Abstract
Objectives: The influence of comorbidity on long-term hospitalization and mortality after COVID-19 in adults (40–59 years) and older adults (≥60 years) is yet to be explored. Methods: This is a Danish population-based cohort study of patients with a first-time positive PCR test for COVID-19 from 1 March 2020, to 28 February 2022 (N = 1,034,103). Exposed cohorts were patients with 1) a Charlson Comorbidity Index (CCI) score of 1–2 and 2) a CCI score ≥3, who were compared to patients without comorbidity (CCI of zero) within the groups of adults (67.9%) and older adults (32.1%) for the risk of hospitalization and mortality. Next, within the age groups, each disease category of the CCI was considered as an exposed cohort and compared to patients who did not have the specific disease of interest. Adjusted hazard ratios (HR) for hospitalization and mortality were estimated by Cox regression models adjusted for confounders. Results: The highest HRs were in adult patients with a CCI score of ≥3. The adjusted HR was 4.54 (95%CI: 4.38–4.70) for hospitalization, and among older adults it was 3.05 (95%CI: 2.99–3.11). The adjusted HR for mortality among adults with a CCI score ≥3 was 21.04 (95%CI: 18.86–23.47), and the adjusted HR for mortality among older adults was 4.61 (95%CI: 4.44–4.78). The underlying disease influenced the risk estimates among adults and older adults, and “dementia” had the highest impact on mortality. Conclusion: A CCI score of 1 or above increases the risk of hospitalization and mortality up to 2 years after a positive PCR test of COVID-19 for adults and older adults. Further, the type of underlying disease in older adults highly influences the risk of hospitalization and mortality.
1. Introduction
SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) infection, known as COVID-19, emerged in December 2019 in Wuhan, China, and spread around the world on an unprecedented scale [1,2]. In different study populations, the consequences of COVID-19 have been examined with a focus on short-term consequences [3,4,5,6].
The risk of infection by COVID-19 is present in both adults (40–59 years) and older adults (≥60 years), but the consequences differ by various predictors where the impact of comorbidity is an important focus area. Comorbidity can be present in all age groups, but in the general population, a higher age also often implies more comorbidity, which gives a special focus on the consequences for adults and older adults [7].
It is well known that age is an independent risk factor for a more serious disease course in the acute phase of the infection [3,4,6,8,9]. Other independent risk factors are male gender and comorbidities that negatively influence on outcomes after COVID-19 infections, i.e., increased severity, increased length of hospital stay, and mortality within short-term follow-up (30 days to 60 days) [3,4,10]. The number of comorbidities has also been shown to be a strong predictor of COVID-19 severity and death within 30 days [3].
It is not well explored to what extent comorbidity and age group may predict long-term adverse outcomes after COVID-19. Additionally, the impact of a single underlying disease on long-term adverse outcomes after COVID-19 in different age groups has not yet been assessed in a nationwide register-based study. Therefore, we aimed to examine the long-term impact of comorbidity in adults (40–59 years) and older adults (≥60 years) who have had a positive COVID-19 polymerase chain reaction (PCR) test, with respect to any hospitalization and mortality within 2 years.
2. Methods
2.1. Setting, Study Design, and Study Population
This is a Danish population-based cohort study. The study population included adults and older adults with an age above 40 years with a COVID-19 PCR test from 1 March 2020 to 28 February 2022. In Denmark, the health care system is tax-financed and with free access for all citizens. The Danish population is predominantly Caucasian (>90%) and there are approximately 5.9 million inhabitants. The uniform health care system and the use of nationwide registers with key information enables us to use an unselected nationwide study design [11,12]. We had access to the Danish Civil Registration System, the National Patient Register, and the nationwide COVID-19 surveillance database (PCR test results for COVID-19), which were made available by Statens Serum Institut to Danish researchers and stored in the Danish Microbiology Database [11,13,14,15]. In Denmark, the COVID-19 pandemic began at the end of February 2020, and community transmission of COVID-19 was present by March 2020 [5].
2.2. Data Sources
The Danish Departments of Clinical Microbiology and Statens Serum Institut carried out laboratory analysis, registration, and release of the national SARS-CoV-2 surveillance data for the present study. The surveillance data include all first-time positive PCR tests for COVID-19 and the personal identification number. Only data on the first positive PCR test for each individual are available. Data on vaccinations include the date of the first, second, and third vaccination and the brand used. The National Patient Register was established in 1977 and holds information from all hospitals on discharges and information on outpatient visits since 1994 [11]. The National Patient Register holds information on the personal identification number, the date of admission plus discharge, and procedure codes for in-hospital treatments. Discharge diagnoses are classified using the International Classification of Disease system (Version 8 was used before 1994, and version 10 after 1994). The Danish Civil Registration System was established in 1968 for all persons living in Denmark and includes key information such as personal identification number, sex at birth, date of birth, immigration, and mortality [14,15]. Data linkage between the registers with COVID-19 surveillance data, COVID-19 vaccination data, the National Patient Register, and the Danish Civil Registration System is possible at an individual level using the unique personal identification number given to all Danish citizens at birth.
3. Cohorts, Exposed and Unexposed
The study population was divided into two age groups, adults (40–59 years) and older adults (≥60 years), and examined separately for the impact of comorbidity in COVID-19 PCR-positive individuals. We used the Charlson Comorbidity Index (CCI) with 10 years of medical history (calculated backward from the date of the first PCR test) [16]. We chose the CCI as the prediction ability has been found appropriate in a Danish setting [17]. We used two different strategies to examine the influence of comorbidity. Firstly, within each age group, we created two separate exposed cohorts of patients with (1) a CCI score of 1–2 and (2) a CCI score ≥3. In both age groups, the reference groups were patients with a CCI score of null. Secondly, we examined the separate effects of each of the underlying diseases included in the CCI. Each specific disease category of the CCI was considered as a separate exposed cohort (in total nine exposed cohorts, as we merged three of the disease categories due to low numbers), and the reference group was patients with a CCI score of null. In these analyses, a patient may be represented in more than one disease category in these comparisons. The CCI was used as the prognostic value of the chronic diseases changed over time. These selected diseases are chosen based on one version of the CCI, and represent the most important non-malignant disease categories that have been shown to have significant prognostic value (i.e., assigned a weight of ≥1, congestive heart failure, dementia, chronic pulmonary disease, rheumatologic disease, mild liver disease, diabetes with chronic complications, hemiplegia or paraplegia, renal disease, and moderate or severe liver disease) [18].
3.1. Outcomes
The outcomes were any kind of hospitalization and mortality with 2 years of follow-up. Any hospitalization (yes/no) was retrieved from the National Patient Register. Any hospitalization was registered and the duration of admission was defined as a minimum of 12 h. We used the first hospitalization after the first positive COVID-19 test in case of multiple hospitalizations. Information on mortality was retrieved from the Danish Civil Registration System.
3.2. Statistics and Confounders
We tabulated baseline data of the age groups, adults and older adults, reporting the frequency and percentages of the main variables. Initially, within each age group, we estimated the hazard ratio (HR) of the outcomes in the groups with a CCI score of 3 or more versus those with no comorbidity (CCI score of zero), and those with a CCI score of 1–2 to those with no comorbidity. We used Cox regression models (multivariable) to compute the crude HR and adjusted HR (aHR) for any hospitalization and mortality. In the analysis for hospitalization, we adjusted the models for sex, age as a continuous variable, and number of vaccinations. In the analysis of mortality, we adjusted for sex, age as a continuous variable, number of vaccinations, and hospitalization as a time-varying variable. Next, we examined the impact of a specific single underlying disease category according to the CCI. We compared each disease category of the CCI to those without the specific disease of interest in a univariable model, i.e., those identified with congestive heart failure were compared to those without congestive heart failure. In these analyses, we adjusted for other comorbid diseases from the CCI, sex, age as a continuous variable, number of vaccinations, and hospitalization in a multivariable model. In the analysis of hospitalization we did not include hospitalization. A patient represented in more than one CCI category was eligible for each of the individual comparisons.
In a sensitivity analysis, according to the analysis of mortality, we tried to omit hospitalization as a time-varying variable from the regression model. In another sensitivity we examined the impact of CCI categories of 0, 1, 2, 3, and ≥4, and in a final analysis of mortality and hospitalization we included age as cubic splines in the model.
We retrieved information on sex and age at the time of a positive COVID-19 PCR test from the National Patient Register and the Danish Civil Registration System. In addition, we retrieved information on the type of hospitalization to the intensive care unit within 7 days after the PCR-positive test, but the variable was solely included for descriptive purposes and not used as a confounder. We retrieved information from the national SARS-CoV-2 surveillance data on the number of vaccinations. All confounders were selected a priori.
3.3. Approval and Ethics
This nationwide register study was approved by the Danish Data Protection Agency under the joint notification of the Region of Southern Denmark (Journal no.: 20/21823). Data were accessed through a secure server at the Danish Health Authorities. Studies based on register-based data that do not involve any direct contact with patients do not require ethical approval according to Danish law.
4. Results
In this cohort study, we included 1,034,103 persons with a positive PCR test, where 702,081 (67.9%) were adults aged 40–59 years and 332,022 (32.1%) were older adults aged ≥60 years. In the adult group, 371,718 (52.9%) were females, and 171,859 (51.8%) among older adults were females. In the adult group, 607,824 (86.6%) had no registered comorbidity according to the CCI, and among older adults, 202,773 (61.1%) had no comorbidity. The most predominant category of disease from the CCI was rheumatologic disease with 10,657 (1.5%) in the adult group, and likewise among older adults with 12,206 (3.7%) persons. Within 7 days after the first positive PCR test, 2559 (0.4%) of the adults and 9035 (2.7%) of the older adults were hospitalized. Table 1 describes the basic characteristics of the study population.

Table 1.
Characteristic of Danish PCR-positive COVID-19 (first) according to adult (40–59 years) and older adult (≥60 years) patients from 1 March 2020 to 28 February 2022.
4.1. CCI Score and the Risk of Hospitalization and Mortality Within 2 Years
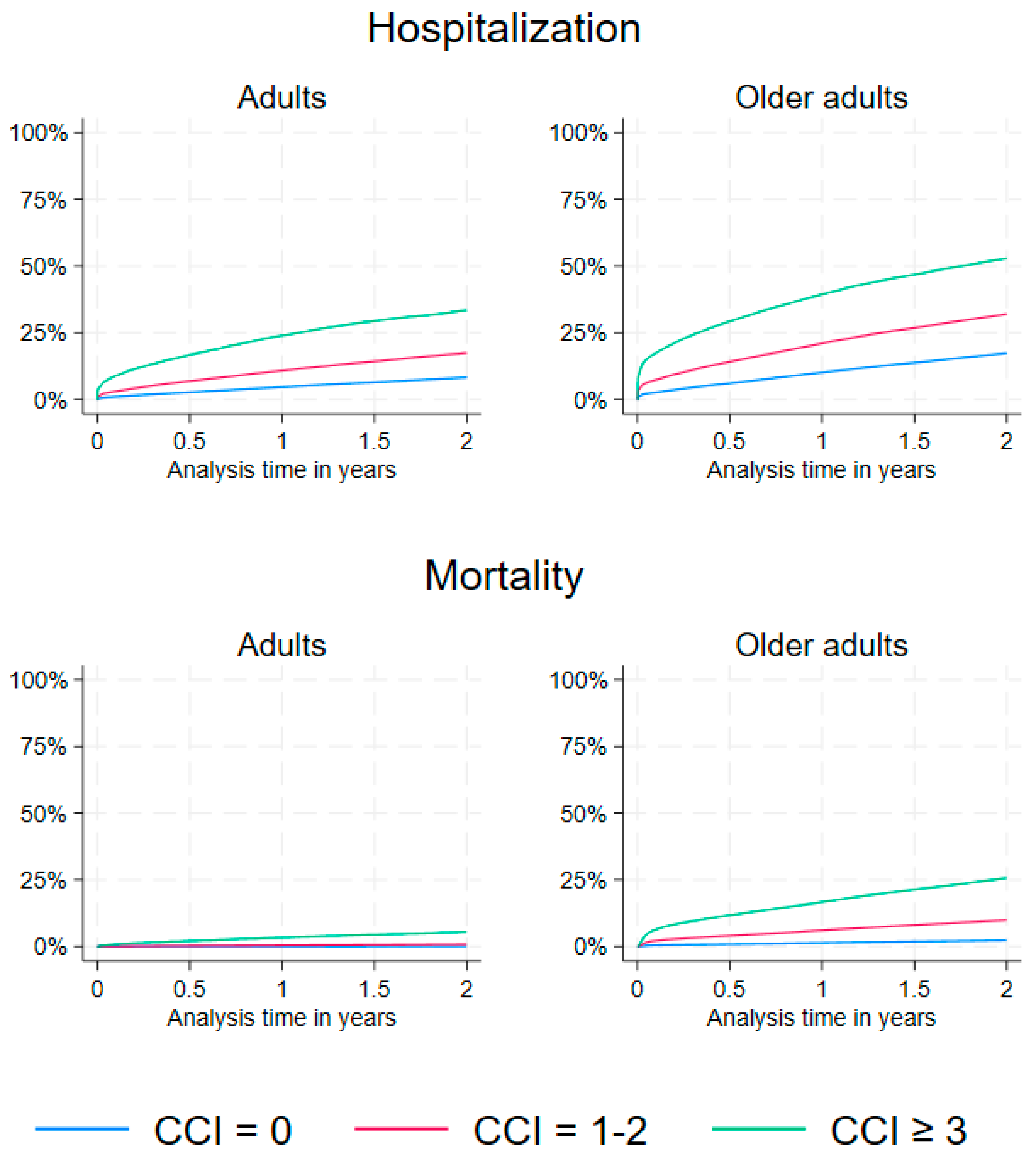
The percentage of hospitalization within 2 years after a positive COVID-19 PCR test among adults increased with a higher CCI score. Specifically, hospitalization occurred in 8.2% of adults with a CCI score of 0, 17.4% of those with a CCI score of 1–2, and 33.3% of those with a CCI score of ≥3 (Table 2, Figure 1). Likewise, hospitalizations occurred in 17.3%, 31.4%, and 51.1% among older adults with CCI scores 0, 1–2, and ≥3, respectively (Table 2, Figure 1). The risk of hospitalization was increased in the CCI score 1–2 and ≥3 compared to persons without comorbidity in the adults and older adults group within 2 years of follow-up (Table 2). The highest adjusted risk estimate was 4.54 (95%CI: 4.38–4.70) in the adult group whereas the risk estimate in the older adult group was 3.05 (95%CI: 2.99–3.11) (Table 2).

Table 2.
Outcomes according to CCI score in Danish PCR-positive COVID-19 (first) patients by adults (40–59 years) and older adults (≥60 years).
Figure 1.
A panel of the cumulative incidence percentage of hospitalization (any kind) and mortality according to CCI score by adults (40–59 years, left panel) and older adults (≥60 years, right panel) in Danish PCR-positive COVID-19 patients with 2 years of follow-up.
Mortality in adults ranged from 0.2% in the group without comorbidity to 0.8% and 5.5% in the group with a CCI score of 1–2 or ≥3, respectively (Table 2, Figure 1). In older adults, the mortality was higher with 2.4% in the group without comorbidity, and 9.9% and 25.7% in the group with a CCI score of 1–2 or ≥3, respectively (Table 2, Figure 1). The adjusted risk of mortality for adults and older adults was increased depending on the CCI score categories 1–2 and ≥3 compared to persons with no comorbidity (Table 2). The highest adjusted risk of mortality was among adults with a CCI score ≥3 with 21.04 (95%CI: 18.86–23.47), and the risk of mortality among older adults was 4.61 (95%CI: 4.44–4.78) (Table 2). In the sensitivity analysis of mortality, where we omitted hospitalization from the model, the conclusions did not change.
4.2. CCI Disease Categories and Risk of Hospitalization and Mortality
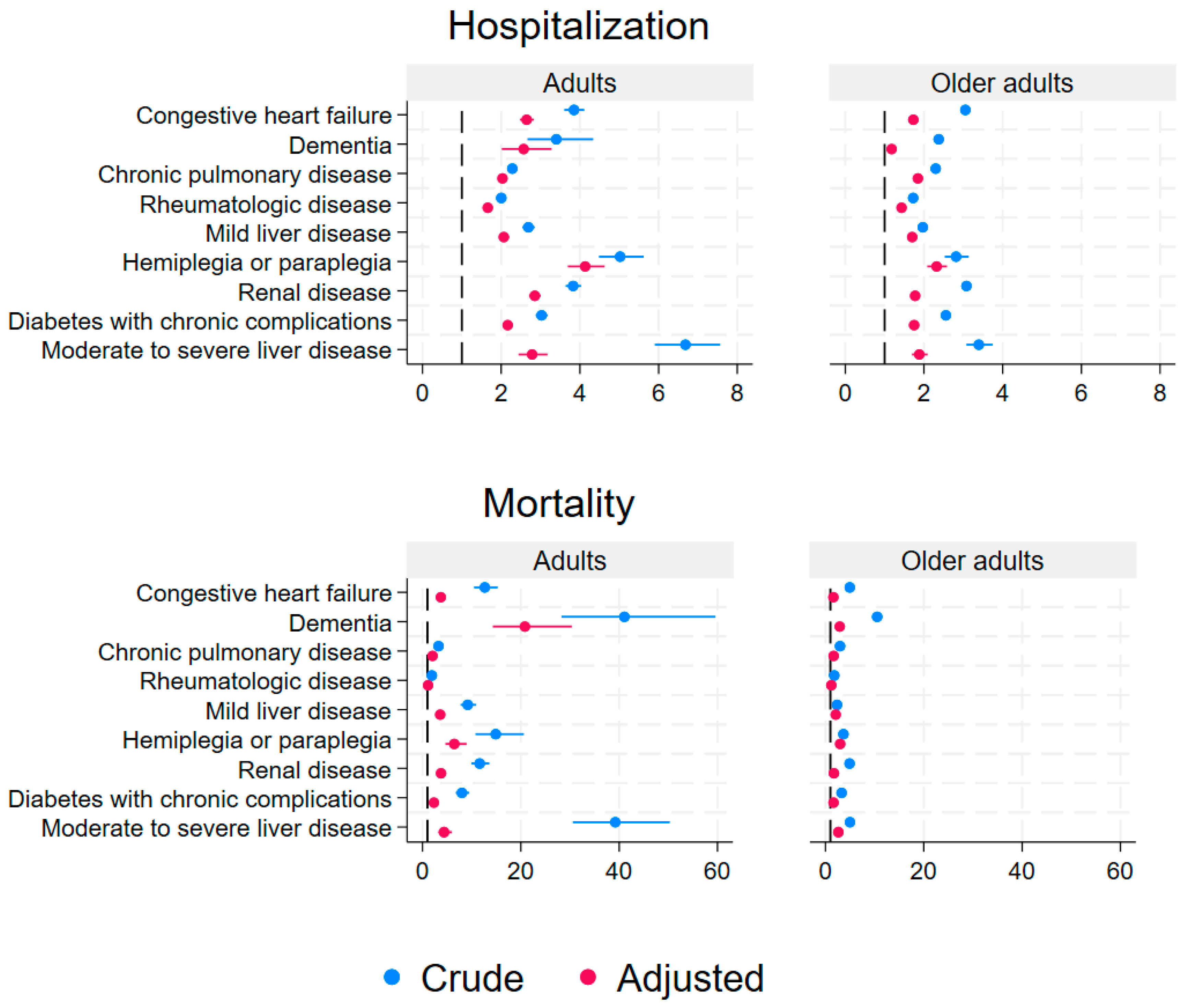
Figure 2 shows the crude and adjusted risk estimates for hospitalization and mortality by disease categories from the CCI for adults and older adults. In adults, the three highest adjusted risk estimates for hospitalization were patients with hemiplegia or paraplegia with a HR of 4.13 (95%CI: 3.69–4.63), renal disease with a HR of 2.85 (95%CI: 2.71–3.01), and moderate or severe liver disease with a HR of 2.78 (95%CI: 2.44–3.18) (Figure 2, Supplementary Table S1). In older adults, the three highest adjusted risk estimates for hospitalization were patients with hemiplegia or paraplegia with a HR of 2.32 (95%CI: 2.08–2.58), and moderate or severe liver disease with a HR of 1.88 (95%CI: 1.69–2.09), and chronic pulmonary disease with a HR of 1.84 (95%CI: 1.81–1.88) (Figure 2, Supplementary Table S1).
Figure 2.
A panel of the crude and adjusted risk estimates for hospitalization and mortality by nine disease categories from the Charlson Comorbidity Index in adults (40–59 years, left panel) and older adults (≥60 years, right panel) with a PCR-positive COVID-19 test in Denmark with 2 years of follow-up.
All adjusted risk estimates for hospitalization depending on specific types of underlying disease categories among adults and older adults were statistically significantly increased, ranging from a HR of 1.18 (95%CI: 1.14–1.22) to 4.13 (95%CI: 3.69–4.63) (Figure 2, Supplementary Table S1). The type of underlying disease, associated with the highest proportions of hospitalization, was “moderate or severe liver disease” for adults at 46.7%, and in older adults it was also “moderate or severe liver disease” at 58.2%. For adults, the proportions of hospitalizations of different disease categories ranged from 18.2–46.7%, and in older adults, the proportions ranged from 37.4–58.2% (Supplementary Table S1).
All adjusted risk estimates for mortality in disease categories were statistically significantly increased in adults and older adults ranging from a HR of 1.61 (95%CI: 1.55–1.68) to 20.83 (95%CI: 14.28–30.37), except for adults with rheumatologic disease, where the HR was 1.13 (95%CI: 0.88–1.45) (Figure 2, Supplementary Table S1). The type of underlying disease with the highest proportions of mortality was “dementia” with 12.2% in adults and 47.6% in older adults (Supplementary Table S1). The percentage of mortality varied depending on disease categories from 0.6% to 12.2% in adults and from 11.7% to 47.6% in older adults (Supplementary Table S1). The sensitivity analysis, where we examined the impact of CCI categories of 0, 1, 2, 3, and ≥4, showed higher HRs with increasing CCI (Supplementary Table S2). Including age as cubic splines instead of a linear variable in the model did not change the results (Supplementary Table S2 and Figure S2).
5. Discussion
From 1 March 2020 to 28 February 2022 in this Danish nationwide cohort study, we identified 1,034,103 adults (40 years or older) with PCR-positive COVID-19, of which 32% were older adults aged ≥60 years. Hospitalization of any kind increased among adults and older adults with increasing CCI scores. In adults, the hospitalization rate ranged from 8.2% to 33.3%, and in older adults, it ranged from 17.3% to 51.1%, according to the cohort categorized by CCI. Comorbidity by the CCI was associated with an increased risk of hospitalization. Mortality increased with increasing CCI scores, regardless of age group. The mortality ranged from 0.2% to 5.5% in adults, and 2.4% in older adults to 25.7% according to the cohort categorized by CCI. We found that the risk of either outcome increased statistically significantly with increasing CCI scores in both adults and older adults, even in patients with a low CCI score of 1–2. When examining the different disease categories from the CCI in adults and older adults, the categories of “moderate or severe liver disease” were the most prognostic type of disease associated with hospitalizations. The risk of mortality was highest in the group of older adults with a CCI score of ≥3 compared to older adults without comorbidity, and “dementia” was the most frequent category for mortality for both age groups.
5.1. Hospitalization
The risk of any hospitalization was increased with increasing CCI category and the risk was increased for all disease categories, especially “dementia” and “renal disease”. The increased risk of hospitalization of our study was similar to the short-term increased risk reported by Reilev et al. [5], and in alignment with the observation of more frequent comorbidities among COVID-19 PCR-positive hospitalized patients [5]. Similar to Reilev et al. [5], the risk for any hospitalization was increased in all categories in our study, and this influence of age was also found in previous studies in other populations [19,20]. In addition, our study found that patients in the category “moderate or severe liver disease” were the ones with the most frequent hospitalizations.
5.2. Mortality
The risk of mortality after COVID-19 has been studied extensively on a short-term basis [6]. Several risk factors have been identified, such as age and comorbidity, and in our study, the risk of mortality was highest in the group of older adults with a CCI score of ≥3 compared to older adults without comorbidity. This finding extends our knowledge of the influence of comorbidity as a risk factor for mortality within 30 days, as found by Reilev et al. [5], where the number of comorbidities increased the risk of mortality and increasing age also increased the risk of mortality among Danish citizens. In a Canadian cohort, Ge et al. [3] have documented that pre-existing comorbidity was a prediction for 30-day mortality in individuals with COVID-19. Again, this study adds a long-term perspective on these associations when using the CCI as the exposure. Our results are not easily comparable with other studies because most studies have been focused on short-term outcomes. This is highlighted in a recent systematic review where an increasing number of diseases, a higher CCI, and an increased frailty level were shown to increase the likelihood of hospitalization and mortality, and where long-term outcomes were warranted [6]. Our study also showed that the risk for mortality was increased for nearly all categories of disease in older adults and adults, except for adult patients with “rheumatologic disease”. In a Swedish cohort of patients with COVID-19 requiring intensive care with one year of follow-up, mortality after 90 days was low, and males had an increased risk of mortality compared to women [21]. Exposure to COVID-19 in patients with comorbidities and long-term mortality could be related to several prognostic factors. Hägglöf et al. [21] found that several diseases, e.g., cardiac disease, COPD/asthma, diabetes, chronic liver disease, and chronic kidney disease were associated with higher mortality. The underlying mechanism for each of the factors may vary and be multifactorial as age also is a known risk factor for mortality in patients with COVID-19 [21,22]. Furthermore, patients with critical illnesses due to COVID-19 are perceived to have an increased risk of mortality later [23].
This study has several strengths. First, we used data from the Danish nationwide health registers, which are well-validated, and included data for the entire population, eliminating selection bias [11]. The unique data linkage between the Danish health registers and mandatory reporting to the registers also enables complete follow-up for all patients, which again eliminates selection bias. Secondly, the data on exposure are registered independently of the outcome data due to the prospectively mandatory reporting to the registers, reducing any information bias. The surveillance database has captured all PCR test results for COVID-19 since the beginning of the pandemic, the diagnosis in the Danish National Patient Register is based on ICD-10 coding, and extensive validation studies have been done [11]. Thirdly, our study adjusted for several important confounders such as sex, age, number of vaccinations, hospitalization, and sequelae of COVID-19 when estimating the long-term risk. Lastly, in Denmark, the COVID-19 pandemic began at the end of February 2020, and at the end of March 2020 the PCR test capacity for COVID-19 was up-scaled to include all individuals with mild to moderate respiratory symptoms suspicious of COVID-19 [5]. The extensive nationwide testing strategy used in Denmark reduced the risk of misclassification. Even though PCR has a high false-negative rate and can be biased towards specific groups, they are considered the best to detect COVID-19 [24].
The study is limited by only using the first available PCR test for COVID-19 for the patients and does not include repeated testing data. In this study, we focused on patients with a positive PCR test, and we were therefore not able to compare with “healthy patients” without COVID-19. The long-term consequences of COVID-19 were thus not compared with a non-COVID-19 cohort of healthy patients or patients with other acute infections to evaluate disease specific outcomes. In our analysis of mortality, we included hospitalization as a confounder. It could be argued that hospitalization is a mediator and not a confounder for these outcomes, but most often patients are hospitalized due to the severity of COVID-19 even though no exact threshold for hospitalization is available from an epidemiological point of view. By adjusting for hospitalization in our analysis we aim to take a proxy measure for the severity of COVID-19 into account. The focus on long-term outcomes for COVID-19 may introduce detection bias because of the introduction of home tests for COVID-19 in 2022, but in our study, we only included PCR-test data for COVID-19 until 28 February 2022, and hereby this bias should be of minor concern. Another limitation is that we have not included biomarkers and other relevant laboratory parameters, such as antinuclear antibodies (ANA) to COVID-19, which are prognostic factors for worse disease [25]. In patients with COVID-19, C-reactive protein levels and the neutrophil-to-lymphocyte ratio have been found to be a potential predictor of mortality [26]. The implication of these inflammatory biomarkers could potentially be examined in future studies focusing on patients with COVID-19 who experience delirium, where inflammation may have a significant role in the pathogenesis of delirium [27]. Additionally, we did not have data on whether patients were treated for their comorbid diseases and the severity of underlying disease, which could provide the basis for future additional analyses of the impact of comorbidity. When using observational register data for research, some inherent limitations are present and should be taken into consideration. This could be unmeasured or residual confounding, even though we were able to adjust for several confounders in our analyses. Furthermore, our data are not suitable to establish the underlying causes from exposure to COVID-19 to hospitalization or mortality, but are excellent for examining associations.
In conclusion, even minor comorbidity (a CCI score of 1–2) increases the risk of any type of hospitalization and mortality up to 2 years after a positive PCR test for COVID-19. There has been a general perception that high comorbidity is associated with worse COVID-19 outcomes, but our study shows that, regardless of age group, only mild comorbidity is associated with hospitalization and death. Furthermore, our study underlines that it is too simple just to refer to the importance of a high or low general status of comorbidity when considering long-term COVID-19 outcomes. In fact, our study shows that it is highly important to consider the impact of each individual’s specific type of underlying disease when it comes to COVID-19 outcomes. Some of the most serious types of underlying disease were hemiplegia or paraplegia, dementia, and moderate-severe liver disease. In this study, we have only examined the long-term risk of hospitalization and mortality after COVID-19. Future studies should examine other COVID-19 outcomes based on patients with certain risk profiles according to types of underlying diseases.
5.3. Patient and Public Involvement
We have presented the initial conceptualization and design of the study for patients and relative representatives who are a part of the research council at the Center for Clinical Epidemiology, Odense University Hospital. The representatives have contributed with input for the selection of the study population and ideas for choosing important outcomes. The representatives have not been involved in the conduct of the study.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13216522/s1. Table S1. Outcomes according to CCI category in Danish PCR-positive COVID-19 (first) by Adults (40–59 years) and older adults (≥60 years) patients. Table S2. Sensitivity. Outcomes according to CCI score in Danish PCR-positive COVID-19 (first) patients by adults (40–59 years) and older adults (≥60 years), when using the age variable as a linear and with cubic splines. Figure S1. Sensitivity. A panel of the crude and adjusted risk estimates for hospitalization and mortality by 9 disease categories from the Charlson comorbidity index in adults (40–59 years, left panel) and older adults (≥60 years, right panel) with a PCR-positive COVID-19 test in Denmark with 2 years of follow-up, when using the age variable as a linear and with cubic splines.
Author Contributions
K.L., J.N., T.K., B.M.N. and J.K. were involved in the conception and design of the study. B.M.N. and J.N. undertook the acquisition of data. J.N. carried out the formal analysis. K.L., J.N., S.K., P.P., T.K., B.M.N. and J.K. stand for the interpretation of data, drafting the article, and revising it critically for important intellectual content. K.L., J.N., S.K., P.P., T.K., B.M.N. and J.K. undertook final approval of the version to be submitted. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by Pfizer Inc. grant number 77494657. The funding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
Institutional Review Board Statement
Studies based on register-based data that do not involve any direct contact with patients do not require ethical approval according to Danish law.
Informed Consent Statement
Not applicable.
Data Availability Statement
The Danish nationwide data used in this study that supports the findings are accessible in raw format, and can be requested from the Danish Health Data Authority (kontakt@sundhedsdata.dk). The acquisition of data is limited and an application for an individual license for a research project is required. The authors do not have special privileges for acquiring the data.
Conflicts of Interest
K.L. is a full-time employee at NHTA and participated in consulting with the life science and pharmaceutical industry. P.P. has received honoraria from Merck Sharp & Dohme, Gilead, Mundipharma, and Pfizer. P.P. has participated in advisory boards for Merck Sharp & Dohme, Sanofi, Gilead, and Biocodex. J.N., S.K., T.K., B.M.N. and J.K. have no conflicts of interest.
References
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef] [PubMed]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Ge, E.; Li, Y.; Wu, S.; Candido, E.; Wei, X. Association of pre-existing comorbidities with mortality and disease severity among 167,500 individuals with COVID-19 in Canada: A population-based cohort study. PLoS ONE 2021, 16, e0258154. [Google Scholar] [CrossRef]
- Huang, Y.-T.; Steptoe, A.; Patel, R.S.; Thomson, F.E.; Cadar, D. The Impact of Long-Term Conditions and Comorbidity Patterns on COVID-19 Infection and Hospitalisation: A Cohort Study. Gerontology 2023, 69, 1200–1210. [Google Scholar] [CrossRef]
- Reilev, M.; Kristensen, K.B.; Pottegård, A.; Lund, L.C.; Hallas, J.; Ernst, M.T.; Christiansen, C.F.; Sørensen, H.T.; Johansen, N.B.; Brun, N.C.; et al. Characteristics and predictors of hospitalization and death in the first 11 122 cases with a positive RT-PCR test for SARS-CoV-2 in Denmark: A nationwide cohort. Int. J. Epidemiol. 2020, 49, 1468–1481. [Google Scholar] [CrossRef] [PubMed]
- Makovski, T.T.; Ghattas, J.; Besnard, S.M.; Ambrozova, M.; Vasinova, B.; Feteira-Santos, R.; Bezzegh, P.; Bollmann, F.P.; Cottam, J.; Haneef, R.; et al. Multimorbidity and frailty are associated with poorer SARS-CoV-2-related outcomes: Systematic review of population-based studies. Aging Clin. Exp. Res. 2024, 36, 40. [Google Scholar] [CrossRef]
- Stockmarr, A.; Frolich, A. Clusters from chronic conditions in the Danish adult population. PLoS ONE 2024, 19, e0302535. [Google Scholar] [CrossRef]
- Pijls, B.G.; Jolani, S.; Atherley, A.; Derckx, R.T.; Dijkstra, J.I.R.; Franssen, G.H.L.; Hendriks, S.; Richters, A.; Venemans-Jellema, A.; Zalpuri, S.; et al. Demographic risk factors for COVID-19 infection, severity, ICU admission and death: A meta-analysis of 59 studies. BMJ Open 2021, 11, e044640. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.J.; Dong, X.; Liu, G.H.; Gao, Y.D. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin. Rev. Allergy Immunol. 2023, 64, 90–107. [Google Scholar] [CrossRef]
- Bouziotis, J.; Arvanitakis, M.; Preiser, J.C.; ISARIC Clinical Characterisation Group. Association of body mass index with COVID-19 related in-hospital death. Clin. Nutr. 2022, 41, 2924–2926. [Google Scholar] [CrossRef]
- Schmidt, M.; Schmidt, S.A.; Sandegaard, J.L.; Ehrenstein, V.; Pedersen, L.; Sorensen, H.T. The Danish National Patient Registry: A review of content, data quality, and research potential. Clin. Epidemiol. 2015, 7, 449–490. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, T. Organization and financing of the Danish health care system. Health Policy 2002, 59, 107–118. [Google Scholar] [CrossRef] [PubMed]
- Voldstedlund, M.; Haarh, M.; Mølbak, K.; the MiBa Board of Representatives. The Danish Microbiology Database (MiBa) 2010 to 2013. Eurosurveillance 2014, 19, 20667. [Google Scholar] [CrossRef]
- Pedersen, C.B. The Danish Civil Registration System. Scand. J. Public Health 2011, 39, 22–25. [Google Scholar] [CrossRef]
- Schmidt, M.; Pedersen, L.; Sorensen, H.T. The Danish Civil Registration System as a tool in epidemiology. Eur. J. Epidemiol. 2014, 29, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Vesterager, J.D.; Madsen, M.; Hjelholt, T.J.; Kristensen, P.K.; Pedersen, A.B. Prediction Ability of Charlson, Elixhauser, and Rx-Risk Comorbidity Indices for Mortality in Patients with Hip Fracture. A Danish Population-Based Cohort Study from 2014–2018. Clin. Epidemiol. 2022, 14, 275–287. [Google Scholar] [CrossRef]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.-M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Mason, K.E.; Maudsley, G.; McHale, P.; Pennington, A.; Day, J.; Barr, B. Age-Adjusted Associations Between Comorbidity and Outcomes of COVID-19: A Review of the Evidence From the Early Stages of the Pandemic. Front. Public Health 2021, 9, 584182. [Google Scholar] [CrossRef]
- Hägglöf, E.; Bell, M.; Zettersten, E.; Engerström, L.; Larsson, E. Long-term survival after intensive care for COVID-19: A nationwide cohort study of more than 8000 patients. Ann. Intensive Care 2023, 13, 76. [Google Scholar] [CrossRef] [PubMed]
- Guillon, A.; Laurent, E.; Godillon, L.; Kimmoun, A.; Grammatico-Guillon, L. Long-term mortality of elderly patients after intensive care unit admission for COVID-19. Intensive Care Med. 2021, 47, 710–712. [Google Scholar] [CrossRef] [PubMed]
- Higgins, A.M.; Berry, L.R.; Lorenzi, E.; Murthy, S.; McQuilten, Z.; Mouncey, P.R.; Al-Beidh, F.; Annane, D.; Arabi, Y.M.; Beane, A.; et al. Long-term (180-Day) Outcomes in Critically Ill Patients With COVID-19 in the REMAP-CAP Randomized Clinical Trial. JAMA 2023, 329, 39–51. [Google Scholar] [PubMed]
- Grønkjær, C.S.; Christensen, R.H.B.; Kondziella, D.; Benros, M.E. Long-term neurological outcome after COVID-19 using all SARS-CoV-2 test results and hospitalisations in Denmark with 22-month follow-up. Nat. Commun. 2023, 14, 4235. [Google Scholar] [CrossRef] [PubMed]
- Muratori, P.; Lenzi, M.; Muratori, L.; Granito, A. Antinuclear antibodies in COVID 19. Clin. Transl. Sci. 2021, 14, 1627–1628. [Google Scholar] [CrossRef]
- Regolo, M.; Vaccaro, M.; Sorce, A. Neutrophil-to-Lymphocyte Ratio (NLR) Is a Promising Predictor of Mortality and Admission to Intensive Care Unit of COVID-19 Patients. J. Clin. Med. 2022, 11, 2235. [Google Scholar] [CrossRef]
- Simone, M.J.; Tan, Z.S. The role of inflammation in the pathogenesis of delirium and dementia in older adults: A review. CNS Neurosci. Ther. 2011, 17, 506–513. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).