AM-PAC 6-Clicks Basic Mobility and Daily Activities Scores Predict 90-Day Modified Rankin Score in Patients with Acute Ischemic Stroke Secondary to Large Vessel Occlusion
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection
2.4. Study Variables and Outcomes
2.5. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Favorable Basic Mobility and Daily Activity Scores Differentiate Patient Outcomes
3.3. Dichotomized Basic Mobility and Daily Activity Scores Are Independent Predictors of Good Stroke Outcomes
3.4. AM-PAC Scores Remain Significant Predictors After Adjusting for Age
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; Howard, V.J.; et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322, Erratum in Circulation 2015, 131, e535. https://doi.org/10.1161/CIR.0000000000000219. Erratum in Circulation 2016, 133, e417. https://doi.org/10.1161/CIR.0000000000000386. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.S.; Lev, M.H.; English, J.D.; Camargo, E.C.; Chou, M.; Johnston, S.C.; Gonzalez, G.; Schaefer, P.W.; Dillon, W.P.; Koroshetz, W.J.; et al. Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA. Stroke 2009, 40, 3834–3840. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saver, J.L.; Chaisinanunkul, N.; Campbell, B.C.V.; Grotta, J.C.; Hill, M.D.; Khatri, P.; Landen, J.; Lansberg, M.G.; Venkatasubramanian, C.; Albers, G.W.; et al. Standardized Nomenclature for Modified Rankin Scale Global Disability Outcomes: Consensus Recommendations from Stroke Therapy Academic Industry Roundtable XI. Stroke 2021, 52, 3054–3062. [Google Scholar] [CrossRef] [PubMed]
- Broderick, J.P.; Adeoye, O.; Elm, J. Evolution of the Modified Rankin Scale and Its Use in Future Stroke Trials. Stroke 2017, 48, 2007–2012. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bowles, K.H.; Ratcliffe, S.J.; Holmes, J.H.; Liberatore, M.; Nydick, R.; Naylor, M.D. Post-acute referral decisions made by multidisciplinary experts compared to hospital clinicians and the patients’ 12-week outcomes. Med. Care 2008, 46, 158–166. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhang, M.Y.; Mlynash, M.; Sainani, K.L.; Albers, G.W.; Lansberg, M.G. Ordinal Prediction Model of 90-Day Modified Rankin Scale in Ischemic Stroke. Front. Neurol. 2021, 12, 727171. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Josephson, S.A.; Hills, N.K.; Johnston, S.C. NIH Stroke Scale reliability in ratings from a large sample of clinicians. Cerebrovasc. Dis. 2006, 22, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Eskioglou, E.; Huchmandzadeh Millotte, M.; Amiguet, M.; Michel, P. National Institutes of Health Stroke Scale Zero Strokes. Stroke 2018, 49, 3057–3059. [Google Scholar] [CrossRef] [PubMed]
- Makharia, A.; Agarwal, A.; Garg, D.; Vishnu, V.Y.; Srivastava, M.V.P. The Pitfalls of NIHSS: Time for a New Clinical Acute Stroke Severity Scoring System in the Emergency? Ann. Indian Acad. Neurol. 2024, 27, 15–18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- André, C. The NIH Stroke Scale is unreliable in untrained hands. J. Stroke Cerebrovasc. Dis. 2002, 11, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Marsh, E.B.; Lawrence, E.; Gottesman, R.F.; Llinas, R.H. The NIH Stroke Scale Has Limited Utility in Accurate Daily Monitoring of Neurologic Status. Neurohospitalist 2016, 6, 97–101. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chye, A.; Hackett, M.L.; Hankey, G.J.; Lundström, E.; Almeida, O.P.; Gommans, J.; Dennis, M.; Jan, S.; Mead, G.E.; Ford, A.H.; et al. Repeated Measures of Modified Rankin Scale Scores to Assess Functional Recovery from Stroke: AFFINITY Study Findings. J. Am. Heart Assoc. 2022, 11, e025425. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- ElHabr, A.K.; Katz, J.M.; Wang, J.; Bastani, M.; Martinez, G.; Gribko, M.; Hughes, D.R.; Sanelli, P. Predicting 90-day modified Rankin Scale score with discharge information in acute ischaemic stroke patients following treatment. BMJ Neurol. Open 2021, 3, e000177. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jette, D.U.; Stilphen, M.; Ranganathan, V.K.; Passek, S.D.; Frost, F.S.; Jette, A.M. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys. Ther. 2014, 94, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Jette, D.U.; Stilphen, M.; Ranganathan, V.K.; Passek, S.; Frost, F.S.; Jette, A.M. Interrater Reliability of AM-PAC “6-Clicks” Basic Mobility and Daily Activity Short Forms. Phys. Ther. 2015, 95, 758–766. [Google Scholar] [CrossRef] [PubMed]
- Jette, D.U.; Stilphen, M.; Ranganathan, V.K.; Passek, S.D.; Frost, F.S.; Jette, A.M. AM-PAC “6-Clicks” functional assessment scores predict acute care hospital discharge destination. Phys. Ther. 2014, 94, 1252–1261. [Google Scholar] [CrossRef] [PubMed]
- Warren, M.; Knecht, J.; Verheijde, J.; Tompkins, J. Association of AM-PAC “6-Clicks” Basic Mobility and Daily Activity Scores with Discharge Destination. Phys. Ther. 2021, 101, pzab043. [Google Scholar] [CrossRef] [PubMed]
- Blackwood, J.; Fernandez, N. AM-PAC 6-Clicks Scores Predict Hospital Discharge Destination in Older Adults with Cardiovascular Disease. Innov. Aging 2018, 2, 489. [Google Scholar] [CrossRef] [PubMed Central]
- Whitlock, K.C.; Mandala, M.; Bishop, K.L.; Moll, V.; Sharp, J.J.; Krishnan, S. Lower AM-PAC 6-Clicks Basic Mobility Score Predicts Discharge to a Postacute Care Facility Among Patients in Cardiac Intensive Care Units. Phys. Ther. 2022, 102, pzab252. [Google Scholar] [CrossRef] [PubMed]
- Hadad, M.J.; Orr, M.N.; Emara, A.K.; Klika, A.K.; Johnson, J.K.; Piuzzi, N.S. PLAN and AM-PAC “6-Clicks” Scores to Predict Discharge Disposition After Primary Total Hip and Knee Arthroplasty. J. Bone Jt. Surg. Am. 2022, 104, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Tuohy, S.; Schwartz-Dillard, J.; McInerney, D.; Nguyen, J.; Edwards, D. RAPT and AM-PAC “6-Clicks”: Do They Correlate on Predicting Discharge Destination After Total Joint Arthroplasty? HSS J. 2024, 20, 29–34. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tracy, B.M.; Victor, M.; Smith, R.N.; Hinrichs, M.J.; Gelbard, R.B. Examining the accuracy of the AM-PAC “6-clicks” at predicting discharge disposition in traumatic brain injury. Brain Inj. 2022, 36, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Mo, K.C.; Schmerler, J.; Olson, J.; Musharbash, F.N.; Kebaish, K.M.; Skolasky, R.L.; Neuman, B.J. AM-PAC mobility scores predict non-home discharge following adult spinal deformity surgery. Spine J. 2022, 22, 1884–1892. [Google Scholar] [CrossRef] [PubMed]
- Arnold, S.M.; Naessens, J.M.; McVeigh, K.; White, L.J.; Atchison, J.W.; Tompkins, J. Can AM-PAC “6-Clicks” Inpatient Functional Assessment Scores Strengthen Hospital 30-Day Readmission Prevention Strategies? Cureus 2021, 13, e14994. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hendrix, P.; Sofoluke, N.; Adams, M.D.; Kunaprayoon, S.; Zand, R.; Kolinovsky, A.N.; Person, T.N.; Gupta, M.; Goren, O.; Schirmer, C.M.; et al. Risk Factors for Acute Ischemic Stroke Caused by Anterior Large Vessel Occlusion. Stroke 2019, 50, 1074–1080. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yedavalli, V.; Koneru, M.; Hoseinyazdi, M.; Copeland, K.; Xu, R.; Luna, L.; Caplan, J.; Dmytriw, A.; Guenego, A.; Heit, J.; et al. Excellent Recanalization and Small Core Volumes Are Associated with Favorable AM-PAC Score in Patients With Acute Ischemic Stroke Secondary to Large Vessel Occlusion. Arch. Rehabil. Res. Clin. Transl. 2023, 5, 100306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fonarow, G.C.; Reeves, M.J.; Zhao, X.; Olson, D.M.; Smith, E.E.; Saver, J.L.; Schwamm, L.H. Get with the Guidelines-Stroke Steering Committee and Investigators. Age-related differences in characteristics, performance measures, treatment trends, and outcomes in patients with ischemic stroke. Circulation 2010, 121, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Freburger, J.K.; Li, D.; Fraher, E.P. Community Use of Physical and Occupational Therapy After Stroke and Risk of Hospital Readmission. Arch. Phys. Med. Rehabil. 2018, 99, 26–34.e5. [Google Scholar] [CrossRef] [PubMed]
- Merchant, J.; Kitsos, G.; Ashby, S.; Kitsos, A.; Hubbard, I.J. Occupational Therapy and Physiotherapy in Acute Stroke: Do Rural Patients Receive Less Therapy? Stroke Res. Treat. 2016, 2016, 1582706. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Freburger, J.K.; Li, D.; Johnson, A.M.; Fraher, E.P. Physical and Occupational Therapy from the Acute to Community Setting After Stroke: Predictors of Use, Continuity of Care, and Timeliness of Care. Arch. Phys. Med. Rehabil. 2018, 99, 1077–1089.e7. [Google Scholar] [CrossRef] [PubMed]
- Soto-Cámara, R.; González-Santos, J.; González-Bernal, J.; Martín-Santidrian, A.; Cubo, E.; Trejo-Gabriel-Galán, J.M. Factors Associated with Shortening of Prehospital Delay among Patients with Acute Ischemic Stroke. J. Clin. Med. 2019, 8, 1712. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| All Patients (n = 282) | |
|---|---|
| Age | 66.4 ± 16.5 |
| Sex | 113 Male (40.1%) |
| 169 Female (59.9%) | |
| Race | 120 Black (42.6%) |
| 141 White (50.0%) | |
| 21 Other (7.4%) | |
| Basic Mobility Score | |||
|---|---|---|---|
| Variable | Favorable (n = 155) | Unfavorable (n = 127) | p-Value |
| Age | 62.7 ± 15.9 | 71.0 ± 16.1 | <0.001 *** |
| Sex | 59 Male (38.1%) 96 Female 61.9%) | 54 Male (42.5) 73 Female (57.5%) | 0.447 |
| Race | 63 Black (40.6%) 76 White (49.0%) 16 Other (10.3%) | 57 Black (44.9%) 65 White (51.2%) 5 Other (3.9%) | 0.124 |
| Daily Activity Score | |||
|---|---|---|---|
| Variable | Favorable (n = 113) | Unfavorable (n = 169) | p-Value |
| Age | 60.8 ± 16.2 | 70.2 ± 15.7 | <0.001 *** |
| Sex | 38 Male (33.6%) 75 Female (66.4%) | 75 Male (44.4%) 94 Female (55.6%) | 0.070 |
| Race | 46 Black (40.7%) 58 White (51.3%) 9 Other (9.0%) | 74 Black (43.8%) 83 White (49.1%) 12 Other (7.1%) | 0.867 |
| Both Favorable | |||
|---|---|---|---|
| Variable | Both (n = 109) | All Others (n = 173) | p-Value |
| Age | 60.4 ± 16.2 | 70.2 ± 15.6 | <0.001 *** |
| Sex | 37 Male (33.9%) 72 Female (66.1%) | 76 Male (43.9%) 97 Female (56.1%) | 0.095 |
| Race | 45 Black (41.3%) 55 White (50.5%) 9 Other (8.3%) | 75 Black (43.4%) 86 White (49.7%) 12 (6.9%) | 0.891 |
| Neither Favorable | |||
|---|---|---|---|
| Variable | Neither (n = 123) | All Others (n = 159) | p-Value |
| Age | 71.0 ± 16.3 | 62.9 ± 15.9 | <0.001 *** |
| Sex | 53 Male (43.1%) 70 Female (56.9%) | 60 Male (37.7%) 99 Female (62.3%) | 0.363 |
| Race | 56 Black (45.5%) 62 White (50.4%) 5 Other (4.1%) | 64 Black (40.3%) 79 White (49.7%) 16 Other (10.1%) | 0.149 |
| Cross-Group (Pairwise Comparisons) | |||||
|---|---|---|---|---|---|
| Variable | Favorable Basic Mobility (n = 155) | Favorable Daily Activity (n = 113) | Both Favorable (n = 109) | p-Value | |
| Age | 62.7 ± 15.9 | 60.8 ± 16.2 | 60.4 ± 16.2 | Both vs. basic mobility: | 0.252 |
| Both vs. daily activity: | 0.854 | ||||
| Sex | 59 Male (38.1%) 96 Female (61.9%) | 38 Male (33.6%) 75 Female (66.4%) | 37 Male (33.9%) 72 Female (66.1%) | Both vs. basic mobility: | 0.490 |
| Both vs. daily activity: | 0.960 | ||||
| Race | 63 Black (40.6%) 76 White (49.0%) 16 Other (10.3%) | 46 Black (40.7%) 58 White (51.3%) 9 Other (9.0%) | 45 Black (41.3%) 55 White (50.5%) 9 Other (8.3%) | Both vs. basic mobility: | 0.852 |
| Both vs. daily activity: | 0.991 | ||||
| p-Value | Modified Rankin Scale | |||||||
|---|---|---|---|---|---|---|---|---|
| p < 0.001 *** | 0 | 1 | 2 | 3 | 4 | 5 | 6 | |
| Basic Mobility | Favorable (n = 155) | 46 (29.7%) | 50 (32.3%) | 32 (20.6%) | 15 (9.7%) | 7 (4.5%) | 1 (0.6%) | 4 (2.6%) |
| Unfavorable (n = 127) | 1 (0.8%) | 7 (5.5%) | 12 (9.4%) | 12 (9.4%) | 38 (29.9% | 11 (8.7%) | 46 (36.2%) | |
| p-Value | Modified Rankin Scale | |||||||
|---|---|---|---|---|---|---|---|---|
| p < 0.001 *** | 0 | 1 | 2 | 3 | 4 | 5 | 6 | |
| Daily Activity | Favorable (n = 113) | 40 (35.4%) | 40 (35.4%) | 23 (20.4%) | 4 (3.5%) | 3 (2.7%) | 0 (0%) | 3 (2.7%) |
| Unfavorable (n = 169) | 7 (4.1%) | 17 (10.1%) | 21 (12.4%) | 23 (13.6%) | 42 (24.9%) | 12 (7.1%) | 47 (27.8%) | |
| p-Value | Modified Rankin Scale | ||||||
|---|---|---|---|---|---|---|---|
| p < 0.001 *** | 0 | 1 | 2 | 3 | 4 | 5 | 6 |
| Both Favorable (n = 109) | 40 (36.7%) | 39 (35.8%) | 21 (19.3%) | 4 (3.7%) | 3 (2.8%) | 0 (0%) | 2 (1.8%) |
| Exactly One Favorable (n = 50) | 6 (12%) | 12 (24%) | 13 (26%) | 11 (22%) | 4 (8%) | 1 (2%) | 3 (6%) |
| Neither Favorable (n = 123) | 1 (0.8%) | 6 (4.9%) | 10 (8.1%) | 12 (9.8%) | 38 (30.9%) | 11 (8.9%) | 45 (36.6%) |
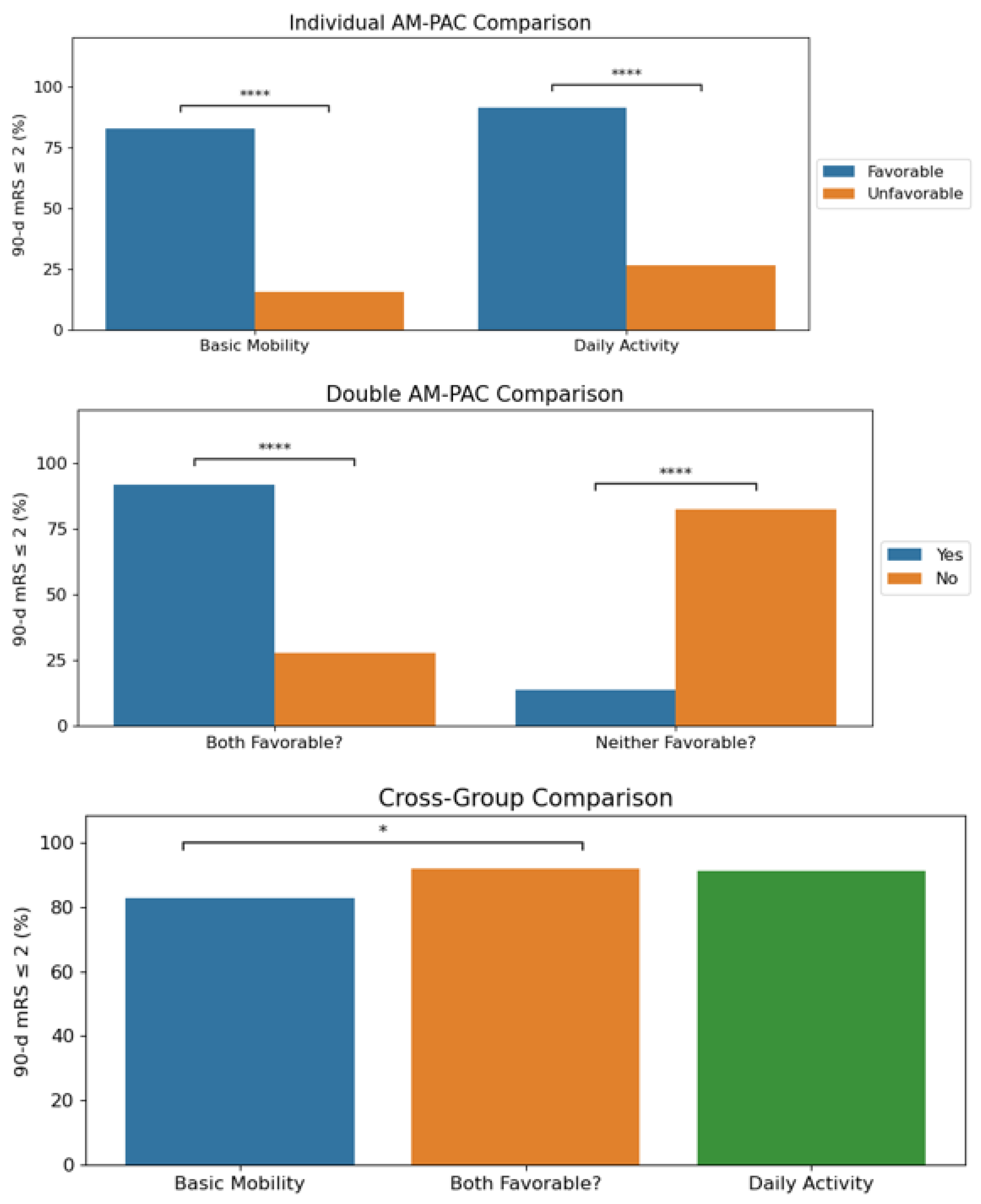
| AM-PAC Group | 90-Day Modified Rankin Scale ≤ 2 (%) | p-Values |
|---|---|---|
| Favorable basic mobility | 128/155 (82.6%) | <0.001 **** |
| Unfavorable basic mobility | 20/127 (15.7%) | |
| Favorable daily activity | 103/113 (91.2%) | <0.001 **** |
| Unfavorable daily activity | 45/169 (26.6%) | |
| Both favorable | 100/109 (91.7%) | <0.001 **** |
| At least one unfavorable | 48/173 (27.7%) | |
| Neither favorable | 17/123 (13.8%) | <0.001 **** |
| At least one favorable | 131/159 (82.4%) |
| AM-PAC Group | 90-Day Modified Rankin Scale ≤ 2 | p-Values | |
|---|---|---|---|
| Favorable basic mobility | 128/155 (82.6%) | 0.032 * | |
| Both favorable | 100/109 (91.7%) | 0.873 | |
| Favorable daily activity | 103/113 (91.2%) | ||
| AM-PAC Group | Odds Ratios (95% CI) | p-Value |
|---|---|---|
| Favorable basic mobility | 22.96 (12.07–43.68) | <0.001 *** |
| Age | 0.97 (0.95–0.99) | 0.005 ** |
| Favorable daily activity | 24.75 (11.81–51.88) | <0.001 *** |
| Age | 0.98 (0.96–0.99) | 0.012 * |
| Both favorable | 25.02 (11.63–53.81) | <0.001 *** |
| Age | 0.98 (0.96–1.00) | 0.016 * |
| Neither favorable | 0.04 (0.02–0.07) | <0.001 *** |
| Age | 0.97 (0.96–0.99) | 0.004 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, A.; Lakhani, D.A.; Balar, A.B.; Salim, H.; Koneru, M.; Hillis, A.; Gonzalez Fernández, M.; Vagal, V.; Urrutia, V.; Faizy, T.D.; et al. AM-PAC 6-Clicks Basic Mobility and Daily Activities Scores Predict 90-Day Modified Rankin Score in Patients with Acute Ischemic Stroke Secondary to Large Vessel Occlusion. J. Clin. Med. 2024, 13, 7119. https://doi.org/10.3390/jcm13237119
Cho A, Lakhani DA, Balar AB, Salim H, Koneru M, Hillis A, Gonzalez Fernández M, Vagal V, Urrutia V, Faizy TD, et al. AM-PAC 6-Clicks Basic Mobility and Daily Activities Scores Predict 90-Day Modified Rankin Score in Patients with Acute Ischemic Stroke Secondary to Large Vessel Occlusion. Journal of Clinical Medicine. 2024; 13(23):7119. https://doi.org/10.3390/jcm13237119
Chicago/Turabian StyleCho, Andrew, Dhairya A. Lakhani, Aneri B. Balar, Hamza Salim, Manisha Koneru, Argye Hillis, Marlis Gonzalez Fernández, Vaibhav Vagal, Victor Urrutia, Tobias D. Faizy, and et al. 2024. "AM-PAC 6-Clicks Basic Mobility and Daily Activities Scores Predict 90-Day Modified Rankin Score in Patients with Acute Ischemic Stroke Secondary to Large Vessel Occlusion" Journal of Clinical Medicine 13, no. 23: 7119. https://doi.org/10.3390/jcm13237119
APA StyleCho, A., Lakhani, D. A., Balar, A. B., Salim, H., Koneru, M., Hillis, A., Gonzalez Fernández, M., Vagal, V., Urrutia, V., Faizy, T. D., Heit, J. J., Albers, G. W., Mazumdar, I., Chen, K., Sepehri, S., Kim, M., Luna, L., Mei, J., Yedavalli, V. S., & Hyson, N. (2024). AM-PAC 6-Clicks Basic Mobility and Daily Activities Scores Predict 90-Day Modified Rankin Score in Patients with Acute Ischemic Stroke Secondary to Large Vessel Occlusion. Journal of Clinical Medicine, 13(23), 7119. https://doi.org/10.3390/jcm13237119






