Platelet Reduction after Transcatheter Aortic Valve Implantation: Results from the PORTRAIT Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Inclusion and Exclusion Criteria
2.3. Definitions and Endpoints
2.4. Statistical Analysis
3. Results
3.1. Study Population
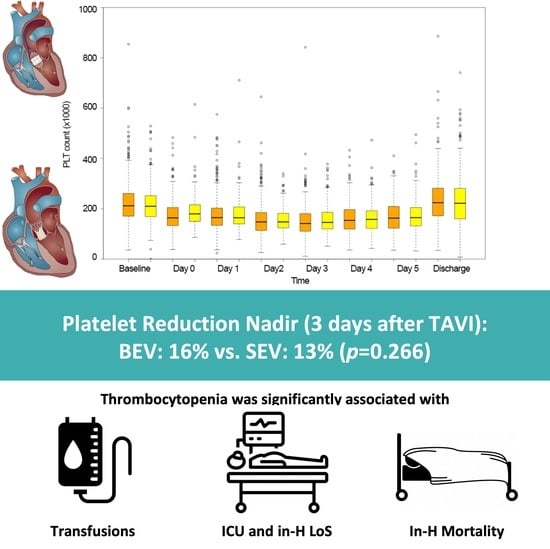
3.2. Changes in Blood Elements after TAVI
3.3. Early Clinical Outcomes after TAVI
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Writing Committee Members; Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Thorac. Cardiovasc. Surg. 2021, 162, e183–e353. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Bourantas, C.V.; Modolo, R.; Baumbach, A.; Søndergaard, L.; Prendergast, B.D.; Ozkor, M.; Kennon, S.; Mathur, A.; Mullen, M.J.; Serruys, P.W. The evolution of device technology in transcatheter aortic valve implantation. EuroIntervention 2019, 14, e1826–e1833. [Google Scholar] [CrossRef] [PubMed]
- Cribier, A. The development of transcatheter aortic valve replacement (TAVR). Glob. Cardiol. Sci. Pr. 2017, 2016, e201632. [Google Scholar] [CrossRef] [PubMed]
- Jiritano, F.; Santarpino, G.; Serraino, G.F.; Ten Cate, H.; Matteucci, M.; Fina, D.; Mastroroberto, P.; Lorusso, R. Peri-procedural thrombocytopenia after aortic bioprosthesis implant: A sys-tematic review and meta-analysis comparison among conventional, stentless, rapid-deployment, and transcatheter valves. Int. J. Cardiol. 2019, 296, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Mitrosz, M.; Chlabicz, M.; Hapaniuk, K.; Kaminski, K.A.; Sobkowicz, B.; Piszcz, J.; Dobrzycki, S.; Musial, W.J.; Hirnle, T.; Tycinska, A.M. Thrombocytopenia associated with TAVI—The summary of possible causes. Adv. Med. Sci. 2017, 62, 378–382. [Google Scholar] [CrossRef]
- Hernández-Enríquez, M.; Chollet, T.; Bataille, V.; Campelo-Parada, F.; Boudou, N.; Bouisset, F.; Grunenwald, E.; Porterie, J.; Freixa, X.; Regueiro, A.; et al. Comparison of the Frequency of Thrombocytopenia After Transfemoral Transcatheter Aortic Valve Implantation Between Balloon-Expandable and Self-Expanding Valves. Am. J. Cardiol. 2019, 123, 1120–1126. [Google Scholar] [CrossRef]
- Dvir, D.; Généreux, P.; Barbash, I.M.; Kodali, S.; Ben-Dor, I.; Williams, M.; Torguson, R.; Kirtane, A.J.; Minha, S.; Badr, S.; et al. Acquired thrombocytopenia after transcatheter aortic valve replacement: Clinical correlates and association with outcomes. Eur. Heart J. 2014, 35, 2663–2671. [Google Scholar] [CrossRef]
- Erkurt, M.A.; Kaya, E.; Berber, I.; Koroglu, M.; Kuku, I. Thrombocytopenia in Adults: Review Article. J. Hematol. 2012, 1, 44–53. [Google Scholar] [CrossRef]
- Santoshi, R.K.; Patel, R.; Patel, N.S.; Bansro, V.; Chhabra, G. A Comprehensive Review of Thrombocytopenia With a Spotlight on Intensive Care Patients. Cureus 2022, 14, e27718. [Google Scholar] [CrossRef]
- VARC-3 WRITING COMMITTEE; Généreux, P.; Piazza, N.; Alu, M.C.; Nazif, T.; Hahn, R.T.; Pibarot, P.; Bax, J.J.; Leipsic, J.A.; Blanke, P.; et al. Valve Academic Research Consortium 3: Updated endpoint definitions for aortic valve clinical research. Eur. Heart J. 2021, 42, 1825–1857. [Google Scholar] [CrossRef]
- Lorusso, R.; Jiritano, F.; Roselli, E.; Shrestha, M.; Folliguet, T.; Meuris, B.; Pollari, F.; Fischlein, T.; the PERSIST-AVR Investigators. Perioperative platelet reduction after sutureless or stented valve implantation: Results from the PERSIST-AVR controlled randomized trial. Eur. J. Cardio-Thorac. Surg. 2021, 60, 1359–1365. [Google Scholar] [CrossRef]
- Vogt, F.; Moscarelli, M.; Pollari, F.; Kalisnik, J.M.; Pfeiffer, S.; Fittkau, M.; Sirch, J.; Pförringer, D.; Jessl, J.; Eckner, D.; et al. Two approaches—One phenomenon—Thrombocytopenia after surgical and transcatheter aortic valve replacement. J. Card. Surg. 2020, 35, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Miura, D.; Takamori, A.; Nogami, E.; Yunoki, J.; Sakaguchi, Y. Predictors of short-term thrombocytopenia after transcatheter aortic valve implantation: A retrospective study at a single Japanese center. BMC Res. Notes 2020, 13, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Mondal, N.K.; Ding, J.; Koenig, S.C.; Slaughter, M.S.; Wu, Z.J. Paradoxical Effect of Nonphysiological Shear Stress on Platelets and von Willebrand Factor. Artif. Organs 2015, 40, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Yerebakan, C.; Kaminski, A.; Westphal, B.; Kundt, G.; Ugurlucan, M.; Steinhoff, G.; Liebold, A. Thrombocytopenia after aortic valve replacement with the Freedom Solo stentless bioprosthesis. Interact. Cardiovasc. Thorac. Surg. 2008, 7, 616–620. [Google Scholar] [CrossRef] [PubMed]
- Corcione, N.; Romano, S.; Morello, A.; Ferraro, P.; Cimmino, M.; Albanese, M.; Tufano, M.; Capasso, D.; Buonpane, S.; Giordano, S.; et al. Thrombocytopenia Complicating Transcatheter Aortic Valve Implantation: Differences Between Two New-Generation Devices. J. Cardiovasc. Transl. Res. 2021, 14, 1104–1113. [Google Scholar] [CrossRef] [PubMed]
- Gallet, R.; Seemann, A.; Yamamoto, M.; Hayat, D.; Mouillet, G.; Monin, J.-L.; Gueret, P.; Couetil, J.-P.; Dubois-Randé, J.-L.; Teiger, E.; et al. Effect of transcatheter (via femoral artery) aortic valve implantation on the platelet count and its consequences. Am. J. Cardiol. 2013, 111, 1619–1624. [Google Scholar] [CrossRef] [PubMed]
- Cubero-Gómez, J.M.; Guerrero Márquez, F.J.; Diaz-de la-Llera, L.; Fernández-Quero, M.; Guisado-Rasco, A.; Villa-Gil-Ortega, M. Severe thrombocytopenia induced by iodinated contrast after coronary angiography: The use of gadolinium contrast and intravascular ultrasound as an alternative to guide percutaneous coronary intervention. Rev. Port. Cardiol. 2017, 36, e1–e61. [Google Scholar] [CrossRef]
- Spagnolo, P.; Giglio, M.; Di Marco, D.; Latib, A.; Besana, F.; Chieffo, A.; Montorfano, M.; Sironi, S.; Alfieri, O.; Colombo, A. Feasibility of ultra-low contrast 64-slice computed tomography angiography before transcatheter aortic valve implantation: A real-world experience. Eur. Heart J. -Cardiovasc. Imaging 2016, 17, 24–33. [Google Scholar] [CrossRef]
- Abu Khadija, H.; Gandelman, G.; Ayyad, O.; Jaber, M.; Poles, L.; Jonas, M.; Paz, O.; Abu Sbaih, F.; Sella, G.; Shimoni, S.; et al. Differential systemic inflammatory responses after TAVI: The role of self versus balloon expandable devices. PLoS ONE 2021, 16, e0258963. [Google Scholar] [CrossRef] [PubMed]
- Jilaihawi, H.; Doctor, N.; Chakravarty, T.; Kashif, M.; Mirocha, J.; Cheng, W.; Lill, M.; Nakamura, M.; Gheorghiu, M.; Makkar, R.R. Major thrombocytopenia after balloon-expandable transcatheter aortic valve replacement: Prognostic implications and comparison to surgical aortic valve replacement. Catheter. Cardiovasc. Interv. 2015, 85, 130–137. [Google Scholar] [CrossRef]
- McCabe, J.M.; Huang, P.; Riedl, L.A.; Devireddy, S.R.; Grondell, J.; Connors, A.C.; Davidson, M.J.; Eisenhauer, A.C.; Welt, F.G.P. Incidence and implications of idiopathic thrombocytopenia following transcatheter aortic valve replacement with the Edwards Sapien© valves: A single center experience. Catheter. Cardiovasc. Interv. 2014, 83, 633–641. [Google Scholar] [CrossRef]
- Flaherty, M.P.; Mohsen, A.; Moore, J.B., 4th; Bartoli, C.R.; Schneibel, E.; Rawasia, W.; Williams, M.L.; Grubb, K.J.; Hirsch, G.A. Predictors and clinical impact of pre-existing and acquired thrombocytopenia following transcatheter aortic valve replacement. Catheter. Cardiovasc. Interv. 2015, 85, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Zahid, S.; Ullah, W.; Khan, M.U.; Abbas, S.; Din, M.T.U.; Uddin, M.F.; Inayat, A.; Ubaid, A.; Salman, F.; Thakkar, S.; et al. Trends, predictors, and outcomes of major bleeding after transcatheter aortic valve implantation, from national inpatient sample (2011–2018). Expert Rev. Cardiovasc. Ther. 2021, 19, 557–563. [Google Scholar] [CrossRef] [PubMed]



| Overall Population (n = 632) | SEV (n = 316) | BEV (n = 316) | SMD | |
|---|---|---|---|---|
| Age (years) | 81.1 ± 6.1 | 81.3 ± 6.1) | 80.9 ± 6.1) | 0.07 |
| Female gender | 333 (52.7%) | 171 (54.1%) | 162 (51.3%) | 0.06 |
| BMI (kg/m2) | 27.3 ± 4.9 | 27.3 ± 4.9 | 27.3 ± 4.9 | −0.01 |
| BSA (m2) | 1.9 ± 0.2 | 1.8 ± 0.2 | 1.9 ± 0.2 | −0.04 |
| Hypertension | 596 (94.3%) | 299 (94.6%) | 297 (94.0%) | 0.06 |
| Diabetes mellitus type II | 249 (39.4%) | 122 (38.6%) | 127 (40.2%) | −0.04 |
| Smoking | 349 (55.2%) | 172 (54.4%) | 177 (56.0%) | −0.04 |
| Dyslipidemia | 460 (72.8%) | 230 (72.8%) | 230 (72.8%) | 0.00 |
| NYHA class | 0.03 | |||
| I | 10 (1.6%) | 5 (1.6%) | 5 (1.6%) | |
| II | 97 (15.3%) | 52 (16.5%) | 45 (14.2%) | |
| III | 420 (66.5%) | 209 (66.1%) | 211 (66.8%) | |
| IV | 105 (16.6%) | 50 (15.8%) | 55 (17.4%) | |
| COPD | 128 (20.3%) | 61 (19.3%) | 67 (21.2%) | −0.06 |
| Atrial fibrillation | 238 (37.7%) | 116 (36.7%) | 122 (38.6%) | −0.04 |
| Prior ischemic stroke | 136 (21.5%) | 84 (26.6%) | 52 (16.5%) | 0.33 |
| PAD | 93 (14.7%) | 57 (18.0%) | 36 (11.4%) | 0.29 |
| Prior MI | 67 (10.6%) | 33 (10.4%) | 34 (10.8%) | −0.02 |
| Prior PCI | 172 (27.2%) | 91 (28.8%) | 81 (25.6%) | 0.09 |
| Prior CABG | 112 (17.7%) | 54 (17.1%) | 58 (18.4%) | −0.01 |
| Prior valve surgery | 142 (22.5%) | 69 (21.8%) | 73 (23.1%) | −0.04 |
| Prior ASA treatment | 23 (3.6%) | 12 (3.8%) | 10 (3.2%) | 0.10 |
| Prior DAPT treatment | 24 (3.8%) | 14 (4.4%) | 10 (3.2%) | 0.15 |
| Prior LMWH treatment | 21 (3.3%) | 12 (3.8%) | 9 (2.8%) | 0.17 |
| Prior warfarin treatment | 17 (2.7%) | 9 (2.8%) | 8 (2.5%) | 0.06 |
| Prior DOAC treatment | 17 (2.7%) | 10 (3.2%) | 7 (2.2%) | 0.16 |
| EuroSCORE II | 6.2 (3.8–10.6) | 6.2 (4.1–11.8) | 6.1 (3.6–11.0) | −0.09 |
| Echocardiographic features | ||||
| AV peak gradient (mmHg) | 62.9 ± 30.9 | 63.6 ± 30.9 | 62.2 ± 30.9 | 0.05 |
| AV mean gradient (mmHg) | 43.7 ± 14.2 | 43.9 ± 14.7 | 43.6 ± 13.8 | 0.01 |
| AVA/BSA (cm2/m2) | 0.40 ± 0.10 | 0.39 ± 0.09 | 0.39 ± 0.10 | 0.01 |
| LVEF (%) | 51.5 ± 12.8 | 51.3 ± 12.2 | 51.6 ± 13.5 | −0.02 |
| AR mean grade | 0.06 | |||
| None | 297 (47.0%) | 143 (45.3%) | 154 (48.7%) | |
| Mild | 72 (11.4%) | 38 (12.0%) | 34 (10.8%) | |
| Moderate | 263 (41.6%) | 135 (42.7%) | 128 (40.5%) | |
| Severe | 0 (0%) | 0 (0%) | 0 (0%) | |
| sPAP (mmHg) | 53.4 ± 16.1 | 52.9 ± 16.3 | 53.9 ± 15.9 | −0.06 |
| Status | −0.08 | |||
| Elective | 586 (92.7%) | 297 (94.0%) | 289 (91.5%) | |
| Urgent | 45 (7.1%) | 18 (5.7%) | 27 (8.5%) | |
| Emergent | 1 (0.2%) | 1 (0.3%) | 0 (0%) | |
| Access | 0.06 | |||
| Femoral artery | 474 (75.0%) | 233 (73.7%) | 241 (76.3%) | |
| LV apex | 157 (24.8%) | 83 (26.3%) | 74 (23.4%) | |
| Ascending aorta | 1 (0.2%) | 0 (0%) | 1 (0.3%) | |
| Carotid artery | 0 (0%) | 0 (0%) | 0 (0%) | |
| Access conversion | 6 (0.9%) | 3 (0.9%) | 3 (0.9%) | 0.00 |
| TIME | Overall Population (n = 632) | SEV (n = 316) | BEV (n = 316) | p-Value |
|---|---|---|---|---|
| Platelet count (×103 µL) | ||||
| Baseline | 211 (171–254) | 208 (169–252) | 213 (177–261) | 0.189 |
| Day 0 | 175 (137–206) | 176 (147–212) | 164 (130–199) | 0.216 |
| Day 1 | 166 (137–205) | 164 (138–208) | 169 (137–202) | 0.912 |
| Day 2 | 149 (120–185) | 150 (124–189) | 149 (112–183) | 0.330 |
| Day 3 | 147 (114–186) | 149 (120–186) | 146 (108–181) | 0.142 |
| Day 4 | 155 (122–200) | 162 (128–197) | 147 (118–200) | 0.203 |
| Day 5 | 166 (126–212) | 166 (136–207) | 165 (122–218) | 0.634 |
| Discharge | 227 (169–283) | 234 (174–290) | 217 (166–278) | 0.196 |
| Hemoglobin (g/dL) | ||||
| Baseline | 12.3 (11.0–13.4) | 12.3 (11.0–13.4) | 12.2 (11.0–13.4) | 0.945 |
| Day 0 | 10.9 (9.9–12.1) | 11.1 (10.0–12.1) | 10.8 (9.9–12.2) | 0.614 |
| Day 1 | 10.4 (9.3–11.5) | 10.5 (9.43–11.4) | 10.4 (9.3–11.6) | 0.810 |
| Day 2 | 10.1 (9.1–11.3) | 10.2 (9.1–11.3) | 10.1 (9.1–11.2) | 0.591 |
| Day 3 | 9.9 (8.9–10.8) | 10.1 (9.1–11.4) | 9.9 (9.1–11.1) | 0.147 |
| Day 4 | 9.8 (9.0–11.1) | 9.9 (9.0–11.2) | 9.9 (9.0–11.2) | 0.561 |
| Day 5 | 9.5 (8.8–11.1) | 10.1 (9.0–11.3) | 10.0 (9.0–11.0) | 0.124 |
| Discharge | 10.8 (9.67–11.7) | 10.5 (9.5–11.7) | 10.6 (9.5–11.7) | 0.143 |
| Red blood cells (×1,000,000/µL) | ||||
| Baseline | 4.2 (3.8–4.6) | 4.2 (3.8–4.6) | 4.1 (3.7–4.5) | 0.677 |
| Day 0 | 3.7 (3.3–4.1) | 3.8 (3.3–4.1) | 3.7 (3.3–4.1) | 0.638 |
| Day 1 | 3.5 (3.2–3.9) | 3.5 (3.1–3.9) | 3.5 (3.2–3.9) | 0.969 |
| Day 2 | 3.5 (3.1–3.9) | 3.4 (3.1–3.7) | 3.4 (3.1–3.9) | 0.623 |
| Day 3 | 3.4 (3.1–3.8) | 3.4 (3.1–3.8) | 3.4 (3.1–3.8) | 0.095 |
| Day 4 | 3.4 (3.1–3.8) | 3.4 (3.1–3.8) | 3.4 (3.1–3.8) | 0.335 |
| Day 5 | 3.3 (3.1–3.7) | 3.3 (3.0–3.8) | 3.4 (3.1–3.7) | 0.199 |
| Discharge | 3.6 (3.3–4.0) | 3.6 (3.3–4.0) | 3.6 (3.3–4.1) | 0.493 |
| White Blood cells (×103 µL) | ||||
| Baseline | 7.0 (5.8–8.4) | 7.0 (5.8–8.2) | 6.9 (5.8–8.7) | 0.494 |
| Day 0 | 8.5 (6.7–10.8) | 8.5 (6.7–10.7) | 8.6 (6.5–11.50) | 0.503 |
| Day 1 | 9.3 (7.7–11.5) | 9.8 (7.9–12.3) | 8.8 (7.4–10.9) | <0.001 |
| Day 2 | 9.0 (7.3–11.4) | 9.5 (7.6–12.1) | 8.7 (7.2–10.3) | <0.001 |
| Day 3 | 8.1 (6.6–10.1) | 8.6 (6.8–10.5) | 7.7 (6.4–9.4) | 0.022 |
| Day 4 | 7.7 (6.2–9.9) | 8.0 (6.7–10.1) | 7.5 (5.9–9.5) | 0.188 |
| Day 5 | 7.5 (6.2–9.6) | 7.7 (6.0–9.7) | 7.2 (5.8–9.0) | 0.772 |
| Discharge | 7.2 (6.0–8.9) | 7.3 (6.1–8.9) | 7.1 (5.8–9.1) | 0.192 |
| Overall Population (n = 632) | SEV (n = 316) | BEV (n = 316) | p-Value | |
|---|---|---|---|---|
| RBC transfusions | 0.138 | |||
| 0 | 495 (78.3%) | 256 (81.0%) | 239 (75.6%) | |
| 1 | 38 (6.0%) | 9 (2.8%) | 29 (9.2%) | |
| 2 | 54 (8.5%) | 28 (8.9%) | 26 (8.2%) | |
| >2 | 45 (7.2%) | 23 (7.2%) | 22 (6.8%) | |
| Echocardiographic features | ||||
| AV peak gradient (mmHg) | 21.6 ± 10.3 | 20.2 ± 10.7 | 23.7 ± 9.9 | 0.274 |
| AV mean gradient (mmHg) | 11.1 ± 5.5 | 10.1 ± 5.8 | 12.2 ± 5.3 | 0.662 |
| LVEF (%) | 55.4 ± 11.9 | 57.3 ± 11.6 | 53.9 ± 12.3 | 0.265 |
| Intraprosthetic regurgitation | 177 (28.1%) | 102 (34.2%) | 75 (24.9%) | 0.065 |
| Paravalvular leak | 177 (28.1%) | 75 (24.9%) | 7 (34.2%) | 0.065 |
| Moderate or severe | 27 (4.2%) | 8 (2.5%) | 19 (6.4%) | 0.062 |
| Antiplatelet/Anticoagulant therapy post-TAVI | ||||
| Post ASA treatment | 338 (53.5%) | 149 (47.2%) | 189 (59.8%) | 0.001 |
| Post DAPT treatment | 238 (37.7%) | 125 (39.6%) | 113 (35.8%) | 0.384 |
| Post LMWH treatment | 12 (1.9%) | 5 (1.6%) | 7 (2.2%) | 0.772 |
| Post warfarin treatment | 193 (31%) | 96 (30.4%) | 100 (31.6%) | 0.731 |
| Post DOAC treatment | 41 (6.5%) | 25 (7.9%) | 16 (5.0%) | 0.560 |
| Early outcomes post-TAVI | ||||
| Intracranial bleeding | 1 (0.2%) | 0 (0%) | 1 (0.3%) | 1.000 |
| Gastrointestinal bleeding | 4 (0.6%) | 2 (0.6%) | 2 (0.6%) | 1.000 |
| Atrial fibrillation | 30 (4.7%) | 16 (6.1%) | 14 (4.4%) | 0.708 |
| ICU LoS | 1 (1–2) | 1 (1–2) | 1 (1–2) | 0.211 |
| In-hospital LoS | 8 (7–13) | 9 (7–13) | 8 (7–12) | 0.386 |
| In-hospital mortality | 40 (6.3%) | 15 (4.7%) | 25 (7.9%) | 0.102 |
| Predictive Estimate (95% Conf. Interval) | p-Value | |
|---|---|---|
| Need for RBC transfusion | 2.611 * (1.907–8.275) | <0.001 |
| Need for FFP transfusion | 23.022 * (2.533–209.216) | 0.007 |
| Need for PLT transfusion | 21.941 * (4.474–107.612) | 0.001 |
| ICU LoS | 1.907 † (1.537– 2.367) | <0.001 |
| Prolonged ICU LoS ‡ | 1.851 * (1.147–2.988) | 0.012 |
| H LoS | 1.086 † (0.948–1.246) | 0.230 |
| Prolonged H LoS § | 1.963 * (1.241–3.105) | 0.004 |
| In-hospital mortality | 3.972 * (1.907–8.275) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiritano, F.; Di Mauro, M.; Serraino, G.F.; Mastroroberto, P.; Caporali, E.; Ferrari, E.; Kowalewski, M.; Scrofani, R.; Patanè, L.; Visicchio, G.; et al. Platelet Reduction after Transcatheter Aortic Valve Implantation: Results from the PORTRAIT Study. J. Clin. Med. 2024, 13, 1579. https://doi.org/10.3390/jcm13061579
Jiritano F, Di Mauro M, Serraino GF, Mastroroberto P, Caporali E, Ferrari E, Kowalewski M, Scrofani R, Patanè L, Visicchio G, et al. Platelet Reduction after Transcatheter Aortic Valve Implantation: Results from the PORTRAIT Study. Journal of Clinical Medicine. 2024; 13(6):1579. https://doi.org/10.3390/jcm13061579
Chicago/Turabian StyleJiritano, Federica, Michele Di Mauro, Giuseppe Filiberto Serraino, Pasquale Mastroroberto, Elena Caporali, Enrico Ferrari, Mariusz Kowalewski, Roberto Scrofani, Leonardo Patanè, Giuseppe Visicchio, and et al. 2024. "Platelet Reduction after Transcatheter Aortic Valve Implantation: Results from the PORTRAIT Study" Journal of Clinical Medicine 13, no. 6: 1579. https://doi.org/10.3390/jcm13061579