Comparative Analysis of Corneal Higher-Order Aberrations after Laser-Assisted In Situ Keratomileusis, Photorefractive Keratectomy, and Small Incision Lenticule Extraction with Correlations to Change in Myopic Q-Value and Spherical Equivalent with and without Astigmatism
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Surgical Methods
2.4. Study Measurements
2.5. Statistical Methods and Data Analysis
3. Results
3.1. Pre-Operative Characteristics
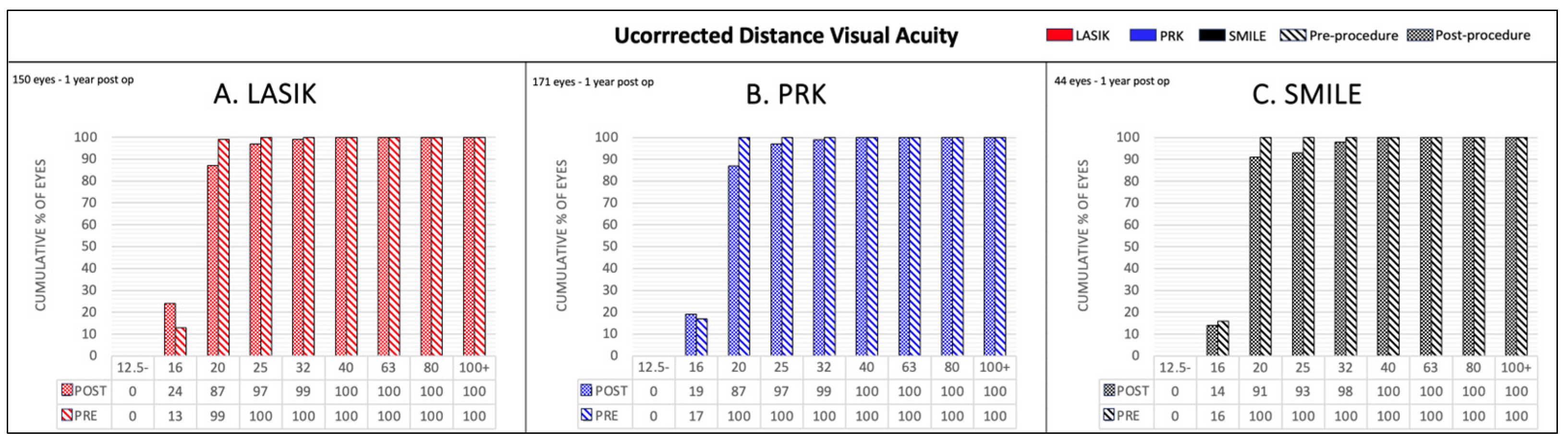
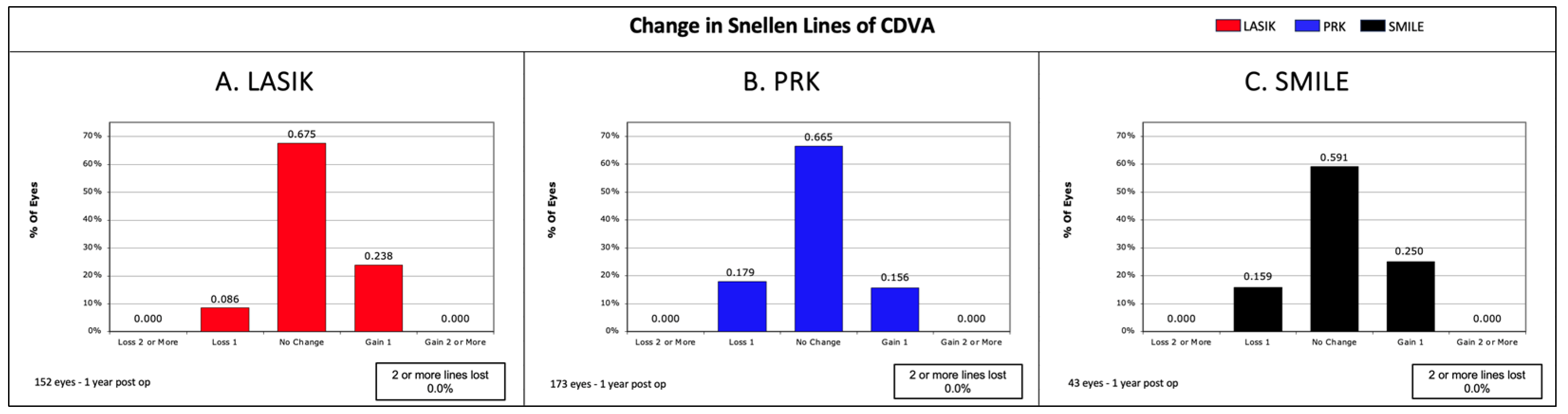
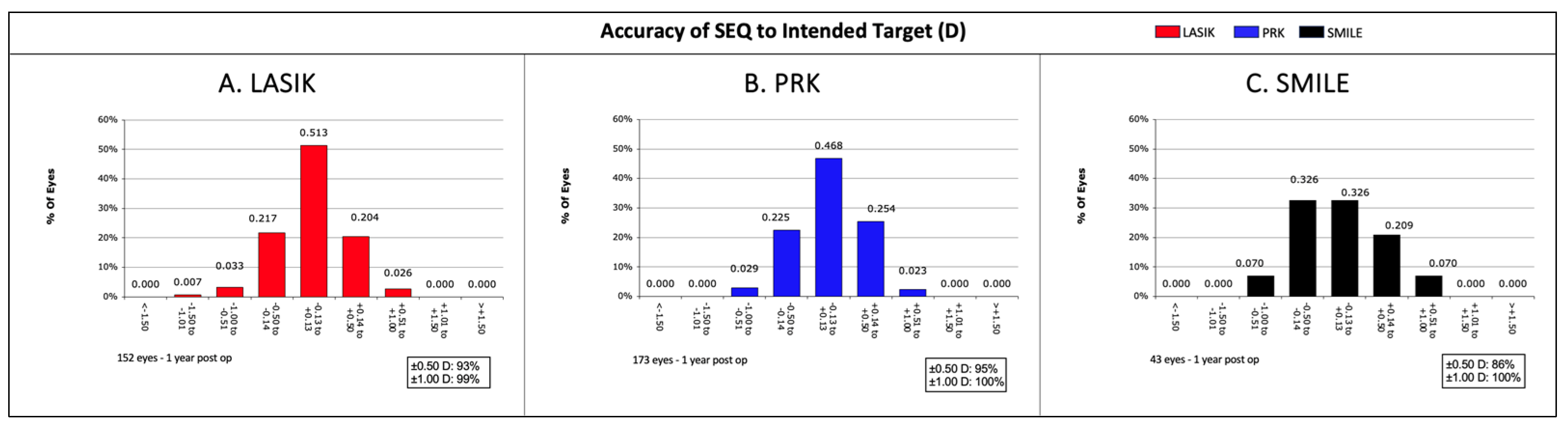
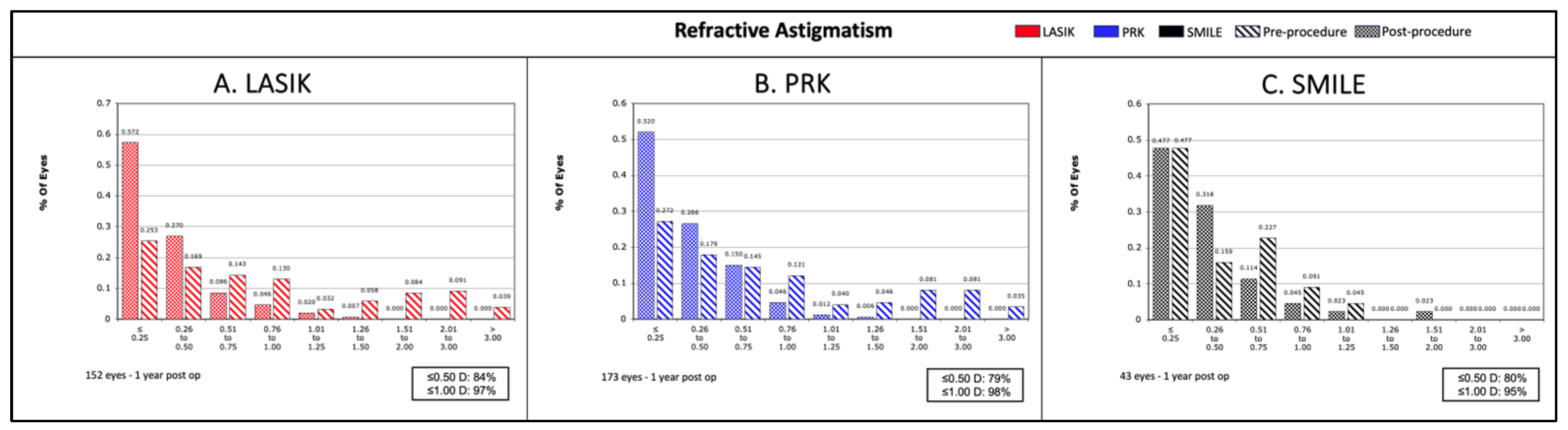
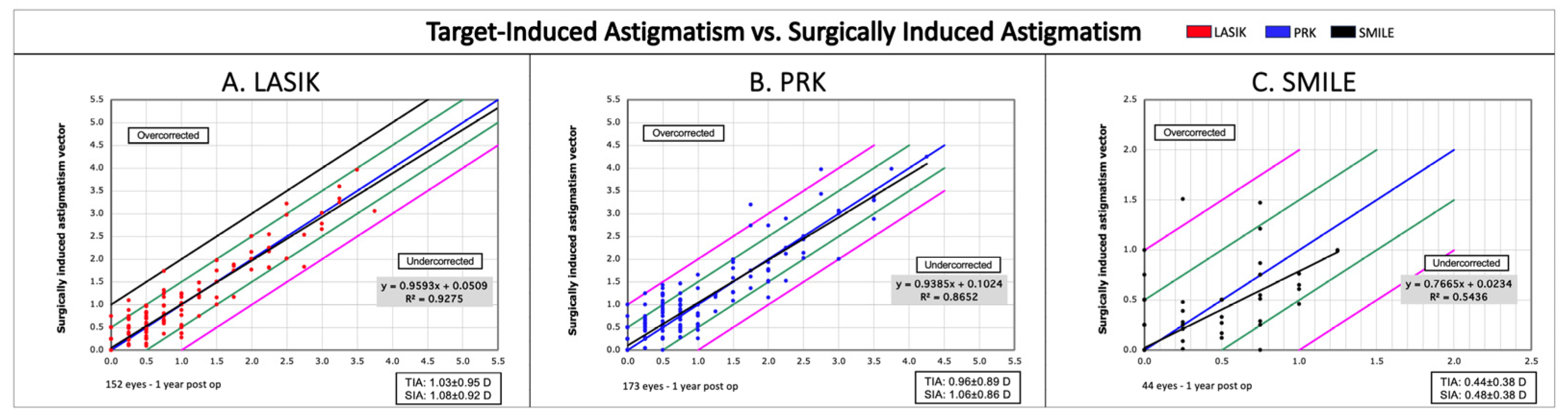
3.2. Visual Outcomes
3.3. Higher-Order Aberration (HOA) Analysis
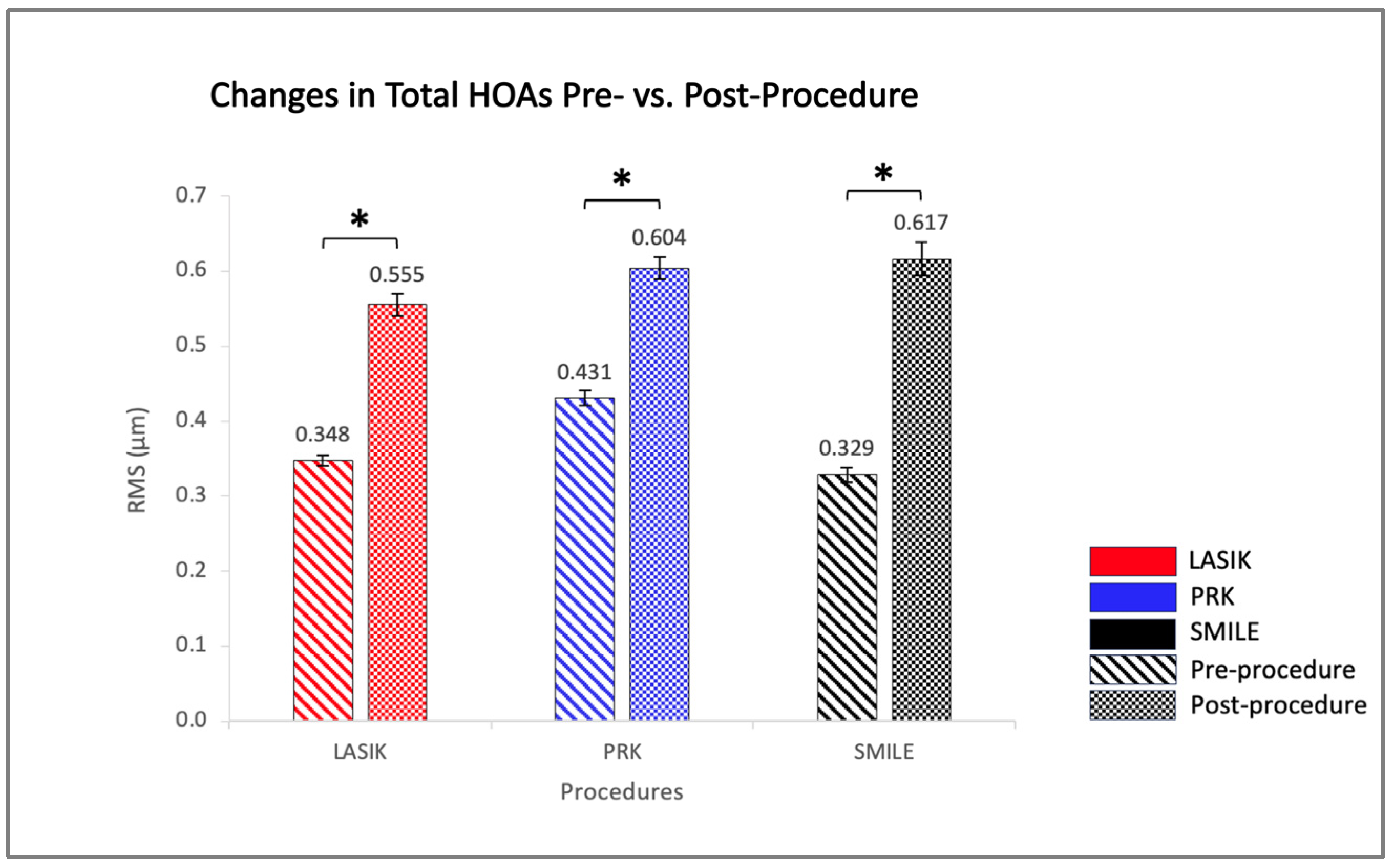
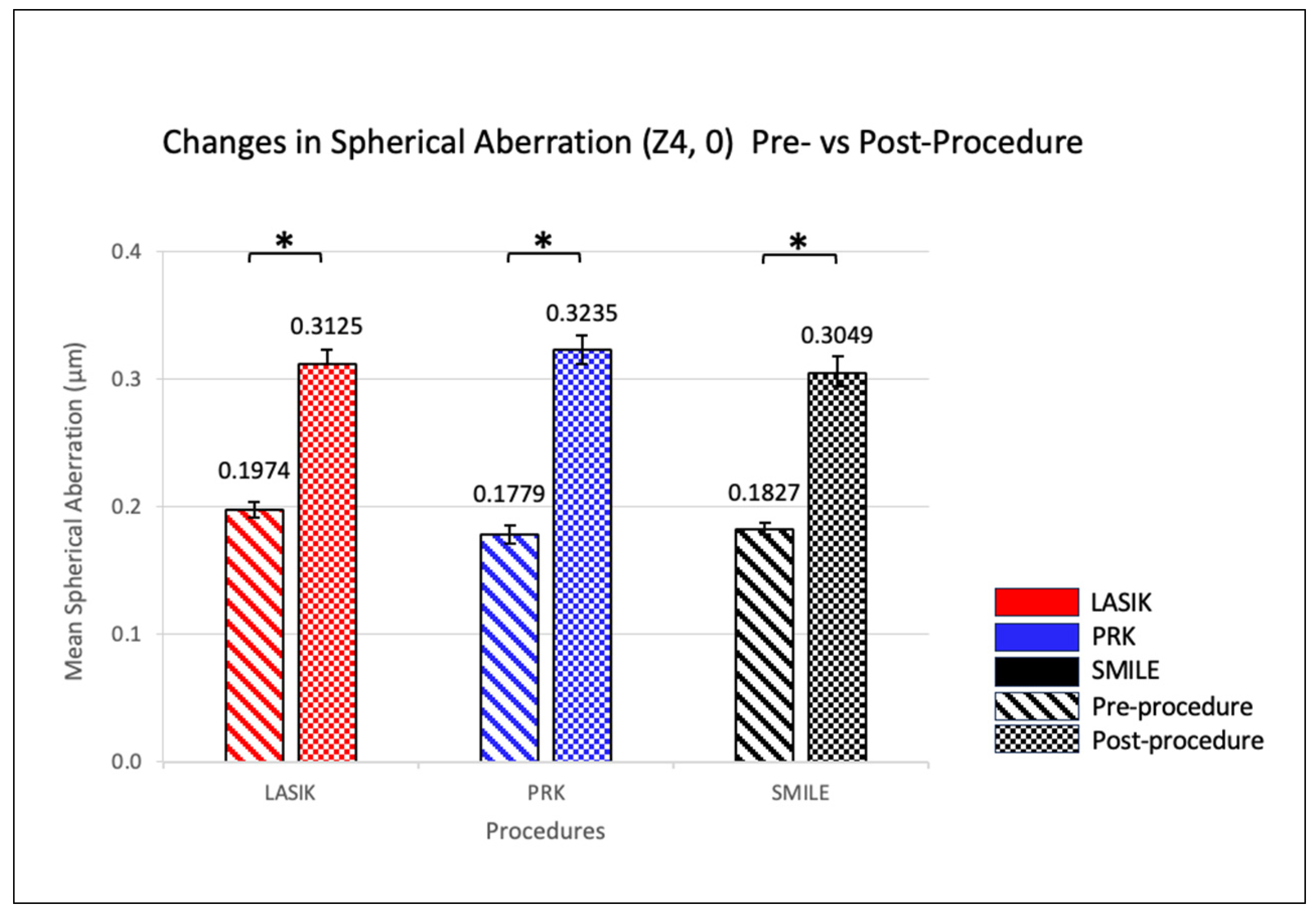
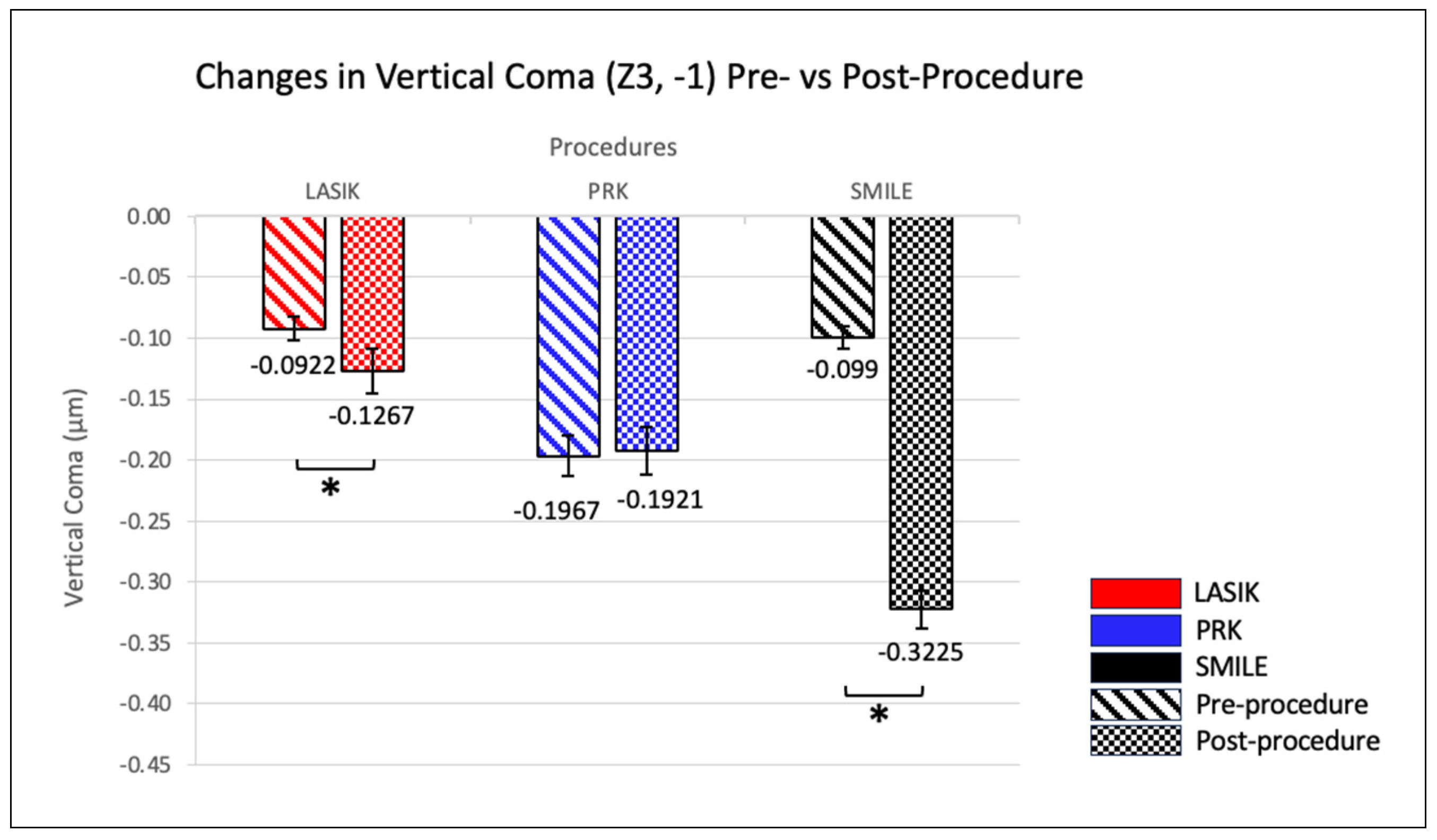
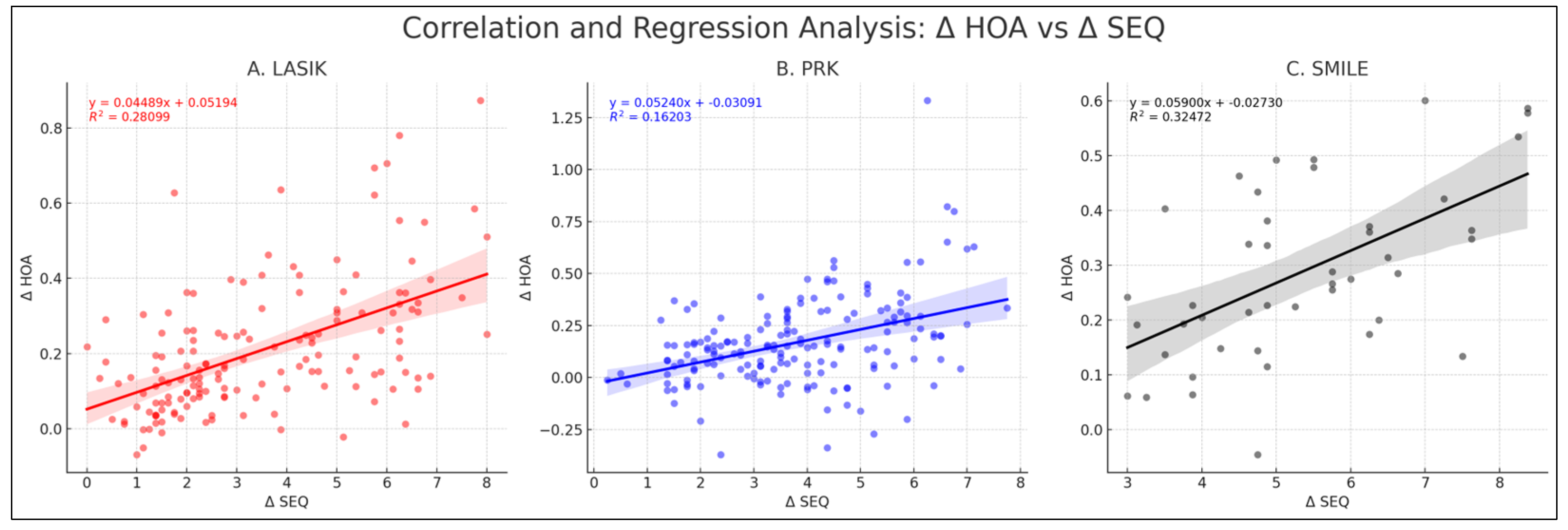
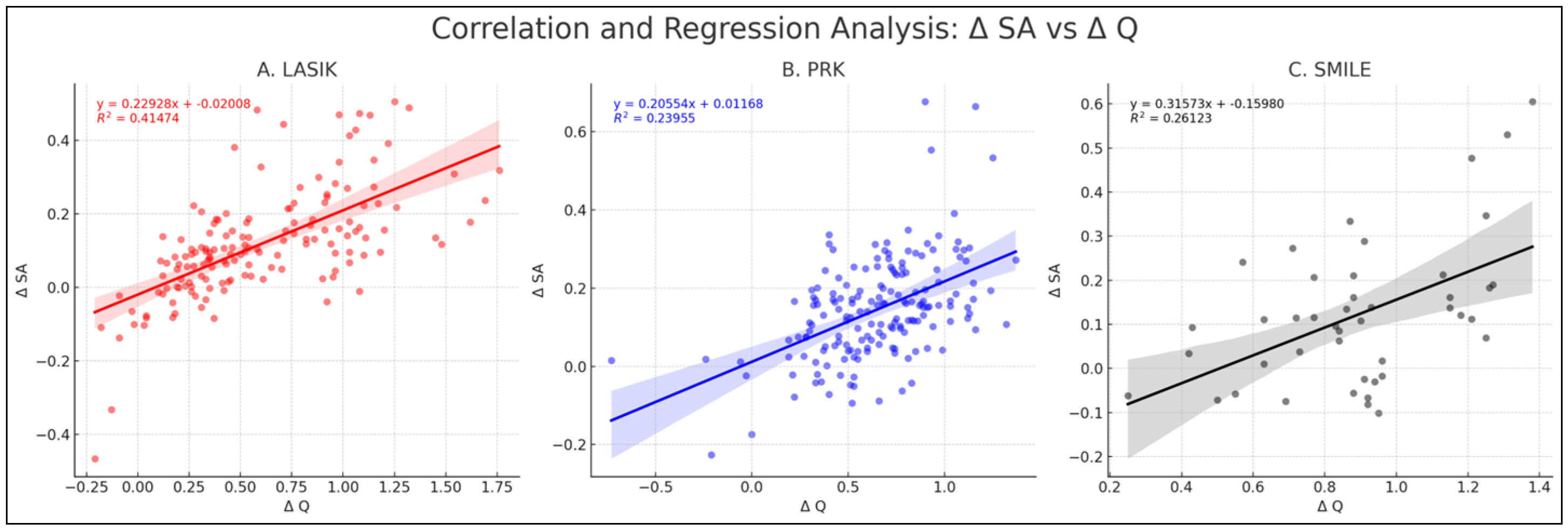
3.4. Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A




| Study | Imaging Modality | Eyes (Approx. Eyes/Patient) | Procedures | Comments | Total HOAs (μm) | Spherical Aberration (μm) | Vertical Coma (μm) | Horizontal Coma (μm) | Oblique Trefoil | Horizontal Trefoil |
|---|---|---|---|---|---|---|---|---|---|---|
| Our Study | Pentacam | 154 (2) | LASIK | 1 year | 0.2070 ± 0.1974 | 0.1160 ± 0.1665 | −0.0348 ± 0.2722 | NS | NS | NS |
| 173 (2) | PRK | 0.1680 ± 1.3092 | 0.1460 ± 0.1666 | NS | NS | −0.0318 ± 0.1802 | NS | |||
| 44 (2) | SMILE | 0.2880 ± 0.1607 | 0.1220 ± 0.6523 | −0.2240 ± 0.2403 | NS | NS | NS | |||
| Wu, et al., 2021 [15] | Pentacam | 88 (2) | LASIK | 6 months | 0.31 ± 0.25 | 0.17 ± 0.11 | 0.24 ± 0.18 | 0.14 ± 0.16 | NR | NR |
| 64 (2) | PRK | 0.31 ± 0.18 | 0.2 ± 0.15 | 0.11 ± 0.15 | 0.12 ± 0.18 | |||||
| Kang E., et al., 2022 [22] | Pentacam | 45 | LASIK | 6 months | NS | NS | NS | NS | ||
| 45 | SMILE | 0.151 ± 0.178 | 0.074 ± 0.162 | 0.181 ± 0.233 | NS | |||||
| Miraftab M., et al., 2021 [16] | Sirius | 124 (1) | LASIK | Stratified by moderate or high myopic patients; moderate results have been included here; 12-month data; 6 mm pupil | 0.38 ± 0.36 | 0.24 ± 0.1 | 0.25 ± 0.23 | NS | ||
| 124 (1) | PRK | 0.33 ± 0.25 | 0.26 ± 0.13 | 0.24 ± 0.24 | NS | |||||
| 124 (1) | SMILE | 0.16 ± 0.32 | 0.11 ± 0.09 | 0.16 ± 0.23 | NS | |||||
References
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Shah, R. History and Results; Indications and Contraindications of SMILE Compared with LASIK. Asia Pac. J. Ophthalmol. 2019, 8, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Jumbo, O.E.; Asfour, S.; Sayed, A.M.; Abdel-Mottaleb, M. Correcting Higher Order Aberrations Using Image Processing. IEEE Trans. Image Process. 2021, 30, 2276–2287. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Sun, X.; Chen, Y. Comparison of Corneal Optical Quality after SMILE, Wavefront-Optimized LASIK and Topography-Guided LASIK for Myopia and Myopic Astigmatism. Front. Med. 2022, 9, 859. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Y.; Lin, P.Y.; Hsu, C.C.; Liu, C.J.L. Comparison of clinical outcomes of LASIK, Trans-PRK, and SMILE for correction of myopia. J. Chin. Med. Assoc. 2022, 85, 145–151. [Google Scholar] [CrossRef]
- Lau, Y.T.Y.; Shih, K.C.; Tse, R.H.K.; Chan, T.C.Y.; Jhanji, V. Comparison of Visual, Refractive and Ocular Surface Outcomes between Small Incision Lenticule Extraction and Laser-Assisted In Situ Keratomileusis for Myopia and Myopic Astigmatism. Ophthalmol. Ther. 2019, 8, 373–386. [Google Scholar] [CrossRef]
- Chiche, A.; Trinh, L.; Baudouin, C.; Denoyer, A. SMILE (Small Incision Lenticule Extraction) among the corneal refractive surgeries in 2018. J. Fr. Ophtalmol. 2018, 41, e245–e252. [Google Scholar] [CrossRef]
- Jung, H.H.; Ji, Y.S.; Oh, H.J.; Yoon, K.C. Higher order aberrations of the corneal surface after laser subepithelial keratomileusis. Korean J. Ophthalmol. 2014, 28, 285–291. [Google Scholar] [CrossRef]
- Jin, H.Y.; Wan, T.; Yu, X.N.; Wu, F.; Yao, K. Corneal higher-order aberrations of the anterior surface, posterior surface, and total cornea after small incision lenticule extraction (SMILE): High myopia versus mild to moderate myopia. BMC Ophthalmol. 2018, 18, 295. [Google Scholar] [CrossRef]
- Chen, X.; Wang, Y.; Zhang, J.; Yang, S.N.; Li, X.; Zhang, L. Comparison of ocular higher-order aberrations after SMILE and Wavefront-guided Femtosecond LASIK for myopia. BMC Ophthalmol. 2017, 17, 42. [Google Scholar] [CrossRef]
- Zhou, X.; Qin, B.; Han, T.; Shang, J.; Chen, Z.; Zhao, J.; Yao, P.; Zhou, X. Long-Term Observation of Higher-Order Aberrations and Microdistortions in Bowman’s Layer after Small Incision Lenticule Extraction for the Correcting Myopia with Spherical Equivalent Higher Than -9.0 Diopters. Front. Med. 2022, 9, 814810. [Google Scholar] [CrossRef] [PubMed]
- Gyldenkerne, A.; Ivarsen, A.; Hjortdal, J. Comparison of corneal shape changes and aberrations induced By FS-LASIK and SMILE for myopia. J. Refract. Surg. 2015, 31, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Xu, Y.; Yang, Y. Comparison of the visual results after SMILE and femtosecond laser-assisted LASIK for myopia. J. Refract. Surg. 2014, 30, 248–254. [Google Scholar] [CrossRef]
- Tian, H.; Gao, W.; Xu, C.; Wang, Y. Clinical outcomes and higher order aberrations of wavefront-guided LASIK versus SMILE for correction of myopia: A systemic review and meta-analysis. Acta Ophthalmol. 2023, 101, 606–618. [Google Scholar] [CrossRef]
- Wu, Y.; Wang, S.; Wang, G.; Zhao, S.; Wei, R.; Huang, Y. Corneal Asphericity and Higher-Order Aberrations after FS-LASIK and Trans-PRK for Myopia. J. Ophthalmol. 2021, 2021, 3765046. [Google Scholar] [CrossRef] [PubMed]
- Miraftab, M.; Hashemi, H.; Aghamirsalim, M.; Fayyaz, S.; Asgari, S. Matched comparison of corneal higher order aberrations induced by SMILE to femtosecond assisted LASIK and to PRK in correcting moderate and high myopia: 3.00 mm vs. 6.00 mm. BMC Ophthalmol. 2021, 21, 216. [Google Scholar] [CrossRef]
- Jahadi Hosseini, S.H.; Abtahi, S.M.; Khalili, M.R. Comparison of Higher Order Aberrations after Wavefront-guided LASIK and PRK: One Year Follow-Up Results. J. Ophthalmic Vis. Res. 2016, 11, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Filini, O.; Salvalai, C.; Boldini, A.; Festa, G.; Delcassi, L.; Morescalchi, F.; Semeraro, F. Two-Year Changes in Corneal Spherical Aberration after Laser-Assisted In Situ Keratomileusis and Photorefractive Keratectomy in Regular and Wavefront-Guided Ablations. Ophthalmol. Ther. 2021, 10, 1003–1014. [Google Scholar] [CrossRef]
- Jun, I.; Kang, D.S.Y.; Roberts, C.J.; Lee, H.; Jean, S.K.; Kim, E.K.; Seo, K.Y. Comparison of Clinical and Biomechanical Outcomes of Small Incision Lenticule Extraction with 120- and 140-µm Cap Thickness. Transl. Vis. Sci. Technol. 2021, 10, 15. [Google Scholar] [CrossRef]
- Kang, D.S.Y.; Lee, H.; Reinstein, D.Z.; Roberts, C.J.; Arba-Mosquera, S.; Archer, T.J.; Kim, E.K.; Seo, K.Y.; Kim, T.I. Comparison of the Distribution of Lenticule Decentration Following SMILE by Subjective Patient Fixation or Triple Marking Centration. J. Refract. Surg. 2018, 34, 446–452. [Google Scholar] [CrossRef]
- Biscevic, A.; Ahmedbegovic-Pjano, M.; Pasalic, A.; Ziga, N.; Gabric, K.; Bohac, M. Changes in the Higher Order Ocular Aberrations and Central Corneal Thickness after T-PRK and Fs-LASIK. Acta Inform. Med. 2020, 28, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.M.; Ryu, I.H.; Lee, I.S.; Kim, J.K.; Kim, S.W.; Ji, Y.W. Comparison of Corneal Higher-Order Aberrations Following Topography-Guided LASIK and SMILE for Myopic Correction: A Propensity Score Matching Analysis. J. Clin. Med. 2022, 11, 6171. [Google Scholar] [CrossRef] [PubMed]


| Demographic | LASIK | PRK | SMILE | p-Values |
|---|---|---|---|---|
| Patients | 83 | 93 | 24 | |
| Eyes | n = 154 | n = 173 | n = 44 | |
| Age Mean ± SD | 34.0 ± 7.2 | 33.5 ± 5.6 | 33.1 ± 6.0 | 0.6224 |
| Age Range | 20, 51 | 20, 44 | 22, 45 | |
| Male-to-Female Ratio | 49 to 34 | 43 to 50 | 11 to 13 | 0.199 |
| Sphere ± SE (D) | −2.997 ± 0.220 | −3.327 ± 0.168 | −5.185 ± 0.350 * | <0.001 |
| Sphere Range (D) | −7.5, 1.5 | −7.75, 1 | −8.5, −2.25 | |
| Cylinder ± SE (D) | −1.024 ± 0.1 | −0.964 ± 0.09 | −0.443 ± 0.072 * | 0.011 |
| Cylinder Range (D) | −5.75, 0 | −4.25, 0 | −1.25, 0 | |
| Spherical Equivalent (D) | −3.509 ± 0.218 | −3.809 ± 0.162 | −5.406 ± 0.346 * | <0.001 |
| Spherical Equivalent Range (D) | −8.375, −0.25 | −8, −0.375 | −8.5, −2.75 | |
| Pachymetery Min (µm) | 548.896 ± 2.719 | 522.664 ± 3.217 * | 551.864 ± 6.832 | <0.001 |
| Pachymetery Apex (µm) | 552.734 ± 2.694 | 526.850 ± 3.179 * | 556.023 ± 0.023 | <0.001 |
| Pachymetery Pupil (µm) | 551.994 ± 2.701 | 526.26 ± 3.185 * | 555.568 ± 6.681 | <0.001 |
| Keratometry Mean ± SE (D) | 43.726 ± 0.146 | 44.175 ± 0.129 | 43.814 ± 0.212 | 0.08 |
| Keratometry Range (D) | 39.95, 47.2 | 41.2, 47.85 | 41.7, 46 | |
| Total HOAs (µm) | 0.348 ± 0.008 | 0.43 ± 0.012 * | 0.329 ± 0.011 | <0.001 |
| Total HOAs Range (µm) | 0.173, 0.625 | 0.197, 0.837 | 0.185, 0.504 | |
| Spherical Aberration (µm) | 0.197 ± 0.009 | 0.178 ± 0.009 | 0.183 ± 0.011 | 0.298 |
| Spherical Aberration Range (µm) | −0.065, 0.434 | −0.077, 0.417 | −0.016, 0.309 | |
| Vertical Coma (µm) | −0.092 ± 0.014 | −0.197 ± 0.021 * | −0.1 ± 0.024 | <0.001 |
| Vertical Coma Range (µm) | −0.349, 0.289 | −0.656, 0.711 | −0.345, 0.18 | |
| Horizontal Coma (µm) | 0.027 ± 0.006 | 0.036 ± 0.006 | 0.043 ± 0.009 | 0.361 |
| Horizontal Coma Range (µm) | −0.507, 0.442 | −0.427, 0.422 | −0.242, 0.249 | |
| Oblique Trefoil (µm) | −0.029 ± 0.008 | −0.01 ± 0.01 | −0.014 ± 0.013 | 0.314 |
| Oblique Trefoil Range (µm) | −0.233, 0.187 | −0.351, 0.268 | −0.184, 0.199 | |
| Horizontal Trefoil (µm) | −0.004 ± 0.005 | −0.006 ± 0.007 | −0.011 ± 0.011 | 0.872 |
| Horizontal Trefoil Range (µm) | −0.266, 0.214 | −0.294, 0.222 | −0.175, 0.201 |
| HOA Subtype Name | Procedure Name | Mean Pre-Test (μm) | Mean Post-Test (μm) | p-Value |
|---|---|---|---|---|
| Total HOAs | LASIK | 0.348 ± 0.00654 | 0.555 ± 0.0145 | <0.05 |
| PRK | 0.431 ± 0.0984 | 0.599 ± 0.0150 | <0.05 | |
| SMILE | 0.329 ± 0.00947 | 0.617 ± 0.0223 | <0.05 | |
| Spherical Aberration | LASIK | 0.197 ± 0.00656 | 0.313 ± 0.0117 | <0.05 |
| PRK | 0.178 ± 0.00709 | 0.324 ± 0.0105 | <0.05 | |
| SMILE | 0.183 ± 0.0950 | 0.305 ± 0.0254 | <0.05 | |
| Vertical Coma | LASIK | −0.0922 ± 0.0106 | −0.127 ± 0.0192 | <0.05 |
| PRK | −0.197 ± 0.0168 | −0.192 ± 0.0198 | 0.78 | |
| SMILE | −0.0990 ± 0.0184 | −0.323 ± 0.0312 | <0.05 | |
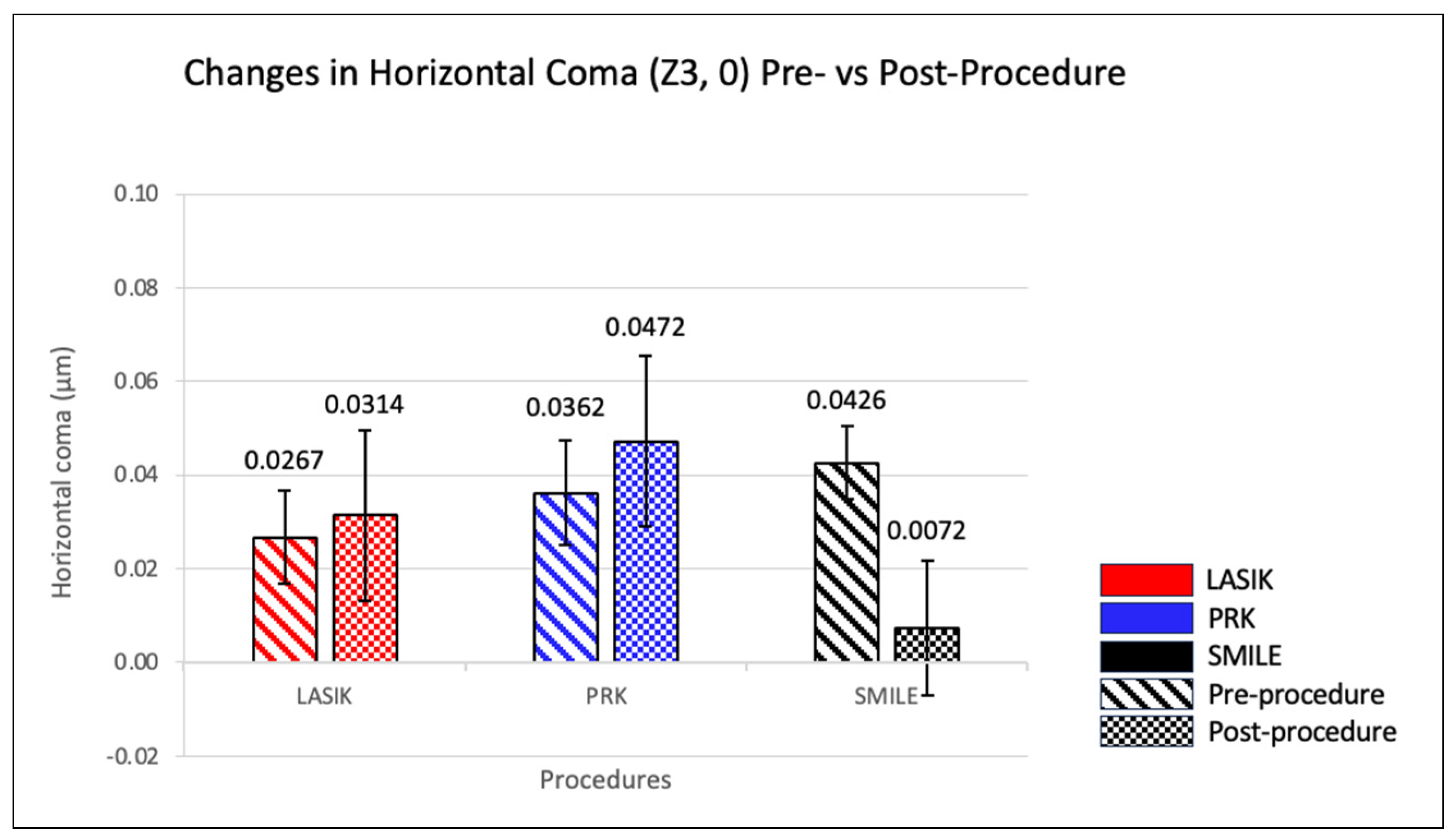
| Horizontal Coma | LASIK | 0.0267 ± 0.0106 | 0.0314 ± 0.0193 | 0.60 |
| PRK | 0.0362 ± 0.0112 | 0.0472 ± 0.0182 | 0.45 | |
| SMILE | 0.0426 ± 0.0156 | 0.00718 ± 0.0285 | 0.22 | |
| Oblique Trefoil | LASIK | −0.0290 ± 0.00746 | −0.0156 ± 0.0103 | 0.18 |
| PRK | −0.00953 ± 0.00843 | −0.0413 ± 0.0108 | <0.05 | |
| SMILE | −0.0145 ± 0.0121 | −0.0134 ± 0.0182 | 0.94 | |
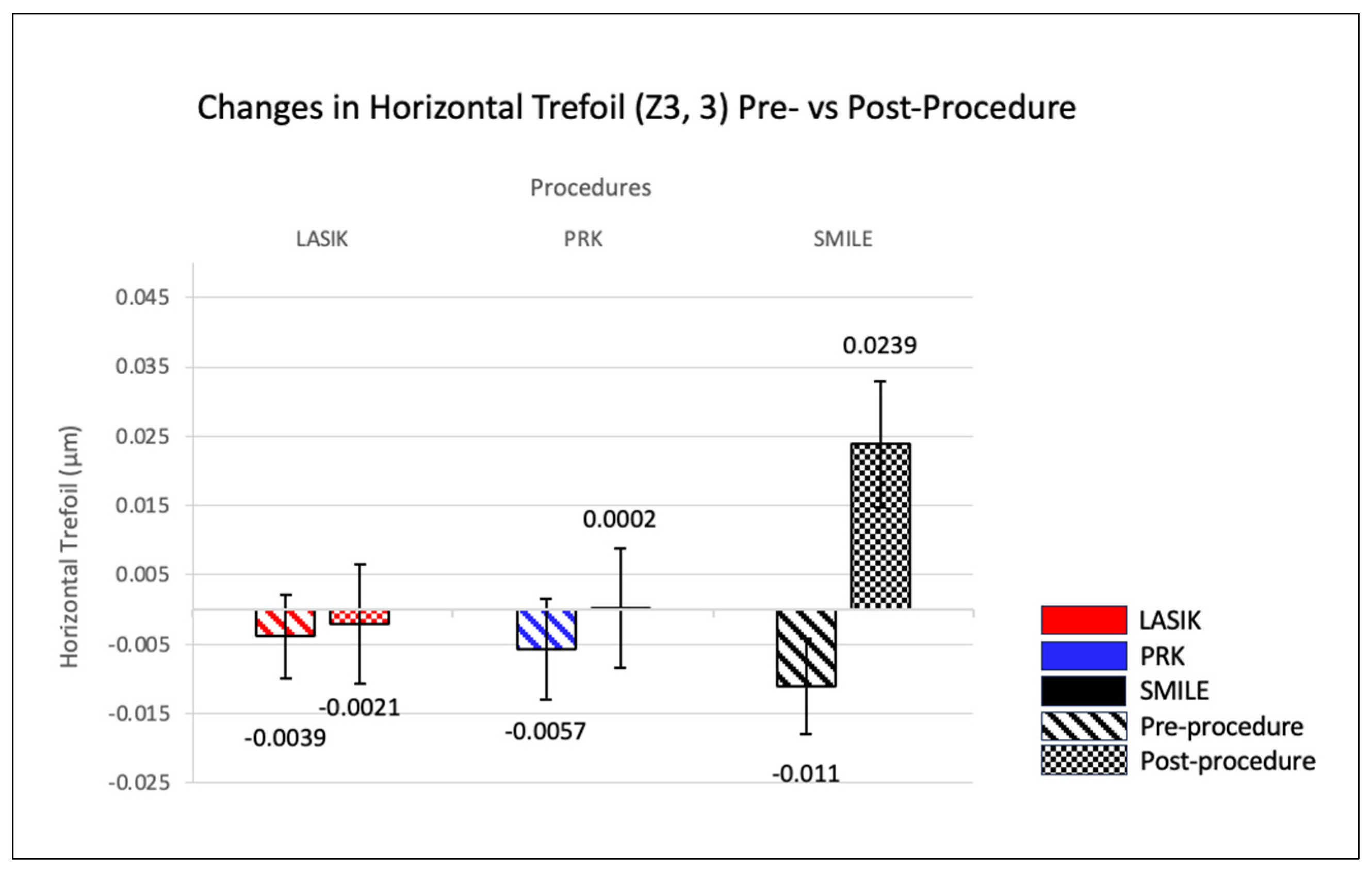
| Horizontal Trefoil | LASIK | −0.00395 ± 0.00649 | −0.00208 ± 0.00912 | 0.84 |
| PRK | −0.00574 ± 0.00730 | 0.000162 ± 0.00858 | 0.22 | |
| SMILE | −0.0110 ± 0.0137 | 0.0239 ± 0.0181 | 0.08 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moshirfar, M.; Omidvarnia, S.; Christensen, M.T.; Porter, K.B.; Theis, J.S.; Olson, N.M.; Stoakes, I.M.; Payne, C.J.; Hoopes, P.C. Comparative Analysis of Corneal Higher-Order Aberrations after Laser-Assisted In Situ Keratomileusis, Photorefractive Keratectomy, and Small Incision Lenticule Extraction with Correlations to Change in Myopic Q-Value and Spherical Equivalent with and without Astigmatism. J. Clin. Med. 2024, 13, 1906. https://doi.org/10.3390/jcm13071906
Moshirfar M, Omidvarnia S, Christensen MT, Porter KB, Theis JS, Olson NM, Stoakes IM, Payne CJ, Hoopes PC. Comparative Analysis of Corneal Higher-Order Aberrations after Laser-Assisted In Situ Keratomileusis, Photorefractive Keratectomy, and Small Incision Lenticule Extraction with Correlations to Change in Myopic Q-Value and Spherical Equivalent with and without Astigmatism. Journal of Clinical Medicine. 2024; 13(7):1906. https://doi.org/10.3390/jcm13071906
Chicago/Turabian StyleMoshirfar, Majid, Soroush Omidvarnia, Michael T. Christensen, Kaiden B. Porter, Josh S. Theis, Nathan M. Olson, Isabella M. Stoakes, Carter J. Payne, and Phillip C. Hoopes. 2024. "Comparative Analysis of Corneal Higher-Order Aberrations after Laser-Assisted In Situ Keratomileusis, Photorefractive Keratectomy, and Small Incision Lenticule Extraction with Correlations to Change in Myopic Q-Value and Spherical Equivalent with and without Astigmatism" Journal of Clinical Medicine 13, no. 7: 1906. https://doi.org/10.3390/jcm13071906





