A High Respiratory Drive Is Associated with Weaning Failure in Patients with COVID-19-Associated Acute Respiratory Distress Syndrome: The Role of the Electrical Activity of the Diaphragm
Abstract
:1. Introduction
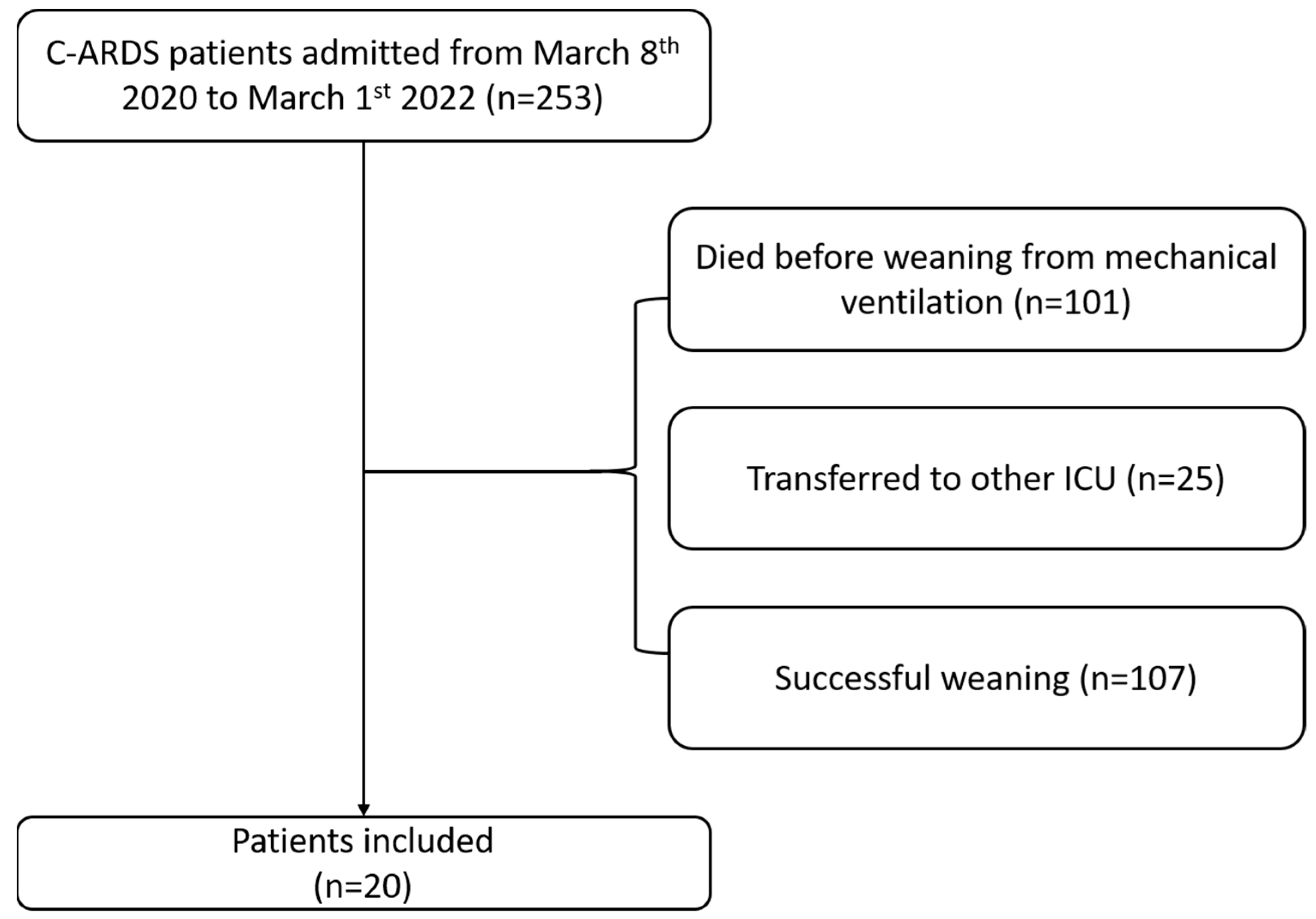
2. Materials and Methods
Statistical Analysis
- pweaning: group effect, to compare the two cohorts.
- pday: time effect, to compare the trend over the days.
- pweaning#day: combined effect, showing the interaction of the group effect with the time effect.
3. Results
4. Discussion
4.1. Comparison of the Findings with Other Studies
4.2. Respiratory Drive and ARDS
4.3. Monitoring of Respiratory Drive during the Weaning Phase
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–2021. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef]
- Matthay, M.A.; Zemans, R.L.; Zimmerman, G.A.; Arabi, Y.M.; Beitler, J.R.; Mercat, A.; Herridge, M.; Randolph, A.G.; Calfee, C.S. Acute respiratory distress syndrome. Nat. Rev. Dis. Primers 2019, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Whittle, J.S.; Pavlov, I.; Sacchetti, A.D.; Atwood, C.; Rosenberg, M.S. Respiratory support for adult patients with COVID-19. J. Am. Coll. Emerg. Physicians Open 2020, 1, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Navas-Blanco, J.R.; Dudaryk, R. Management of Respiratory Distress Syndrome due to COVID-19 infection. BMC Anesthesiol. 2020, 20, 177. [Google Scholar] [CrossRef]
- Silva, P.L.; Ball, L.; Rocco, P.R.M.; Pelosi, P. Power to mechanical power to minimize ventilator-induced lung injury? Intensive Care Med. Exp. 2019, 7, 38. [Google Scholar] [CrossRef]
- Heyland, D.K.; Cook, D.J.; Griffith, L.; Keenan, S.P.; Brun-Buisson, C. The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. The Canadian Critical Trials Group. Am. J. Respir. Crit. Care Med. 1999, 159, 1249–1256. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, E.H.; Tracy, L.; Hill, C.; Fraser, V.J.; Kollef, M.H. The occurrence of ventilator-associated pneumonia in a community hospital: Risk factors and clinical outcomes. Chest 2001, 120, 555–561. [Google Scholar] [CrossRef]
- Beitler, J.R.; Malhotra, A.; Thompson, B.T. Ventilator-induced Lung Injury. Clin. Chest Med. 2016, 37, 633–646. [Google Scholar] [CrossRef] [PubMed]
- Boles, J.M.; Bion, J.; Connors, A.; Herridge, M.; Marsh, B.; Melot, C.; Pearl, R.; Silverman, H.; Stanchina, M.; Vieillard-Baron, A.; et al. Weaning from mechanical ventilation. Eur. Respir. J. 2007, 29, 1033–1056. [Google Scholar] [CrossRef]
- Beduneau, G.; Pham, T.; Schortgen, F.; Piquilloud, L.; Zogheib, E.; Jonas, M.; Grelon, F.; Runge, I.; Nicolas, T.; Grange, S.; et al. Epidemiology of Weaning Outcome according to a New Definition. The WIND Study. Am. J. Respir. Crit. Care Med. 2017, 195, 772–783. [Google Scholar] [CrossRef]
- Funk, G.C.; Anders, S.; Breyer, M.K.; Burghuber, O.C.; Edelmann, G.; Heindl, W.; Hinterholzer, G.; Kohansal, R.; Schuster, R.; Schwarzmaier-D’Assie, A.; et al. Incidence and outcome of weaning from mechanical ventilation according to new categories. Eur. Respir. J. 2010, 35, 88–94. [Google Scholar] [CrossRef]
- Bordon, J.; Akca, O.; Furmanek, S.; Cavallazzi, R.S.; Suliman, S.; Aboelnasr, A.; Sinanova, B.; Ramirez, J.A. Acute Respiratory Distress Syndrome and Time to Weaning Off the Invasive Mechanical Ventilator among Patients with COVID-19 Pneumonia. J. Clin. Med. 2021, 10, 2935. [Google Scholar] [CrossRef]
- Bertoni, M.; Spadaro, S.; Goligher, E.C. Monitoring Patient Respiratory Effort During Mechanical Ventilation: Lung and Diaphragm-Protective Ventilation. Crit. Care 2020, 24, 106. [Google Scholar] [CrossRef]
- Sinderby, C.; Navalesi, P.; Beck, J.; Skrobik, Y.; Comtois, N.; Friberg, S.; Gottfried, S.B.; Lindstrom, L. Neural control of mechanical ventilation in respiratory failure. Nat. Med. 1999, 5, 1433–1436. [Google Scholar] [CrossRef]
- Sinderby, C.A.; Beck, J.C.; Lindstrom, L.H.; Grassino, A.E. Enhancement of signal quality in esophageal recordings of diaphragm EMG. J. Appl. Physiol. 1997, 82, 1370–1377. [Google Scholar] [CrossRef]
- Umbrello, M.; Antonucci, E.; Muttini, S. Neurally Adjusted Ventilatory Assist in Acute Respiratory Failure-A Narrative Review. J. Clin. Med. 2022, 11, 1863. [Google Scholar] [CrossRef]
- Luo, Y.M.; Moxham, J.; Polkey, M.I. Diaphragm electromyography using an oesophageal catheter: Current concepts. Clin. Sci. 2008, 115, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Sinderby, C.; Beck, J.; Spahija, J.; de Marchie, M.; Lacroix, J.; Navalesi, P.; Slutsky, A.S. Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 2007, 131, 711–717. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.; Gottfried, S.B.; Navalesi, P.; Skrobik, Y.; Comtois, N.; Rossini, M.; Sinderby, C. Electrical activity of the diaphragm during pressure support ventilation in acute respiratory failure. Am. J. Respir. Crit. Care Med. 2001, 164, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Spinelli, E.; Mauri, T.; Beitler, J.R.; Pesenti, A.; Brodie, D. Respiratory drive in the acute respiratory distress syndrome: Pathophysiology, monitoring, and therapeutic interventions. Intensive Care Med. 2020, 46, 606–618. [Google Scholar] [CrossRef] [PubMed]
- Force, A.D.T.; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA 2020, 323, 1843–1844. [Google Scholar] [CrossRef]
- Foti, G.; Giannini, A.; Bottino, N.; Castelli, G.P.; Cecconi, M.; Grasselli, G.; Guatteri, L.; Latronico, N.; Langer, T.; Monti, G.; et al. Management of critically ill patients with COVID-19: Suggestions and instructions from the coordination of intensive care units of Lombardy. Minerva Anestesiol. 2020, 86, 1234–1245. [Google Scholar] [CrossRef]
- Umbrello, M.; Guglielmetti, L.; Formenti, P.; Antonucci, E.; Cereghini, S.; Filardo, C.; Montanari, G.; Muttini, S. Qualitative and quantitative muscle ultrasound changes in patients with COVID-19-related ARDS. Nutrition 2021, 91–92, 111449. [Google Scholar] [CrossRef]
- Ouellette, D.R.; Patel, S.; Girard, T.D.; Morris, P.E.; Schmidt, G.A.; Truwit, J.D.; Alhazzani, W.; Burns, S.M.; Epstein, S.K.; Esteban, A.; et al. Liberation From Mechanical Ventilation in Critically Ill Adults: An Official American College of Chest Physicians/American Thoracic Society Clinical Practice Guideline: Inspiratory Pressure Augmentation During Spontaneous Breathing Trials, Protocols Minimizing Sedation, and Noninvasive Ventilation Immediately After Extubation. Chest 2017, 151, 166–180. [Google Scholar] [CrossRef]
- Williams, E.C.; Motta-Ribeiro, G.C.; Vidal Melo, M.F. Driving Pressure and Transpulmonary Pressure: How Do We Guide Safe Mechanical Ventilation? Anesthesiology 2019, 131, 155–163. [Google Scholar] [CrossRef]
- Suarez-Sipmann, F.; Santos, A.; Bohm, S.H.; Borges, J.B.; Hedenstierna, G.; Tusman, G. Corrections of Enghoff’s dead space formula for shunt effects still overestimate Bohr’s dead space. Respir. Physiol. Neurobiol. 2013, 189, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef]
- Zhu, J.; Wei, Z.; Suryavanshi, M.; Chen, X.; Xia, Q.; Jiang, J.; Ayodele, O.; Bradbury, B.D.; Brooks, C.; Brown, C.A.; et al. Characteristics and outcomes of hospitalised adults with COVID-19 in a Global Health Research Network: A cohort study. BMJ Open 2021, 11, e051588. [Google Scholar] [CrossRef] [PubMed]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef] [PubMed]
- Tiruneh, S.A.; Tesema, Z.T.; Azanaw, M.M.; Angaw, D.A. The effect of age on the incidence of COVID-19 complications: A systematic review and meta-analysis. Syst. Rev. 2021, 10, 80. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Piernas, C.; Astbury, N.M.; Hippisley-Cox, J.; O’Rahilly, S.; Aveyard, P.; Jebb, S.A. Associations between body-mass index and COVID-19 severity in 6.9 million people in England: A prospective, community-based, cohort study. Lancet Diabetes Endocrinol. 2021, 9, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Gamberini, L.; Tonetti, T.; Spadaro, S.; Zani, G.; Mazzoli, C.A.; Capozzi, C.; Giampalma, E.; Bacchi Reggiani, M.L.; Bertellini, E.; Castelli, A.; et al. Factors influencing liberation from mechanical ventilation in coronavirus disease 2019: Multicenter observational study in fifteen Italian ICUs. J. Intensive Care 2020, 8, 80. [Google Scholar] [CrossRef] [PubMed]
- Kasugai, D.; Ozaki, M.; Nishida, K.; Hiraiwa, H.; Jingushi, N.; Numaguchi, A.; Omote, N.; Shindo, Y.; Goto, Y. Usefulness of Respiratory Mechanics and Laboratory Parameter Trends as Markers of Early Treatment Success in Mechanically Ventilated Severe Coronavirus Disease: A Single-Center Pilot Study. J. Clin. Med. 2021, 10, 2513. [Google Scholar] [CrossRef] [PubMed]
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020, 395, 1763–1770. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Vassalli, F.; Romitti, F. Benefits and risks of the P/F approach. Intensive Care Med. 2018, 44, 2245–2247. [Google Scholar] [CrossRef]
- Karbing, D.S.; Kjaergaard, S.; Smith, B.W.; Espersen, K.; Allerod, C.; Andreassen, S.; Rees, S.E. Variation in the PaO2/FiO2 ratio with FiO2: Mathematical and experimental description, and clinical relevance. Crit. Care 2007, 11, R118. [Google Scholar] [CrossRef]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef]
- Telias, I.; Brochard, L.; Goligher, E.C. Is my patient’s respiratory drive (too) high? Intensive Care Med. 2018, 44, 1936–1939. [Google Scholar] [CrossRef]
- Vaporidi, K.; Akoumianaki, E.; Telias, I.; Goligher, E.C.; Brochard, L.; Georgopoulos, D. Respiratory Drive in Critically Ill Patients. Pathophysiology and Clinical Implications. Am. J. Respir. Crit. Care Med. 2020, 201, 20–32. [Google Scholar] [CrossRef]
- Piquilloud, L.; Beloncle, F.; Richard, J.M.; Mancebo, J.; Mercat, A.; Brochard, L. Information conveyed by electrical diaphragmatic activity during unstressed, stressed and assisted spontaneous breathing: A physiological study. Ann. Intensive Care 2019, 9, 89. [Google Scholar] [CrossRef]
- Roze, H.; Lafrikh, A.; Perrier, V.; Germain, A.; Dewitte, A.; Gomez, F.; Janvier, G.; Ouattara, A. Daily titration of neurally adjusted ventilatory assist using the diaphragm electrical activity. Intensive Care Med. 2011, 37, 1087–1094. [Google Scholar] [CrossRef]
- Muttini, S.; Villani, P.G.; Trimarco, R.; Bellani, G.; Grasselli, G.; Patroniti, N. Relation between peak and integral of the diaphragm electromyographic activity at different levels of support during weaning from mechanical ventilation: A physiologic study. J. Crit. Care 2015, 30, 7–12. [Google Scholar] [CrossRef]
- Colombo, D.; Cammarota, G.; Bergamaschi, V.; De Lucia, M.; Corte, F.D.; Navalesi, P. Physiologic response to varying levels of pressure support and neurally adjusted ventilatory assist in patients with acute respiratory failure. Intensive Care Med. 2008, 34, 2010–2018. [Google Scholar] [CrossRef] [PubMed]
- Roze, H.; Germain, A.; Perrier, V.; Dewitte, A.; Joannes-Boyau, O.; Fleureau, C.; Ouattara, A. Effect of flumazenil on diaphragm electrical activation during weaning from mechanical ventilation after acute respiratory distress syndrome. Br. J. Anaesth. 2015, 114, 269–275. [Google Scholar] [CrossRef]
- Tipton, M.J.; Harper, A.; Paton, J.F.R.; Costello, J.T. The human ventilatory response to stress: Rate or depth? J. Physiol. 2017, 595, 5729–5752. [Google Scholar] [CrossRef]
- Pham, T.; Telias, I.; Piraino, T.; Yoshida, T.; Brochard, L.J. Asynchrony Consequences and Management. Crit. Care Clin. 2018, 34, 325–341. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Uchiyama, A.; Matsuura, N.; Mashimo, T.; Fujino, Y. The comparison of spontaneous breathing and muscle paralysis in two different severities of experimental lung injury. Crit. Care Med. 2013, 41, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Sklienka, P.; Frelich, M.; Bursa, F. Patient Self-Inflicted Lung Injury-A Narrative Review of Pathophysiology, Early Recognition, and Management Options. J. Pers. Med. 2023, 13, 593. [Google Scholar] [CrossRef]
- Jonkman, A.H.; de Vries, H.J.; Heunks, L.M.A. Physiology of the Respiratory Drive in ICU Patients: Implications for Diagnosis and Treatment. Crit. Care 2020, 24, 104. [Google Scholar] [CrossRef]
- Schmidt, M.; Banzett, R.B.; Raux, M.; Morelot-Panzini, C.; Dangers, L.; Similowski, T.; Demoule, A. Unrecognized suffering in the ICU: Addressing dyspnea in mechanically ventilated patients. Intensive Care Med. 2014, 40, 1–10. [Google Scholar] [CrossRef]
- Schmidt, M.; Kindler, F.; Gottfried, S.B.; Raux, M.; Hug, F.; Similowski, T.; Demoule, A. Dyspnea and surface inspiratory electromyograms in mechanically ventilated patients. Intensive Care Med. 2013, 39, 1368–1376. [Google Scholar] [CrossRef]
- Doorduin, J.; Roesthuis, L.H.; Jansen, D.; van der Hoeven, J.G.; van Hees, H.W.H.; Heunks, L.M.A. Respiratory Muscle Effort during Expiration in Successful and Failed Weaning from Mechanical Ventilation. Anesthesiology 2018, 129, 490–501. [Google Scholar] [CrossRef]
- Dres, M.; Schmidt, M.; Ferre, A.; Mayaux, J.; Similowski, T.; Demoule, A. Diaphragm electromyographic activity as a predictor of weaning failure. Intensive Care Med. 2012, 38, 2017–2025. [Google Scholar] [CrossRef]
- Liu, L.; Liu, H.; Yang, Y.; Huang, Y.; Liu, S.; Beck, J.; Slutsky, A.S.; Sinderby, C.; Qiu, H. Neuroventilatory efficiency and extubation readiness in critically ill patients. Crit. Care 2012, 16, R143. [Google Scholar] [CrossRef] [PubMed]
- Vallverdu, I.; Calaf, N.; Subirana, M.; Net, A.; Benito, S.; Mancebo, J. Clinical characteristics, respiratory functional parameters, and outcome of a two-hour T-piece trial in patients weaning from mechanical ventilation. Am. J. Respir. Crit. Care Med. 1998, 158, 1855–1862. [Google Scholar] [CrossRef] [PubMed]
- Capdevila, X.J.; Perrigault, P.F.; Perey, P.J.; Roustan, J.P.; d’Athis, F. Occlusion pressure and its ratio to maximum inspiratory pressure are useful predictors for successful extubation following T-piece weaning trial. Chest 1995, 108, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, M.; Rezoagli, E.; Bronco, A.; Rabboni, F.; Grasselli, G.; Foti, G.; Bellani, G. Accessory and Expiratory Muscles Activation During Spontaneous Breathing Trial: A Physiological Study by Surface Electromyography. Front. Med. 2022, 9, 814219. [Google Scholar] [CrossRef] [PubMed]
- Merdji, H.; Long, M.T.; Ostermann, M.; Herridge, M.; Myatra, S.N.; De Rosa, S.; Metaxa, V.; Kotfis, K.; Robba, C.; De Jong, A.; et al. Sex and gender differences in intensive care medicine. Intensive Care Med. 2023, 49, 1155–1167. [Google Scholar] [CrossRef] [PubMed]

| Whole Cohort n = 20 | Weaning Success n = 13 (65%) | Weaning Failure n = 7 (35%) | p-Value | |
|---|---|---|---|---|
| Anthropometric measures | ||||
| Male sex (n - %) | 17 (85) | 11 (84.6) | 6 (85.7) | 0.7300 |
| Actual body weight (kg) | 83 (75–93) | 82 (77.50–91) | 85 (71–95) | >0.9999 |
| Height (cm) | 170 (165–175) | 171 (162–175) | 170 (168–172) | 0.4011 |
| Predicted body weight (kg) | 54 (60–67) | 64 (58–67) | 64 (62–65) | 0.4691 |
| Body mass index (kg/m2) | 29.8 (25.3–32.8) | 29.7 (25.8–32.9) | 30.0 (24.8–32.1) | 0.9684 |
| Age (years) | 66 (60–69) | 63 (59–68) | 69 (64–74) | 0.0291 |
| Comorbidities | ||||
| Hypertension (n - %) | 7 (35) | 11 (68.80) | 18 (75) | 0.6650 |
| Diabetes (n - %) | 3 (15) | 1 (6.25) | 4 (16.70) | 0.9524 |
| COPD (n - %) | 3 (15) | 1 (7.7) | 2 (28.6) | 0.2120 |
| AACCI (points) | 3 (2–5) | 3 (2–5) | 4 (3–5) | 0.3539 |
| Severity scores | ||||
| SOFA (points) | 3 (2–4) | 3 (2–4) | 4 (2–8) | 0.2369 |
| SAPS II (points) | 28 (23–34) | 27 (18–29) | 35 (28–49) | 0.0190 |
| Biochemical parameters | ||||
| PCT (μg/L) | 0.28 (0.19–0.76) | 0.34 (0.21–0.82) | 0.27 (0.18–0.34) | 0.5782 |
| CRP (mg/dL) | 9.0 (2.8–14.6) | 9.9 (2–17.9) | 7.2 (3.7–11.8) | 0.4054 |
| Fibrinogen (mg/dL) | 640 (562–674) | 660 (579–674) | 580 (548–690) | 0.8429 |
| D-dimer (ng/mL) | 1024 (560–1666) | 591 (520–1695) | 1503 (1151–1638) | 0.1223 |
| Hb (g/dL) | 12.1 (10.9–13.4) | 12 (11–12.8) | 12.2 (10.3–13.6) | 0.9684 |
| PLTs (103/μL) | 242 (183–299) | 257 (214–331) | 187 (183–257) | 0.1776 |
| WBC (103/μL) | 9.5 (7.4–13.6) | 9.4 (6.7–13) | 10.5 (8.1–16.7) | 0.3620 |
| Creatinine (mg/dL) | 0.68 (0.53–0.85) | 0.66 (0.62–0.81) | 0.70 (0.55–0.96) | 0.6917 |
| Bilirubin (mg/dL) | 0.50 (0.40–0.76) | 0.40 (0.40–0.60) | 0.60 (0.40–0.80) | 0.1939 |
| AST–GOT (U/L) | 35 (24.50–43) | 37 (29–46) | 29 (19–36) | 0.1776 |
| ALT–GPT (U/L) | 33.50 (22–45) | 38 (25–73) | 27 (16–41) | 0.1220 |
| Ventilatory parameters | ||||
| PEEP (cmH2O) | 10 (10–12) | 10 (10–10) | 12 (10–12) | 0.1511 |
| FiO2 (%) | 75 (57–82) | 70 (60–80) | 80 (50–100) | 0.6591 |
| Tv (mL) | 480 (450–480) | 480 (450–480) | 480 (420–490) | 0.7988 |
| Tv/PBW (mL/kg) | 7.27 (6.98–7.98) | 7.49 (6.80–8.43) | 7.27 (6.98–7.66) | 0.1403 |
| Pplat (cmH2O) | 20 (18–21) | 19 (18–21) | 20 (16–23) | 0.7682 |
| DP (cmH2O) | 10 (8–11) | 10 (8–11) | 9 (8–12) | 0.6195 |
| Crs (mL/cmH2O) | 53 (43–57) | 50 (44–56) | 53 (38–61) | 0.6252 |
| pH | 7.44 (7.36–7.46) | 7.44 (7.37–7.46) | 7.42 (7.36–7.51) | 0.9682 |
| PaCO2 (mmHg) | 43 (37–51) | 43 (37–51) | 43 (41–49) | 0.8423 |
| PaO2 (mmHg) | 99 (82–134) | 99 (74–124) | 131 (84–141) | 0.2847 |
| PaO2/FiO2 (mmHg) | 148 (126–177) | 140 (122–165) | 171 (131–235) | 0.1221 |
| BE (mmol/L) | 4.4 (2.1–8.9) | 4.1 (2.2–5.9) | 5.6 (2.1–9.1) | 0.7213 |
| EtCO2 (mmHg) | 31 (27–37) | 33 (29–38) | 29 (27–34) | 0.2754 |
| Outcomes | ||||
| Duration of ventilation (days) | 35 (13–44) | 36 (8–44) | 32 (30–39) | 0.9053 |
| ICU length of stay (days) | 36 (13–45) | 37 (9–45) | 35 (30–39) | 0.8740 |
| Weaning Success n = 13 (65%) | Weaning Failure n = 7 (35%) | pweaning | pday | pweaning#day | |
|---|---|---|---|---|---|
| PEEP (cmH2O) | 0.8218 | 0.0880 | 0.7518 | ||
| T0 | 10 (7–10) | 10 (8–10) | |||
| T1 | 10 (6–12) | 8 (8–10) | |||
| T2 | 10 (8–12) | 10 (8–10) | |||
| T3 | 10 (8–10) | 10 (8–10) | |||
| T7 | 8 (8–10) | 8 (8–10) | |||
| T10 | 8 (6–9) | 8 (7–8) | |||
| FiO2 (%) | <0.0001 | 0.7325 | 0.0005 | ||
| T0 | 40 (40–60) | 50 (45–55) | |||
| T1 | 50 (40–60) | 50 (50–60) | |||
| T2 | 50 (40–55) | 60 (50–70) | |||
| T3 | 40 (40–60) | 60 (55–70) | |||
| T7 | 37 (35–45) | 70 (60–80) | |||
| T10 | 40 (32–40) | 65 (45–80) | |||
| RR (1/min) | 0.3448 | 0.0564 | 0.0054 | ||
| T0 | 20 (19–24) | 20 (14–22) | |||
| T1 | 23 (20–25) | 24 (20–26) | |||
| T2 | 24 (20–25) | 24 (14–26) | |||
| T3 | 22 (18–25) | 26 (22–28) | |||
| T7 | 20 (18–28) | 29 (28–32) | |||
| T10 | 25 (19–32) | 24 (20–27) | |||
| Tv (mL) | 0.1172 | 0.7661 | 0.2139 | ||
| T0 | 616 (486–715) | 600 (585–631) | |||
| T1 | 581 (537–660) | 570 (457–696) | |||
| T2 | 527 (432–636) | 640 (457–660) | |||
| T3 | 572 (511–646) | 610 (457–745) | |||
| T7 | 566 (493–655) | 475 (390–550) | |||
| T10 | 584 (468–600) | 492 (380–642) | |||
| Tv/PBW (mL/kg) | 0.1187 | 0.7671 | 0.2746 | ||
| T0 | 9.9 (8.2–10.8) | 9.3 (8.7–9.8) | |||
| T1 | 8.6 (8.2–11.1) | 8.4 (7.1–10.8) | |||
| T2 | 9.0 (6.8–10.9) | 9.7 (7.1–11.4) | |||
| T3 | 8.7 (8.0–10.4) | 9.2 (7.1–12.4) | |||
| T7 | 9.6 (8.7–9.9) | 7.1 (6.0–8.0) | |||
| T10 | 9.3 (7.7–12.5) | 7.2 (5.6–9.5) | |||
| MVe (L/min) | 0.6522 | 0.8115 | 0.4490 | ||
| T0 | 14 (13–15) | 12 (9–16) | |||
| T1 | 12 (10–15) | 13 (12–14) | |||
| T2 | 13 (10–15) | 12 (9–16) | |||
| T3 | 13 (10–14) | 16 (13–18) | |||
| T7 | 13 (12–16) | 13 (12–15) | |||
| T10 | 14 (9–18) | 12 (10–11) | |||
| EAdi (μV) | <0.0001 | 0.0075 | 0.0800 | ||
| T0 | 15 (14–16) | 20 (15–30) | |||
| T1 | 13 (12–16) | 25 (13–29) | |||
| T2 | 14 (12–16) | 24 (16–30) | |||
| T3 | 13 (12–14) | 18 (10–22) | |||
| T7 | 13 (10–14) | 25 (14–30) | |||
| T10 | 14 (12–20) | 28 (18–35) | |||
| PaO2 (mmHg) | 0.0576 | 0.5596 | 0.0465 | ||
| T0 | 96 (85–104) | 97 (87–114) | |||
| T1 | 100 (91–112) | 100 (83–119) | |||
| T2 | 102 (96–107) | 109 (70–139) | |||
| T3 | 90 (80–119) | 90 (65–117) | |||
| T7 | 99 (77–127) | 78 (65–91) | |||
| T10 | 105 (98–118) | 74 (69–91) | |||
| PaCO2 (mmHg) | <0.0001 | 0.5577 | 0.6513 | ||
| T0 | 41 (36–45) | 43 (38–57) | |||
| T1 | 39 (38–45) | 47 (38–50) | |||
| T2 | 40 (36–45) | 48 (40–62) | |||
| T3 | 40 (37–45) | 47 (39–52) | |||
| T7 | 44 (36–50) | 54 (43–56) | |||
| T10 | 45 (36–48) | 53 (53–55) | |||
| PaO2/FiO2 (mmHg) | <0.0001 | 0.7632 | 0.0001 | ||
| T0 | 210 (125–260) | 185 (167–228) | |||
| T1 | 224 (157–280) | 189 (166–200) | |||
| T2 | 258 (185–291) | 161 (151–232) | |||
| T3 | 218 (150–291) | 148 (105–213) | |||
| T7 | 262 (220–302) | 111 (89–163) | |||
| T10 | 298 (224–353) | 136 (92–191) | |||
| Crs (mL/cmH2O) | 0.2431 | 0.0987 | 0.3311 | ||
| T0 | 32 (28–40) | 39 (26–43) | |||
| T1 | 35 (28–40) | 38 (27–46) | |||
| T2 | 31 (30–35) | 41 (26–48) | |||
| T3 | 36 (26–40) | 33 (25–40) | |||
| T7 | 34 (28–36) | 26 (23–38) | |||
| T10 | 31 (27–39) | 27 (21–34) | |||
| EtCO2 (mmHg) | 0.1738 | 0.2703 | 0.3215 | ||
| T0 | 30 (28–35) | 26 (24–40) | |||
| T1 | 27 (26–37) | 29 (26–35) | |||
| T2 | 30 (26–35) | 32 (28–34) | |||
| T3 | 30 (25–35) | 31 (26–36) | |||
| T7 | 35 (30–37) | 33 (29–35) | |||
| T10 | 33 (31–38) | 38 (37–40) | |||
| Vd/Vt (%) | 0.0001 | 0.4257 | 0.7019 | ||
| T0 | 25.0 (19.3–29.2) | 37.5 (29.8–43.6) | |||
| T1 | 25.0 (22.5–32.5) | 32.4 (25.5–36.5) | |||
| T2 | 25.7 (16.6–33.3) | 32.0 (26.1–33.3) | |||
| T3 | 26.9 (17.7–32.4) | 34.1 (33.3–41.6) | |||
| T7 | 20.4 (17.3–28.2) | 38.8 (30.9–41.0) | |||
| T10 | 23.4 (14.5–24.4) | 28.0 (25.2–32.0) |
| Variable | Univariate | Multivariate |
|---|---|---|
| Age | OR 0.60 (95%CI 0.52–0.78) | OR 0.02 (95%CI 0.01–0.11) |
| PaO2/FiO2 | OR 1.02 (95%CI 1.01–1.11) | OR 1.10 (95%CI 1.01–1.21) |
| EAdi | OR 0.86 (95%CI 0.81–0.93) | OR 0.16 (95%CI 0.08–0.34) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muttini, S.; Jona Falco, J.; Cuevas Cairo, I.; Umbrello, M. A High Respiratory Drive Is Associated with Weaning Failure in Patients with COVID-19-Associated Acute Respiratory Distress Syndrome: The Role of the Electrical Activity of the Diaphragm. J. Clin. Med. 2024, 13, 1120. https://doi.org/10.3390/jcm13041120
Muttini S, Jona Falco J, Cuevas Cairo I, Umbrello M. A High Respiratory Drive Is Associated with Weaning Failure in Patients with COVID-19-Associated Acute Respiratory Distress Syndrome: The Role of the Electrical Activity of the Diaphragm. Journal of Clinical Medicine. 2024; 13(4):1120. https://doi.org/10.3390/jcm13041120
Chicago/Turabian StyleMuttini, Stefano, Jacopo Jona Falco, Ilmari Cuevas Cairo, and Michele Umbrello. 2024. "A High Respiratory Drive Is Associated with Weaning Failure in Patients with COVID-19-Associated Acute Respiratory Distress Syndrome: The Role of the Electrical Activity of the Diaphragm" Journal of Clinical Medicine 13, no. 4: 1120. https://doi.org/10.3390/jcm13041120







