Multiple Subpial Transection for the Treatment of Landau–Kleffner Syndrome—Review of the Literature
Abstract
1. Introduction
2. Review Methods
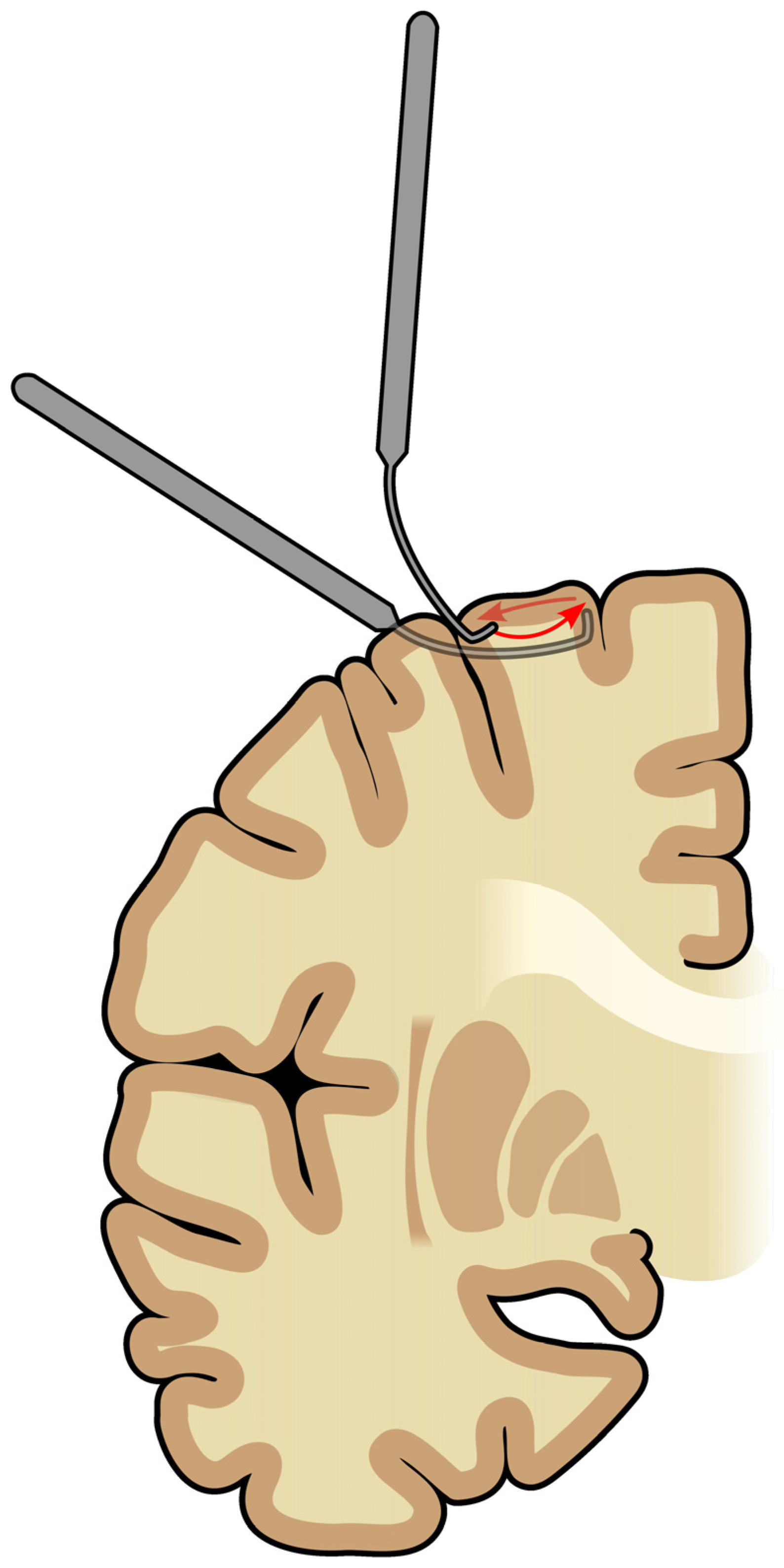
3. Overview of Treatment Options for LKS
4. Qualification for the MST Procedure
5. Magnetoencephalography
6. Seizure Outcomes
7. Language Outcomes
8. Behavior Outcomes
9. EEG Outcomes
10. Cognitive Outcomes
11. Complications
12. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| AEDs | Antiepileptic drugs |
| AER | Autistic epileptiform regression |
| BDNF | Brain-derived neurotrophic factor |
| CSWS | Continuous spikes in slow wave sleep |
| DEE-SWAS | Developmental epileptic encephalopathy with spike-and-wave activation in sleep |
| ECoG | Electrocorticography |
| EE-SWAS | Epileptic encephalopathy with spike-and-wave activation in sleep |
| EOWPVT-R | Expressive One Word Picture Vocabulary Test-revised |
| ESES | Electrical status epilepticus during sleep |
| GRIN2A | Glutamate Ionotropic Receptor NMDA Type Subunit 2A |
| ILAE | International League Against Epilepsy |
| IQ | Intelligence quotient |
| LKS | Landau–Kleffner syndrome |
| MEG | Magnetoencephalography |
| MHXT | Methohexital suppression test |
| MST | Multiple subpial transection |
| N/A | Not available |
| NMDA | N-methyl-D-aspartate receptor |
| N-REM | Non-rapid eye movement sleep |
| PPVT-R | Peabody Picture Vocabulary Test-revised |
| SWAS | Spike-and-wave activation in sleep |
| WHO | World Health Organization |
References
- Epilepsy. Available online: https://www.who.int/en/news-room/fact-sheets/detail/epilepsy (accessed on 5 August 2023).
- Specchio, N.; Wirrell, E.C.; Scheffer, I.E.; Nabbout, R.; Riney, K.; Samia, P.; Guerreiro, M.; Gwer, S.; Zuberi, S.M.; Wilmshurst, J.M.; et al. International League Against Epilepsy Classification and Definition of Epilepsy Syndromes with Onset in Childhood: Position Paper by the ILAE Task Force on Nosology and Definitions. Epilepsia 2022, 63, 1398–1442. [Google Scholar] [CrossRef] [PubMed]
- Landau, W.M.; Kleffner, F.R. Syndrome of Acquired Aphasia with Convulsive Disorder in Children. Neurology 1957, 7, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Landau–Kleffner Syndrome. StatPearls, NCBI Bookshelf. Available online: https://www.ncbi.nlm.nih.gov/books/NBK547745/ (accessed on 5 August 2023).
- Epilepsy Syndromes in Children—UpToDate. Available online: https://www.uptodate.com/contents/epilepsy-syndromes-in-children?search=surgeryinepilepsy&topicRef=101361&source=related_link (accessed on 17 April 2023).
- Meador, K.J.; Loring, D.W.; Flanigin, H.F. History of Epilepsy Surgery. J. Epilepsy 1989, 2, 21–25. [Google Scholar] [CrossRef]
- Bermeo-Ovalle, A.; Smith, M.C. Multiple Subpial Transection; John Wiley & Sons, Ltd.: Oxford, UK, 2016. [Google Scholar]
- Morrell, F.; Whisler, W.W.; Bleck, T.P. Multiple Subpial Transection: A New Approach to the Surgical Treatment of Focal Epilepsy. J. Neurosurg. 1989, 70, 231–239. [Google Scholar] [CrossRef]
- Buelow, J.M.; Aydelott, P.; Pierz, D.M.; Heck, B. Multiple Subpial Transection for Landau–Kleffner Syndrome. AORN J. 1996, 63, 725–739. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 134, 178–189. [Google Scholar] [CrossRef]
- Kotagal, P. Current Status of Treatments for Children with Electrical Status in Slow-Wave Sleep (ESES/CSWS). Epilepsy Curr. 2017, 17, 214–216. [Google Scholar] [CrossRef]
- Shbarou, R. Current Treatment Options for Early-Onset Pediatric Epileptic Encephalopathies. Curr. Treat. Options Neurol. 2016, 18, 44. [Google Scholar] [CrossRef]
- Nariai, H.; Duberstein, S.; Shinnar, S. Treatment of Epileptic Encephalopathies: Current State of the Art. J. Child Neurol. 2018, 33, 41–54. [Google Scholar] [CrossRef]
- Van Den Munckhof, B.; Van Dee, V.; Sagi, L.; Caraballo, R.H.; Veggiotti, P.; Liukkonen, E.; Loddenkemper, T.; Sánchez Fernández, I.; Buzatu, M.; Bulteau, C.; et al. Treatment of Electrical Status Epilepticus in Sleep: A Pooled Analysis of 575 Cases. Epilepsia 2015, 56, 1738–1746. [Google Scholar] [CrossRef]
- Sinclair, D.B.; Snyder, T.J. Corticosteroids for the Treatment of Landau–Kleffner Syndrome and Continuous Spike-Wave Discharge during Sleep. Pediatr. Neurol. 2005, 32, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Becker, L.L.; Kaindl, A.M. Corticosteroids in Childhood Epilepsies: A Systematic Review. Front. Neurol. 2023, 14, 1142253. [Google Scholar] [CrossRef] [PubMed]
- Fainberg, N.; Harper, A.; Tchapyjnikov, D.; Mikati, M.A. Response to Immunotherapy in a Patient with Landau–Kleffner Syndrome and GRIN2A Mutation. Epileptic Disord. 2016, 18, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Moresco, L.; Bruschettini, M.; Calevo, M.G.; Siri, L. Pharmacological Treatment for Continuous Spike-Wave during Slow Wave Sleep Syndrome and Landau–Kleffner Syndrome (Review). Cochrane Database Syst. Rev. 2020, 11, CD013132. [Google Scholar] [CrossRef]
- Sánchez Fernández, I.; Chapman, K.; Peters, J.M.; Klehm, J.; Jackson, M.C.; Berg, A.T.; Loddenkemper, T. Treatment for Continuous Spikes and Waves during Sleep (CSWS): Survey on Treatment Choices in North America. Epilepsia 2014, 55, 1099–1108. [Google Scholar] [CrossRef]
- Cross, J.H.; Neville, B.G.R. The Surgical Treatment of Landau–Kleffner Syndrome. Epilepsia 2009, 50, 63–67. [Google Scholar] [CrossRef]
- Castillo, E.M.; Butler, I.J.; Baumgartner, J.E.; Passaro, A.; Papanicolaou, A.C. When Epilepsy Interferes With Word Comprehension: Findings in Landau–Kleffner Syndrome. J. Child Neurol. 2008, 23, 97–101. [Google Scholar] [CrossRef]
- Morrell, F. Varieties of Human Secondary Epileptogenesis. J. Clin. Neurophysiol. 1989, 6, 227–275. [Google Scholar] [CrossRef]
- Morrell, F.; Whisler, W.W.; Smith, M.C.; Hoeppner, T.J.; de Toledo-morrell, L.; Pierre-louis, S.J.C.; Kanner, A.M.; Buclow, J.M.; Ristanovic, R.; Bergen, D.; et al. Landau–Kleffner Syndrome. Treatment with Subpial Intracortical Transection. Brain 1995, 118 Pt 6, 1529–1546. [Google Scholar] [CrossRef]
- Paetau, R. Magnetoencephalography in Landau–Kleffner Syndrome. Epilepsia 2009, 50, 51–54. [Google Scholar] [CrossRef]
- Irwin, K.; Birch, V.; Lees, J.; Polkey, C.; Alarcon, G.; Binnie, C.; Smedley, M.; Baird, G.; Robinson, R.O. Multiple Subpial Transection in Landau–Kleffner Syndrome. Dev. Med. Child Neurol. 2001, 43, 248–252. [Google Scholar] [PubMed]
- Sawhney, I.M.S.; Robertson, I.J.; Polkey, C.E.; Binnie, C.D.; Elwes, R.D.C. Multiple Subpial Transection: A Review of 21 Cases. J. Neurol. Neurosurg. Psychiatry 1995, 58, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Neville, B.G.R.; Harkness, W.F.J.; Cross, J.H.; Cass, H.C.; Burch, V.C.; Lees, J.A.; Taylor, D.C. Surgical Treatment of Severe Autistic Regression in Childhood Epilepsy. Pediatr. Neurol. 1997, 16, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Nass, R.; Gross, A.; Wisoff, J.; Devinsky, O. Outcome of Multiple Subpial Transections for Autistic Epileptiform Regression. Pediatr. Neurol. 1999, 21, 464–470. [Google Scholar] [CrossRef]
- Grote, C.L.; Van Slyke, P.; Hoeppner, J.A.B. Language Outcome Following Multiple Subpial Transection for Landau–Kleffner Syndrome. Brain 1999, 122 Pt 3, 561–566. [Google Scholar] [CrossRef]
- Downes, M.; Greenaway, R.; Clark, M.; Helen Cross, J.; Jolleff, N.; Harkness, W.; Kaliakatsos, M.; Boyd, S.; White, S.; Neville, B.G.R. Outcome Following Multiple Subpial Transection in Landau–Kleffner Syndrome and Related Regression. Epilepsia 2015, 56, 1760–1766. [Google Scholar] [CrossRef]
- Kheder, A.; Wongwiangjunt, S.; Kotagal, P. Comment on Outcome Following Multiple Subpial Transection in Landau–Kleffner Syndrome and Related Regression. Epilepsia 2016, 57, 674. [Google Scholar] [CrossRef]
- Downes, M.; Greenaway, R.; Clark, M.; Cross, J.H.; Jolleff, N.; Harkness, W.; Kaliakatsos, M.; Boyd, S.; White, S.; Neville, B.G.R. In Response: Comment on Outcome Following Multiple Subpial Transection in Landau–Kleffner Syndrome and Related Regression. Epilepsia 2016, 57, 674–675. [Google Scholar] [CrossRef]

| Number of LKS Patients | Time of Assessment | Engel Class I | Engel Class II | Engel Class III | Engel Class IV | Seizure Improvement, Not Specified | Surgical Procedures, % of Patients | Additional Information | Authors |
|---|---|---|---|---|---|---|---|---|---|
| 10 | N/A | N/A | N/A | N/A | N/A | 50% | MST, not detailed | - | Cross [20] |
| 12 | 13–78 months | 75% * | N/A | N/A | N/A | - | MHXT (100% *); MST of Wernicke (100% *) and Broca (N/A) area; Temporal lobectomy (16.7% *) | Two additional patients had no evidence of seizures (not included). Seizure-relapse patients (25%) achieved no benefit in the language domain. | Morrell [23] |
| 5 | Post-surgery | 60% | 40% * | 0% * | 0% * | - | Carotid amytal and thiopentone suppression tests (N/A) MST, usually of superior and middle temporal gyri | - | Irwin [25] |
| 5 | At the latest available follow-up | 100% | 0% | 0% | 0% | - | After seizure relapse, one of the patients was reoperated on and regained Engel I class. | ||
| 3 | N/A | 66.7% * | N/A | N/A | N/A | - | Carotid amytal test; extensive MST ** of precentral gyrus, sylvian area, and posterior temporal and parietal lobes (33.3% *). MST ** (66.7% *) | - | Sawhney [26] |
| 1 | 6 months | 100% * | 0% | 0% | 0% | - | MST, not detailed | - | Neville [27] |
| Number of LKS Patients | Time of Assessment | Language Function Improvement, % | Regaining Normal Language Function, % | Surgical Procedures, % of Patients | Additional Information | Authors |
|---|---|---|---|---|---|---|
| 10 | N/A | 70% | 0% | MST, not detailed | - | Cross [20] |
| 14 | 13–78 months | 79% | 50% | MHXT (92.9% *); MST of Wernicke (100% *) and Broca (N/A) area; temporal lobectomy (14.3% *) | - | Morrell [23] |
| 5 | Post-surgery | 100% | 0% | Carotid amytal and thiopentone suppression tests (N/A); MST ***, usually of superior and middle temporal gyri | - | Irwin [25] |
| 5 | At the last available follow-up | 100% | 0% | |||
| 3 | N/A | 100% | N/A | Carotid amytal and thiopentone test; extensive MST ** of precentral gyrus, sylvian area, and posterior temporal and parietal lobes (33.3% *); MST ** (66.7% *) | - | Sawhney [26] |
| 1 | - | 100% | - | MST, not detailed | - | Neville [27] |
| 13 | 0.6–6.6 years | 53.85% * a | N/A | MHXT (N/A); MST: fronto-temporo-parietal (61.5% *), fronto-temporal (15.4% *); temporo-parietal (15.4% *), and temporal (7.7% *) | We excluded one patient from calculations due to lacking post-operative PPVT-R measure | Grote [29] |
| 14 | 0.5–6.6 years | 57.14% * b | N/A | MHXT (N/A); MST: fronto-temporo-parietal (57.1% *), fronto-temporal (14.3% *); temporo-parietal (21.4% *), and temporal (7.1% *) | - | |
| 13 | - | 23.08% * | 7.7% * | MHXT (N/A) and/or MEG (N/A); MST **, posterior temporal region | - | Downes [30] |
| Number of LKS Patients | Time of Assessment | Behavioral Improvement | Surgical Procedures, % of Patients | Authors |
|---|---|---|---|---|
| 10 | N/A | 10% | MST, not detailed | Cross [20] |
| 5 | Post-surgery | 100% | Carotid amytal and thiopentone suppression tests (N/A); MST *, usually of superior and middle temporal gyri | Irwin [25] |
| 5 | At the last available follow-up | 100% | ||
| 1 | 6 months | 100% | MST, not detailed | Neville [27] |
| Number of LKS Patients | Normal EEG Activity | Surgical Procedures %, of Patients | Additional Information | Authors |
|---|---|---|---|---|
| 10 | 30% | MST, not detailed | - | Cross [20] |
| 14 | 64% | MHXT (92.9% *); MST of Wernicke (100% *) and Broca (N/A) area; temporal lobectomy (14.3% *) | 3 of 5 patients with recurrent EEG abnormalities presented a recurrence of clinical seizures | Morrell [23] |
| 5 | 100% | Carotid amytal (N/A) and thiopentone suppression tests (N/A). MST *, usually of superior and middle temporal gyri | - | Irwin [25] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duda, P.; Duda, N.; Kostelecka, K.; Woliński, F.; Góra, J.; Granat, M.; Bryliński, Ł.; Teresińska, B.; Karpiński, R.; Czyżewski, W.; et al. Multiple Subpial Transection for the Treatment of Landau–Kleffner Syndrome—Review of the Literature. J. Clin. Med. 2024, 13, 7580. https://doi.org/10.3390/jcm13247580
Duda P, Duda N, Kostelecka K, Woliński F, Góra J, Granat M, Bryliński Ł, Teresińska B, Karpiński R, Czyżewski W, et al. Multiple Subpial Transection for the Treatment of Landau–Kleffner Syndrome—Review of the Literature. Journal of Clinical Medicine. 2024; 13(24):7580. https://doi.org/10.3390/jcm13247580
Chicago/Turabian StyleDuda, Piotr, Natalia Duda, Katarzyna Kostelecka, Filip Woliński, Joanna Góra, Michał Granat, Łukasz Bryliński, Barbara Teresińska, Robert Karpiński, Wojciech Czyżewski, and et al. 2024. "Multiple Subpial Transection for the Treatment of Landau–Kleffner Syndrome—Review of the Literature" Journal of Clinical Medicine 13, no. 24: 7580. https://doi.org/10.3390/jcm13247580
APA StyleDuda, P., Duda, N., Kostelecka, K., Woliński, F., Góra, J., Granat, M., Bryliński, Ł., Teresińska, B., Karpiński, R., Czyżewski, W., & Baj, J. (2024). Multiple Subpial Transection for the Treatment of Landau–Kleffner Syndrome—Review of the Literature. Journal of Clinical Medicine, 13(24), 7580. https://doi.org/10.3390/jcm13247580








