts. Their study unveiled a positive association between social avoidance behaviors and pain-induced disability [62]. Consequently, such behaviors might exacerbate the disability engendered by migraines, curtailing the overall quality of life in affected individuals.
4. Depression, Self-Efficacy, Catastrophizing, and Migraine-Related Disability
Many studies have delved into the multifaceted characteristics and elements associated with migraine, encompassing psychological facets such as pain catastrophizing, depression, and self-efficacy. Klonowski et al. (2022) highlighted that psychological factors exhibit a stronger association with the perceived level of headache-related disability rather than with pain frequency [63]. Emotional states undeniably play a pivotal role in these patients. Corroborating this, Kim et al. (2021) showed altered emotional responses to pain perception in patients with migraines, identifying pain-related anxiety as a significant influencer of headache-associated disability [64].
Elsewhere, D’Amico et al. (2015) postulated that the incorporation of psychosocial variables into assessment protocols could enhance our comprehension and management of headache-associated impairment and quality of life among individuals suffering from migraines [65].
Recent observations indicate that even in those without coexisting psychiatric conditions, particular behavioral and psychological elements correlate with migraines, notably those categorized as chronic [66]. This investigation determined that patients with chronic migraines manifest heightened tendencies toward pain catastrophizing, showcasing more pronounced cognition related to helplessness and rumination compared with episodic migraine and asymptomatic controls.
Pain catastrophizing, defined as a negative cognitive and emotional response to pain, emerges as a potent determinant in pain perception and management among those with migraines [67]. Studies, including that of Mortazavi Nasiri et al. (2017), have discerned a positive correlation of pain catastrophizing with headache-related disability. Intense pain, as elucidated by their research, mediates this relationship, suggesting that maladaptive coping strategies, such as catastrophizing, might exacerbate pain experiences in these patients [68]. Additionally, Bond et al. (2015) reported that 25% of participants with migraines and obesity exhibited clinical catastrophization, which correlated with an increased frequency of attacks and a worse pain impact [69].
Conversely, the role of self-efficacy—defined as the belief in one’s ability to manage and overcome challenges—is instrumental in the context of migraines. Yousefi Afrashteh et al. (2023) found that pain self-efficacy mediated the perception of life’s meaning, social support, spiritual well-being, and pain catastrophizing with quality of life in individuals suffering from migraines [70]. In essence, the belief in one’s capability to manage pain could influence how migraine is experienced and its impact on daily life.
From another perspective, Woldeamanuel et al. (2020) offered an intriguing insight by identifying distinct natural clusters in patients with chronic migraine. Patients with higher levels of self-efficacy and physical activity reported less migraine-related disability, depression, and other symptoms [71].
It is vital to note that various psychological variables can impact pain perception and headache-related perception. Self-efficacy emerges as a crucial factor to counter and mitigate the adverse effects of migraines, whereas pain catastrophization acts as a barrier that intensifies some migraine-related symptoms. It is imperative for physiotherapists to recognize the complexity and multidimensionality of migraines to be able to provide more effective active treatment strategies.
5. Behavioral Modifications, Lifestyle Changes, and Physical Activity in Migraine Management
The significance of maintaining a consistent and healthy lifestyle is a recurrent theme in migraine literature. It has been highlighted that significant disruptions in daily routines, such as skipping meals or altering sleep patterns, correlate with the onset of migraine attacks [72]. Prior research has evaluated regular lifestyle behaviors, including sleep, exercise, meal patterns, and hydration, and found them to independently influence migraine occurrences. For example, in the study developed by Merril and Gibbons (2023), sleep disorders were associated with a 130% higher risk of having migraines. If participants had sleep disorders in conjunction with mental illness, this risk heightened to 289% [73]. Patients with chronic migraines exhibited fewer consistent lifestyle behaviors compared with those with episodic migraines [74]. Along these lines, the literature accentuates the pertinence of addressing health-related behaviors in episodic migraines, given that disruptions in daily routines and fluctuations in stress, sleep, and other factors can modulate both migraine onset and severity [75].
Although pharmacotherapy plays an indispensable role in migraine treatment, various studies have underscored the significance of lifestyle interventions in managing the frequency and severity of migraines, including modifications in stress management, establishing regular sleep patterns, maintaining a balanced diet, and performing physical activity [76]. In this context, maintaining consistent health behaviors is vital. Rosenberg et al. (2018) advise that because establishing and maintaining behavioral changes is challenging, they ought to be bolstered by a multidisciplinary team, and they posit that consistent daily routines could be an important tool for enhanced migraine management [75].
Among the recommended lifestyle modifications, exercise is most prominent. Barber and Pace (2020) offered a review of the contribution of exercise in migraine prevention, elucidating its potential biological and psychological benefits in migraine management. They highlighted how exercise can attenuate inflammatory markers and how an aerobic exercise regimen can markedly diminish migraine frequency and intensity [77]. In line with this, Oliveira et al. (2017), in a randomized controlled trial, probed how aerobic exercise might correlate with changes in plasma cytokine concentrations and its association with migraine prevention. Their study found that exercise induced a decline in migraine days, anxiety levels, and plasma cytokine (interleukin-12p70) levels [78]. There were significant correlations between the post-intervention levels of interleukin-12p70 levels, migraine days and anxiety scores, with the authors proposing a specific anti-inflammatory mechanism through which regular aerobic exercise could prevent migraines [78].
Addressing exercise as a preventive agent in a cohort study, Hagan et al. (2021) pinpointed how routine moderate-to-vigorous aerobic exercise (three times a week) might correlate with a reduction in headache frequency among adults with episodic migraines. This research suggests that exercise could be beneficial, especially for those already on prophylactic medication, emphasizing the merits of a combined approach [79]. This reduction in migraine frequency and other symptoms, such as migraine intensity and duration, has been observed in different clinical trials in which moderate, continuous aerobic exercise has been evaluated against usual care alone [80,81,82]. Similarly, high-intensity aerobic exercise has also been shown to reduce these symptoms in various clinical trials [82,83,84].
Other exercise modalities, such as yoga or resistance training, have also demonstrated a possible reduction in migraine symptoms and disability [85,86,87,88,89,90,91,92], showing that different exercise options may be accounted for in managing migraines. Likewise, a recently published network meta-analysis showed that yoga and moderate and high-intensity aerobic exercise were significantly superior to pharmacological treatment alone. However, the quality of evidence was very low for all these approaches [93].
6. Multimodal Physiotherapy in Patients with Migraine, Based on a Biobehavioral Approach
The biobehavioral paradigm for the assessment and management of patients with pain-related disorders accentuates the interplay of psychological factors, including learning history, present emotional and cognitive states, beliefs, acquired behaviors, and coping mechanisms and skills, alongside physiological disorders that influence the perception of pain and associated disability [94]. The interaction between comorbidities, such as psychiatric or other inflammatory diseases, external stressors, such as a low socioeconomic status or night-shift jobs, and migraines, which are characterized by an altered pain-processing and cortical hyper-responsiveness, frequently results in a worsening of the symptoms and a higher disability [19]. From a therapeutic standpoint, this model equips patients with the capability to self-manage pain, thereby enhancing overall functioning [95]. Given the biobehavioral traits associated with patients with migraines, we posit this model as a prime candidate for application within the physiotherapy approach.
Physiotherapy with a biobehavioral focus is defined as a therapeutic practice that combines evidence-based interventions with a multidimensional viewpoint, embracing both biological and psychosocial factors in patient diagnosis and treatment [19]. This therapeutic modality is anchored within a framework that centralizes the patient within the care paradigm, fostering a holistic understanding of their needs and circumstances [19]. Furthermore, within this approach, therapeutic procedures and decisions are navigated and recalibrated through structured clinical reasoning processes, ensuring a coherent, efficacious, and individually tailored intervention. Notwithstanding, some barriers can be present for this model, highlighting the need for the adequate structuring of this approach, given the high variability of interventions shown in studies [19].
A multimodal physiotherapy approach grounded in a biobehavioral paradigm integrates treatments such as patient therapeutic education, therapeutic exercise, and orthopedic manual therapy, among others. Evidence for this approach has been documented in patients with chronic neck pain [96], chronic lower back pain [97], temporomandibular disorders [98], chronic tension-type headache [99], and radial nerve injuries [100].
Our therapeutic proposition for addressing patients with migraines is rooted in this biobehavioral paradigm. Although there is abundant evidence on the efficacy of various therapeutic exercise prescription modalities in patients with migraines, there is currently no scientific evidence on the effect of combining patient therapeutic education with exercise. Evidence has showcased the impact of therapeutic education on reducing the frequency, intensity, and disability of patients with migraine [101]. Additionally, prior scientific findings delineate how educational strategies influence the outcomes of therapeutic exercise [102,103,104]. Therapeutic patient education is defined as “a therapeutic modality that explicitly entails a dynamic communication and interaction system with the patient, grounded in a biobehavioral paradigm, incorporating educational or formative activities that promote learning and the acquisition of adaptive skills to bolster self-management and knowledge, facilitating shifts in beliefs, attitudes, and behaviors associated with functional loss” [105].
7. A New Model of Therapeutic Education in Motor Behavior
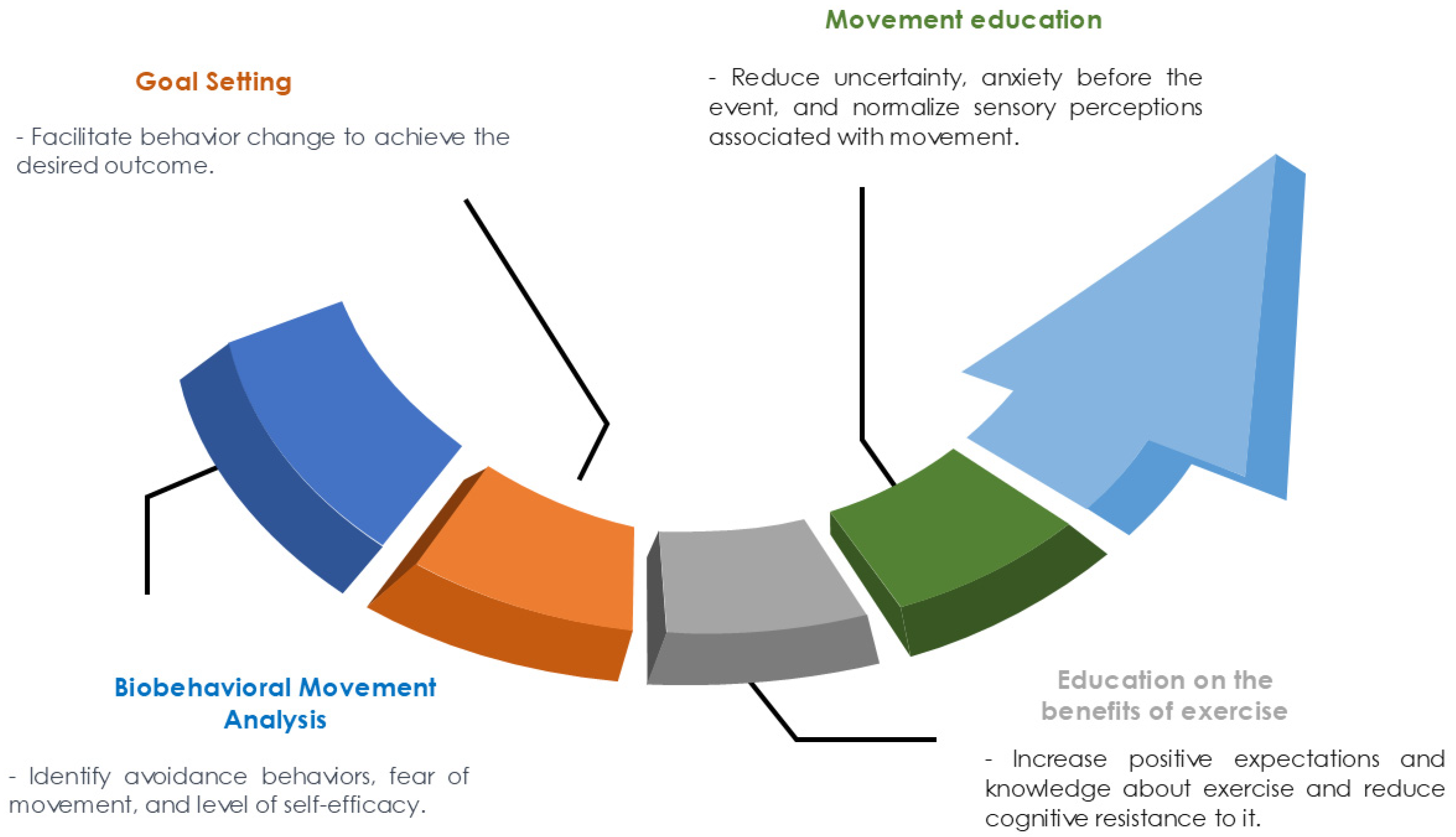
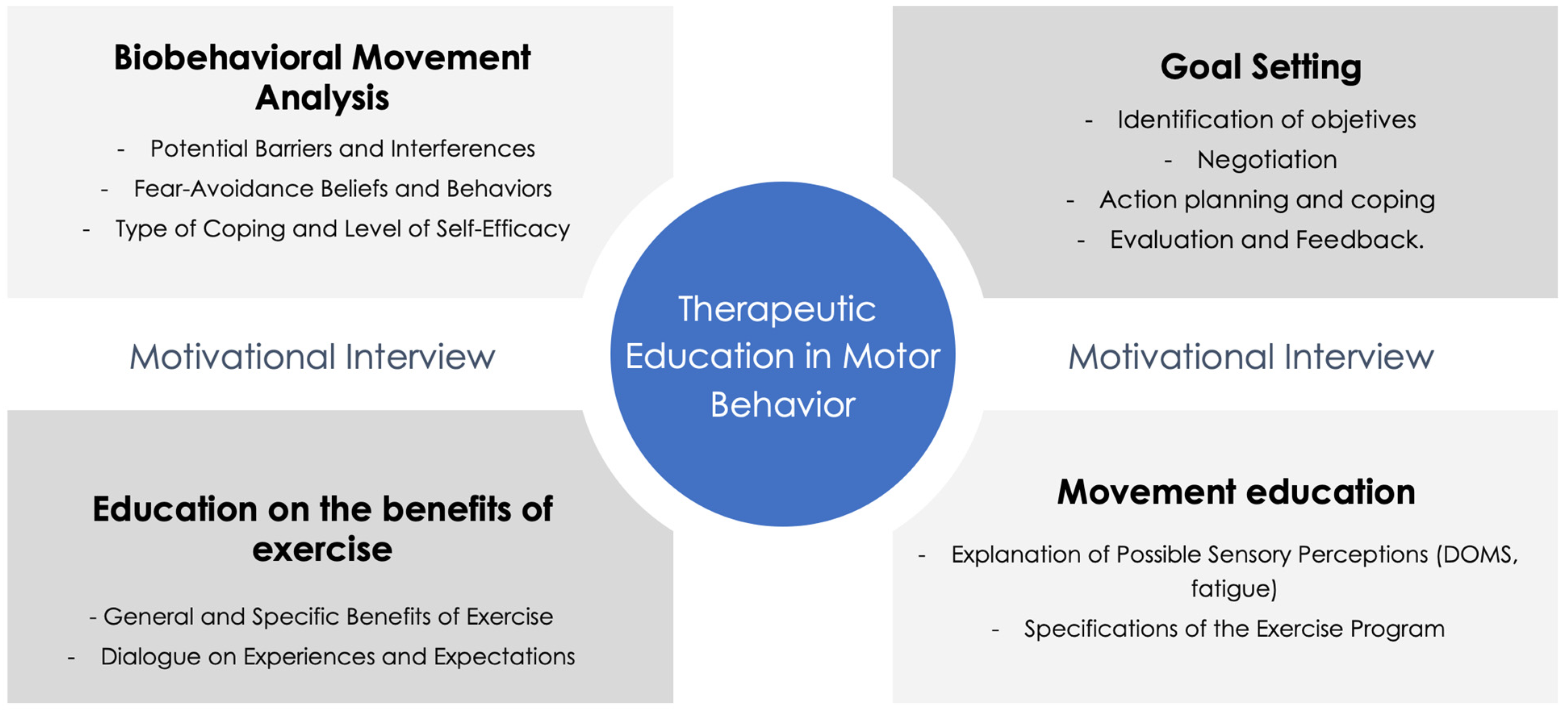
We propose a therapeutic education model for patients with migraines focused on increasing the effects of therapeutic exercise, which we call “therapeutic education in motor behavior”. The model establishes the four following processes or phases of action: (1) a biobehavioral analysis of movement; (2) goal setting; (3) education on the benefits of exercise; and (4) education on movement (Figure 1). The model uses motivational interviewing as a communication method for improving the motivation intrinsic to change (Figure 2).
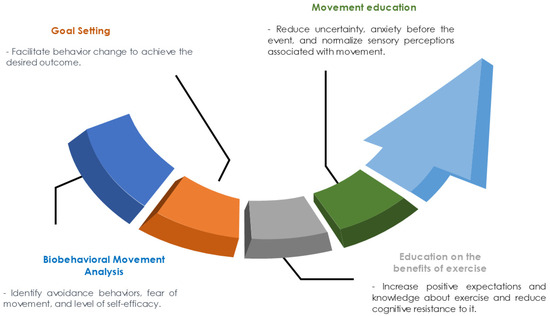
Figure 1.
Therapeutic education on motor behavior.
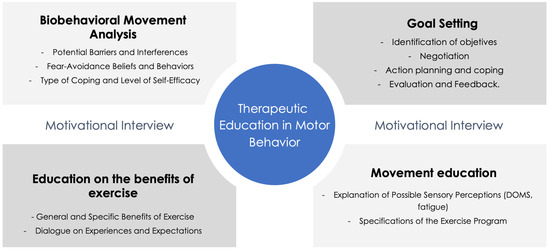
Figure 2.
Conceptual framework for therapeutic education on motor behavior.
7.1. Biobehavioral Movement Analysis
This phase is essential when determining the behavioral, cognitive, motivational, and emotional factors that affect the practice of therapeutic exercise. The analysis uses interviews, self-recordings, and a qualitative analysis of movement. During the analysis, it is important to identify avoidance behaviors, fear of movement, and self-efficacy levels.
7.2. Goal Setting
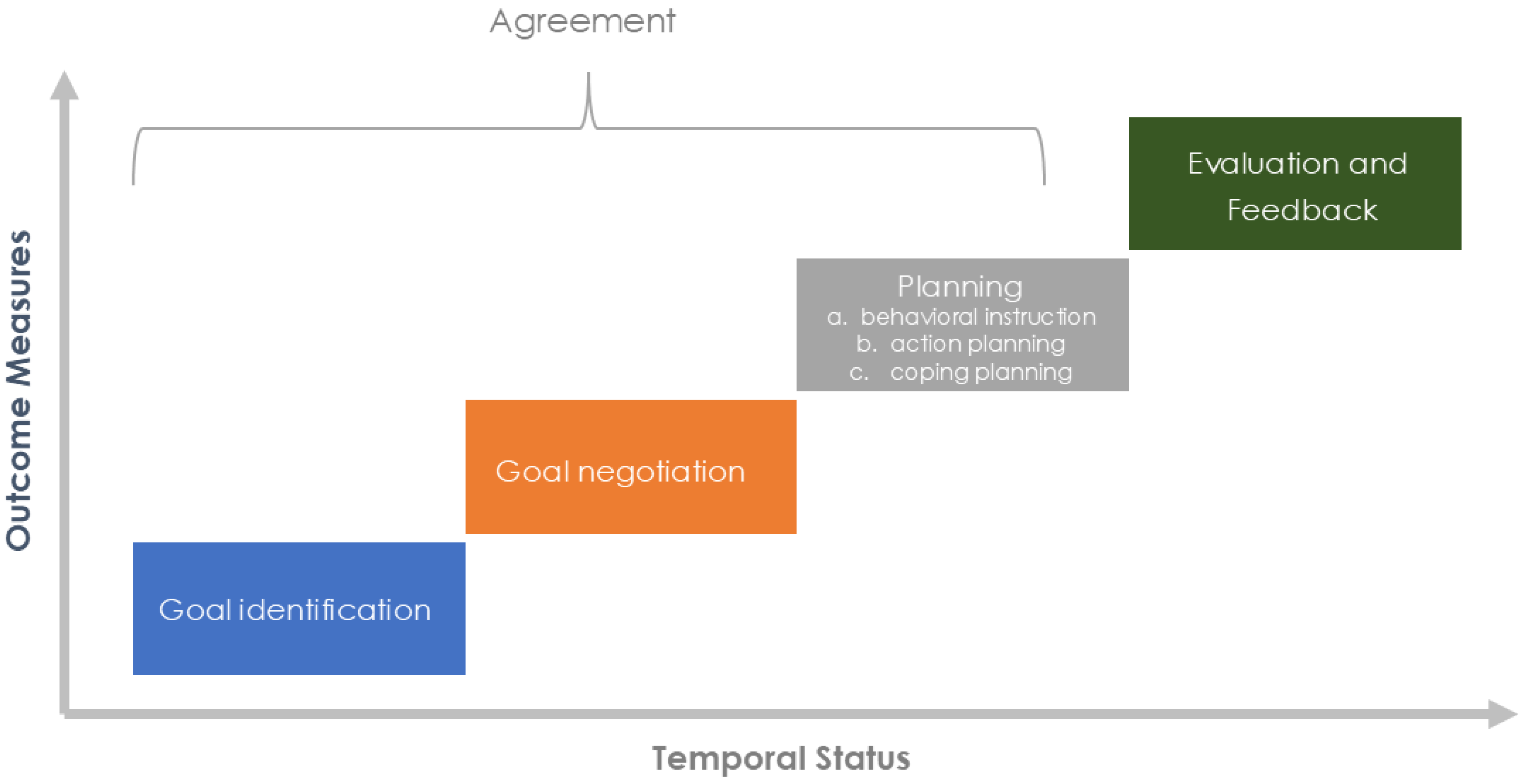
Goal setting is a collaborative process between patients and clinicians that seeks to facilitate behavioral change to achieve the desired outcome [106]. Several theories (such as the goal-setting theory, the health action process approach, and Bandura’s social learning theory) provide a rationale for the process of achieving and setting goals [107,108].
In practical terms, goal setting should be developed by applying the following components: goal negotiation, goal identification, planning (action planning and coping), evaluation, and feedback [108] (Figure 3). Goal setting should also have realistic and specific goals for the patient’s condition, created with short-term goals, quantified with reliable measurements, and established based on agreement with the patients.
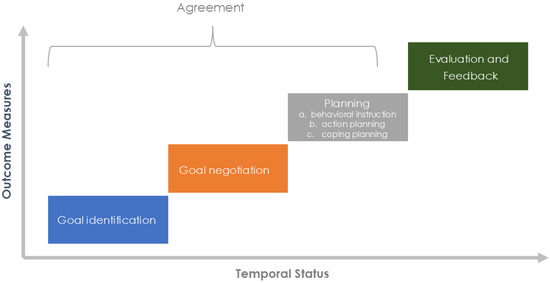
Figure 3.
Goal-oriented therapeutic process.
There are three pedagogical strategies developed during or after goal setting, detailed as follows: (1) behavioral instruction, which is based on introducing content that helps the patient incorporate and perform the exercises in their daily routine; (2) action planning, which are specific plans for achieving the objective; and (3) coping planning, in which plans are established that describe how to overcome potential barriers.
7.3. Education on the Benefits of Exercise
In this phase, the patient is educated on the positive effects of exercise in general and its possible effects on their signs and symptoms. The model is designed to allow patients to express their experiences and expectations regarding exercise. The aim of this phase is for the patient to increase their knowledge regarding exercise, increase their positive expectations, and reduce their cognitive resistance to exercise.
7.4. Movement Education
This phase includes the essential aspect that patients should know, which is the possible perceptions associated with exercise that can occur during and after the practice. This knowledge could help patients reduce their uncertainty and stress before exercising and normalize those perceptions (e.g., informing patients that the exercise can initially result in post-exercise muscle soreness, which will eventually disappear as the body physically adapts to the exercise program). It is also relevant to explain to the patients about the signs of fatigue and how to discriminate between fatigue and other symptoms.
Movement education also includes learning about the program’s specifications (exercise modalities, types of exercise, physical skills to be developed, physiological adaptations to be achieved).
8. Integration of the Motivational Interview in Therapeutic Education
This model of therapeutic education uses motivational interviewing as a communication technique to enhance the intrinsic motivation to change. Motivational interviewing is a highly effective communication method for physical therapy practice and is defined as a collaborative, goal-oriented, person-centered method to increase intrinsic and autonomous motivation for change [109,110], and it is a method often used as a synonym for person-centered counseling [110]. Miller and Rose (2009) have noted that motivational interviewing is relatively brief, applicable to a wide range of problem areas, complementary to other active treatment methods, and can be learned by a wide range of professionals in clinical settings [111]. Evidence has suggested that when motivational interviewing is combined with active therapy, the effect size is larger [112] and the effect is more durable [113]. Tuccero et al. (2016), suggested that motivational interviewing is effective when combined with other therapeutic approaches, such as education and cognitive–behavioral therapy [114].
Motivational interviewing focuses on the language of change and is defined by the application of communication techniques, including the use of open-ended questions, making statements, engaging in reflective listening to express empathy, using summaries, and eliciting self-motivated statements [115,116]. Motivational interviewing is structured around the following principles: expressing empathy, creating discrepancies between current behavior and future goals, managing resistance, and promoting self-efficacy [110,115]. Using empathy as a feature of patient–clinician communication reduces patient anxiety and distress and leads to improved clinical outcomes [117]. A fundamental challenge in active therapies is motivating patients to acquire adequate self-management skills, increasing patient commitment [118] and thereby improving engagement with the prescribed therapy [119].
8.1. Time Planning of the Model
The therapeutic education model in motor behavior is designed to be implemented over a period of 8 to 12 weeks, with weekly sessions lasting 60 to 90 min. Each week addresses a key component of the model, offering a structured yet flexible approach that adapts to the individual progress of each patient.
During the first two weeks, a biobehavioral analysis and the setting of personalized goals are conducted. This phase is crucial, as it identifies the cognitive, emotional, and behavioral factors that may influence the patient’s ability to engage in therapeutic exercise and their perception of pain. Through structured interviews, self-recordings, and qualitative movement analysis, factors such as the fear of movement, self-efficacy, and pain avoidance behaviors are explored. Based on this information, realistic and specific goals are established, which are continuously adjusted throughout the program to align with the patient’s progress. This dynamic goal-setting process ensures that interventions are tailored to the patient’s individual development.
Simultaneously, education on the benefits of exercise begins in the first week and is reinforced throughout the program. The goal of this phase is to ensure that patients understand how physical exercise can positively impact their migraine symptoms and overall well-being. By increasing their knowledge of the benefits of exercise, the aim is to reduce cognitive resistance and increase positive expectations of success.
Movement education becomes more prominent between the third and fifth weeks of the program, although it remains a central component throughout the intervention. During this phase, patients learn to interpret the sensations that may arise during and after exercise, such as fatigue, pain, or other sensory perceptions. The objective is to normalize these perceptions and help patients differentiate between normal fatigue and symptoms that may be related to migraines. This education reduces uncertainty prior to exercise and prepares patients to adopt a more proactive approach toward movement.
The therapeutic education model is complemented by the prescription of therapeutic exercise, which is tailored to each patient’s clinical evolution. This adjustment allows the exercise to be progressive and to adapt to both the patient’s physical capabilities and psychological response.
8.2. Human Resources Required
The successful implementation of the model requires a multidisciplinary team of specialized professionals working in a coordinated manner to address both the physical and emotional aspects of migraine treatment.
The team includes neurologists specializing in headaches, trained in motivational interviewing. These professionals are responsible for overseeing the clinical management of the patients and monitoring the progression of migraines, ensuring that the treatment is not only effective in reducing attacks but also enhances the patient’s overall well-being.
In addition, physiotherapists specializing in chronic pain and therapeutic exercise prescription play a crucial role in implementing exercise programs and educating patients about movement. These physiotherapists, also trained in motivational interviewing, guide patients in practicing safe and effective exercises, adjusting the treatment plans according to the patient’s physical and emotional responses.
Finally, clinical psychologists trained in motivational interviewing are tasked with managing the behavioral and motivational aspects of the treatment. They work to address avoidance behaviors, fear of movement, and other psychological factors that may interfere with the adoption of healthy behaviors, such as regular exercise.
It is essential that all professionals involved receive specific training in the therapeutic education model, ensuring coherent and effective program implementation while integrating both physical and psychological interventions.
8.3. Measures to Evaluate Model Effectiveness
Evaluating the effectiveness of the therapeutic education model is crucial to measuring its impact on both migraine symptom reduction and patient quality of life. Several clinical and behavioral measures will be employed to provide a comprehensive assessment.
The frequency and intensity of migraine attacks will be evaluated using patient-administered diaries. This will allow for a detailed follow-up of symptom progression throughout the program and will provide clear insight into the treatment’s impact on the frequency and severity of migraine episodes.
Patient quality of life will be assessed using validated scales such as the Migraine Disability Assessment (MIDAS), the 36-Item Short-Form Health Survey (SF-36), and the Headache Impact Test-6 (HIT-6). These tools provide a detailed analysis of the migraine’s impact on daily activities and the general health of patients, helping to track progress based on improved functionality and reduced disability.
Additionally, the Biobehavioral Pain and Movement Questionnaire (BioPMovQ) will be used to measure variables such as self-efficacy, movement avoidance behaviors, perceived functional capacity, and disability related to pain. This questionnaire offers an in-depth assessment of the relationships between chronic pain and motor behavior from a biobehavioral perspective, allowing for a more profound analysis of how pain influences motor behavior.
Furthermore, improvements in motor and behavioral skills will be assessed through functional tests and self-evaluations conducted by the patients. These measures will provide critical information on the patient’s functional progress and their ability to incorporate therapeutic exercises into daily life.
9. Exercise Prescription in Patients with Migraine
A clinical practice guideline has recently been published, and its primary aim is to offer recommendations to healthcare and exercise specialists, including neurologists, physiotherapists, and exercise physiologists, concerning prescribing exercise for patients with migraines [120]. The evidence indicates that specific exercise modalities are effective in ameliorating symptoms (e.g., headache frequency, disability, and the quality of life in patients with migraine).
Modalities with a Grade B recommendation, such as aerobic exercise [28,34,77,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138]; continuous moderate-intensity aerobic exercise [78,79,81,139,140,141,142,143,144,145,146,147]; yoga [77,85,86,87,88,91,138,148,149,150]; and lifestyle and exercise recommendations [74,76,151,152,153,154], display promising benefits in symptom improvement. Notably, yoga, including physical postures, breathing techniques, and mindfulness exercises, is likely to decrease the frequency and disability of migraine episodes [120]. Furthermore, it is pivotal to emphasize the recommendation to integrate exercise alongside other lifestyle advices. These include maintaining consistent sleep and eating schedules, adequate hydration, stress management relaxation techniques, and abstaining from excessive medication consumption [74,76,151,152,153,154]. These interventions evidenced a reduction in pain frequency and an improvement in the quality of life of patients who suffer from episodic and chronic migraines [120]. Table 1 describes the therapeutic exercise interventions and their respective prescription parameters.

Table 1.
Prescription parameters for each exercise modality included in the clinical practice guidelines.
Modalities that received a Grade C recommendation, such as relaxation techniques [143,155,156,157], high-intensity interval training [83,141,142], continuous low-intensity aerobic exercise [158,159], Tai Chi [160], and resistance training [92], also exhibited benefits, albeit with a less robust evidence base compared with the Grade B-recommended modalities [120]. For instance, Tai Chi, a balance training program, demonstrated an improvement in migraine frequency in patients with episodic migraine following a 12-week intervention [160]. Relaxation techniques, including methods such as progressive muscle relaxation and visualization, have shown improvements in headache frequency after a minimum of 6 weeks of implementation [143,155,156,157].
Conversely, certain exercises, like those targeting neck endurance, showed no significant improvements in frequency, intensity, or disability in patients with episodic migraine [161]. This suggests that not all exercises are beneficial for all patients, underscoring the need for individualized prescription.
10. Expert Recommendations for the Prescription of Therapeutic Exercise in Patients with Migraine
Despite mounting evidence over the past decade regarding the benefits of exercise, questions persist that must be addressed to optimize the prescription of therapeutic exercise in patients with migraine. As we await empirical scientific evidence to clarify these uncertainties, the consensus of experts in exercise prescription emerges as a valuable guide for tailoring treatment for these patients. A study has recently been published on the prescription of therapeutic exercise for patients with migraine based on this consensus [162].
From the consensus findings, the optimal exercise parameters comprise sessions of 30–60 min, 3 days a week, focusing on continuous moderate-intensity aerobic exercise. Furthermore, relaxation and breathing exercises of 5–20 min daily were added [162]. Regarding additional considerations, it is recommended for initial exercise supervision to evolve toward patient self-regulation and independence. Psychological elements, including pain catastrophizing, fear-avoidance beliefs, disability, anxiety, and depression, were identified as factors that could impact adherence and exercise efficacy in these individuals. Gradual exposure to exercise might help improve these psychological factors, thereby enhancing the intervention’s efficacy [162].
On another note, experts also highlight the relevance of yoga and concurrent training as therapeutic exercise recommendations for these patients [162]. Table 2 provides details on the specific variables and characteristics of the therapeutic exercise prescription suggested by the experts.

Table 2.
Prescription parameters, considerations, and recommendations suggested by the experts.
11. Conclusions
The scientific literature reveals a complex relationship between migraines and physical activity. Studies indicate that individuals with migraines tend to be less physically active than asymptomatic controls, even during headache-free periods. Physical inactivity also correlates with a higher migraine prevalence. Furthermore, kinesiophobia is present in a significant percentage of patients with migraines, exacerbating functional disability and limiting quality of life. Psychological aspects such as pain catastrophizing, depression, and self-efficacy also influence migraine-related disability. These findings underscore the importance of integrating multidisciplinary therapeutic approaches, which include physical activity and behavioral intervention, for effective migraine management.
In this regard, therapeutic interventions can be approached through a biobehavioral paradigm emphasizing the interaction of psychological and physiological factors. Physiotherapy based on this approach integrates treatments such as therapeutic education and exercise, promoting pain self-management. Although evidence supports the efficacy of these interventions in other painful conditions, the combination of education and exercise in migraine warrants further research. A model of therapeutic education focused on enhancing the effects of exercise is proposed, with phases ranging from education about exercise benefits to goal setting. This model employs motivational interviewing, an effective method for enhancing intrinsic motivation for change. Recent guidelines suggest that certain exercise modalities, such as yoga and aerobic exercise, are beneficial for patients with migraines, although the necessity for individualized prescription is emphasized. Integrating exercise with other lifestyle recommendations is essential to optimize outcomes in patients with migraines.
Author Contributions
Conceptualization, R.L.T. and A.P.-A.; methodology, R.L.T. and A.P.-A.; formal analysis, R.L.T., A.P.-A. and Á.R.-V.; investigation, R.L.T., A.P.-A. and Á.R.-V.; writing—original draft preparation, R.L.T., A.P.-A., Á.R.-V. and A.B.d.O.; writing—review and editing, R.L.T., A.P.-A., Á.R.-V. and A.B.d.O.; visualization, R.L.T.; supervision, R.L.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Puledda, F.; Messina, R.; Goadsby, P.J. An update on migraine: Current understanding and future directions. J. Neurol. 2017, 264, 2031. [Google Scholar] [CrossRef] [PubMed]
- Ashina, M.; Katsarava, Z.; Do, T.P.; Buse, D.C.; Pozo-Rosich, P.; Özge, A.; Krymchantowski, A.V.; Lebedeva, E.R.; Ravishankar, K.; Yu, S.; et al. Migraine: Epidemiology and systems of care. Lancet 2021, 397, 1485–1495. [Google Scholar] [CrossRef]
- Ferrari, M.D.; Goadsby, P.J.; Burstein, R.; Kurth, T.; Ayata, C.; Charles, A.; Ashina, M.; Maagdenberg, A.M.J.M.v.D.; Dodick, D.W. Migraine. Nat. Rev. Dis. Primers 2022, 8, 2. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.B.; Queiroz, L.P.; Rocha-Filho, P.S.; Sarmento, E.M.; Peres, M.F.P. Annual Indirect Costs Secondary to Headache Disability in Brazil. Cephalalgia 2020, 40, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Linde, M.; Gustavsson, A.; Stovner, L.J.; Steiner, T.J.; Barré, J.; Katsarava, Z.; Lainez, J.M.; Lampl, C.; Lantéri-Minet, M.; Rastenyte, D.; et al. The cost of headache disorders in Europe: The Eurolight project. Eur. J. Neurol. 2012, 19, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Steiner, T.J.; Stovner, L.J.; Jensen, R.; Uluduz, D.; Katsarava, Z. Migraine remains second among the world’s causes of disability, and first among young women: Findings from GBD2019. J. Headache Pain 2020, 21, 137. [Google Scholar] [CrossRef] [PubMed]
- Battista, S.; Lazzaretti, A.; Coppola, I.; Falsiroli Maistrello, L.; Rania, N.; Testa, M. Living with migraine: A meta-synthesis of qualitative studies. Front. Psychol. 2023, 14, 1129926. [Google Scholar] [CrossRef]
- Estave, P.M.; Beeghly, S.; Anderson, R.; Margol, C.; Shakir, M.; George, G.; Berger, A.; O’connell, N.; Burch, R.; Haas, N.; et al. Learning the full impact of migraine through patient voices: A qualitative study. Headache 2021, 61, 1004–1020. [Google Scholar] [CrossRef]
- O’Bryant, S.E.; Marcus, D.A.; Rains, J.C.; Penzien, D.B. Neuropsychology of migraine: Present status and future directions. Expert Rev. Neurother. 2005, 5, 363–370. [Google Scholar] [CrossRef]
- Marcus, D.A. Central nervous system abnormalities in migraine. Expert Opin. Pharmacother. 2003, 4, 1709–1715. [Google Scholar] [CrossRef]
- Demarquay, G.; Mauguière, F. Central Nervous System Underpinnings of Sensory Hypersensitivity in Migraine: Insights from Neuroimaging and Electrophysiological Studies. Headache 2016, 56, 1418–1438. [Google Scholar] [CrossRef] [PubMed]
- Ashina, S.; Bentivegna, E.; Martelletti, P.; Eikermann-Haerter, K. Structural and Functional Brain Changes in Migraine. Pain Ther. 2021, 10, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Goadsby, P.J.; Holland, P.R.; Martins-Oliveira, M.; Hoffmann, J.; Schankin, C.; Akerman, S. Pathophysiology of migraine: A disorder of sensory processing. Physiol. Rev. 2017, 97, 553–622. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, D.J.; Dumkrieger, G.M.; Hentz, J.G.; Dodick, D.W.; Schwedt, T.J. Physical impairment during and between migraine attacks: A daily diary study of patients with chronic migraine. Cephalalgia 2024, 44, 3331024241249747. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, G.F.; Luedtke, K.; Pinheiro, C.F.; Moraes, R.; Lemos, T.W.; Bigal, M.E.; Dach, F.; Bevilaqua-Grossi, D. Migraine with Aura Is Related to Delayed Motor Control Reaction and Imbalance Following External Perturbations. Front. Neurol. 2021, 12, 755990. [Google Scholar] [CrossRef]
- Young, W.B.; Gangal, K.S.; Aponte, R.J.; Kaiser, R.S. Migraine with unilateral motor symptoms: A case-control study. J. Neurol. Neurosurg. Psychiatry 2007, 78, 600–604. [Google Scholar] [CrossRef]
- La Touche, R. Introduciendo la dimensión motora dentro de la conceptualización de la experiencia del dolor. J. Move Ther. Sci. 2021, 3, 269–277. [Google Scholar] [CrossRef]
- Seng, E.K.; Shapiro, R.E.; Buse, D.C.; Robbins, M.S.; Lipton, R.B.; Parker, A. The unique role of stigma in migraine-related disability and quality of life. Headache 2022, 62, 1354–1364. [Google Scholar] [CrossRef]
- Rosignoli, C.; Ornello, R.; Onofri, A.; Caponnetto, V.; Grazzi, L.; Raggi, A.; Leonardi, M.; Sacco, S. Applying a biopsychosocial model to migraine: Rationale and clinical implications. J. Headache Pain 2022, 23, 100. [Google Scholar] [CrossRef]
- Seng, E.K.; Buse, D.C.; Klepper, J.E.; Ma, S.J.M.; Grinberg, A.S.; Grosberg, B.M.; Pavlovic, J.M.; Robbins, M.S.; Vollbracht, S.E.; Lipton, R.B. Psychological Factors Associated with Chronic Migraine and Severe Migraine-Related Disability: An Observational Study in a Tertiary Headache Center. Headache 2017, 57, 593. [Google Scholar] [CrossRef]
- Waliszewska-Prosół, M.; Montisano, D.A.; Antolak, M.; Bighiani, F.; Cammarota, F.; Cetta, I.; Corrado, M.; Ihara, K.; Kartamysheva, R.; Petrušić, I.; et al. The impact of primary headaches on disability outcomes: A literature review and meta-analysis to inform future iterations of the Global Burden of Disease study. J. Headache Pain 2024, 25, 27. [Google Scholar] [CrossRef] [PubMed]
- Stewart, W.F.; Lipton, R.B.; Dowson, A.J.; Sawyer, J. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology 2001, 56, S20–S28. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Rendas-Baum, R.; Varon, S.F.; Kosinski, M. Validation of the Headache Impact Test (HIT-6TM) across episodic and chronic migraine. Cephalalgia 2011, 31, 357. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, G.P.; Ramadan, N.M.; Aggarwal, S.K.; Newman, C.W. The Henry Ford Hospital Headache Disability Inventory (HDI). Neurology 1994, 44, 837–842. [Google Scholar] [CrossRef]
- Minen, M.T.; Anglin, C.; Boubour, A.; Squires, A.; Herrmann, L. Meta-Synthesis on Migraine Management. Headache 2018, 58, 22–44. [Google Scholar] [CrossRef]
- Pomes, L.M.; Guglielmetti, M.; Bertamino, E.; Simmaco, M.; Borro, M.; Martelletti, P. Optimising migraine treatment: From drug-drug interactions to personalized medicine. J. Headache Pain 2019, 20, 56. [Google Scholar] [CrossRef]
- Pérez-Muñoz, A.; Buse, D.C.; Andrasik, F. Behavioral Interventions for Migraine. Neurol. Clin. 2019, 37, 789–813. [Google Scholar] [CrossRef]
- Song, T.-J.; Chu, M.K. Exercise in Treatment of Migraine Including Chronic Migraine. Curr. Pain Headache Rep. 2021, 25, 14. [Google Scholar] [CrossRef]
- Demarquay, G.; Mawet, J.; Guégan-Massardier, E.; de Gaalon, S.; Donnet, A.; Giraud, P.; Lantéri-Minet, M.; Lucas, C.; Moisset, X.; Roos, C.; et al. Revised guidelines of the French headache society for the diagnosis and management of migraine in adults. Part 3: Non-pharmacological treatment. Rev. Neurol. 2021, 177, 753–759. [Google Scholar] [CrossRef]
- Schytz, H.W.; Amin, F.M.; Jensen, R.H.; Carlsen, L.; Maarbjerg, S.; Lund, N.; Aegidius, K.; Thomsen, L.L.; Bach, F.W.; Beier, D.; et al. Reference programme: Diagnosis and treatment of headache disorders and facial pain. Danish Headache Society, 3rd edition, 2020. J. Headache Pain 2021, 22, 22. [Google Scholar] [CrossRef]
- American Headache Society. The American Headache Society Position Statement On Integrating New Migraine Treatments Into Clinical Practice. Headache 2019, 59, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Buse, D.C.; Andrasik, F. Behavioral Medicine for Migraine. Neurol. Clin. 2009, 27, 445–465. [Google Scholar] [CrossRef] [PubMed]
- Kropp, P.; Meyer, B.; Meyer, W.; Dresler, T. An update on behavioral treatments in migraine—Current knowledge and future options. Expert Rev. Neurother. 2017, 17, 1059–1068. [Google Scholar] [CrossRef] [PubMed]
- Amin, F.M.; Aristeidou, S.; Baraldi, C.; Czapinska-Ciepiela, E.K.; Ariadni, D.D.; Di Lenola, D.; Fenech, C.; Kampouris, K.; Karagiorgis, G.; Braschinsky, M.; et al. The association between migraine and physical exercise. J. Headache Pain 2018, 19, 83. [Google Scholar] [CrossRef]
- Koppen, H.; van Veldhoven, P.L.J. Migraineurs with exercise-triggered attacks have a distinct migraine. J. Headache Pain 2013, 14, 99. [Google Scholar] [CrossRef][Green Version]
- Varkey, E.; Grüner Sveälv, B.; Edin, F.; Ravn-Fischer, A.; Cider, Å. Provocation of Migraine after Maximal Exercise: A Test-Retest Study. Eur. Neurol. 2017, 78, 22–27. [Google Scholar] [CrossRef]
- Farris, S.G.; Thomas, J.G.; Abrantes, A.M.; Godley, F.A.; Roth, J.L.; Lipton, R.B.; Pavlovic, J.; Bond, D.S. Intentional avoidance of physical activity in women with migraine. Cephalalgia Rep. 2018, 1, 251581631878828. [Google Scholar] [CrossRef]
- Farris, S.G.; Thomas, J.G.; Abrantes, A.M.; Lipton, R.B.; Burr, E.K.; Godley, F.A.; Roth, J.L.; Pavlovic, J.M.; Bond, D.S. Anxiety sensitivity and intentional avoidance of physical activity in women with probable migraine. Cephalalgia 2019, 39, 1465–1469. [Google Scholar] [CrossRef]
- Rogers, D.G.; Bond, D.S.; Bentley, J.P.; Smitherman, T.A. Objectively Measured Physical Activity in Migraine as a Function of Headache Activity. Headache 2020, 60, 1930–1938. [Google Scholar] [CrossRef]
- Stronks, D.L.; Tulen, J.H.M.; Bussmann, J.B.J.; Mulder, L.J.M.M.; Passchier, J. Interictal daily functioning in migraine. Cephalalgia 2004, 24, 271–279. [Google Scholar] [CrossRef]
- Varkey, E.; Hagen, K.; Zwart, J.A.; Linde, M. Physical activity and headache: Results from the Nord-Trøndelag Health Study (HUNT). Cephalalgia 2008, 28, 1292–1297. [Google Scholar] [CrossRef] [PubMed]
- Denche-Zamorano, Á.; Paredes-Mateos, V.; Pastor-Cisneros, R.; Carlos-Vivas, J.; Contreras-Barraza, N.; Iturra-Gonzalez, J.A.; Mendoza-Muñoz, M. Physical Activity Level, Depression, Anxiety, and Self-Perceived Health in Spanish Adults with Migraine: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 13882. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.; Mercante, J.P.P.; Bensenor, I.M.; Goulart, A.C.; Peres, M.F.P. Headache disability, lifestyle factors, health perception, and mental disorder symptoms: A cross-sectional analysis of the 2013 National Health Survey in Brazil. Neurol. Sci. 2022, 43, 2723–2734. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, A.B.; Mercante, J.P.P.; Peres, M.F.P.; Molina, M.D.C.B.; Lotufo, P.A.; Benseñor, I.M.; Goulart, A.C. Physical inactivity and headache disorders: Cross-sectional analysis in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Cephalalgia 2021, 41, 1467–1485. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.B.; Peres, M.F.P.; Mercante, J.P.P.; Molina, M.D.C.B.; Lotufo, P.A.; Benseñor, I.M.; Goulart, A.C. Physical activity pattern and migraine according to aura symptoms in the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) cohort: A cross-sectional study. Headache 2022, 62, 977–988. [Google Scholar] [CrossRef]
- Master, H.; Annis, J.; Huang, S.; Beckman, J.A.; Ratsimbazafy, F.; Marginean, K.; Carroll, R.; Natarajan, K.; Harrell, F.E.; Roden, D.M.; et al. Association of step counts over time with the risk of chronic disease in the All of Us Research Program. Nat. Med. 2022, 28, 2301–2308. [Google Scholar] [CrossRef]
- Domingues, R.B.; Teixeira, A.L.; Domingues, S.A. Physical practice is associated with less functional disability in medical students with migraine. Arq. Neuropsiquiatr. 2011, 69, 39–43. [Google Scholar] [CrossRef]
- Bond, D.S.; Thomas, J.G.; O’leary, K.C.; Lipton, R.B.; Peterlin, B.L.; Roth, J.; Rathier, L.; Wing, R.R. Objectively measured physical activity in obese women with and without migraine. Cephalalgia 2015, 35, 886–893. [Google Scholar] [CrossRef]
- Ornello, R.; Ripa, P.; Pistoia, F.; Degan, D.; Tiseo, C.; Carolei, A.; Sacco, S. Migraine and body mass index categories: A systematic review and meta-analysis of observational studies. J. Headache Pain 2015, 16, 27. [Google Scholar] [CrossRef]
- Gelaye, B.; Sacco, S.; Brown, W.J.; Nitchie, H.L.; Ornello, R.; Peterlin, B.L. Body composition status and the risk of migraine: A meta-analysis. Neurology 2017, 88, 1795–1804. [Google Scholar] [CrossRef]
- Kori, S.; Miller, R.; Todd, D. Kinesiophobia: A new view of chronic pain behavior. Pain Manag. 1990, 3, 35–43. [Google Scholar]
- Vlaeyen, J.W.S.; Kole-Snijders, A.M.J.; Rotteveel, A.M.; Ruesink, R.; Heuts, P.H.T.G. The role of fear of movement/(re)injury in pain disability. J. Occup. Rehabil. 1995, 5, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Leeuw, M.; Houben, R.M.A.; Severeijns, R.; Picavet, H.S.J.; Schouten, E.G.W.; Vlaeyen, J.W.S. Pain-related fear in low back pain: A prospective study in the general population. Eur. J. Pain 2007, 11, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Giusti, E.M.; Manna, C.; Varallo, G.; Cattivelli, R.; Manzoni, G.M.; Gabrielli, S.; D’amario, F.; Lacerenza, M.; Castelnuovo, G. The Predictive Role of Executive Functions and Psychological Factors on Chronic Pain after Orthopaedic Surgery: A Longitudinal Cohort Study. Brain Sci. 2020, 10, 685. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, M.K.E.; Larsson, M.; Östlund, H.; Styf, J. Kinesiophobia among patients with musculoskeletal pain in primary healthcare. J. Rehabil. Med. 2006, 38, 37–43. [Google Scholar] [CrossRef]
- Bränström, H.; Fahlström, M. Kinesiophobia in patients with chronic musculoskeletal pain: Differences between men and women. J. Rehabil. Med. 2008, 40, 375–380. [Google Scholar] [CrossRef]
- Perrot, S.; Trouvin, A.-P.; Rondeau, V.; Chartier, I.; Arnaud, R.; Milon, J.-Y.; Pouchain, D. Kinesiophobia and physical therapy-related pain in musculoskeletal pain: A national multicenter cohort study on patients and their general physicians. Jt. Bone Spine 2018, 85, 101–107. [Google Scholar] [CrossRef]
- Benatto, M.T.; Bevilaqua-Grossi, D.; Carvalho, G.F.; Bragatto, M.M.; Pinheiro, C.F.; Straceri Lodovichi, S.; Dach, F.; Fernández-De-Las-Peñas, C.; Florencio, L.L. Kinesiophobia is associated with migraine. Pain Med. 2019, 20, 846–851. [Google Scholar] [CrossRef]
- Altay, H.; Celenay, S.T. An investigation of the relationship between cutaneous allodynia and kinesiophobia, gastrointestinal system symptom severity, physical activity and disability in individuals with migraine. Korean J. Pain 2023, 36, 137–146. [Google Scholar] [CrossRef]
- Pinheiro, C.F.; Bevilaqua-Grossi, D.; Florencio, L.L.; Bragatto, M.M.; Benatto, M.T.; Dach, F.; Bigal, M.E.; Carvalho, G.F. Is kinesiophobia related to fear of falling, dizziness disability, and migraine disability in patients with migraine? Physiother. Theory Pract. 2022, 38, 2727–2735. [Google Scholar] [CrossRef]
- Martins, I.P.; Gouveia, R.G.; Parreira, E. Kinesiophobia in migraine. J. Pain 2006, 7, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Ruscheweyh, R.; Pereira, D.; Hasenbring, M.I.; Straube, A. Pain-related avoidance and endurance behaviour in migraine: An observational study. J. Headache Pain 2019, 20, 9. [Google Scholar] [CrossRef] [PubMed]
- Klonowski, T.; Kropp, P.; Straube, A.; Ruscheweyh, R. Psychological factors associated with headache frequency, intensity, and headache-related disability in migraine patients. Neurol. Sci. 2022, 43, 1255–1266. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Bae, D.W.; Park, S.G.; Park, J.W. The impact of Pain-related emotions on migraine. Sci. Rep. 2021, 11, 577. [Google Scholar] [CrossRef]
- D’Amico, D.; Grazzi, L.; Bussone, G.; Curone, M.; Di Fiore, P.; Usai, S.; Leonardi, M.; Giovannetti, A.M.; Schiavolin, S.; Raggi, A. Are depressive symptomatology, self-efficacy, and perceived social support related to disability and quality of life in patients with chronic migraine associated to medication overuse? Data from a cross-sectional study. Headache 2015, 55, 636–645. [Google Scholar] [CrossRef]
- Pistoia, F.; Salfi, F.; Saporito, G.; Ornello, R.; Frattale, I.; D’aurizio, G.; Tempesta, D.; Ferrara, M.; Sacco, S. Behavioral and psychological factors in individuals with migraine without psychiatric comorbidities. J. Headache Pain 2022, 23, 110. [Google Scholar] [CrossRef]
- Alvarez-Astorga, A.; García-Azorín, D.; Hernández, M.; de la Red, H.; Sotelo, E.; Uribe, F.; Guerrero, A. Pain catastrophising in a population of patients with migraine. Neurologia 2021, 36, 24–28. [Google Scholar] [CrossRef]
- Mortazavi Nasiri, F.S.; Pakdaman, S.; Dehghani, M.; Togha, M. The Relationship between Pain Catastrophizing and Headache-Related Disability: The Mediating Role of Pain Intensity. Jpn. Psychol. Res. 2017, 59, 266–274. [Google Scholar] [CrossRef]
- Bond, D.S.; Buse, D.C.; Lipton, R.B.; Thomas, J.G.; Rathier, L.; Roth, J.; Pavlovic, J.M.; Evans, E.W.; Wing, R.R. Clinical Pain Catastrophizing in Women with Migraine and Obesity. Headache 2015, 55, 923–933. [Google Scholar] [CrossRef]
- Yousefi Afrashteh, M.; Abbasi, M.; Abbasi, M. The relationship between meaning of life, perceived social support, spiritual well-being and pain catastrophizing with quality of life in migraine patients: The mediating role of pain self-efficacy. BMC Psychol. 2023, 11, 17. [Google Scholar] [CrossRef]
- Woldeamanuel, Y.W.; Sanjanwala, B.M.; Peretz, A.M.; Cowan, R.P. Exploring Natural Clusters of Chronic Migraine Phenotypes: A Cross-Sectional Clinical Study. Sci. Rep. 2020, 10, 2804. [Google Scholar] [CrossRef] [PubMed]
- Seng, E.K.; Gosnell, I.; Sutton, L.; Grinberg, A.S. Behavioral Management of Episodic Migraine: Maintaining a Healthy Consistent Lifestyle. Curr. Pain Headache Rep. 2022, 26, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Merrill, R.M.; Gibbons, I.S. Comorbidity of Sleep Disorders, Mental Illness, and Migraine or Headaches. SN Compr. Clin. Med. 2023, 5, 283. [Google Scholar] [CrossRef]
- Woldeamanuel, Y.W.; Cowan, R.P. The impact of regular lifestyle behavior in migraine: A prevalence case–referent study. J. Neurol. 2016, 263, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, L.; Butler, N.; Seng, E.K. Health Behaviors in Episodic Migraine: Why Behavior Change Matters. Curr. Pain Headache Rep. 2018, 22, 65. [Google Scholar] [CrossRef]
- Agbetou, M.; Adoukonou, T. Lifestyle Modifications for Migraine Management. Front. Neurol. 2022, 13, 719467. [Google Scholar] [CrossRef]
- Barber, M.; Pace, A. Exercise and Migraine Prevention: A Review of the Literature. Curr. Pain Headache Rep. 2020, 24, 39. [Google Scholar] [CrossRef]
- Oliveira, A.B.; Bachi, A.L.L.; Ribeiro, R.T.; Mello, M.T.; Vaisberg, M.; Peres, M.F.P. Exercise-Induced Change in Plasma IL-12p70 Is Linked to Migraine Prevention and Anxiolytic Effects in Treatment-Naïve Women: A Randomized Controlled Trial. Neuroimmunomodulation 2017, 24, 293–299. [Google Scholar] [CrossRef]
- Hagan, K.K.; Li, W.; Mostofsky, E.; Bertisch, S.M.; Vgontzas, A.; Buettner, C.; Mittleman, M.A. Prospective cohort study of routine exercise and headache outcomes among adults with episodic migraine. Headache J. Head Face Pain 2021, 61, 493–499. [Google Scholar] [CrossRef]
- Eslami, R.; Parnow, A.; Pairo, Z.; Nikolaidis, P.; Knechtle, B. The effects of two different intensities of aerobic training protocols on pain and serum neuro-biomarkers in women migraineurs: A randomized controlled trail. Eur. J. Appl. Physiol. 2021, 121, 609–620. [Google Scholar] [CrossRef]
- Narin, S.O.; Pinar, L.; Erbas, D.; Oztürk, V.; Idiman, F. The effects of exercise and exercise-related changes in blood nitric oxide level on migraine headache. Clin. Rehabil. 2003, 17, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Pairo, Z.; Parnow, A.H.; Sari-aslani, P.; Eslami, R. Effect of Moderate Intensity Aerobic Exercise on Migraine Headache Indexes and Quality of Life Improvement in Women with Migraine. Q. Horiz. Med. Sci. 2016, 22, 291–297. [Google Scholar] [CrossRef]
- Matin, H.; Taghian, F.; Chitsaz, A. Artificial intelligence analysis to explore synchronize exercise, cobalamin, and magnesium as new actors to therapeutic of migraine symptoms: A randomized, placebo-controlled trial. Neurol. Sci. 2022, 43, 4413–4424. [Google Scholar] [CrossRef] [PubMed]
- Peiro, Z.; Parnow, A.; Sari Aslani, P.; Eslami, R. The Influence of High Intensity Aerobic Training on Migraine Indices and Quality of Life Improvement in Women with Migraine Disorder. Sport Physiol. 2017, 9, 115–130. [Google Scholar] [CrossRef]
- Boroujeni, M.; Marandi, S.; Esfarjani, F.; Sattar, M.; Shaygannejad, V.; Javanmard, S. Yoga intervention on blood NO in female migraineurs. Adv. Biomed. Res. 2015, 4, 259. [Google Scholar] [CrossRef]
- John, P.J.; Sharma, N.; Sharma, C.M.; Kankane, A. Effectiveness of Yoga Therapy in the Treatment of Migraine Without Aura: A Randomized Controlled Trial. Headache J. Head Face Pain 2007, 47, 654–661. [Google Scholar] [CrossRef]
- Kisan, R.; Sujan, M.U.; Adoor, M.; Rao, R.; Nalini, A.; Kutty, B.M.; Murthy, B.C.; Raju, T.R.; Sathyaprabha, T.N. Effect of Yoga on migraine: A comprehensive study using clinical profile and cardiac autonomic functions. Int. J. Yoga 2014, 7, 126–132. [Google Scholar] [CrossRef]
- Kumar, A.; Bhatia, R.; Sharma, G.; Dhanlika, D.; Vishnubhatla, S.; Singh, R.K.; Dash, D.; Tripathi, M.; Srivastava, M.P. Effect of yoga as add-on therapy in migraine (CONTAIN): A randomized clinical trial. Neurology 2020, 94, e2203–e2212. [Google Scholar] [CrossRef]
- Kumari, S.; Dhar, M.; Pathania, M.; Kumar, N.; Kulshrestha, P.; Singh, A. Yoga as an Adjuvant therapy in management of migraine- An open label randomised trial. J. Fam. Med. Prim. Care 2022, 11, 5410. [Google Scholar] [CrossRef]
- Mohammadi, R.; Afroundeh, R.; Khajehlandi, M.; Ghiami, H.; Bahram, M. Effect of 8-Weeks Yoga Exercises on Migraine Headache Induces, Serum Levels of Serotonin and Nitric Oxide in Women with Migraine. J. Appl. Exerc. Physiol. 2020, 16, 73–86. [Google Scholar] [CrossRef]
- Wells, R.E.; O’connell, N.; Pierce, C.R.; Estave, P.; Penzien, D.B.; Loder, E.; Zeidan, F.; Houle, T.T. Effectiveness of Mindfulness Meditation vs Headache Education for Adults with Migraine. JAMA Intern. Med. 2021, 181, 317. [Google Scholar] [CrossRef] [PubMed]
- Aslani, P.S.; Hassanpour, M.; Razi, O.; Knechtle, B. Resistance training reduces pain indices and improves quality of life and body strength in women with migraine disorders. Sport Sci. Health 2021, 18, 433–443. [Google Scholar] [CrossRef]
- Reina-Varona, Á.; Madroñero-Miguel, B.; Fierro-Marrero, J.; Paris-Alemany, A.; La Touche, R. Efficacy of various exercise interventions for migraine treatment: A systematic review and network meta-analysis. Headache 2024, 64, 873–900. [Google Scholar] [CrossRef] [PubMed]
- Gil-Martínez, A.; Paris-Alemany, A.; López-de-Uralde-Villanueva, I.; La Touche, R. Management of pain in patients with temporomandibular disorder (TMD): Challenges and solutions. J. Pain Res. 2018, 11, 571–587. [Google Scholar] [CrossRef]
- Carlson, C.R. Psychological considerations for chronic orofacial pain. Oral Maxillofac. Surg. Clin. N. Am. 2008, 20, 185–195. [Google Scholar] [CrossRef]
- López-de-Uralde-Villanueva, I.; Beltran-Alacreu, H.; Fernández-Carnero, J.; La Touche, R. Pain management using a multimodal physiotherapy program including a biobehavioral approach for chronic nonspecific neck pain: A randomized controlled trial. Physiother. Theory Pract. 2020, 36, 45–62. [Google Scholar] [CrossRef]
- Grande-Alonso, M.; Suso-Martí, L.; Cuenca-Martínez, F.; Pardo-Montero, J.; Gil-Martínez, A.; La Touche, R. Physiotherapy Based on a Biobehavioral Approach with or without Orthopedic Manual Physical Therapy in the Treatment of Nonspecific Chronic Low Back Pain: A Randomized Controlled Trial. Pain Med. 2019, 20, 2571–2587. [Google Scholar] [CrossRef]
- Marcos-Martín, F.; González-Ferrero, L.; Martín-Alcocer, N.; Paris-Alemany, A.; La Touche, R. Multimodal physiotherapy treatment based on a biobehavioral approach for patients with chronic cervico-craniofacial pain: A prospective case series. Physiother. Theory Pract. 2018, 34, 671–681. [Google Scholar] [CrossRef]
- Beltran-Alacreu, H.; Lopez-de-Uralde-Villanueva, I.; La Touche, R. Multimodal Physiotherapy Based on a Biobehavioral Approach as a Treatment for Chronic Tension-Type Headache: A Case Report. Anesth. Pain Med. 2015, 5, e32697. [Google Scholar] [CrossRef]
- Cuenca-Martínez, F.; Grande-Alonso, M.; Suso-Martí, L.; La Touche, R. Therapeutic exercise based on biobehavioral approach for the rehabilitation of a radial nerve injury after surgical removal of a schwannoma: A case report. J. Exerc. Rehabil. 2019, 15, 628–635. [Google Scholar] [CrossRef]
- Kindelan-Calvo, P.; Gil-Martínez, A.; Paris-Alemany, A.; Pardo-Montero, J.; Muñoz-García, D.; Angulo-Díaz-Parreño, S.; La Touche, R. Effectiveness of Therapeutic Patient Education for Adults with Migraine. A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Med. 2014, 15, 1619–1636. [Google Scholar] [CrossRef] [PubMed]
- Button, K.; Roos, P.E.; Spasić, I.; Adamson, P.; van Deursen, R.W.M. The clinical effectiveness of self-care interventions with an exercise component to manage knee conditions: A systematic review. Knee 2015, 22, 360–371. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.D.; Valenzuela, T.; Booth, J.; Taylor, J.L.; Barry, B.K. Explicit Education About Exercise-Induced Hypoalgesia Influences Pain Responses to Acute Exercise in Healthy Adults: A Randomized Controlled Trial. J. Pain 2017, 18, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Jönsson, T.; Ekvall Hansson, E.; Thorstensson, C.A.; Eek, F.; Bergman, P.; Dahlberg, L.E. The effect of education and supervised exercise on physical activity, pain, quality of life and self-efficacy—An intervention study with a reference group. BMC Musculoskelet. Disord. 2018, 19, 198. [Google Scholar] [CrossRef] [PubMed]
- La Touche, R. Prescripción de ejercicio terapéutico en Fisioterapia. Las bases elementales de la identidad profesional. J. Move Ther. Sci. 2020, 2, 71–77. [Google Scholar] [CrossRef]
- Wade, D.T. Goal setting in rehabilitation: An overview of what, why and how. Clin. Rehabil. 2009, 107, 291–295. [Google Scholar] [CrossRef]
- Scobbie, L.; Wyke, S.; Dixon, D. Identifying and applying psychological theory to setting and achieving rehabilitation goals. Clin. Rehabil. 2009, 23, 321–333. [Google Scholar] [CrossRef]
- Scobbie, L.; Dixon, D.; Wyke, S. Goal setting and action planning in the rehabilitation setting: Development of a theoretically informed practice framework. Clin. Rehabil. 2011, 25, 468–482. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Ten things that motivational interviewing is not. Behav. Cogn. Psychother. 2009, 37, 129–140. [Google Scholar] [CrossRef]
- Miller, W.; Rollnick, S. Motivational Interviewing: Helping People Change, 3rd ed.; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Miller, W.R.; Rose, G.S. Toward a Theory of Motivational Interviewing. Am. Psychol. 2009, 64, 527–537. [Google Scholar] [CrossRef]
- Burke, B.L.; Arkowitz, H.; Menchola, M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. J. Consult. Clin. Psychol. 2003, 71, 843–861. [Google Scholar] [CrossRef] [PubMed]
- Hettema, J.; Steele, J.; Miller, W.R. Meta-análisis: Motivational interviewing. Annu. Rev. Clin. Psychol. 2005, 1, 91–111. [Google Scholar] [CrossRef] [PubMed]
- Tuccero, D.; Railey, K.; Briggs, M.; Hull, S.K. Behavioral Health in Prevention and Chronic Illness Management: Motivational Interviewing. Prim. Care Clin. Off. Pract. 2016, 43, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.; Gibbie, T.; Lubman, D.I. Motivational interviewing techniques: Facilitating behaviour change in the general practice setting. Aust. Fam. Physician 2012, 41, 660–667. [Google Scholar] [PubMed]
- Stewart, E.E.; Fox, C. Encouraging patients to change unhealthy behaviors with motivational interviewing. Fam. Pract. Manag. 2011, 18, 21–25. [Google Scholar]
- Derksen, F.; Bensing, J.; Lagro-Janssen, A. Effectiveness of empathy in general practice: A systematic review. Br. J. Gen. Pract. 2013, 63, e76–e84. [Google Scholar] [CrossRef]
- Protheroe, J.; Rogers, A.; Kennedy, A.P.; Macdonald, W.; Lee, V. Promoting patient engagement with self-management support information: A qualitative meta-synthesis of processes influencing uptake. Implement. Sci. 2008, 3, 44. [Google Scholar] [CrossRef]
- Bigi, S. Communication skills for patient engagement: Argumentation competencies as means to prevent or limit reactance arousal, with an example from the Italian healthcare system. Front. Psychol. 2016, 7, 1472. [Google Scholar] [CrossRef]
- La Touche, R.; Fierro-Marrero, J.; Sánchez-Ruíz, I.; de Rivera-Romero, B.R.; Cabrera-López, C.D.; Lerma-Lara, S.; Requejo-Salinas, N.; de Asís-Fernández, F.; Elizagaray-García, I.; Fernández-Carnero, J.; et al. Prescription of therapeutic exercise in migraine, an evidence-based clinical practice guideline. J. Headache Pain 2023, 24, 68. [Google Scholar] [CrossRef]
- Herranz-Gómez, A.; García-Pascual, I.; Montero-Iniesta, P.; La Touche, R.; Paris-Alemany, A. Effectiveness of Exercise and Manual Therapy as Treatment for Patients with Migraine, Tension-Type Headache or Cervicogenic Headache: An Umbrella and Mapping Review with Meta-Meta-Analysis. Appl. Sci. 2021, 11, 6856. [Google Scholar] [CrossRef]
- La Touche, R.; Pérez, J.J.F.; Acosta, A.P.; Campodónico, L.G.; García, S.M.; Juárez, D.A.; García, B.S.; Angulo-Díaz-Parreño, S.; Cuenca-Martínez, F.; Suso-Martí, L.; et al. Is aerobic exercise helpful in patients with migraine? A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 965–982. [Google Scholar] [CrossRef] [PubMed]
- Lemmens, J.; De Pauw, J.; Van Soom, T.; Michiels, S.; Versijpt, J.; van Breda, E.; Castien, R.; De Hertogh, W. The effect of aerobic exercise on the number of migraine days, duration and pain intensity in migraine: A systematic literature review and meta-analysis. J. Headache Pain 2019, 20, 16. [Google Scholar] [CrossRef] [PubMed]
- Luedtke, K.; Allers, A.; Schulte, L.H.; May, A. Efficacy of interventions used by physiotherapists for patients with headache and migraine—Systematic review and meta-analysis. Cephalalgia 2016, 36, 474–492. [Google Scholar] [CrossRef] [PubMed]
- Varangot-Reille, C.; Suso-Martí, L.; Romero-Palau, M.; Suárez-Pastor, P.; Cuenca-Martínez, F. Effects of Different Therapeutic Exercise Modalities on Migraine or Tension-Type Headache: A Systematic Review and Meta-Analysis with a Replicability Analysis. J. Pain 2022, 23, 1099–1122. [Google Scholar] [CrossRef]
- Ahn, A.H. Why Does Increased Exercise Decrease Migraine? Curr. Pain Headache Rep. 2013, 17, 379. [Google Scholar] [CrossRef]
- Busch, V.; Gaul, C. Sport bei Migräne. Der Schmerz 2008, 22, 137–147. [Google Scholar] [CrossRef]
- Busch, V.; Gaul, C. Exercise in Migraine Therapy—Is There Any Evidence for Efficacy? A Critical Review. Headache J. Head Face Pain 2008, 48, 890–899. [Google Scholar] [CrossRef]
- Daenen, L.; Varkey, E.; Kellmann, M.; Nijs, J. Exercise, Not to Exercise, or How to Exercise in Patients with Chronic Pain? Applying Science to Practice. Clin. J. Pain 2015, 31, 108–114. [Google Scholar] [CrossRef]
- Guarín-Duque, H.A.; Pablo-Navarro, B.; Bermúdez-Moreno, G.; Barrientos-Jaramillo, E.; Andrés-Rueda, S.; Hernández-Artal, B. Aportaciones del ejercicio al mejoramiento de los síntomas de la migraña y el papel de Enfermería. Revis. Bibliogr. Ocronos 2021, 4, 164. [Google Scholar]
- Hindiyeh, N.A.; Krusz, J.C.; Cowan, R.P. Does Exercise Make Migraines Worse and Tension Type Headaches Better? Curr. Pain Headache Rep. 2013, 17, 380. [Google Scholar] [CrossRef]
- Irby, M.B.; Bond, D.S.; Lipton, R.B.; Nicklas, B.; Houle, T.T.; Penzien, D.B. Aerobic Exercise for Reducing Migraine Burden: Mechanisms, Markers, and Models of Change Processes. Headache J. Head Face Pain 2016, 56, 357–369. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Mattiuzzi, C.; Sanchis-Gomar, F. Physical exercise and migraine: For or against? Ann. Transl. Med. 2018, 6, 181. [Google Scholar] [CrossRef] [PubMed]
- Mauskop, A. Nonmedication, Alternative, and Complementary Treatments for Migraine. Contin. Lifelong Learn. Neurol. 2012, 18, 796–806. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.S.; Minen, M.T. Complementary and Integrative Health Treatments for Migraine. J. Neuro-Ophthalmol. 2019, 39, 360–369. [Google Scholar] [CrossRef]
- Robblee, J.; Starling, A.J. SEEDS for success: Lifestyle management in migraine. Cleve Clin. J. Med. 2019, 86, 741–749. [Google Scholar] [CrossRef]
- Tepper, S.J. Nutraceutical and Other Modalities for the Treatment of Headache. Contin. Lifelong Learn. Neurol. 2015, 21, 1018–1031. [Google Scholar] [CrossRef]
- Wells, R.E.; Beuthin, J.; Granetzke, L. Complementary and Integrative Medicine for Episodic Migraine: An Update of Evidence from the Last 3 Years. Curr. Pain Headache Rep. 2019, 23, 10. [Google Scholar] [CrossRef]
- Ahmadi, Z. The effect of 8-week aerobic exercise on migraine headache indices and blood nitric oxide level in women with migraine. Sport Physiol. 2015, 7, 33–50. [Google Scholar]
- Oliveira, A.B.; Ribeiro, R.T.; Mello, M.T.; Tufik, S.; Peres, M.F.P. Anandamide Is Related to Clinical and Cardiorespiratory Benefits of Aerobic Exercise Training in Migraine Patients: A Randomized Controlled Clinical Trial. Cannabis Cannabinoid Res. 2019, 4, 275–284. [Google Scholar] [CrossRef]
- Hanssen, H.; Minghetti, A.; Magon, S.; Rossmeissl, A.; Papadopoulou, A.; Klenk, C.; Schmidt-Trucksäss, A.; Faude, O.; Zahner, L.; Sprenger, T.; et al. Superior Effects of High-Intensity Interval Training vs. Moderate Continuous Training on Arterial Stiffness in Episodic Migraine: A Randomized Controlled Trial. Front. Physiol. 2017, 8, 1086. [Google Scholar] [CrossRef]
- Hanssen, H.; Minghetti, A.; Magon, S.; Rossmeissl, A.; Rasenack, M.; Papadopoulou, A.; Klenk, C.; Faude, O.; Zahner, L.; Sprenger, T.; et al. Effects of different endurance exercise modalities on migraine days and cerebrovascular health in episodic migraineurs: A randomized controlled trial. Scand. J. Med. Sci. Sports 2018, 28, 1103–1112. [Google Scholar] [CrossRef] [PubMed]
- Varkey, E.; Cider, Å.; Carlsson, J.; Linde, M. Exercise as migraine prophylaxis: A randomized study using relaxation and topiramate as controls. Cephalalgia 2011, 31, 1428–1438. [Google Scholar] [CrossRef] [PubMed]
- Darabaneanu, S.; Overath, C.H.; Rubin, D.; Lüthje, S.; Sye, W.; Niederberger, U.; Gerber, W.-D.; Weisser, B. Aerobic Exercise as a Therapy Option for Migraine: A Pilot Study. Int. J. Sports Med. 2011, 32, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Luedtke, K.; Starke, W.; von Korn, K.; Szikszay, T.M.; Schwarz, A.; May, A. Neck treatment compared to aerobic exercise in migraine: A preference-based clinical trial. Cephalalgia Rep. 2020, 3, 251581632093068. [Google Scholar] [CrossRef]
- Overath, C.H.; Darabaneanu, S.; Evers, M.C.; Gerber, W.-D.; Graf, M.; Keller, A.; Niederberger, U.; Schäl, H.; Siniatchkin, M.; Weisser, B. Does an aerobic endurance programme have an influence on information processing in migraineurs? J. Headache Pain 2014, 15, 11. [Google Scholar] [CrossRef]
- Varkey, E.; Cider, Å.; Carlsson, J.; Linde, M. A Study to Evaluate the Feasibility of an Aerobic Exercise Program in Patients with Migraine. Headache J. Head Face Pain 2009, 49, 563–570. [Google Scholar] [CrossRef]
- Long, C.; Ye, J.; Chen, M.; Gao, D.; Huang, Q. Effectiveness of yoga therapy for migraine treatment: A meta-analysis of randomized controlled studies. Am. J. Emerg. Med. 2022, 58, 95–99. [Google Scholar] [CrossRef]
- Wu, Q.; Liu, P.; Liao, C.; Tan, L. Effectiveness of yoga therapy for migraine: A meta-analysis of randomized controlled studies. J. Clin. Neurosci. 2022, 99, 147–151. [Google Scholar] [CrossRef]
- Mehta, J.N.; Parikh, S.; Desai, S.D.; Solanki, R.C.; Pathak, A.G. Study of Additive Effect of Yoga and Physical Therapies to Standard Pharmacologic Treatment in Migraine. J. Neurosci. Rural. Pract. 2021, 12, 060–066. [Google Scholar] [CrossRef]
- Lemstra, M.; Stewart, B.; Olszynski, W.P. Effectiveness of Multidisciplinary Intervention in the Treatment of Migraine: A Randomized Clinical Trial. Headache J. Head Face Pain 2002, 42, 845–854. [Google Scholar] [CrossRef]
- Bond, D.S.; Thomas, J.G.; Lipton, R.B.; Roth, J.; Pavlovic, J.M.; Rathier, L.; O’Leary, K.C.; Evans, E.W.; Wing, R.R. Behavioral Weight Loss Intervention for Migraine: A Randomized Controlled Trial. Obesity 2018, 26, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Seok, J.I.; Cho, H.I.; Chung, C.-S. From Transformed Migraine to Episodic Migraine: Reversion Factors. Headache J. Head Face Pain 2006, 46, 1186–1190. [Google Scholar] [CrossRef] [PubMed]
- Gaul, C.; van Doorn, C.; Webering, N.; Dlugaj, M.; Katsarava, Z.; Diener, H.-C.; Fritsche, G. Clinical outcome of a headache-specific multidisciplinary treatment program and adherence to treatment recommendations in a tertiary headache center: An observational study. J. Headache Pain 2011, 12, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Meyer, B.; Keller, A.; Wöhlbier, H.-G.; Overath, C.H.; Müller, B.; Kropp, P. Progressive muscle relaxation reduces migraine frequency and normalizes amplitudes of contingent negative variation (CNV). J. Headache Pain 2016, 17, 37. [Google Scholar] [CrossRef]
- Minen, M.T.; Adhikari, S.; Padikkala, J.; Tasneem, S.; Bagheri, A.; Goldberg, E.; Powers, S.; Lipton, R.B. Smartphone-Delivered Progressive Muscle Relaxation for the Treatment of Migraine in Primary Care: A Randomized Controlled Trial. Headache J. Head Face Pain 2020, 60, 2232–2246. [Google Scholar] [CrossRef]
- Meyer, B.; Keller, A.; Müller, B.; Wöhlbier, H.-G.; Kropp, P. Progressive Muskelrelaxation nach Jacobson bei der Migräneprophylaxe. Der Schmerz 2018, 32, 250–258. [Google Scholar] [CrossRef]
- Santiago, M.D.S.; Carvalho, D.d.S.; Gabbai, A.A.; Pinto, M.M.P.; Moutran, A.R.C.; Villa, T.R. Amitriptyline and aerobic exercise or amitriptyline alone in the treatment of chronic migraine: A randomized comparative study. Arq. Neuropsiquiatr. 2014, 72, 851–855. [Google Scholar] [CrossRef][Green Version]
- Köseoglu, E.; Akboyraz, A.; Soyuer, A.; Ersoy, A. Aerobic Exercise and Plasma Beta Endorphin Levels in Patients with Migrainous Headache Without Aura. Cephalalgia 2003, 23, 972–976. [Google Scholar] [CrossRef]
- Xie, Y.J.; Tian, L.; Hui, S.S.-C.; Qin, J.; Gao, Y.; Zhang, D.; Ma, T.; Suen, L.K.P.; Wang, H.H.; Liu, Z.-M.; et al. Efficacy and feasibility of a 12-week Tai Chi training for the prophylaxis of episodic migraine in Hong Kong Chinese women: A randomized controlled trial. Front. Public Health 2022, 10, 1000594. [Google Scholar] [CrossRef]
- Benatto, M.T.; Florencio, L.L.; Bragatto, M.M.; Dach, F.; Fernández-De-Las-Peñas, C.; Bevilaqua-Grossi, D. Neck-specific strengthening exercise compared with sham ultrasound when added to home-stretching exercise in patients with migraine: Study protocol of a two-armed, parallel-groups randomized controlled trial. Chiropr. Man. Ther. 2020, 28, 22. [Google Scholar] [CrossRef]
- Reina-Varona, Á.; Madroñero-Miguel, B.; Gaul, C.; Hall, T.; Oliveira, A.B.; Bond, D.S.; Peñas, C.F.-D.L.; Florencio, L.L.; Carvalho, G.F.; Luedtke, K.; et al. Therapeutic Exercise Parameters, Considerations, and Recommendations for Migraine Treatment: An International Delphi Study. Phys. Ther. 2023, 103, pzad080. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).